METOJECT PEN 12.5 mg INJECTABLE SOLUTION IN PRE-FILLED PEN


How to use METOJECT PEN 12.5 mg INJECTABLE SOLUTION IN PRE-FILLED PEN
Translated with AI
This page provides general information and does not replace a doctor’s consultation. Always consult a doctor before taking any medication. Seek urgent medical care if symptoms are severe.
Show originalContents of the leaflet
Introduction
Package Leaflet: Information for the User
MetojectPEN 7.5mg solution for injection in pre-filled pen
MetojectPEN 10mg solution for injection in pre-filled pen
MetojectPEN 12.5mg solution for injection in pre-filled pen
MetojectPEN 15mg solution for injection in pre-filled pen
MetojectPEN 17.5mg solution for injection in pre-filled pen
MetojectPEN 20mg solution for injection in pre-filled pen
MetojectPEN 22.5mg solution for injection in pre-filled pen
MetojectPEN 25mg solution for injection in pre-filled pen
MetojectPEN 27.5mg solution for injection in pre-filled pen
MetojectPEN 30mg solution for injection in pre-filled pen
methotrexate
Read all of this leaflet carefully before you start using this medicine because it contains important information for you.
- Keep this leaflet, you may need to read it again.
- If you have any further questions, ask your doctor or pharmacist.
- This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours.
- If you experience any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet. See section 4.
Contents of the pack
- What Metoject PEN is and what it is used for
- What you need to know before you use Metoject PEN
- How to use Metoject PEN
- Possible side effects
- Storing Metoject PEN
- Contents of the pack and other information
1. What Metoject PEN is and what it is used for
Metoject PEN is indicated for the treatment of:
- active rheumatoid arthritis in adult patients,
- severe active polyarticular forms of juvenile idiopathic arthritis, when the response to non-steroidal anti-inflammatory drugs (NSAIDs) has not been adequate,
- moderate to severe psoriasis in adult patients, and severe psoriatic arthritis in adults,
- mild to moderate Crohn's disease in adult patients when adequate treatment with other medicines is not possible.
Rheumatoid arthritis (RA)is a chronic disease of the connective tissue, characterized by inflammation of the synovial membranes (joint membranes). These membranes produce a fluid that acts as a lubricant in many joints. Inflammation causes thickening of the membrane and swelling of the joint.
Juvenile arthritisaffects children and adolescents under 16 years of age. Polyarticular forms are indicated if there is involvement of 5 or more joints in the first 6 months of the disease.
Psoriasisis a chronic and frequent skin disease, characterized by red patches covered with thick, dry, silvery, and adherent scales.
Psoriatic arthritisis a type of arthritis with psoriatic lesions on the skin and nails, especially in the joints of the fingers and toes.
Metoject PEN modifies and slows down the progression of the disease.
Crohn's disease is a type of inflammatory bowel disease that can affect any part of the gastrointestinal tract, causing symptoms such as abdominal pain, diarrhea, vomiting, or weight loss.
2. What you need to know before you use Metoject PEN
Do not use Metoject PEN
- if you are allergic to methotrexate or any of the other ingredients of this medicine (listed in section 6),
- if you have severe liver or kidney disease or blood disorders,
- if you regularly drink large amounts of alcohol,
- if you have a severe infection, such as tuberculosis, HIV, or other immunodeficiency syndromes,
- if you have oral ulcers, gastric ulcers, or intestinal ulcers,
- if you are pregnant or breastfeeding (see section "Pregnancy, breastfeeding, and fertility"),
- if you are receiving live vaccines at the same time.
Warnings and precautions
Talk to your doctor or pharmacist before starting Metoject PEN
- if you are elderly or generally feel unwell and weak,
- if you have liver problems,
- if you have dehydration problems (loss of fluids).
- if you have diabetes mellitus and are being treated with insulin.
Special precautions for treatment with Metoject PEN
Methotrexate temporarily affects the production of sperm and eggs, which is reversible in most cases. Methotrexate can cause abortions and severe birth defects. If you are a woman, you should avoid becoming pregnant while using methotrexate and for at least 6 months after stopping treatment. If you are a man, you should avoid fathering a child if you are receiving methotrexate and for at least 3 months after stopping treatment. See also section "Pregnancy, breastfeeding, and fertility".
Follow-up tests and recommended precautions
Even if methotrexate is used in low doses, serious side effects can occur. To detect them in time, your doctor will need to perform tests and analytical controls.
Before starting treatment
Before starting treatment, you will have blood tests to check that you have enough blood cells. You will also have blood tests to check liver function and to find out if you have hepatitis. Additionally, serum albumin (a blood protein), hepatitis status (liver infection), and kidney function will be checked. Your doctor may also decide to perform other liver tests; some of these may involve images of the liver, and others may require taking a small tissue sample from the liver to examine it in more detail. Your doctor may also check if you have tuberculosis and may have a chest X-ray or a lung function test.
During treatment
Your doctor may perform the following tests:
- Examination of the oral cavity and pharynx to identify changes in the mucous membrane, such as inflammation or ulceration.
- Blood tests/blood cell counts with cell count and measurement of serum methotrexate levels.
- Blood tests to check liver function.
- Imaging tests to check liver function.
- Removal of a small tissue sample from the liver to examine it in more detail.
- Blood tests to check kidney function.
- Respiratory tract monitoring and, if necessary, a lung function test.
It is very important that you attend these scheduled tests.
If the results of any of these tests are abnormal, your doctor will adjust your treatment accordingly.
Elderly patients
Elderly patients treated with methotrexate should be closely monitored by a doctor to detect possible side effects as soon as possible.
The age-related decline in liver and kidney function and low body reserves of folic acid in the elderly require a relatively low dose of methotrexate.
Other precautions
Acute pulmonary hemorrhage has been reported with methotrexate in patients with underlying rheumatologic disease. If you notice blood when coughing or spitting, you should contact your doctor immediately.
Methotrexate can affect the immune system and vaccination results. It can also affect the results of immunological tests. It can reactivate chronic inactive infections (such as herpes zoster ["shingles"], tuberculosis, hepatitis B or C). During treatment with Metoject PEN, you should not receive live vaccines.
Methotrexate can make your skin more sensitive to sunlight. Avoid intense sunlight and do not use sunbeds or UV lamps without medical advice. To protect your skin from intense sunlight, wear suitable clothing or use a sunscreen with a high protection factor.
During treatment with methotrexate, radiation-induced dermatitis and sunburn (memory reactions) may recur. Psoriatic lesions may worsen during UV radiation and simultaneous administration of methotrexate.
An increase in lymph node size (lymphoma) may occur, and in such cases, treatment should be discontinued.
Diarrhea can be a side effect of Metoject PEN and requires discontinuation of treatment. If you have diarrhea, talk to your doctor.
Certain brain disorders (encephalopathy/leukoencephalopathy) have been reported in cancer patients treated with methotrexate. It cannot be ruled out that these side effects may occur when methotrexate is used to treat other diseases.
If you, your partner, or your caregiver notice the onset or worsening of neurological symptoms, such as general muscle weakness, vision changes, changes in thinking, memory, and orientation that cause confusion and changes in personality, contact your doctor immediately because these may be symptoms of a rare and severe brain infection called progressive multifocal leukoencephalopathy (PML).
Using Metoject PEN with other medicines
Tell your doctor or pharmacist if you are taking, have recently taken, or might take any other medicines. Keep this in mind for medicines that you may take in the future.
The effect of treatment may be affected if Metoject PEN is administered at the same time as certain medicines:
- Antibiotics such as tetracyclines, chloramphenicol, non-absorbable broad-spectrum antibiotics, penicillins, glycopeptides, sulfonamides, ciprofloxacin, and cefalotin (medicines to prevent or treat certain infections).
- Non-steroidal anti-inflammatory drugs (NSAIDs) or salicylates (medicines for pain or inflammation, such as acetylsalicylic acid, diclofenac, or ibuprofen, or pyrazolones).
- Metamizole (synonyms novaminsulfon and dipyrone) (medicine for severe pain and/or fever).
- Probenecid (medicine for gout).
- Weak organic acids such as loop diuretics.
- Medicines that can cause adverse effects on the bone marrow, such as trimethoprim-sulfamethoxazole (an antibiotic) and pyrimethamine.
- Other medicines used to treat rheumatoid arthritis, such as leflunomide, sulfasalazine, and azathioprine.
- Cyclosporin (to suppress the immune system).
- Mercaptopurine (a cytostatic medicine).
- Retinoids (medicines for psoriasis and other skin diseases).
- Theophylline (medicine for bronchial asthma and other lung diseases).
- Certain medicines for stomach discomfort, such as omeprazol and pantoprazol.
- Hypoglycemic agents (medicines used to reduce blood sugar levels).
Vitamins containing folic acidmay alter the effect of your treatment and should only be taken when advised by your doctor.
Live vaccines should be avoided.
Using Metoject PEN with food, drinks, and alcohol
During treatment with Metoject PEN, you should avoid consuming alcohol and large amounts of coffee, caffeinated soft drinks, and black tea.
Pregnancy, breastfeeding, and fertility
Pregnancy
Do not use Metoject PEN during pregnancy or if you are trying to become pregnant. Methotrexate can cause birth defects, harm the fetus, or cause abortions. It is associated with malformations of the skull, face, heart, and blood vessels, brain, and limbs. Therefore, it is very important that methotrexate is not administered to pregnant patients or those planning to become pregnant.
In women of childbearing age, any possibility of pregnancy should be ruled out with appropriate measures, such as a pregnancy test before starting treatment.
You should avoid becoming pregnant while taking methotrexate and for at least 6 months after stopping treatment, using reliable contraceptive methods during this time (see also section "Warnings and precautions").
If you become pregnant during treatment or suspect that you may be pregnant, consult your doctor as soon as possible. You should be informed about the risk of harmful effects on the child during treatment.
If you wish to become pregnant, consult your doctor, who may refer you to a specialist for information before the planned start of treatment.
Breastfeeding
Stop breastfeeding before and during treatment with Metoject PEN.
Male fertility
Available data do not indicate an increased risk of malformations or abortions if the father takes a dose of methotrexate less than 30 mg/week. However, this risk cannot be completely ruled out. Methotrexate can be genotoxic, which means it can cause genetic mutations. Methotrexate can affect sperm production and cause birth defects. Therefore, you should avoid fathering a child or donating sperm while taking methotrexate and for at least 3 months after stopping treatment.
Driving and using machines
Treatment with Metoject PEN can cause side effects that affect the central nervous system, such as fatigue and dizziness. Therefore, the ability to drive or use machines may be affected in some cases. If you feel tired or drowsy, you should not drive or use machines.
Metoject PEN contains sodium
This medicine contains less than 1 mmol of sodium (23 mg) per dose;it is essentially "sodium-free".
3. How to use Metoject PEN
Important dosage warning for Metoject PEN (methotrexate):
Use Metoject PEN only once a weekfor the treatment of rheumatoid arthritis, juvenile idiopathic arthritis, psoriasis, and psoriatic arthritis and Crohn's disease. Overuse of Metoject PEN (methotrexate) can be fatal. Read section 3 of this leaflet carefully. If you have any doubts, consult your doctor or pharmacist before using this medication.
Follow your doctor's instructions for administering this medication exactly. If in doubt, consult your doctor or pharmacist again.
Your doctor will determine the dose, which will be adjusted individually. Normally, the treatment takes between 4 and 8 weeks to take effect.
The injection of Metoject PEN is administered subcutaneously (under the skin) by or under the supervision of a doctor or healthcare professional only once a week. Together with your doctor, you will choose a day of the week that suits you to receive the injection.
Use in children and adolescents
The doctor decides what the appropriate dose is for children and adolescents with polyarticular forms of juvenile idiopathic arthritis.
Metoject PEN is not recommended for use in children under 3 years of agebecause experience is limited in this age group.
Duration and method of administration
Metoject PEN is injected once a week!
The attending doctor will decide on the duration of treatment. The treatment of rheumatoid arthritis, juvenile idiopathic arthritis, psoriasis vulgaris, psoriatic arthritis, and Crohn's disease with Metoject PEN is long-term treatment.
At the start of treatment, Metoject PEN may be injected by medical staff. However, your doctor may decide that you can learn to inject Metoject PEN yourself. You will receive the necessary training for this.
Under no circumstances should you attempt to inject yourselfunless you have been taught to do so.
Read the "Instructions for use" at the end of this leaflet for guidance on how to use Metoject PEN correctly.
Note that the entire contents must be used.
The handling and disposal of the medication and the pre-filled pen will be done in accordance with local regulations. Pregnant healthcare staff should not handle or administer Metoject PEN.
Methotrexate should not come into contact with the skin or mucous membranes. If it does come into contact, the affected area should be rinsed immediately with plenty of water.
If you use more Metoject PEN than you should
If you use more Metoject PEN than you should, consult your doctor immediately.
If you suspect that you (or someone else) have administered too much Metoject PEN, contact your doctor or go to the nearest hospital immediately or consult the Toxicology Information Service, phone 91 562 04 20. They will decide what measures to take based on the severity of the poisoning. Bring the medication with you if you go to the doctor or hospital.
If you forget to use Metoject PEN
Do not use a double dose to make up for forgotten doses.
If you stop treatment with Metoject PEN
If you stop treatment with Metoject PEN, consult your doctor immediately.
If you feel that the effect of Metoject PEN is too strong or too weak, consult your doctor or pharmacist.
4. Possible side effects
Like all medicines, this medicine can cause side effects, although not everybody gets them.
The frequency and severity of side effects will depend on the dose and frequency of administration. It is essential that your doctor performs regular checks, as serious side effects can occur even with the lowest doses. Your doctor will perform tests to detect abnormalitiesthat occur in the blood (such as low white blood cell count, low platelet count, or lymphoma) and changes in the kidneys and liver.
If you experience any of the following symptoms, contact your doctor immediately, as they may indicate a serious, potentially life-threatening side effect that requires urgent specific treatment:
- Dry cough, difficulty breathing, and fever; may be signs of lung inflammation [frequent]
- Blood when coughing or spitting; may be signs of pulmonary hemorrhage [unknown frequency]
- Symptoms of liver damage such as yellowing of the skin or whites of the eyes; methotrexate can cause chronic liver damage (liver cirrhosis), scarring of the liver (liver fibrosis), fatty liver degeneration [all infrequent], acute liver inflammation (hepatitis) [rare], and liver failure [very rare]
- Allergic symptoms such as skin rash, including itching, swelling of the hands, feet, ankles, face, lips, mouth, or throat (which can cause difficulty swallowing or breathing) and feeling of fainting;these may be signs of severe allergic reactions or anaphylactic shock [rare]
- Symptoms of kidney damage such as swelling of the hands, ankles, or feet or changes in urination frequency or decreased (oliguria) or absent (anuria) urine;these may be signs of kidney failure [rare]
- Symptoms of infection, e.g., fever, chills, pain, sore throat;methotrexate can make you more prone to infections. Serious infections such as a certain type of pneumonia (Pneumocystis jirovecii pneumonia) or sepsis [rare] can occur
- Symptoms such as weakness on one side of the body (stroke) or pain, swelling, redness, and unusual heat in one leg (deep vein thrombosis);this can happen when a blood clot breaks loose and blocks a blood vessel(thromboembolic event) [rare]
- Fever and severe deterioration of your general condition, or sudden fever accompanied by sore throat or mouth pain, or urinary problems; methotrexate can cause a sharp drop in the number of certain white blood cells (agranulocytosis) and severe bone marrow suppression [very rare]
- Unexpected bleeding, e.g., bleeding gums, blood in the urine, vomiting blood, or bruising,these may be signs of a severe decrease in the number of platelets caused by severe episodes of bone marrow depression [very rare]
- Symptoms such as severe headache, often in combination with fever, stiff neck, nausea, vomiting, disorientation, and sensitivity to lightmay indicate inflammation of the brain membranes (aseptic meningitis) [very rare]
- Certain brain disorders (encephalopathy/leukoencephalopathy) have been reported in cancer patients treated with methotrexate; these side effects cannot be ruled out when methotrexate treatment is used to treat other diseases; signs of this type of brain disorder may be altered mental state,movement disorders (ataxia), visual disorders, or memory disorders[unknown frequency]
- Severe skin rash or blistering of the skin (this can also affect the mouth, eyes, and genitals); these may be signs of a condition called Stevens-Johnson syndrome or toxic epidermal necrolysis [very rare]
The following are other side effects that may occur:
Very common:may affect more than 1 in 10 people
- Inflammation of the mouth lining, indigestion, nausea, loss of appetite, abdominal pain.
- Abnormal test results for liver function (ASAT, ALAT, bilirubin, alkaline phosphatase).
Common:may affect up to 1 in 10 people
- Mouth ulcers, diarrhea.
- Skin rash, redness of the skin, itching.
- Headache, fatigue, drowsiness.
- Decreased blood cell production with decreased white blood cell, red blood cell, or platelet count.
Uncommon:may affect up to 1 in 100 people
- Inflammation of the throat.
- Inflammation of the intestine, vomiting, pancreatitis, black or tarry stools, gastrointestinal ulcers, and bleeding.
- Reactions similar to sunburn due to increased skin sensitivity to sunlight, hair loss, increased number of rheumatoid nodules, skin ulcers, shingles, blood vessel inflammation, herpes-like rash, hives.
- Onset of diabetes mellitus.
- Dizziness, confusion, depression.
- Decreased serum albumin.
- Decreased number of all blood cells and platelets.
- Inflammation and ulceration of the urinary bladder or vagina, decreased kidney function, urinary disorders.
- Pain in the joints, muscle pain, reduced bone mass.
Rare:may affect up to 1 in 1,000 people
- Inflammation of the gum tissue.
- Increased skin pigmentation, acne, bruising on the skin due to bleeding from the blood vessels (ecchymosis, petechiae), allergic inflammation of the blood vessels.
- Decreased number of antibodies in the blood.
- Infection (including reactivation of inactive chronic infections), red eyes (conjunctivitis).
- Changes in mood (mood alterations).
- Visual disturbances.
- Inflammation of the sac around the heart, fluid accumulation in the sac around the heart, obstruction of heart filling due to fluid in the sac surrounding the heart.
- Low blood pressure.
- Scarring of the lung tissue (pulmonary fibrosis), difficulty breathing, and asthma, fluid accumulation in the sac surrounding the lung.
- Stress fracture.
- Electrolyte disturbances.
- Fever, altered wound healing.
Very rare:may affect up to 1 in 10,000 people
- Toxic and acute dilation of the intestine (toxic megacolon).
- Increased pigmentation of the nails, inflammation of the cuticles (acute paronychia), deep infection of the hair follicles (furunculosis), visible enlargement of small blood vessels.
- Pain, loss of strength, or sensation of numbness or tingling/sensitivity to stimuli less than normal, altered taste (metallic taste), seizures, paralysis, meningism.
- Visual disturbance, non-inflammatory eye disorder (retinopathy).
- Loss of sexual appetite, impotence, breast enlargement in men, altered sperm formation (oligospermia), menstrual disorders, vaginal discharge.
- Increased size of lymph nodes (lymphoma).
- Lymphoproliferative disorders (excessive increase in white blood cells).
Frequency not known:cannot be estimated from the available data
- Increased number of certain white blood cells.
- Nosebleeds.
- Protein in the urine.
- Feeling of weakness.
- Damage to the jawbone (secondary to excessive increase in white blood cells).
- Destruction of tissue at the injection site.
- Redness and peeling of the skin.
- Swelling.
Subcutaneous administration of methotrexate is well-tolerated locally. Only mild local skin reactions (such as burning sensations, erythema, swelling, color change, severe itching, pain) were observed, which decreased during treatment.
Reporting of side effects
If you experience any side effects, consult your doctor or pharmacist, even if they are possible side effects not listed in this leaflet. You can also report them directly through the Spanish Medicines Monitoring System for Human Use: www.notificaRAM.es. By reporting side effects, you can help provide more information on the safety of this medicine.
5. Storage of Metoject PEN
Keep this medicine out of the sight and reach of children.
Store below 25°C. Do not freeze.
Keep the pre-filled pens in the outer packaging to protect them from light.
Do not use this medicine after the expiry date stated on the carton and on the pre-filled pen after EXP. The expiry date is the last day of the month indicated.
Medicines should not be disposed of via wastewater or household waste. Dispose of the packaging and any unused medicine in the pharmacy's SIGRE collection point. If in doubt, ask your pharmacist how to dispose of the packaging and any unused medicine. This will help protect the environment.
6. Container Contents and Additional Information
Composition of MetojectPEN
- The active ingredient is methotrexate.
1 pre-filled pen with 0.15 ml of solution contains 7.5 mg of methotrexate.
1 pre-filled pen with 0.2 ml of solution contains 10 mg of methotrexate.
1 pre-filled pen with 0.25 ml of solution contains 12.5 mg of methotrexate.
1 pre-filled pen with 0.3 ml of solution contains 15 mg of methotrexate.
1 pre-filled pen with 0.35 ml of solution contains 17.5 mg of methotrexate.
1 pre-filled pen with 0.4 ml of solution contains 20 mg of methotrexate.
1 pre-filled pen with 0.45 ml of solution contains 22.5 mg of methotrexate.
1 pre-filled pen with 0.5 ml of solution contains 25 mg of methotrexate.
1 pre-filled pen with 0.55 ml of solution contains 27.5 mg of methotrexate.
1 pre-filled pen with 0.6 ml of solution contains 30 mg of methotrexate.
- The other components are sodium chloride, sodium hydroxide, and hydrochloric acid to adjust the pH and water for injectable preparations.
Appearance of the Product and Container Contents
This medicine is presented as an injectable solution in a pre-filled pen.
The solution is yellow-brown and transparent.
The pre-filled Metoject PEN is a three-step auto-injector with a yellow cap and a yellow injection button.
The pre-filled Metoject PEN is a two-step auto-injector with a translucent cap and a blue safety protector for the needle.
The following pack sizes are marketed:
Metoject PEN is available in packs of 1, 2, 4, 5, 6, 10, 11, 12, 14, 15, and 24 pre-filled pens.
Only some pack sizes may be marketed.
Marketing Authorization Holder and Manufacturer
medac Gesellschaft für klinische Spezialpräparate mbH
Theaterstr. 6
22880 Wedel
Germany
Tel.: +49 4103 8006-0
Fax: +49 4103 8006-100
You can request more information about this medicine by contacting the local representative of the marketing authorization holder:
Laboratorios Gebro Pharma, S.A.
Avenida Tibidabo n° 29
08022 Barcelona
Spain
Tel. +34 93 205 86 86
This medicine is authorized in the Member States of the European Economic Areaand in the United Kingdom (Northern Ireland)with the following names:
Austria, Slovakia, Slovenia, Spain, Finland, Greece, Hungary, Netherlands, United Kingdom (Northern Ireland), Czech Republic:
Metoject PEN
Iceland, Sweden: Metojectpen
Germany: metex PEN
Estonia, Latvia, Lithuania, Norway: Metex
Poland, Portugal:
Metex PEN
Denmark:
Metex Pen
Belgium:
Metoject
Date of the Last Revision of this Leaflet:August2024.
Detailed and updated information on this medicine is available on the website of the Spanish Agency for Medicines and Health Products (AEMPS) http://www.aemps.gob.es
You can access detailed and updated information on how to administer this medicine by scanning the QR code included in the packaging with your mobile phone (smartphone). You can also access this information at the following internet addresses:
Metoject PEN 7.5 mg solution for injection in pre-filled pen:
https://cima.aemps.es/info/78639
Metoject PEN 10 mg solution for injection in pre-filled pen:
https://cima.aemps.es/info/78632
Metoject PEN 12.5 mg solution for injection in pre-filled pen:
https://cima.aemps.es/info/78633
Metoject PEN 15 mg solution for injection in pre-filled pen:
https://cima.aemps.es/info/78634
Metoject PEN 17.5 mg solution for injection in pre-filled pen:
https://cima.aemps.es/info/78704
Metoject PEN 20 mg solution for injection in pre-filled pen:
https://cima.aemps.es/info/78638
Metoject PEN 22.5 mg solution for injection in pre-filled pen:
https://cima.aemps.es/info/78635
Metoject PEN 25 mg solution for injection in pre-filled pen:
https://cima.aemps.es/info/78636
Metoject PEN 27.5 mg solution for injection in pre-filled pen:
https://cima.aemps.es/info/78637
Metoject PEN 30 mg solution for injection in pre-filled pen:
https://cima.aemps.es/info/78631
Instructions for Use
Recommendations
- Read the following instructions carefully before starting the injection.
- Always use the injection technique advised by your doctor, pharmacist, or nurse.
Additional Information
The handling and disposal of the medicine and the pre-filled pen will be carried out in accordance with local regulations. Pregnant healthcare personnel should not handle or administer Metoject PEN.
Methotrexate should not come into contact with the skin or mucous membranes. If it does, the affected area should be rinsed immediately with plenty of water.
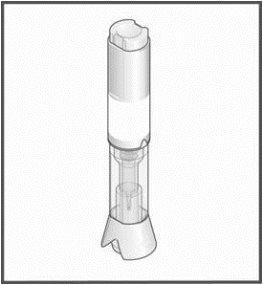
Components of thepre-filled MetojectPEN | |
| Injection button Handling area Transparent control zone Cap |
|
|
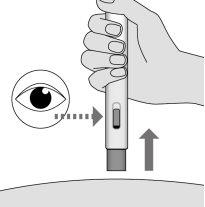
What to do before administering the injection
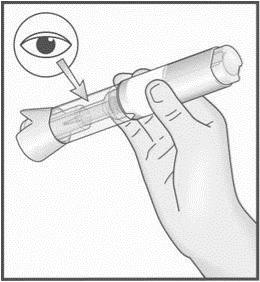
| |
| If the pre-filled Metoject PEN appears to be damaged do not use it. Use another pen and contact your doctor, pharmacist, or nurse. If a small air bubble is visible through the transparent control zone, this will not affect your dose or harm you. If you cannot see or examine the system correctly before the injection, ask someone around you for help. |
|
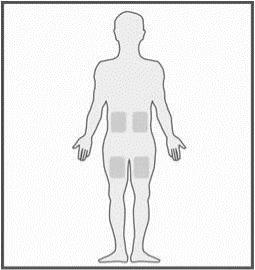
Where to Administer the Injection | |
| The most suitable areas for your injection are:
|
How to Prepare the Injection
|
|
| |
Note: once you have removed the cap, administer the injection without delay. | |
|
|
|
|
How to Administer the Injection: | |
|
|
Note: Do not remove the pre-filled Metoject PEN from the skin before the end of the injection to avoid an incomplete injection. If the injection does not fire, release the button, ensure that the pre-filled Metoject PEN is firmly pressed against the skin, and press the button firmly. If you have hearing problems, count 5 seconds from the moment you press the button and then lift the pre-filled Metoject PEN from the injection site. | |
|
Before throwing away the pre-filled Metoject PEN, visually check that there is no liquid left in the pen, in the lower part of the transparent control zone. If there is any liquid left in the pen, it means that not all the medicine has been injected correctly, and you should consult your doctor. |
Note
To avoid any injury, never insert your fingers into the opening of the protective tubethat covers the needle. Do not destroy the pen.
Who to Contact in Case of Need
- If you have any doubts or problems, contact your doctor, pharmacist, or nurse.
If you or someone around you is injured with the needle, consult your doctor immediately and throw away the pre-filled Metoject PEN.
INSTRUCTIONS FOR USE
The following "Instructions for Use" contain information on how to inject the pre-filled Metoject PEN.
Read these "Instructions for Use" to the end before using the pre-filled pen for subcutaneous injection. Read the "Instructions for Use" every time you receive a new prescription and keep them in case you need to consult them after the injection.
Every time you receive a new medicine or a different dose of the medicine, always make sure it matches what your doctor has prescribed. Before starting to use the pen, the healthcare professional will show you or your caregiver how to use it correctly.
Donot use the pen unless the healthcare professional has shown you how to do it. If you or your caregiver have any questions, contact the healthcare professional.
Important Information You Should Know Before Administering the Injection with the Pre-filled MetojectPEN |
Administer the injection with the pre-filled MetojectPEN once a week only and always on the same day of the week. Do not administer the injection or handle the product if you are pregnant.
Do notremove the cap until just before the injection. Do notshare the pen with anyone else. Do notuse the pen if:
In case of doubt, contact the healthcare professional. |
Storage of the Pre-filled MetojectPEN
- Store below 25 °C.
- Transport and store the pen in the outer packaging to protect it from light.
- Store the pen in a safe place out of sight and reach of children.
Do notfreeze.
Do notstore at a temperature above 25 °C.
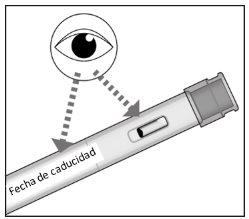
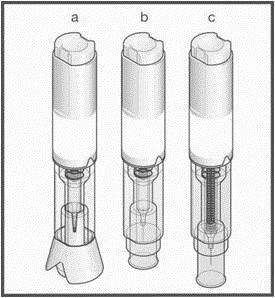
Pre-filled MetojectPEN (FigureA)
The pre-filled Metoject PEN is a disposable two-step auto-injector with a fixed dose. It is available in 10 different doses ranging from 7.5 mg to 30 mg.
Beforeuse | Afteruse | ||
Cap (translucent) Inspection window (the yellow medicine is inside) Piston (the position varies depending on the prescribed dose)
7.5 mg 15 mg 30 mg (example dose) Color code zone(individual for each dose) |
|
| Blue safety protector for the needle
Cap (the needle protector is inside) Blue piston rod (indicates that the injection is complete) Product label (to check the dose and expiration date) |
FigureA
Material Needed for the Injection (FigureB)
On the day of the weekly injection, look for a comfortable place and make sure the area is well-lit and that you have a flat and clean work surface (e.g., a table) to place all the necessary material for the injection.
You will need:
- the pre-filled Metoject PEN.
Make sure you have the following additional materials to administer the injection, as they are not included in the packaging:
- your calendar to check the day of the weekly injection,
- a skin cleaning product, such as an alcohol disinfectant; if you do not have one, you can use water and soap,
- a cotton swab or gauze to treat the injection site,
- a container for the disposal of medical waste in accordance with local regulations.
| ||||
Calendar showing the day of the weekly injection | Pre-filled Metoject PEN | Skin cleaning product | Cotton swab or gauze | Container for the disposal of medical waste |
FigureB
Preparation of the Injection | |
Do notremove the cap until you are ready to administer the injection. |
FigureC |
Check the name and dose that appear on the pen and make sure you have the correct medicine. If you cannot see it well, ask for help. |
- Check the expiration date on the pen label.
- Do not use the pen if it is expired.
- Examine the medication through the inspection window by turning it upside down or gently shaking it. The medication inside the pen should be clear and yellow.
- Do not administer the injection if the solution is cloudy, discolored, or contains particles.
- You may see one or more air bubbles. This is normal. Do not attempt to remove them.
- You may notice a scale on the window; disregard it.
- Make sure the pen is not damaged and the cap is firmly attached. Do not use the pen if it appears damaged or if the cap has been removed or is not securely attached.
If the pen has expired, appears damaged, or does not look as expected, do not use it and contact your healthcare professional.
Place the pen carefully on a flat, clean surface (e.g., a table) before proceeding with the following steps.
FigureD
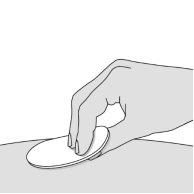
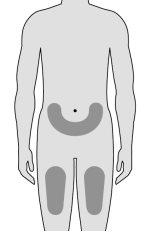
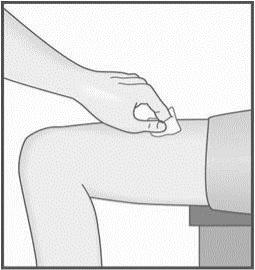
- Choose the injection site (Figure E)
- The injection can be administered in:
- the upper part of the thighs,
- the lower abdomen, except for the area within 5 cm around the navel.
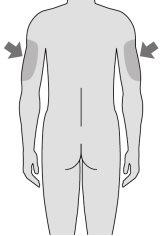
- If your caregiver is administering the injection, they can also use the upper outer part of the arm.
- Choose a different site each time you administer an injection.
When choosing the injection site:
Do notadminister the injection in other parts of the body.
Do notadminister the injection in areas where the skin is bruised, tender, scaly, red, or hardened.
Do notadminister the injection where you have moles, scars, or stretch marks.
Do notadminister the injection through clothing.
FigureE
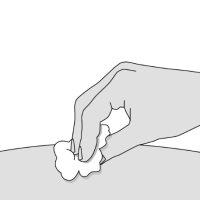
Do notfan or blow on the area you just cleaned. Do nottouch the injection site again until you have finished administering the injection. |
FigureF |
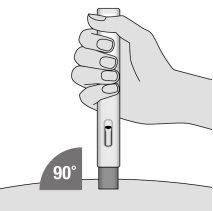
Injecting the dose | |
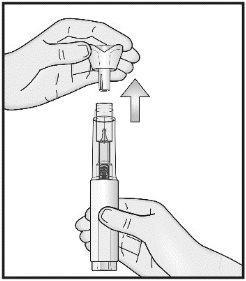
Do not remove the cap until you are ready to administer the injection. Do notput the cap back on the pen after it has been removed.
Do notbend or twist the cap while pulling it.
Do nottouch the blue safety shield for the needle with your fingers. If you do, you may accidentally trigger the injection and cause an injury. |
FigureG |
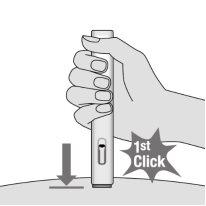
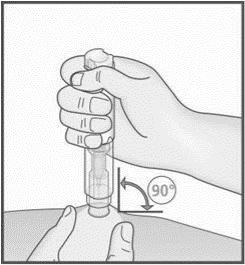
|
FigureH |
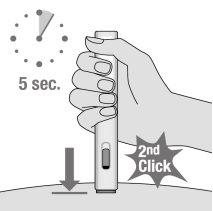
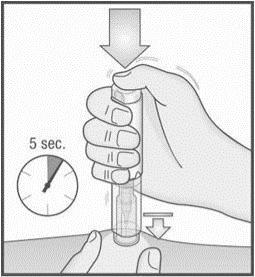
Do notchange the position of the pen once the injection has started. |
FigureI |
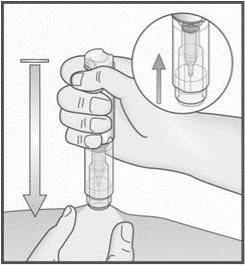
Do notremove the pen until at least 5 seconds have passed. |
FigureJ |
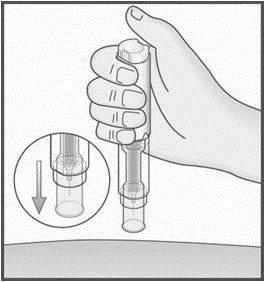
If you still see remaining yellow medication in the inspection window, you may not have received the full dose. If this happens or you have any other concerns, contact your healthcare professional. Do nottouch the blue safety shield for the needle after the injection, as this could cause an injury. |
FigureK |
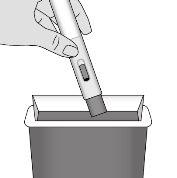
After the injection | |
Do notrub the injection site. |
FigureL |
Each pen can only be used once. Do notput the cap back on the pen. Keep the used pen and its cap out of sight and reach of children.
The medication and the pre-filled pen should be disposed of according to local regulations.
Properly dispose of expired, unused, or damaged Metoject PEN pre-filled pens. |
FigureM |
- Country of registration
- Active substance
- Prescription requiredYes
- Manufacturer
- This information is for reference only and does not constitute medical advice. Always consult a doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to METOJECT PEN 12.5 mg INJECTABLE SOLUTION IN PRE-FILLED PENDosage form: INJECTABLE, 10 mg/ 1 mlActive substance: methotrexateManufacturer: Ebewe Pharma Ges.M.B.H. Nfg.KgPrescription requiredDosage form: INJECTABLE, 15 mgActive substance: methotrexateManufacturer: Ebewe Pharma Ges.M.B.H. Nfg.KgPrescription requiredDosage form: INJECTABLE, 20 mgActive substance: methotrexateManufacturer: Ebewe Pharma Ges.M.B.H. Nfg.KgPrescription required
Online doctors for METOJECT PEN 12.5 mg INJECTABLE SOLUTION IN PRE-FILLED PEN
Discuss questions about METOJECT PEN 12.5 mg INJECTABLE SOLUTION IN PRE-FILLED PEN, including use, safety considerations and prescription review, subject to medical assessment and local regulations.
Frequently Asked Questions








 (locks after injection, the needle is inside)
(locks after injection, the needle is inside)