OROXELAM 5 mg SOLUÇÃO ORAL
Pergunte a um médico sobre a prescrição de OROXELAM 5 mg SOLUÇÃO ORAL

Como usar OROXELAM 5 mg SOLUÇÃO ORAL
Introdução
Prospecto: informação para o utilizador
Oroxelam 2,5 mg solução bucal
Oroxelam 5 mg solução bucal
Oroxelam 7,5 mg solução bucal
Oroxelam 10 mg solução bucal
midazolam
Leia todo o prospecto detenidamente antes de começar a usar este medicamento, porque contém informações importantes para si.
- Conserva este prospecto, porque pode ter que voltar a lê-lo.
- Se tiver alguma dúvida, consulte o seu médico ou farmacêutico.
- Este medicamento foi-lhe receitado apenas para si, e não deve dá-lo a outras pessoas, mesmo que tenham os mesmos sintomas que si, porque pode prejudicá-las.
- Se experimentar efeitos adversos, consulte o seu médico ou farmacêutico, mesmo que se trate de efeitos adversos que não aparecem neste prospecto. Ver seção 4.
Conteúdo do prospecto
- O que é Oroxelam e para que é utilizado
- O que necessita de saber antes de começar a usar Oroxelam
- Como usar Oroxelam
- Possíveis efeitos adversos
- Conservação de Oroxelam
- Conteúdo do envase e informação adicional
1. O que é Oroxelam e para que é utilizado
Oroxelam solução bucal contém um medicamento chamado midazolam. Midazolam pertence a um grupo de medicamentos conhecidos como benzodiazepinas.
Oroxelam é utilizado para deter uma crise convulsiva súbita e prolongada em lactentes desde 3 meses a adultos.
Em lactentes de 3 meses a menores de 6 meses, o tratamento deve ser administrado apenas num hospital em que se possa monitorizar o paciente e que conte com equipamento de reanimação.
Este medicamento deve ser utilizado apenas por pais/cuidadores quando se tenha diagnosticado epilepsia ao paciente.
2. O que necessita de saber antes de começar a usar Oroxelam
- Não use Oroxelam se o paciente tiver:
- alergia ao midazolam, às benzodiazepinas (como o diazepam) ou a algum dos outros componentes deste medicamento (incluídos na seção 6);
- uma doença dos nervos e músculos que produz fraqueza muscular (miastenia grave);
- sérias dificuldades respiratórias em repouso (Oroxelam pode fazer com que as dificuldades respiratórias piorem);
- uma doença que produz interrupções frequentes da respiração enquanto se dorme (síndrome de apneia do sono);
- problemas hepáticos graves.
Advertências e precauções:
Crianças:
Consulte o seu médico ou farmacêutico antes de começar a usar Oroxelam se o paciente:
- Tiver uma afecção renal, hepática ou cardíaca;
- Tiver uma afecção pulmonar que produz dificuldade respiratória de forma periódica.
Adultos:
Consulte o seu médico ou farmacêutico antes de começar a usar Oroxelam se:
- Você é maior de 60 anos.
- Você padece uma doença crónica (como insuficiência respiratória, ou insuficiência renal, hepática ou cardíaca).
- Você está debilitado (tem uma doença que o faz sentir muito débil, exausto e sem energia).
Este medicamento pode fazer com que as pessoas se esqueçam do que ocorreu após terem sido administradas. Deve-se observar detidamente os pacientes após a administração deste medicamento.
Este medicamento deve ser evitado em pacientes com antecedentes de alcoolismo ou toxicomania.
É mais provável que ocorram incidentes potencialmente mortais entre os pacientes com dificuldades respiratórias ou problemas cardíacos, especialmente quando se administram doses mais altas de Oroxelam.
Crianças menores de 3 meses: Oroxelam não deve ser administrado a crianças menores de 3 meses devido à falta de informação neste grupo etário.
Pacientes de idade avançada:
Os pacientes de idade avançada são mais sensíveis aos efeitos das benzodiazepinas.
Se tiver alguma dúvida sobre se algo do anterior é aplicável ao paciente, consulte o seu médico ou farmacêutico antes de administrar este medicamento.
Outros medicamentos e Oroxelam
Informar o seu médico ou farmacêutico se o paciente está utilizando, utilizou recentemente ou possa ter que utilizar qualquer outro medicamento. Se tiver alguma dúvida sobre algum medicamento que o paciente está tomando e que possa afetar o uso de Oroxelam, consulte o seu médico ou farmacêutico.
Isso é sumamente importante, porque o uso de mais de um medicamento ao mesmo tempo pode potenciar ou debilitar o efeito dos medicamentos tomados.
Os efeitos de Oroxelam podem intensificar-se com os seguintes medicamentos:
- antiepilépticos (para tratar a epilepsia), p. ex.: fenitoína
- antibióticos, p. ex.: eritromicina, claritromicina
- antifúngicos, p. ex.: cetoconazol, voriconazol, fluconazol, itraconazol, posaconazol
- medicamentos para as úlceras, p. ex.: cimetidina, ranitidina e omeprazol
- medicamentos utilizados para tratar a tensão arterial, p. ex.: diltiazem, verapamil
- alguns medicamentos utilizados para o VIH e SIDA, p. ex.: saquinavir, combinação de lopinavir/ritonavir
- analgésicos narcóticos (calmantes muito fortes), p. ex.: fentanil
- medicamentos utilizados para reduzir a gordura do sangue, p. ex.: atorvastatina
- medicamentos utilizados para tratar as náuseas, p. ex.: nabilona
- hipnóticos (medicamentos para induzir o sono)
- antidepressivos sedantes (medicamentos para tratar a depressão que produzem sono)
- sedantes (medicamentos para ajudar a relaxar)
- anestésicos (medicamentos para aliviar a dor)
- antihistamínicos (medicamentos para tratar alergias)
Os efeitos de Oroxelam podem reduzir-se com os seguintes medicamentos:
- rifampicina (utilizada para tratar a tuberculose)
- xantinas (utilizadas para tratar a asma)
- a erva de São João (um medicamento à base de plantas). Deve-se evitar nos pacientes que tomam Oroxelam.
Oroxelam pode aumentar o efeito de alguns relaxantes musculares, p. ex.: baclofeno (produzindo um aumento do sono). Este medicamento também pode fazer com que alguns medicamentos deixem de funcionar igual de bem, p. ex.: levodopa (um medicamento que se utiliza para tratar a doença de Parkinson).
Consulte o seu médico ou farmacêutico para obter mais informações sobre os medicamentos que o paciente deve evitar enquanto toma Oroxelam.
Uso de Oroxelam com alimentos e bebidas
O paciente não deve beber álcool enquanto toma Oroxelam. O álcool pode incrementar os efeitos sedantes deste medicamento e produzir-lhe muito sono.
O paciente não deve beber sumo de toranja enquanto toma Oroxelam. O sumo de toranja pode incrementar os efeitos sedantes deste medicamento e produzir-lhe muito sono.
Gravidez
Se a paciente que vai receber este medicamento está grávida ou em período de amamentação, acredita que possa estar grávida ou tem intenção de ficar grávida, consulte o seu médico antes de utilizar este medicamento.
A administração de doses altas de Oroxelam durante os últimos 3 meses de gravidez pode produzir batimento cardíaco anómalo no feto. As crianças nascidas após a administração deste medicamento durante o parto também podem apresentar dificuldade para mamar, dificuldades respiratórias e um tom muscular pobre ao nascer.
Amamentação
Informar o médico se a paciente está a amamentar. Apesar de que pequenas quantidades de Oroxelam podem passar para o leite materno, pode que não seja necessário suspender a amamentação. O médico aconselhará sobre se a paciente deve amamentar o bebê após receber uma única dose deste medicamento.
Condução e uso de máquinas
Oroxelam pode fazer com que o paciente se sinta sonolento, se esqueça das coisas ou veja afetada a sua concentração e coordenação. Isso pode interferir na execução de tarefas que requerem habilidade, tais como conduzir, andar de bicicleta ou utilizar máquinas.
Após receber este medicamento, o paciente não deve conduzir, andar de bicicleta nem utilizar máquinas até que se tenha recuperado por completo. Pergunte ao seu médico se necessita de mais informações.
Oroxelam contém sódio
Este medicamento contém menos de 1 mmol de sódio (23 mg) por seringa oral, isto é, essencialmente “isento de sódio”.
3. Como administrar Oroxelam
Siga exatamente as instruções de administração deste medicamento indicadas pelo seu médico. Em caso de dúvida, consulte novamente o seu médico ou farmacêutico.
Dose
O médico prescreverá a dose de Oroxelam apropriada, que normalmente vai depender da idade do paciente. Cada uma das doses tem uma cor diferente, que é mostrada na caixa, no tubo e na seringa que contém o medicamento.
Dependendo da idade, o paciente receberá uma das seguintes doses, em um envase etiquetado expressamente por cores:
Intervalo de idade | Dose | Cor da Etiqueta |
3 meses a menores de 1 ano | 2,5 mg | Amarela |
1 ano a menores de 5 anos | 5 mg | Azul |
5 anos a menores de 10 anos | 7,5 mg | Roxa |
10 anos a adultos | 10 mg | Laranja |
Uma seringa oral contém uma dose completa. Não administre mais de uma dose.
Os lactentes de 3 meses a menores de 6 meses apenas devem receber tratamento num hospital em que se possa monitorizar o paciente e que conte com equipamento de reanimação.
Preparação para a administração deste medicamento
Se o paciente apresentar uma crise convulsiva, deixe que o seu corpo se mova livremente, não tente segurá-lo. Mova-o apenas se correr perigo por sua proximidade a, por exemplo, águas profundas, fogo ou objetos cortantes.
Apoie a cabeça do paciente sobre algum objeto acolchoado, como, por exemplo, um travesseiro ou no seu colo. Verifique que o medicamento contém a dose correta para o paciente, de acordo com a sua idade.
Como administrar este medicamento
Pedir a um médico, farmacêutico ou enfermeiro que o ensine como tomar ou administrar este medicamento. Em caso de dúvida, pergunte sempre ao seu médico, farmacêutico ou enfermeiro.
A informação sobre como administrar este medicamento também aparece na etiqueta do tubo.
Oroxelam não deve ser injetado. Não se deve colocar nenhuma agulha na seringa.
Paso 1 | |
| Segurar o tubo de plástico, quebrar o lacre por um extremo e retirar a cápsula de fechamento. Retirar a seringa do tubo. |
Paso 2 | |
| Retirar a cápsula de fechamento transparente da ponta da seringa e descartá-la de forma segura. |
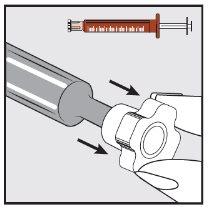
Paso 3 | |
| Com a ajuda do dedo indicador e do polegar, puxar suavemente para trás da bochecha do paciente. Colocar a ponta da seringa na parte posterior do espaço entre a bochecha e a gengiva inferior. |
Paso 4 | |
| Pressionar lentamente o êmbolo da seringa até que se detenha. Deve-se introduzir lentamente toda a solução no espaço entre a gengiva e a bochecha (cavidade bucal). Se o médico prescrever (para volumes grandes e/ou pacientes mais pequenos), pode-se administrar lentamente aproximadamente a metade da dose em um lado da boca e, a seguir, a outra metade no outro lado da boca do paciente. |
Quando chamar uma ambulância
Siga SEMPRE as recomendações de tratamento proporcionadas pelo médico do paciente ou tal como lhe indicou o profissional de saúde. Em caso de dúvida, solicite ajuda médica urgente se:
- A crise convulsiva não remite em um prazo de 10 minutos.
- É incapaz de esvaziar o conteúdo da seringa ou derrama algo do mesmo.
- A respiração do paciente se ralentiza ou detém (p. ex.: respiração lenta ou superficial ou lábios azuis).
- Observa sinais de infarto de miocárdio que podem incluir dor torácica ou dor que irradia ao pescoço e ombros e se estende até o braço esquerdo.
- O paciente vomita e a crise convulsiva não remite em um prazo de 10 minutos.
- Administra demasiado Oroxelam e observa sinais de sobredose que incluem:
- Sonolência, cansaço, fadiga
- Confusão ou desorientação
- Ausência de reflexo no joelho ou de resposta a um puxão
- Dificuldades respiratórias (respiração lenta ou superficial)
- Pressão arterial baixa (tontura e sensação de desmaio)
- Coma
Conserva a seringa para mostrar ao pessoal de saúde da ambulância ou ao médico.
Não administre mais quantidade de medicamento do que a prescrita pelo médico para o paciente.
Se o paciente vomitar
- Não administre ao paciente outra dose de Oroxelam.
- Se a crise convulsiva não remite em um prazo de 10 minutos, ligue para uma ambulância.
Se tiver alguma outra dúvida sobre o uso deste medicamento, pergunte ao seu médico ou farmacêutico.
4. Possíveis efeitos adversos
Como todos os medicamentos, este medicamento pode produzir efeitos adversos, embora nem todas as pessoas os sofram.
Efeitos adversos graves
Solicite atenção médica imediata ou ligue para um telefone para pedir uma ambulância se o paciente experimentar os seguintes efeitos adversos:
- Dificuldade respiratória grave, p. ex.: respiração lenta ou superficial ou lábios azuis. Em casos muito raros, pode parar a respiração.
- Infarto de miocárdio. Os sinais podem incluir dor torácica que pode irradiar ao pescoço e ombros do paciente e estender-se até o seu braço esquerdo.
- Inchaço de face, lábios, língua ou garganta que dificulte engolir ou respirar, ou pele pálida, pulso débil e rápido, ou sensação de perda do conhecimento. É possível que esteja tendo uma reação alérgica grave.
Outros efeitos adversos
Se o paciente experimentar qualquer tipo de efeito adverso, consulte o seu médico, farmacêutico ou enfermeiro, mesmo que se trate de possíveis efeitos adversos que não aparecem neste prospecto.
Efeitos adversos frequentes (podem afetar até 1 de cada 10 pessoas):
- Sentir-se e estar doente (náuseas e vómitos).
- Sonolência ou estar menos consciente
Efeitos adversos pouco frequentes (podem afetar até 1 de cada 100 pessoas):
- Erupção cutânea, urticária (ronchas), picor
Efeitos adversos muito raros (podem afetar até 1 de cada 10.000 pessoas):
- Agitação, inquietude, hostilidade, ira ou agressividade, excitação, confusão, euforia (sensação excessiva de alegria ou excitação) ou alucinações (ver e possivelmente ouvir coisas que realmente não ocorrem)
- Espasmos musculares e tremores musculares (tremor dos músculos que não se pode controlar)
- Nível de alerta reduzido
- Dor de cabeça
- Tontura
- Dificuldade para coordenar os músculos
- Crisis convulsivas (convulsões)
- Perda transitória da memória. A duração depende da quantidade de Oroxelam administrada.
- Pressão arterial baixa, frequência cardíaca lenta ou enrubescimento da face e pescoço (rubor)
- Espasmo laríngeo (contracção das cordas vocais que produz dificuldade respiratória e ruído ao respirar)
- Prisão de ventre
- Secura da boca
- Cansaço
- Soluço
Comunicação de efeitos adversos
Se experimentar qualquer tipo de efeito adverso, consulte o seu médico, farmacêutico ou enfermeiro, mesmo que se trate de possíveis efeitos adversos que não aparecem neste prospecto. Também pode comunicá-los diretamente através do Sistema Espanhol de Farmacovigilância de Medicamentos de Uso Humano: www.notificaram.es. Mediante a comunicação de efeitos adversos, você pode contribuir para proporcionar mais informações sobre a segurança deste medicamento.
5. Conservação de Oroxelam
Mantenha este medicamento fora da vista e do alcance das crianças.
Não utilize este medicamento após a data de validade que aparece no envase e nas etiquetas do tubo e da seringa para uso oral, após CAD. A data de validade é o último dia do mês que se indica.
Conservar por debaixo de 30 ºC
Mantenha a seringa para uso oral no tubo de plástico protetor.
Não utilize este medicamento se o envase estiver aberto ou danificado.
E
Os medicamentos não devem ser jogados nos esgotos nem na lixeira. Deposite os envases e os medicamentos que não necessita no Ponto SIGRE da farmácia. Pergunte ao seu farmacêutico como se livrar dos envases e dos medicamentos que já não necessita. Dessa forma, ajudará a proteger o meio ambiente.
6. Conteúdo do envase e informação adicional
Composição de oroxelam
O princípio ativo é midazolam
- Oroxelam 2,5 mg - Cada seringa precarregada para uso oral contém midazolam hidrocloruro equivalente a 2,5 mg de midazolam em 0,5 ml de solução.
- Oroxelam 5 mg - Cada seringa precarregada para uso oral contém midazolam hidrocloruro equivalente a 5 mg de midazolam em 1 ml de solução.
- Oroxelam 7,5 mg - Cada seringa precarregada para uso oral contém midazolam hidrocloruro equivalente a 7,5 mg de midazolam em 1,5 ml de solução.
- Oroxelam 10 mg - Cada seringa precarregada para uso oral contém midazolam hidrocloruro equivalente a 10 mg de midazolam em 2 ml de solução.
Os demais componentes são cloreto de sódio, água purificada, ácido clorídrico e hidróxido de sódio (para ajustar o pH).
Aspecto do produto e conteúdo do envase
Oroxelam 2,5 mg – envase com etiqueta amarela
Oroxelam 5 mg – envase com etiqueta azul
Oroxelam 7,5 mg – envase com etiqueta roxa
Oroxelam 10 mg – envase com etiqueta laranja
Oroxelam solução bucal é um líquido transparente e incolor.
Apresenta-se em uma seringa precarregada para uso oral de cor âmbar, sem agulha, com êmbolo e tampão. Cada seringa para uso oral vem envasada individualmente em um tubo de plástico protetor.
Oroxelam apresenta-se em caixas que contêm 2 ou 4 seringas precarregadas para uso oral (da mesma dosagem).
Pode ser que apenas alguns tamanhos de envase sejam comercializados.
Titular da autorização de comercialização e responsável pela fabricação
Titular da autorização de comercialização
Exeltis Healthcare, S.L.
Avenida de Miralcampo, 7.
Polígono Industrial Miralcampo.
19200 Azuqueca de Henares.
Guadalajara.
Espanha
Responsável pela fabricação
Laboratórios Liconsa S.A.
Av. de Miralcampo, 7
19200 Azuqueca de Henares
Guadalajara.
Espanha
Este medicamento está autorizado nos estados membros do espaço económico europeu com os seguintes nomes:
SE: Midazolam medical valley 2,5 mg, 5 mg, 7,5 mg, 10 mg munhålelösning.
FI: Midazolam medical valley 2,5 mg, 5 mg, 7,5 mg, 10 mg liuos suuonteloon.
DE: Midazaxiro 2,5 mg, 5 mg, 7,5 mg, 10 mg lösung zur anwendung in der mundhöhle.
NO: Midazolam medical valley 2,5 mg, 5 mg, 7,5 mg, 10 mg munnvann, oppløsning.
NL: Midazolam xiromed 2,5 mg, 5 mg, 7,5 mg, 10 mg oplossing voor oromucosaal gebruik.
DK: Midazolam medical valley 2,5 mg, 5 mg, 7,5 mg, 10 mg mundhulevæske, opløsning.
IS: Midazolam medical valley 2,5 mg, 5 mg, 7,5 mg, 10 mg munnholslausn.
FR: Midazolam liconsa 2,5 mg, 5 mg, 7,5 mg, 10 mg solution buccale.
IE: Midazolam liconsa 2,5 mg, 5 mg, 7,5 mg, 10 mg oromucosal solution.
RO: Midazolam desitin 2,5 mg, 5 mg, 7,5 mg, 10 mg soluție bucofaringiană.
ES: Oroxelam 2,5 mg, 5 mg, 7,5 mg, 10 mg solución bucal
PL: Soloxelam.
IT: Oroxelam.
Data da última revisão deste prospecto:março 2025
A informação detalhada deste medicamento está disponível na página web da Agência Espanhola de Medicamentos e Produtos Sanitários (AEMPS) http://www.aemps.gob.es

Quanto custa o OROXELAM 5 mg SOLUÇÃO ORAL em Espanha em 2025?
O preço médio do OROXELAM 5 mg SOLUÇÃO ORAL em dezembro de 2025 é de cerca de 86.8 EUR. Os valores podem variar consoante a região, a farmácia e a necessidade de receita. Confirme sempre com uma farmácia local ou fonte online para obter informações atualizadas.
- País de registo
- Preço médio em farmácia86.8 EUR
- Substância ativa
- Requer receita médicaSim
- Fabricante
- Esta informação é apenas para referência e não constitui aconselhamento médico. Consulte sempre um médico antes de tomar qualquer medicamento. A Oladoctor não se responsabiliza por decisões médicas baseadas neste conteúdo.
- Alternativas a OROXELAM 5 mg SOLUÇÃO ORALForma farmacêutica: GEL/PASTA/LÍQUIDO ORAL, 10 mg de cloridrato de midazolamSubstância ativa: midazolamFabricante: Neuraxpharm Pharmaceuticals S.L.Requer receita médicaForma farmacêutica: GEL/PASTA/LÍQUIDO ORAL, 2,5 mg de cloridrato de midazolamSubstância ativa: midazolamFabricante: Neuraxpharm Pharmaceuticals S.L.Requer receita médicaForma farmacêutica: GEL/PASTA/LÍQUIDO ORAL, 5 mg de cloridrato de midazolamSubstância ativa: midazolamFabricante: Neuraxpharm Pharmaceuticals S.L.Requer receita médica
Alternativas a OROXELAM 5 mg SOLUÇÃO ORAL noutros países
As melhores alternativas com o mesmo princípio ativo e efeito terapêutico.
Alternativa a OROXELAM 5 mg SOLUÇÃO ORAL em Polónia
Alternativa a OROXELAM 5 mg SOLUÇÃO ORAL em Ukraine
Médicos online para OROXELAM 5 mg SOLUÇÃO ORAL
Avaliação de posologia, efeitos secundários, interações, contraindicações e renovação da receita de OROXELAM 5 mg SOLUÇÃO ORAL – sujeita a avaliação médica e regras locais.