
DROSBELALLEFLEX 3 MG/0,02 MG COMPRIMIDOS RECUBIERTOS CON PELICULA

Cómo usar DROSBELALLEFLEX 3 MG/0,02 MG COMPRIMIDOS RECUBIERTOS CON PELICULA
Traducción generada por IA
Este contenido ha sido traducido automáticamente y se ofrece solo con fines informativos. No sustituye la consulta con un profesional sanitario.
Ver originalContenido del prospecto
Introducción
Prospecto: información para el paciente
Drosbelalleflex 3mg /0,02mg Comprimidos recubiertos con película
Drospirenona /Etinilestradiol
Lea todo el prospecto detenidamente antes de empezar a tomar este medicamento, porque contiene información importante para usted.
- Conserve este prospecto, ya que puede tener que volver a leerlo.
- Si tiene alguna duda, consulte a su médico o farmacéutico.
- Este medicamento se le ha recetado solamente a usted, y no debe dárselo a otras personas aunque tengan los mismos síntomas que usted, ya que puede perjudicarles.
- Si experimenta cualquier tipo de efecto adverso, consulte a su médico o farmacéutico, incluso si se trata de efectos adversos que no aparecen en este prospecto. Ver sección 4.
Información importante sobre los anticonceptivos hormonales combinados (AHC):
- Son uno de los métodos reversibles de anticoncepción más fiables cuando se utilizan correctamente
- Aumentan ligeramente el riesgo de tener un coágulo sanguíneo en las venas y arterias, especialmente en el primer año o al reiniciar la toma de un anticonceptivo hormonal combinado tras una pausa de 4 o más semanas
- Por favor, esté alerta y consulte a su médico si cree que presenta síntomas de coágulo sanguíneo (ver sección 2, «Coágulos sanguíneos»)
Contenido del prospecto
- Qué es Drosbelalleflex y para qué se utiliza
- Qué necesita saber antes de empezar a tomar Drosbelalleflex
- Cómo tomar Drosbelalleflex
- Posibles efectos adversos
- Conservación de Drosbelalleflex
- Contenido del envase e información adicional
1. Qué es Drosbelalleflex y para qué se utiliza
- Drosbelalleflex es una píldora anticonceptiva que se utiliza para evitar el embarazo.
- Cada uno de los 24 comprimidos contiene una pequeña cantidad de dos hormonas femeninas diferentes, denominadas drospirenona y etinilestradiol.
- Los anticonceptivos que contienen dos hormonas se denominan anticonceptivos combinados.
2. Qué necesita saber antes de empezar a tomar Drosbelalleflex
Antes de empezar a tomar Drosbelalleflex debe consultar con su médico cómo usar este producto. Antes de empezar a tomar Drosbelalleflex debe leer la información sobre coágulos sanguíneos en la sección 2. Es especialmente importante leer los síntomas de un coágulo sanguíneo; consulte la sección 2 «Coágulos sanguíneos». Antes de empezar a tomar Drosbelalleflex, su médico le hará algunas preguntas sobre sus antecedentes clínicos personales y familiares. El médico también le medirá la presión arterial y, dependiendo de su situación personal, podrá llevar a cabo algunas otras pruebas. En este prospecto se describen varias situaciones en las que usted debe interrumpir el uso de Drosbelalleflex, o en las que la fiabilidad de Drosbelalleflex puede disminuir. En dichas situaciones, usted no debería mantener relaciones sexuales o debería tomar precauciones anticonceptivas adicionales no hormonales, por ejemplo, uso de preservativo u otro método de barrera. No utilice el método del ritmo ni el de la temperatura. Estos métodos pueden no ser fiables puesto que Drosbelalleflex altera los cambios mensuales de la temperatura corporal y del moco cervical. Drosbelalleflex, al igual que otros anticonceptivos hormonales, no protege frente a la infección por el VIH (SIDA) o cualquier otra enfermedad de transmisión sexual. |
No tome Drosbelalleflex:
No debe utilizar Drosbelalleflex si padece alguno de los siguientes trastornos. Si padece alguno de los siguientes trastornos, debe informar a su médico. Su médico le dirá cuál sería el método anticonceptivo alternativo más adecuado.
- Si tiene (o ha tenido alguna vez) un coágulo sanguíneo en un vaso sanguíneo de las piernas (trombosis venosa profunda, TVP), de los pulmones (embolia pulmonar, EP) u otros órganos;
- Si tiene conocimiento de que sufre un trastorno que afecta a la coagulación, como deficiencia de proteína C, deficiencia de proteína S, deficiencia de antitrombina III, factor V de Leiden o anticuerpos antifosfolípidos;
- Si precisa cirugía o no está de pie durante mucho tiempo (consulte la sección «Coágulos sanguíneos»);
- Si usted tiene (o ha tenido en el pasado) un ataque al corazón o un accidente cerebrovascular;
- Si tiene (o ha tenido alguna vez) angina de pecho (una afección que causa un dolor torácico intenso y que puede ser el primer signo de un infarto de miocardio) o un accidente isquémico transitorio (AIT, síntomas transitorios de accidente cerebrovascular);
- Si tiene alguna de las enfermedades siguientes, que pueden aumentar el riesgo de presentar una trombosis en las arterias:
- diabetes grave con daños en los vasos sanguíneos
- tensión arterial muy alta
- niveles de grasa muy altos en la sangre (colesterol o triglicéridos)
- una enfermedad conocida como hiperhomocisteinemia
- Si tiene (o ha tenido en el pasado) un tipo de migraña llamado «migraña con aura»;
- Si usted tiene (o ha tenido en el pasado) una enfermedad del hígado y su función hepática no se ha normalizado todavía;
- Si sus riñones no funcionan bien (insuficiencia renal);
- Si usted tiene (o ha tenido en el pasado) un tumor en el hígado;
- Si usted tiene (o ha tenido en el pasado) o se sospecha que tiene cáncer de mama o cáncer de los órganos sexuales;
- Si usted tiene hemorragias vaginales de causa desconocida;
- Si es alérgica a etinilestradiol o drospirenona, o a cualquiera de los demás componentes de este medicamento (incluidos en la sección 6). Esto puede manifestarse con picor, erupción cutánea o hinchazón.
- No tome Drosbelalleflex si tiene hepatitis C y está tomando medicamentos que contienen ombitasvir/paritaprevir/ritonavir y dasabuvir, glecaprevir/pibrentasvir o sofosbuvir/velpatasvir/voxilaprevir (ver también la sección Uso de Drosbelalleflex con otros medicamentos).
Información adicional sobre poblaciones especiales
Niños y adolescentes
Drosbelalleflex no está indicado para su uso después de la menopausia.
Mujeres en edad avanzada
Drosbelalleflex no está indicado para su uso después de la menopausia.
Mujeres con insuficiencia hepática
No tome Drosbelalleflex si usted sufre una enfermedad hepática. Ver secciones “No use Drosbelalleflex” y “Advertencias y precauciones”.
Mujeres con insuficiencia renal
No tome Drosbelalleflex si usted está sufriendo un mal funcionamiento de sus riñones o un fallo renal agudo. Ver secciones “No use Drosbelalleflex” y “Advertencias y precauciones”.
Advertencias y precauciones
¿Cuándo debe contactar con su médico? Solicite atención médica urgente
Para obtener una descripción de los síntomas de estos efectos adversos graves consulte la sección «Cómo reconocer un coágulo sanguíneo». |
Informe a su médico si padece alguno de estos trastornos.
- En algunas situaciones, usted deberá tener especial cuidado mientras use Drosbelalleflex o cualquier otro anticonceptivo hormonal combinado, y puede ser necesario que su médico le examine de forma periódica.
También debe informar a su médico si la afección se desarrolla o empeora mientras está usando Drosbelalleflex.si una pariente cercana tiene o ha tenido alguna vez cáncer de mama;
- si tiene alguna enfermedad del hígado o de la vesícula biliar;
- si es diabética;
- si sufre depresión;
- si tiene enfermedad de Crohn o colitis ulcerosa (enfermedad inflamatoria intestinal crónica);
- si tiene lupus eritematoso sistémico (LES, una enfermedad que afecta al sistema de defensa natural);
- si tiene síndrome hemolítico urémico (SHU, un trastorno en la coagulación que causa insuficiencia renal);
- si tiene anemia drepanocítica (una enfermedad hereditaria de los glóbulos rojos);
- si tiene niveles elevados de grasa en la sangre (hipertrigliceridemia) o antecedentes familiares positivos de este trastorno. La hipertrigliceridemia se ha asociado a un mayor riesgo de desarrollo de pancreatitis (inflamación del páncreas);
- si precisa cirugía o no está de pie durante mucho tiempo (consulte la sección 2 «Coágulos sanguíneos»);
- si acaba de dar a luz tiene un mayor riesgo de presentar coágulos sanguíneos. Debe preguntar a su médico cuánto tiempo después de dar a luz puede empezar a tomar Drosbelalleflex;
- Si tiene inflamación en las venas bajo la piel (tromboflebitis superficial);
- si tiene varices;
- si tiene epilepsia (consulte la sección «Otros medicamentos y Drosbelalleflex»)
- si tiene una enfermedad que ha aparecido por primera vez durante el embarazo o la utilización previa de hormonas sexuales (p. ej., pérdida de audición, una enfermedad de la sangre llamada porfiria, erupción cutánea con ampollas durante el embarazo (herpes gestacional), una enfermedad nerviosa que causa movimientos espasmódicos del organismo (corea de Sydenham);
- si usted tiene o ha tenido alguna vez manchas de color pardo dorado (cloasma), también llamadas «manchas del embarazo», especialmente en la cara. En este caso, evite la exposición directa al sol o a los rayos ultravioleta;
- Si experimenta síntomas de angioedema como hinchazón de cara, lengua y/o garganta y/o dificultad para tragar o urticaria con posible dificultad para respirar, contacte con un médico inmediatamente. Los productos que contienen estrógenos pueden causar o empeorar los síntomas de angioedema hereditario y adquirido.
COÁGULOS SANGUÍNEOS
La toma de anticonceptivos hormonales combinados como Drosbelalleflex aumenta el riesgo de desarrollar coágulos sanguíneos en comparación con no tomarlos. En casos aislados, un coágulo sanguíneo puede bloquear los vasos sanguíneos y causar problemas graves.
Los coágulos sanguíneos pueden desarrollarse
- en venas (lo que se conoce como «trombosis venosa», «tromboembolia venosa» o TEV)
- en las arterias (lo que se conoce como «trombosis arterial», «tromboembolia arterial» o TEA).
La recuperación tras los coágulos sanguíneos no siempre es completa. En casos aislados pueden presentarse efectos crónicos o, muy raramente, estos pueden ser mortales.
Es importante tener en cuenta que el riesgo global de un coágulo sanguíneo nocivo causado por Drosbelalleflex es bajo.
CÓMO RECONOCER UN COÁGULO SANGUÍNEO
Solicite atención médica urgente si nota alguno de los siguientes signos o síntomas.
¿Experimenta alguno de estos signos? | ¿Qué puede estar padeciendo? |
| Trombosis venosa profunda |
Si no está segura consulte a su médico, ya que algunos de estos síntomas, como la tos o la dificultad para respirar, pueden ser confundidos con un trastorno más leve, como una infección de las vías respiratorias (p. ej., un «resfriado común»). | Embolia pulmonar |
Síntomas que se presentan de forma más frecuente en un ojo:
| Trombosis de la vena retiniana (coágulo sanguíneo en el ojo) |
| Infarto de miocardio |
Ocasionalmente, los síntomas de un accidente cerebrovascular pueden ser breves y con una recuperación total y casi inmediata, pero debe buscar atención médica urgente porque existe el riesgo de sufrir otro accidente. | Accidente cerebrovascular |
| Coágulos sanguíneos que bloquean otros vasos sanguíneos |
COÁGULOS SANGUÍNEOS EN UNA VENA
¿Qué puede suceder si se forma un coágulo sanguíneo en una vena?
- Se ha relacionado la toma de anticonceptivos hormonales combinados con un aumento del riesgo de coágulos sanguíneos venosos (trombosis venosa). No obstante, estos efectos adversos son infrecuentes. De modo más frecuente, se presentan durante el primer año de uso de un anticonceptivo hormonal combinado.
- Si se forma un coágulo sanguíneo en una vena de la pierna o pie, puede causar una trombosis venosa profunda (TVP).
- Si un coágulo sanguíneo se desplaza desde la pierna y se aloja en un pulmón puede provocar una embolia pulmonar.
- Muy raramente, se puede formar un coágulo sanguíneo en una vena de otro órgano, como el ojo (trombosis de la vena retiniana).
¿Cuándo es mayor el riesgo de desarrollar un coágulo sanguíneo en una vena?
El riesgo de desarrollar un coágulo sanguíneo en una vena es máximo durante el primer año tras de la primera toma de un anticonceptivo hormonal combinado. El riesgo también puede ser mayor después de reiniciar la toma de un anticonceptivo hormonal combinado (el mismo u otro producto) tras una pausa de 4 semanas o más.
Después del primer año, el riesgo disminuye, pero siempre es algo mayor que al no utilizar anticonceptivos hormonales combinados.
Al dejar de usar Drosbelalleflex el riesgo de sufrir un coágulo sanguíneo desciende hasta niveles normales al cabo de algunas semanas.
¿Cuál es el riesgo de desarrollar un coágulo sanguíneo?
El riesgo depende del riesgo innato de TEV y del tipo de anticonceptivos hormonales combinados que toma.
El riesgo global de sufrir un coágulo sanguíneo en la pierna o en el pulmón (TVP o EP) con Drosbelalleflex es bajo.
- De 10.000 mujeres que no toman anticonceptivos hormonales combinados y no están embarazadas, unas 2 pueden tener un coágulo sanguíneo en un año.
- De 10.000 mujeres que toman anticonceptivos hormonales combinados que contienen levonorgestrel, noretisterona o norgestimato, entre 5 y 7 pueden tener un coágulo sanguíneo en un año.
- De 10.000 mujeres que toman anticonceptivos hormonales combinados que contienen drospirenona como Drosbelalleflex entre 9 y 12 pueden tener un coágulo sanguíneo en un año.
- El riesgo de coágulo sanguíneo varía según sus antecedentes médicos personales (consulte «Factores que aumentan el riesgo de coágulo sanguíneo» a continuación)
Riesgo de desarrollo de coágulo sanguíneo en un año | |
Mujeres que no usanun anticonceptivo hormonal combinado/parche/anillo y no están embarazadas | Cerca de 2 mujeres de cada 10.000 |
Mujeres que usan un comprimido anticonceptivo hormonal combinado que contiene levonorgestrel, noretisterona o norgestimato | Entre 5 y 7 mujeres de cada 10.000 |
Mujeres que usan Drosbelalleflex | Entre 9 y 12 mujeres de cada 10.000 |
Factores que aumentan el riesgo de coágulo sanguíneo en una vena
El riesgo de coágulo sanguíneo con Drosbelalleflex es bajo, pero algunos trastornos aumentan el riesgo. El riesgo aumenta:
- si tiene sobrepeso (índice de masa corporal o IMC por encima de 30 kg/m²);
- si alguno de sus familiares cercanos ha tenido un coágulo sanguíneo en la pierna, los pulmones o en cualquier otro órgano a una edad temprana (p. ej., antes de los 50 años). Si es así, usted podría sufrir un trastorno hereditario en la coagulación;
- si precisa cirugía o no puede estar de pie durante mucho tiempo debido a una lesión o enfermedad, o tiene la pierna enyesada. Se puede tener que interrumpir la toma de Drosbelalleflex durante varias semanas antes de la cirugía o mientras tenga movilidad reducida. Si necesita interrumpir la toma de Drosbelalleflex pida a su médico que le indique cuándo puede reiniciar la toma.
- al envejecer (especialmente a partir de los 35 años, aproximadamente);
- si ha dado a luz hace pocas semanas;
El riesgo de desarrollo de coágulo sanguíneo aumenta con la cantidad de trastornos que sufre.
Los viajes en avión (> 4 horas) pueden aumentar temporalmente el riesgo de coágulo sanguíneo, especialmente si ya sufre alguno de los factores antes indicados.
Es importante que informe a su médico si cumple alguno de estos supuestos, aunque no está segura. Su médico puede decidir interrumpir la toma de Drosbelalleflex
Si alguna de estos supuestos se altera mientras toma Drosbelalleflex, p. ej., que un familiar cercano sufra una trombosis por causas desconocidas, o si aumenta mucho de peso, informe a su médico.
COÁGULOS SANGUÍNEOS EN UNA ARTERIA
¿Qué puede suceder si se forma un coágulo sanguíneo en una arteria?
Al igual que un coágulo sanguíneo en una vena, un coágulo en una arteria puede causar problemas graves. Por ejemplo, puede causar un ataque al corazón o un accidente cerebrovascular.
Factores que aumentan el riesgo de coágulo sanguíneo en una arteria
Es importante tener en cuenta que el riesgo de ataque al corazón o accidente cerebrovascular debido a la toma de Drosbelalleflex es muy bajo pero puede aumentar:
- con la edad (a partir de aproximadamente 35 años);
- si es fumadora.Cuando toma un anticonceptivo hormonal combinado como Drosbelalleflex se le aconseja dejar de fumar. Si no puede dejar de fumar y tiene más de 35 años, su médico puede aconsejarle la utilización de un tipo distinto de anticoncepción;
- si tiene sobrepeso;
- si tiene la tensión arterial alta;
- si alguno de sus familiares cercanos ha sufrido un ataque al corazón o un accidente cerebrovascular a una edad temprana (antes de los 50 años). En este caso, usted también puede presentar un mayor riesgo de ataque al corazón o accidente cerebrovascular;
- si usted o alguno de sus familiares cercanos tiene un nivel elevado de grasa en la sangre (colesterol o triglicéridos);
- si sufre migrañas, especialmente migrañas con aura;
- si tiene problemas de corazón (trastornos de las válvulas, alteración del ritmo cardíaco conocida como fibrilación auricular);
- si tiene diabetes.
Si tiene más de una de estas afecciones o si alguna de ellas es particularmente grave, el riesgo de desarrollar un coágulo sanguíneo puede ser aún mayor.
Si alguno de estos supuestos se altera mientras toma Drosbelalleflex, p. ej., si empieza a fumar, un familiar cercano sufre una trombosis por causas desconocidas o si aumenta mucho de peso, informe a su médico.
Drosbelalleflex y cáncer
Se han observado casos de cáncer de mama con una frecuencia ligeramente mayor en las mujeres que utilizaban píldoras combinadas, pero se desconoce si la causa es el tratamiento. Por ejemplo, puede ser que se detecten más tumores en mujeres que usan anticonceptivos combinados porque son examinadas por el médico más a menudo. La incidencia de tumores de mama disminuye gradualmente después de dejar de tomar anticonceptivos hormonales combinados. Es importante que se explore con regularidad las mamas y que se ponga en contacto con su médico si nota cualquier bulto.
En raras ocasiones se han comunicado tumores benignos en el hígado, y más raramente tumores malignos en usuarias de anticonceptivos. Acuda a su médico si usted sufre un dolor abdominal inusualmente fuerte.
Trastornos psiquiátricos
Algunas mujeres que utilizan anticonceptivos hormonales como Drosbelalleflex han notificado depresión o un estado de ánimo deprimido. La depresión puede ser grave y a veces puede inducir pensamiento suicidas. Si experimenta alteraciones del estado de ánimo y síntomas depresivos, póngase en contacto con su médico para obtener asesoramiento médico adicional lo antes posible.
Sangrado entre periodos
Durante los primeros meses en los que usted esté tomando Drosbelalleflex, puede tener sangrados inesperados (sangrados fuera de del intervalo sin comprimidos). Si estos sangrados persisten después de unos meses, o comienzan tras unos meses, su médico debe investigar la causa.
Qué debe hacer si no tiene la regla durante el intervalo de 4días sin comprimidos
Si ha tomado todos los comprimidos correctamente, no ha sufrido vómitos ni diarrea grave y no ha tomado otros medicamentos, es muy poco probable que esté embarazada.
En caso de que el sangrado previsto no se produzca dos veces sucesivas, podría estar embarazada. Acuda a su médico inmediatamente.
Si recibe tratamiento con Drosbelalleflex para retrasar los periodos, normalmente no se produce hemorragia por privación cada 4 semanas sino con una frecuencia reducida, con intervalos de hasta 120 días. Un embarazo inesperado puede ser difícil de reconocer. Si por cualquier motivo cree que podría estar embarazada, debe realizarse una prueba de embarazo. Si el resultado es positivo, o todavía tiene dudas, póngase en contacto con su médico.
No comience con la siguiente tira hasta que no esté segura de que no está embarazada.
Niños y adolescentes
Drosbelalleflex solo está indicado después de la menarquía.
Otros medicamentos y Drosbelalleflex
Informe al médico en todo momento sobre medicamentos o preparados a base de hierbas que está tomando. Informe también a cualquier otro médico o dentista que le recete otro medicamento (o a su farmacéutico) de que usa Drosbelalleflex. Ellos pueden indicarle si usted debe tomar precauciones anticonceptivas adicionales (p. ej., preservativos) y, si es así, durante cuánto tiempo o, si debe cambiar el uso de algún otro medicamento que esté tomando |
Algunos medicamentos:
- pueden tener influencia en los niveles sanguíneos de Drosbelalleflex
- pueden provocar que este sea menos efectivo en la prevencion del embarazo,
- pueden causar sangrados inesperados.
Entre ellos se incluyen:
- medicamentos utilizados en el tratamiento de:
- la epilepsia (p. ej. primidona, fenitoína, barbitúricos, carbamazepina, oxcarbazepina)
- la tuberculosis (p. ej. rifampicina)
- infecciones víricas por VIH y virus de la Hepatitis C (los llamados inhibidores de proteasa e inhibidores no nucleósidos de transcriptasa inversa como ritonavir, nevirapina, efivarenz)
- infecciones fúngicas (griseofulvina, ketoconazol)
- artritis, artrosis (etoricoxib)
- la presión alta en los vasos sanguíneos de los pulmones (bosentán)
- y los preparados a base de hierba de San Juan
Drosbelalleflex puede influir sobre el efecto de otros medicamentos, por ejemplo:
- medicamentos que contienen ciclosporina
- el antiepiléptico lamotrigina (puede llevar a un aumento de la frecuencia de convulsiones)
- teofilina (utilizado para tratar problemas respiratorios)
- tizanidina (utilizado para tratar ek dolor muscular y/o los calambres musculares)
No tome Drosbelalleflex si usted tiene Hepatitis C y está tomando medicamentos que contienen ombitasvir/paritaprevir/ritonavir y dasabuvir o glecaprevir/pibrentasvir o sofosbuvir/velpatasvir/voxilaprevir, ya que estos medicamentos pueden causar aumentos en los parámetros que miden la función hepática en la sangre (aumento de la enzima hepática ALT).
Su médico le prescribirá otro tipo de anticonceptivo antes de comenzar el tratamiento con estos medicamentos. Drosbelalleflex se puede volver a tomar aproximadamente 2 semanas después de la finalización de este tratamiento. Consulte sección “No use Drosbelalleflex”
Consulte a su médico o farmacéutico antes de utilizar cualquier medicamento.
Toma de Drosbelalleflexcon los alimentos y bebidas
Drosbelalleflex se puede tomar con o sin alimentos, y con algo de agua si fuera necesario.
Pruebas analíticas
Si usted necesita un análisis de sangre, comente con su médico o con el personal del laboratorio que está tomando un anticonceptivo, ya que los anticonceptivos orales pueden influir en los resultados de algunas pruebas.
Embarazo
Si usted está embarazada, no debe tomar Drosbelalleflex. Si se queda embarazada mientras toma Drosbelalleflex debe interrumpir el tratamiento inmediatamente y ponerse en contacto con su médico. Si desea quedarse embarazada, puede dejar de tomar Drosbelalleflex en cualquier momento (consulte también «Si interrumpe el tratamiento con Drosbelalleflex»).
Consulte a su médico o farmacéutico antes de utilizar cualquier medicamento.
Lactancia
En general, no se recomienda tomar Drosbelalleflex durante el periodo de lactancia. Si usted quiere tomar anticonceptivos mientras está en el periodo de lactancia, debe consultar con su médico.
Consulte a su médico o farmacéutico antes de utilizar cualquier medicamento.
Conducción y uso de máquinas
No hay información que sugiera que el uso de Drosbelalleflex tenga algún efecto sobre la capacidad para conducir o para utilizar máquinas.
Drosbelalleflex contiene lactosa y sodio.
Si su médico le ha indicado que padece una intolerancia a ciertos azúcares, consulte con él antes de tomar este medicamento.
Este medicamento contiene menos de 23 mg de sodio (1mmol) por comprimido; esto es, esencialmente “exento de sodio”.
3. Cómo tomar Drosbelalleflex
Siga exactamente las instrucciones de administración de este medicamento indicadas por su médico. Consulte a su médico o farmacéutico si tiene dudas.
Cada tira contiene 24 comprimidos.
Tome un comprimido de Drosbelalleflex todos los días, con algo de agua si fuera necesario. Puede tomar los comprimidos con o sin alimentos, pero debe tomarlos cada día a la misma hora aproximadamente.
Toma de comprimidos
Fase obligatoria (día1 a día24)
Empiece por el comprimido que tiene marcado el día de la semana de que se trate. Cuando se empieza a tomar Drosbelalleflex, los comprimidos se deben tomar de forma ininterrumpida durante un mínimo de 24 días, tras los cuales puede:
- dejar de tomar comprimidos durante un intervalo de 4 días en el que comenzará su periodo menstrual,
- o continuar tomando los comprimidos hasta un máximo de 120 días (vea la fase flexible), lo que retrasará el inicio de su periodo.
Fase flexible (día25 a día120)
Entre los días 25 y 120, los comprimidos se pueden tomar de forma ininterrumpida durante un máximo de 120 días (momento en el que se habrán terminado todas las tiras incluidas en este envase). Dentro de este periodo, usted puede decidir si desea retrasar su periodo o iniciar el intervalo de 4 días sin comprimidos.
Si usted ha decidido continuar la toma de comprimidos durante 120 días, vaya directamente alos 4 días sin comprimidos, completando los 120 días de toma de comprimidos.
Su periodo comenzará en el intervalo de 4 días sin comprimidos. Normalmente esto ocasionará sangrado.
Si se produce un sangrado continuo (tres días consecutivos) en la fase flexible (días 25-120), es recomendable iniciar un intervalo de 4 días sin comprimidos, lo que inducirá el periodo. Este intervalo de 4 días sin comprimidos reducirá el número total de días con sangrado.
Intervalo sin comprimidos
El intervalo sin comprimidos nunca debe superar los 4 días de duración y solo debe iniciarse si se han estado tomando los comprimidos de forma ininterrumpida durante 24 días.
Durante el intervalo de 4días sin comprimidossuele producirse sangrado y es posible que no haya terminado antes de iniciar el siguiente ciclo de comprimidos.
Después de cada intervalo de 4días sin comprimidosse inicia un nuevo ciclo de toma de una duración mínima de 24 días y un máximo de 120 días. Tras la fase obligatoria de 24 días de toma ininterrumpida de comprimidos, puede decidir iniciar o no un intervalo de 4 días sin comprimidos entre los días 25 y 120.
Se recomienda iniciar una nueva tira, que contiene 24 comprimidos, para cada fase obligatoria y después de un intervalo de 4 días sin comprimidos, para facilitar una correcta administración del producto.
Reglas generales de dosificación:
- Solo puede iniciarse un intervalo de 4 días sin comprimidos si se han estado tomando los comprimidos de forma ininterrumpida durante un mínimo de 24 días, es decir, tras completar la fase obligatoria.
- Después de un intervalo de 4 días sin comprimidos se iniciará una nueva fase obligatoria, por lo que deberán tomarse comprimidos de forma ininterrumpida durante un mínimo de 24 días antes de poder programar una nueva interrupción.
Preparación de las tiras del blíster
Para llevar un control de la toma diaria del anticonceptivo, cada envase de Drosbelalleflex incluye 35 (5x7) tiras adhesivas que llevan impresos los días de la semana,. Usted debe saber el día de la semana en el que va a tomar el primer comprimido.
Escoja la tira de la semana que empieza con el día en que toma el primer comprimido. Por ejemplo, si toma su primer comprimido un miércoles, utilice la tira que empieza con «MIE».
A continuación, tiene que pegar la tira semanal en la parte superior de la tira del blíster, donde se indica «Colocar la etiqueta aquí». Ahora tendrá un día marcado por encima de cada comprimido y podrá comprobar visualmente si ha tomado el comprimido. Las flechas indican el orden de toma de los comprimidos.
Si usa Drosbelalleflex de este modo, también está protegida frente al embarazo durante los 4 días en los que no toma comprimidos.
Si tiene tiras del blíster sin acabar, puede tomar los comprimidos restantes durante la fase flexible. Elija una nueva tira semanal con el día de la semana en el que empieza a tomar los comprimidos restantes y colóquela encima del primer comprimido restante que vaya a tomar. Pegue la nueva tira semanal encima de la tira anterior. Vea Preparación de las tiras del blíster.
El nuevo envase deberá recetarse con suficiente antelación, es decir, antes de usar la última tira del envase para garantizar que usted no agota sus existencias de comprimidos.
Si no está segura de cómo proceder, consulte con su médico.
¿Cuándo puede empezar con la primera tira del blíster?
- Si no ha tomado ningún anticonceptivo hormonal en el mes anterior
Comience a tomar Drosbelalleflex el primer día del ciclo (es decir, el primer día de su menstruación). Si comienza Drosbelalleflex el primer día de su menstruación, está protegida inmediatamente frente a un embarazo. También puede comenzar los días 2–5 del ciclo, pero en ese caso debe utilizar métodos anticonceptivos adicionales (p. ej., un preservativo) durante los 7 primeros días.
- Cambio desde un anticonceptivo hormonal combinado, anillo anticonceptivo combinado vaginal o parche
Puede comenzar a tomar Drosbelalleflex preferentemente el día después de tomar el último comprimido activo (el último comprimido que contiene principios activos) de su anticonceptivo anterior, y como muy tarde el día siguiente de los días sin comprimidos (o después del último comprimido inactivo) de su anticonceptivo anterior. Cuando cambie desde un anillo anticonceptivo combinado vaginal o parche, siga las recomendaciones de su médico.
- Cambio desde un método basado exclusivamente en gestágenos (píldora de solo gestágeno, inyección, implante o sistema intrauterino de liberación (SIL) de gestágenos)
Puede cambiar desde la píldora de solo gestágenos cualquier día. Si se trata de un implante o un SIL, el mismo día de su retirada; si se trata de un inyectable, cuando corresponda la siguiente inyección. En todos los casos es recomendable que utilice medidas anticonceptivas adicionales (p. ej., un preservativo) durante los 7 primeros días de la toma de los comprimidos.
- Después de un aborto
Siga las recomendaciones de su médico.
- Después de tener un niño
Puede comenzar a tomar Drosbelalleflex entre 21 y 28 días después del parto. Si comienza más de 28 días después, debe utilizar uno de los métodos denominados de barrera (p. ej., preservativos) durante los 7 primeros días del uso de Drosbelalleflex.
Si, después de tener un niño, usted ya ha tenido relaciones sexuales, antes de comenzar a tomar Drosbelalleflex, debe estar segura de no estar embarazada o esperar a su siguiente menstruación.
- Si está en periodo de lactancia y quiere empezar a tomarDrosbelalleflex (nuevamente) después de tener un bebé
Lea la sección «Lactancia».
Consulte a su médico si tiene dudas sobre cuando empezar.
Si toma más Drosbelalleflex del que debe
No se han comunicado casos en los que la ingestión de una sobredosis de Drosbelalleflex haya causado daños graves.
Si toma varios comprimidos de una sola vez, puede encontrarse mal o tener vómintos o hemorragia vaginal. Esta hemorragia puede aparecer incluso en chicas que aún no han tenido ele primer periodo menstrual, si accidentalmente han tomado este medicamento.Si usted ha tomado demasiados comprimidos de Drosbelalleflex, o descubre que un niño los ha tomado, consulte con su médico o farmacéutico. También puede llamar al Servicio de Información Toxicológica, teléfono 91 562 04 20, indicando el medicamento y la cantidad tomada.
Si olvidó tomar Drosbelalleflex
Si olvidó un comprimido (uno de los 24 comprimidos de la tira), debe hacer lo siguiente:
- Si han pasado menos de 24 horasdesde que tomó un comprimido, la protección frente al embarazo no disminuye. Tome el comprimido tan pronto como se acuerde y, después, tome los comprimidos siguientes a la hora habitual.
- Si han pasado más de 24 horasdesde que tomó un comprimido, la protección frente al embarazo puede reducirse. Cuanto más comprimidos haya olvidado, mayor es el riesgo de quedarse embarazada.
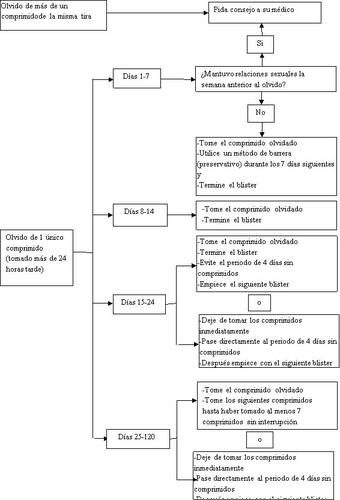
El riesgo de protección incompleta frente al embarazo es máximo si usted olvida tomar un comprimido al principio o al final del blíster. A continuación se enumeran las recomendaciones que debe seguir en esta situación (véase también el diagrama a continuación):
- Olvido de más de un comprimido del blíster
Consulte con su médico.
- Olvido de un comprimido durante los días 1-7
Tome el comprimido que haya olvidado tan pronto como se acuerde, aunque esto signifique tomar dos comprimidos al mismo tiempo. Siga tomando los comprimidos a la hora habitual y utilice precauciones anticonceptivas adicionalesdurante los 7 días siguientes, p. ej., preservativos. Si usted ha mantenido relaciones sexuales en la semana previa al olvido del comprimido debe saber que hay riesgo de embarazo. En ese caso, consulte con su médico.
- Olvido de un comprimido durante los días 8-14
Tome el comprimido que haya olvidado tan pronto como se acuerde, aunque esto signifique tomar dos comprimidos al mismo tiempo. Siga tomando los comprimidos siguientes a la hora habitual. La protección frente al embarazo no disminuye y usted no necesita tomar precauciones adicionales.
- Olvido de un comprimido durante los días 15-24
Puede elegir entre dos posibilidades:
- Tome el comprimido que haya olvidado tan pronto como se acuerde, aunque esto signifique tomar dos comprimidos al mismo tiempo. Siga tomando los comprimidos siguientes a su hora habitual hasta acabar los 24 comprimidos. Evite el intervalo de 4 días sin comprimidos y comience el nuevo blíster (el día de inicio será diferente al anterior).
Probablemente, tendrá la regla al final del segundo blíster (durante el intervalo de 4 días sin comprimidos) aunque puede presentar manchado o hemorragias durante la toma del segundo blíster.
- También puede dejar de tomar los comprimidos y pasar directamente al periodo de 4 días sin comprimidos (antes de iniciar este periodo sin comprimidos, anote el día en que ha olvidado tomar el comprimido).Si quiere empezar un nuevo blíster en el mismo día en que lo hace normalmente, reduzca el intervalo sin comprimidos a menos de 4días.
Si usted sigue una de estas dos recomendaciones, permanecerá protegida frente al embarazo.
- Olvido de un comprimido durante los días 25-120
Puede elegir entre las siguientes opciones, sin necesidad de adoptar precauciones anticonceptivas adicionales.
- Tome el comprimido que haya olvidado tan pronto como se acuerde, aunque esto signifique tomar dos comprimidos al mismo tiempo, y tome los comprimidos siguientes a la hora habitual hasta que haya tomado al menos 7 comprimidos sin interrupción.
- Deje de tomar los comprimidos, inicie un intervalo de 4 días sin comprimidos (contando el día que olvido tomar el comprimido) e inicie posteriormente un nuevo ciclo de toma de Drosbelalleflex.
- Si ha olvidado tomar algún comprimido de una tira y no tiene la regla durante el intervalo de 4 días sin comprimidos, esto puede significar que está embarazada. En este caso, debe acudir a su médico antes de seguir con el siguiente blíster.
Qué debe hacer en caso de vómitos o diarrea intensa
Si tiene vómitos en las 3-4 horas siguientes a la toma de un comprimido o si padece diarrea intensa, hay riesgo de que los principios activos del comprimido no sean absorbidos totalmente por su organismo. Es similar a lo que ocurre cuando usted olvida tomar un comprimido. Tras los vómitos o la diarrea, debe tomar un comprimido de una tira blíster de reserva lo antes posible. Si es posible, tómelo en las 24 horas posteriores a la hora habitual en que toma su anticonceptivo. Si no es posible o han transcurrido más de 24 horas, siga los consejos de la sección «Si olvidó tomar Drosbelalleflex».
Si interrumpe el tratamiento con Drosbelalleflex
Puede dejar de tomar Drosbelalleflex siempre que lo desee. Si no quiere quedarse embarazada, consulte con su médico acerca de otros métodos eficaces de control de la natalidad. Si quiere quedarse embarazada, es aconsejable que deje de tomar Drosbelalleflex y espere hasta su menstruación antes de intentar quedarse embarazada. Así podrá calcular la fecha estimada del parto más fácilmente.
Si tiene cualquier otra duda sobre el uso de este producto, pregunte a su médico o farmacéutico.
4. Posibles efectos adversos
Al igual que todos los medicamentos, Drosbelalleflex puede producir efectos adversos, aunque no todas las personas los sufran.
Si sufre algún efecto adverso, especialmente si es grave y persistente, o siente algún cambio en la salud que considere que puede ser causado por Drosbelalleflex, consulte con su médico.
Las mujeres que toman anticonceptivos hormonales combinados presentan un mayor riesgo de coágulos sanguíneos en las venas (tromboembolia venosa, TEV) o coágulos sanguíneos en las arterias (tromboembolia arterial, TEA). Para obtener información más detallada sobre los distintos riesgos de tomar anticonceptivos hormonales combinados, vea la sección 2 «Qué necesita saber antes de empezar a tomar Drosbelalleflex».
Contacte con un médico inmediatamente si experimenta cualquiera de los siguientes síntomas de angioedema: hinchazón de la cara, lengua y/o garganta y/o dificultad para tragar o urticaria con posible dificultad para respirar (ver también sección “Advertencias y precauciones”)
A continuación se describen los efectos adversos relacionados con el uso de Drosbelalleflex:
- Efectos adversos frecuentes(afectan a entre 1 y 10 usuarios de cada 100):
- cambios en el estado de ánimo
- dolor de cabeza
- náuseas
- dolor de las mamas, problemas con los periodos como periodos irregulares, ausencia de menstruación
- labilidad emocional, depresión, disminución de la libido
- Efectos adversos poco frecuentes(afectan a entre 1 y 10 usuarios de cada 1.000):
- depresión, nerviosismo, somnolencia
- mareo, hormigueo
- migraña, varices, aumento de la tensión arterial
- dolor de estómago, vómitos, indigestión, gases intestinales, inflamación del estómago, diarrea
- acné, picor, erupción cutánea
- molestias y dolores, como dolor de espalda, dolor en las extremidades, calambres musculares
- infección vaginal por hongos, dolor en la región abdominal inferior (pélvica), aumento de tamaño de las mamas, bultos benignos en las mamas, hemorragias uterinas/vaginales (que suelen remitir a lo largo del tratamiento), secreción vaginal, sofocos, inflamación de la vagina (vaginitis), problemas con las reglas, reglas dolorosas, reglas más cortas, reglas abundantes, sequedad vaginal, citología vaginal anormal, pérdida de interés por el sexo
- falta de energía, aumento de la sudoración, retención de líquidos
- aumento de peso
La depresión, la disminución del interés sexual y las migrañas son efectos adversos frecuentes asociados al uso de Drosbelalleflex en una pauta flexible de hasta 120 días.
- Efectos adversos raros(afectan a entre 1 y 10 usuarios de cada 10.000):
- candidiasis (una infección por hongos)
- anemia, aumento del número de plaquetas en la sangre
- reacción alérgica
- trastorno hormonal (endocrino)
- aumento del apetito, pérdida del apetito, concentración de potasio en la sangre anormalmente elevada, concentración de sodio en la sangre anormalmente baja
- ausencia de orgasmo, insomnio
- vértigo, temblores
- trastornos oculares, como inflamación de los párpados, sequedad ocular
- latido cardíaco inusualmente rápido
- inflamación de una vena, sangrado nasal, desvanecimiento
- aumento de tamaño del abdomen, trastorno intestinal, sensación de flatulencia, hernia de estómago, infección de la boca por hongos, estreñimiento, sequedad de boca
- dolor en las vías biliares o la vesícula biliar, inflamación de la vesícula biliar
- manchas pardo-amarillentas en la piel, eccema, pérdida de pelo, inflamación de la piel parecida al acné, sequedad de piel, inflamación de la piel con hinchazones, crecimiento excesivo del pelo, trastornos de la piel, marcas de tensión sobre la piel, inflamación de la piel, inflamación de la piel por fotosensibilidad, nódulos de la piel
- relaciones sexuales difíciles o dolorosas, inflamación de la vagina (vulvovaginitis), hemorragias después de las relaciones sexuales, metrorragia de privación, quiste en las mamas, aumento del número de células mamarias (hiperplasia), bultos malignos en las mamas, crecimiento anormal de la superficie mucosa del cuello del útero, encogimiento o pérdida del recubrimiento del útero, quistes ováricos, aumento de tamaño del útero
- malestar general
- pérdida de peso
- coágulos sanguíneos nocivos en una vena o arteria, por ejemplo:
- en una pierna o pie (es decir, TVP)
- en un pulmón (es decir, EP)
- infarto de miocardio
- accidente cerebrovascular
- mini accidente cerebrovascular o síntomas temporales similares a un accidente cerebrovascular, conocidos como accidente isquémico transitorio (AIT)
- coágulos sanguíneos en el hígado, estómago/intestino, riñones u ojos.
La probabilidad de sufrir un coágulo sanguíneo puede aumentar si padece algún trastorno que aumenta el riesgo (vea la sección 2 para obtener más información sobre los trastornos que aumentan el riesgo de coágulos sanguíneos y los síntomas de un coágulo sanguíneo).
También se han comunicado los siguientes efectos adversos, pero su frecuencia no puede estimarse a partir de los datos disponibles: hipersensibilidad, eritema multiforme (erupción cutánea con enrojecimiento y llagas en forma de escarapela).
Comunicación de efectos adversos:
Si experimenta cualquier tipo de efecto adverso, consulte a su médico o farmacéutico, incluso si se trata de posibles efectos adversos que no aparecen en este prospecto. También puede comunicarlos directamente a través del Sistema Español de Farmacovigilancia de Medicamentos de Uso Humano website: www.notificaram.es. Mediante la comunicación de efectos adversos usted puede contribuir a proporcionar más información sobre la seguridad de este medicamento.
5. Conservación de Drosbelalleflex
Mantener este medicamento fuera de la vista y del alcance de los niños.
Conservar por debajo de 30°C.
No utilice este medicamento después de la fecha de caducidad que aparece en la tira y en el estuche de cartón después de «CAD». La fecha de caducidad es el último día del mes que se indica.
Los medicamentos no se deben tirar por los desagües ni a la basura.
Deposite los envases y los medicamentos que no necesita en el Punto SIGRE de la farmacia. En caso de duda pregunte a su farmacéutico cómo deshacerse de los envases y de los medicamentos que no necesita. De esta forma ayudará a proteger el medio ambiente.
6. Contenido del envase e información adicional
Composición de Drosbelalleflex
- Los principios activos son drospirenona y etinilestradiol. Cada comprimido recubierto con película contiene 3 miligramos de drospirenona y 0,02 miligramos de etinilestradiol.
- Los demás componentes son: lactosa monohidrato, almidón de maíz pregelatinizado, povidona (E1201), croscarmelosa sódica, polisorbato 80, estearato de magnesio (E572), alcohol de polivinilo, dióxido de titanio (E171), macrogol, talco (E553b), óxido de hierro amarillo (E172), óxido de hierro rojo (E172) y óxido de hierro negro (E172).
Aspecto del producto y contenido del envase
- Cada tira de Drosbelalleflex contiene 24 comprimidos recubiertos con película
- Drosbelallelflex está disponible en cajas de 5 tiras blíster; cada caja contiene 120 comprimidos en total.
- Cada envase de Drosbelalleflex incluye 35 (5 × 7) pegatinas adhesivas con los días de la semana impresos.
Titular de la autorización de comercialización
Exeltis Healthcare S.L
Avda. de Miralcampo 7.
Polígono Industrial Miralcampo.
19200 Azuqueca de Henares. (Guadalajara)
España
Responsable de la fabricación
Laboratorios León Farma, S.A.
C/ La Vallina, s/n,
Polígono Industrial Navatejera,
Villaquilambre 24193 (León),
España
Este medicamento está autorizado en los estados miembros del Espacio Económico Europeo con los siguientes nombres:
Holanda: Talia 0.02 mg/3 mg filmomhulde tabletten
Alemania: Drosbelalleflex Langzyklus 0.02 mg/3 mg filmtabletten
Austria: Drosbelalleflex Langzyklus 0.02 mg/3 mg filmtabletten
Belgica: Pernyella 0,02 mg/3 mg comprimé pelliculé
Estonia: Talia
España Drosbelalleflex 0.02 mg/3 mg comprimidos recubiertos con película
Finlandia: Diza 0,02 mg/3 mg kalvopäällysteiset tabletit
Francia: Pernyella 0,02 mg/3 mg comprimé pelliculé
Italia: Perliq
Hungría: Jangee flexibilis 3 mg/0,02 mg
Letonia: Talia 0,02 mg/3 mg apvalkotas tabletes
Luxemburgo: Pernyella 0,02 mg/3 mg comprimé pelliculé
Polonia: Naraya Flex
Portugal: Drosbelalleflex 0,02 mg/3 mg comprimido revestido
Suecia: Diza
Fecha de la última revisión de este prospecto: noviembre 2024
La información detallada y actualizada de este medicamento está disponible en la página web de la Agencia Española de Medicamentos y Productos Sanitarios (AEMPS) http://www.aemps.gob.es
- País de registro
- Principio activo
- Requiere recetaSí
- Fabricante
- Esta información es de carácter general y no sustituye la consulta con un profesional sanitario.
- Alternativas a DROSBELALLEFLEX 3 MG/0,02 MG COMPRIMIDOS RECUBIERTOS CON PELICULAForma farmacéutica: COMPRIMIDO, 3 mg/0,03 mgPrincipio activo: drospirenone and ethinylestradiolFabricante: Laboratorios Cinfa S.A.Requiere recetaForma farmacéutica: COMPRIMIDO, 3 mg/0,03 mgPrincipio activo: drospirenone and ethinylestradiolFabricante: Laboratorios Cinfa S.A.Requiere recetaForma farmacéutica: COMPRIMIDO, 3 mg/0,02 mgPrincipio activo: drospirenone and ethinylestradiolFabricante: Laboratorios Cinfa S.A.Requiere receta
Médicos online para DROSBELALLEFLEX 3 MG/0,02 MG COMPRIMIDOS RECUBIERTOS CON PELICULA
Comenta la dosis, los posibles efectos secundarios, interacciones, contraindicaciones o la revisión de receta de DROSBELALLEFLEX 3 MG/0,02 MG COMPRIMIDOS RECUBIERTOS CON PELICULA, sujeto a valoración médica y a la normativa local.
Preguntas frecuentes






