
IOMERON 250 MG IODO/ML SOLUCIÓN INYECTABLE

Cómo usar IOMERON 250 MG IODO/ML SOLUCIÓN INYECTABLE
Traducción generada por IA
Este contenido ha sido traducido automáticamente y se ofrece solo con fines informativos. No sustituye la consulta con un profesional sanitario.
Ver originalContenido del prospecto
- Introducción
- Qué es Iomeron 250 mg Iodo/ml solución inyectable y para qué se utiliza
- Qué necesita saber antes de empezar a usar Iomeron 250 mg Iodo/ml solución inyectable
- Cómo usar Iomeron 250 mg Iodo/ml solución inyectable
- Posibles efectos adversos
- Conservación de Iomeron 250 mg Iodo/ml solución inyectable
- Contenido del envase e información adicional
Introducción
PROSPECTO: INFORMACIÓN PARA EL USUARIO
Iomeron250 mg Iodo/ml solución inyectable
Iomeprol
Lea todo el prospecto detenidamente antes de empezar a usar este medicamento, porque contiene información importante para usted.
- Conserve este prospecto, ya que puede tener que volver a leerlo.
- Si tiene alguna duda, consulte a su médico o farmacéutico.
- Este medicamento se le ha recetado solamente a usted y no debe dárselo a otras personas, aunque tengan los mismos síntomas que usted, ya que puede perjudicarles.
- Si experimenta efectos adversos, consulte a su médico, incluso si se trata de efectos adversos que no aparecen en este prospecto. Ver sección 4.
Contenido del prospecto:
- Qué es Iomeron 250 mg Iodo/ml solución inyectable y para qué se utiliza
- Qué necesita saber antes de empezar a usar Iomeron 250 mg Iodo/ml solución inyectable
- Cómo usar Iomeron 250 mg Iodo/ml solución inyectable
- Posibles efectos adversos
- Conservación de Iomeron 250 mg Iodo/ml solución inyectable
- Contenido del envase e información adicional
1. Qué es Iomeron 250 mg Iodo/ml solución inyectable y para qué se utiliza
Este medicamento es únicamente para uso diagnóstico.
Iomeron pertenece al grupo de medicamentos denominados medios de contraste para rayos X de baja osmolaridad, hidrosolubles y nefrotópicos.
Iomeron se utiliza para mejorar la visualización de diferentes zonas corporales mediante determinadas técnicas radiológicas. En adultos se usa para urografía intravenosa, tomografía computarizada (TC) de cabeza y cuerpo, flebografía periférica, flebografía por sustracción digital, arteriografía por sustracción digital y mielografía. En niños de 0 a 18 años para urografía intravenosa, tomografía computarizada (TC) de cabeza y cuerpo, flebografía por sustracción digital y arteriografía periférica.
2. Qué necesita saber antes de empezar a usar Iomeron 250 mg Iodo/ml solución inyectable
No use Iomeron 250 mg Iodo/ml solución inyectable
- Si es alérgico al iomeprol o a cualquiera de los demás componentes de este medicamento (incluidos en la sección 6).
- Si padece paraproteinemia de Waldeström.
- Si padece trastornos hepáticos o renales graves.
- Si padece mieloma múltiple.
Las investigaciones de genitales femeninos están contraindicadas en caso de sospecha de embarazo o embarazo confirmado y en caso de inflamación aguda.
La repetición inmediata de la administración de Iomeron si se produce un fallo en la técnica está contraindicada en mielografía.
Advertencias y precauciones
- Antes de iniciar el examen deberá estar adecuadamente hidratado, y deberá abstenerse de ingerir alimentos en las dos horas anteriores al examen.
- En estados de ansiedad y dolor, ya que pueden intensificarse las reacciones adversas relacionadas con el medio de contraste. En estos casos se puede administrar un sedante.
- Si se utiliza en ancianos.
- Si padece asma.
- Si alguna vez ha desarrollado una erupción cutánea grave o descamación de la piel, ampollas y/o llagas en la boca después de haber recibido medios de contraste iodados.
- Si padece fiebre del heno, urticaria o alergias alimentarias, ya que los pacientes con antecedentes de alergia son más susceptibles a sufrir reacciones adversas a los medios de contraste iodados.
- Si sufre hipertiroidismo y/o bocio nodular, ya que el uso de medios de contraste no iónicos puede desencadenar crisis tiroideas.
- Si sufre insuficiencia renal.
- Si padece diabetes mellitus; estos pacientes pueden desarrollar acidosis láctica si están en tratamiento con biguanidas (p.ej. Metformina). Como precaución, en pacientes con insuficiencia renal moderada las biguanidas deberán suspenderse en el momento o 48 horas antes del examen con un medio de contraste y reestablecerse sólo después de haber controlado que la función renal se ha recuperado.
- Si padece feocromocitoma (un tipo de tumor), ya que pueden aparecer crisis hipertensivas después de utilizar el medio de contraste por vía intravascular. Se recomienda la premedicación con bloqueantes alfa adrenérgicos.
- Si padece anemia falciforme (un tipo de anemia), ya que los medios de contraste pueden agravar su enfermedad.
- Si padece miastenia gravis (enfermedad que produce debilidad en los músculos), porque su enfermedad podría empeorar.
- En caso de enfermedad cardiovascular grave, especialmente si sufre insuficiencia cardiaca, arteriopatías coronarias (enfermedad de los vasos sanguíneos del corazón), hipertensión pulmonar y valvulopatías coronarias.
- Cuando padezca alteraciones del Sistema Nervioso Central, ya que pueden aparecer crisis convulsivas.
- En caso de alcoholismo y drogadicción.
Se recomienda realizar una fluoroscopia para minimizar la extravasación durante la inyección.
Podría experimentar un trastorno cerebral a corto plazo, llamado encefalopatía, durante o poco después del procedimiento de obtención de imágenes. Informe a su médico de inmediato si nota cualquiera de los síntomas relacionados con esta afección, descrita en la sección 4.
Se han observado trastornos tiroideos tras la administración de Iomeron tanto en niños como en adultos. Los lactantes también pueden estar expuestos a través de la madre durante el embarazo. Su médico podría necesitar realizar pruebas de la función tiroidea antes y/o después de la administración de Iomeron.
Se han notificado reacciones cutáneas graves incluyendo síndrome de Stevens-Johnson (SSJ), necrólisis epidérmica tóxica (NET), pustulosis exantemática generalizada aguda (PEGA), y reacción a fármaco con eosinofilia y síntomas sistémicos (DRESS) asociadas al uso de Iomeron. Acuda inmediatamente al médico si observa alguno de los síntomas relacionados con estas reacciones cutáneas graves descritas en la sección 4.
Consulte a su médico antes de empezar a usar Iomeron 250 mg Iodo/ml solución inyectable.
Niños
Los niños de edad inferior a un año y sobre todo los neonatos son particularmente susceptibles a desequilibrios electrolíticos y a alteraciones hemodinámicas.
Otros medicamentos e Iomeron 250 mg Iodo/ml solución inyectable
Informe a su médico si está utilizando, ha utilizado recientemente o pudiera tener que utilizar cualquier otro medicamento.
No se debe interrumpir el tratamiento con fármacos anticonvulsivos y se debe asegurar su administración en dosis óptimas.
En pacientes tratados con medicamentos inmunomoduladores, como la Interleucina-2, son más frecuentes las reacciones de tipo alérgico a medios de contraste y pueden manifestarse como reacciones tardías.
Este medicamento no debe mezclarse con otros.
Interferencias con pruebas analíticas:
Los medios de contraste iodados pueden interferir con los estudios de la función tiroidea, ya que la capacidad del tiroides de captar radioisótopos se verá reducida durante períodos de dos semanas o más.
Altas concentraciones de medios de contraste en plasma y en orina pueden alterar los resultados de las pruebas de laboratorio de bilirrubina, proteínas y sustancias inorgánicas (por ej. hierro, cobre, calcio, fosfato).
Uso de Iomeron250 mg Iodo/ml solución inyectable con los alimentos y bebidas
Si no existen instrucciones específicas del médico, se puede seguir una dieta normal el día del examen. Confirmar una adecuada ingestión de líquidos. Sin embargo, deberá abstenerse de ingerir alimentos en las dos horas anteriores al examen.
Embarazo y lactancia
Si está embarazada o en periodo de lactancia, cree que podría estar embarazada o tiene intención de quedarse embarazada, consulte a su médico antes de utilizar este medicamento.
Embarazo
Debe informar a su médico si está embarazada o cree que pudiera estarlo.
Al igual que para otros medios de contraste no iónicos, no existen estudios controlados en mujeres embarazadas que confirmen la inocuidad del producto en el humano. Ya que, siempre que sea posible, se debe evitar la exposición a radiaciones durante el embarazo, debería evaluarse cuidadosamente la relación riesgo/beneficio de cualquier examen con rayos X, con o sin medios de contraste.
Si está embarazada, y ha recibido Iomeron durante el embarazo, se recomienda analizar la función tiroidea de su recién nacido.
Lactancia
Los medios de contraste son escasamente excretados por leche materna, siendo remota la posibilidad de que el lactante sufra algún daño.
Conducción y uso de máquinas
No se conocen efectos sobre la capacidad para conducir y utilizar máquinas.
3. Cómo usar Iomeron 250 mg Iodo/ml solución inyectable
Este medicamento siempre será administrado por personal cualificado y debidamente formado, en hospitales o clínicas que dispongan del personal y equipos necesarios.
La dosis que se le administrará variará dependiendo del tipo de exploración, edad, peso corporal, gasto cardiaco y estado general que usted presente, así como de la técnica utilizada.
Si usa más Iomeron 250 mg Iodo/ml solución inyectable del que debe
La sobredosificación puede causar graves reacciones adversas, principalmente a través de los efectos sobre el sistema cardiovascular y pulmonar.
El tratamiento de una sobredosis está orientado al mantenimiento de todas las funciones vitales y prevé la rápida instauración de terapia sintomática. Iomeron puede ser eliminado del cuerpo mediante diálisis.
En caso de sobredosis o ingestión accidental, consulte a su médico o farmacéutico o llame al Servicio de Información Toxicológica, teléfono 91 562 04 20, indicando el medicamento y la cantidad ingerida.
Si tiene dudas en el uso de este producto, consulte con su médico o farmacéutico.
4. Posibles efectos adversos
Al igual que todos los medicamentos, este medicamento puede producir efectos adversos, aunque no todas las personas los sufran.
Generalmente, los efectos adversos van de leves a moderados y son de naturaleza transitoria. Sin embargo, se han notificado reacciones graves y potencialmente mortales, a veces con resultado de muerte. En la mayoría de los casos, las reacciones surgen en los minutos siguientes a la administración, aunque a veces pueden aparecer más tarde.
Informe inmediatamente a su médico si sufre alguno de los siguientes síntomas: respiración sibilante repentina, dificultad respiratoria, inflamación de los párpados, cara o labios, erupción cutánea o picor que afecta a todo el cuerpo.
Se han notificado los siguientes efectos adversos:
Administración intravascular
Frecuentes(puede afectar hasta 1 de cada 10 personas):
- sensación de calor
Poco frecuentes(puede afectar hasta 1 de cada 100 personas):
- dolor de cabeza
- mareos
- aumento de la presión sanguínea
- dificultad para respirar
- náuseas, vómitos
- rubor, urticaria, picor
- dolor en el pecho, calor y dolor en el lugar de inyección
Raras(puede afectar hasta 1 de cada 1000 personas)
- desmayos
- ritmo cardiaco lento o rápido
- disminución de la presión sanguínea
- erupción cutánea
- dolor de espalda
- astenia, rigidez, fiebre
- aumento de creatinina en sangre
Frecuencia no conocida(no puede estimarse a partir de los datos disponibles):
- Póngase en contacto con un médico cuanto antes si experimenta una reacción cutánea grave, como:
- ampollas, descamación de la piel, úlceras en la boca, garganta, nariz, genitales y ojos. Estas graves erupciones cutáneas pueden ir precedidas de fiebre y síntomas similares a los de la gripe (síndrome de Stevens-Johnson, necrólisis epidérmica tóxica).
- una erupción roja y escamosa con bultos bajo la piel y ampollas acompañada de fiebre. Los síntomas suelen aparecer al inicio del tratamiento (pustulosis exantemática generalizada aguda).
- una erupción generalizada, temperatura corporal elevada y aumento de los ganglios linfáticos (síndrome DRESS o síndrome de hipersensibilidad al fármaco)
- ansiedad, síndrome hipercinético (aumento de la actividad motora), confusión
- reacciones alérgicas
- hipertiroidismo
- pérdida de apetito (anorexia)
- alteración del gusto, dificultad para hablar, enfermedad que afecta al funcionamiento del cerebro, edema cerebral (líquido en el cerebro), problemas transitorios en el aporte de sangre al cerebro con pocas o ninguna secuela (accidentes isquémicos transitorios), pérdida de memoria, somnolencia, sensibilidad alterada (hormigueo, picor) apoplejía, pérdida de consciencia, temblores, coma, convulsiones, alteración del sentido del olfato
- trastorno cerebral (encefalopatía) con síntomas que incluyen dolor de cabeza, dificultades de visión, pérdida de visión, confusión, convulsiones, pérdida de coordinación, pérdida de movimiento en una parte del cuerpo, problemas en el habla y pérdida de conciencia
- ceguera temporal, deterioro de la vista, conjuntivitis, aumento del lagrimeo, fotopsia (visión de luces)
- infarto de miocardio, paro cardiaco, opresión en el pecho, trastornos del ritmo cardiaco, angina de pecho, insuficiencia cardiaca, formación de coágulos en las arterias coronarias (después de la inserción de un catéter), latido irregular del corazón, trastornos de la conducción cardiaca, pulso rápido y débil
- enrojecimiento, shock (fuerte caída de la presión sanguínea), palidez, cansancio, piel fría y húmeda, consciencia reducida) causado por la dilatación repentina y grave de los vasos sanguíneos, coloración azul de la piel y mucosas, coágulos, vasoespasmo y, como consecuencia, isquemia.
- insuficiencia circulatoria (colapso circulatorio)
- obstrucción de la arteria coronaria (después de la inserción de un catéter)
- parada respiratoria, tos, síndrome de dificultad respiratoria aguda (SDRA), respiración sibilante, ataques de asma, acumulación de líquido en la garganta, líquido en los pulmones, inflamación de la mucosa nasal que se caracteriza por tener la nariz obstruida, estornudos y descarga (rinitis), ronquera (disfonía), aporte insuficiente de oxígeno a los tejidos (hipoxia), dolor de garganta y laringe, constricción repentina de las vías respiratorias (broncoespasmo)
- incontinencia intestinal, diarrea, dolor abdominal, exceso de salivación, dificultad para tragar, inflamación del páncreas junto con un fuerte dolor en la parte superior del abdomen que se irradia hacia la espalda con náuseas y vómitos (pancreatitis), agrandamiento de las glándulas salivares, obstrucción intestinal
- reacciones de hipersensibilidad grave, caracterizadas por síntomas como el aumento de la producción de sudor, mareos, picor, dolor de cabeza pulsátil, opresión en la garganta, inflamación de la mucosa de la boca y la garganta, que dificultan la respiración
- eccema, erupción cutánea, aumento de la producción de sudor, acumulación repentina de líquido en piel y mucosas (por ejemplo la garganta o la lengua), posiblemente con dificultad para respirar y/o picor y erupción cutánea (angioedema), aparición de ampollas circulares en la piel (cuyo centro suele ser de un color más pálido) (eritema multiforme)
- dolor en las articulaciones, rigidez muscular
- fallo renal agudo, incontinencia urinaria, anomalías en la orina, disminución de la producción de orina
- sensación generalizada de enfermedad (malestar general), escalofríos, sensación de frío localizado, sed, reacción en el lugar de inyección, hematoma en el lugar de inyección
- trastornos sanguíneos (disminución del número de plaquetas) acompañado de hematomas y propensión a sangrar (trombocitopenia)
- anemia hemolítica (disminución anormal de los glóbulos rojos que puede causar fatiga, frecuencia cardiaca rápida y dificultad respiratoria)
Puede producirse hipotiroidismo transitorio en niños menores de 3 años.
En algunos casos, las alteraciones se detectan durante las exploraciones médicas (valores sanguíneos, pruebas de la función cardiaca y hepática).
Administración en el líquido cefalorraquídeo
Muy frecuentes(más de 1 de cada 10 personas):
- dolor de cabeza
Frecuentes(más de 1 de cada 100 personas y menos de 1 de cada 10 personas):
- mareos
- aumento de la presión sanguínea
- náuseas, vómitos
- dolor de espalda, dolor en las extremidades
- reacción en el lugar de inyección
Poco frecuentes(más de 1 de cada 1.000 personas y menos de 1 de cada 100 personas):
- pérdida de consciencia
- sensibilidad alterada
- somnolencia
- disminución de la presión sanguínea
- enrojecimiento
- rigidez muscular
- dolor de cuello
- sensación de calor
- dolor en el pecho
- fiebre
Frecuencia no conocida(no puede estimarse a partir de los datos disponibles):
- reacciones alérgicas
- epilepsia
- erupción cutánea
- malestar general
- trastorno cerebral (encefalopatía) con síntomas que incluyen dolor de cabeza, dificultades de visión, pérdida de visión, confusión, convulsiones, pérdida de coordinación, pérdida de movimiento en una parte del cuerpo, problemas en el habla y pérdida de conciencia
Consulte a su médico si experimenta síntomas graves o reacciones alérgicas (hipersensibilidad), o si los síntomas persisten durante periodos largos de tiempo.
El perfil de seguridad de iomeprol es similar en adultos y niños para todas las vías de administración.
Comunicación de efectos adversos
Si experimenta cualquier tipo de efecto adverso, consulte a su médico, incluso si se trata de posibles efectos adversos que no aparecen en este prospecto. También puede comunicarlos directamente a través del Sistema Español de Farmacovigilancia de Medicamentos de Uso Humano http://www.notificaRam.es. Mediante la comunicación de efectos adversos usted puede contribuir a proporcionar más información sobre la seguridad de este medicamento.
5. Conservación de Iomeron 250 mg Iodo/ml solución inyectable
Mantener este medicamento fuera de la vista y del alcance de los niños.
Conservar el frasco en el embalaje exterior para protegerlo de la luz.
Aunque la sensibilidad de iomeprol a los rayos X es baja, es aconsejable guardar el producto fuera del alcance de radiaciones ionizantes.
No utilice este medicamento después de la fecha de caducidad que aparece en el envase después de CAD. La fecha de caducidad es el último día del mes que se indica.
Los medicamentos no se deben tirar por los desagües ni a la basura. En caso de duda, pregunte a su farmacéutico cómo deshacerse de los envases y de los medicamentos que no necesita. De esta forma ayudará a proteger el medio ambiente.
6. Contenido del envase e información adicional
Composición de Iomeron 250 mg Iodo/ml solución inyectable
- El principio activo es iomeprol. 1 ml de solución inyectable contiene 510,3 mg de iomeprol, equivalentes a 250 mg de iodo.
- Los demás componentes son trometamol, ácido clorhídrico para ajustar el pH y agua para preparaciones inyectables c.s.p.
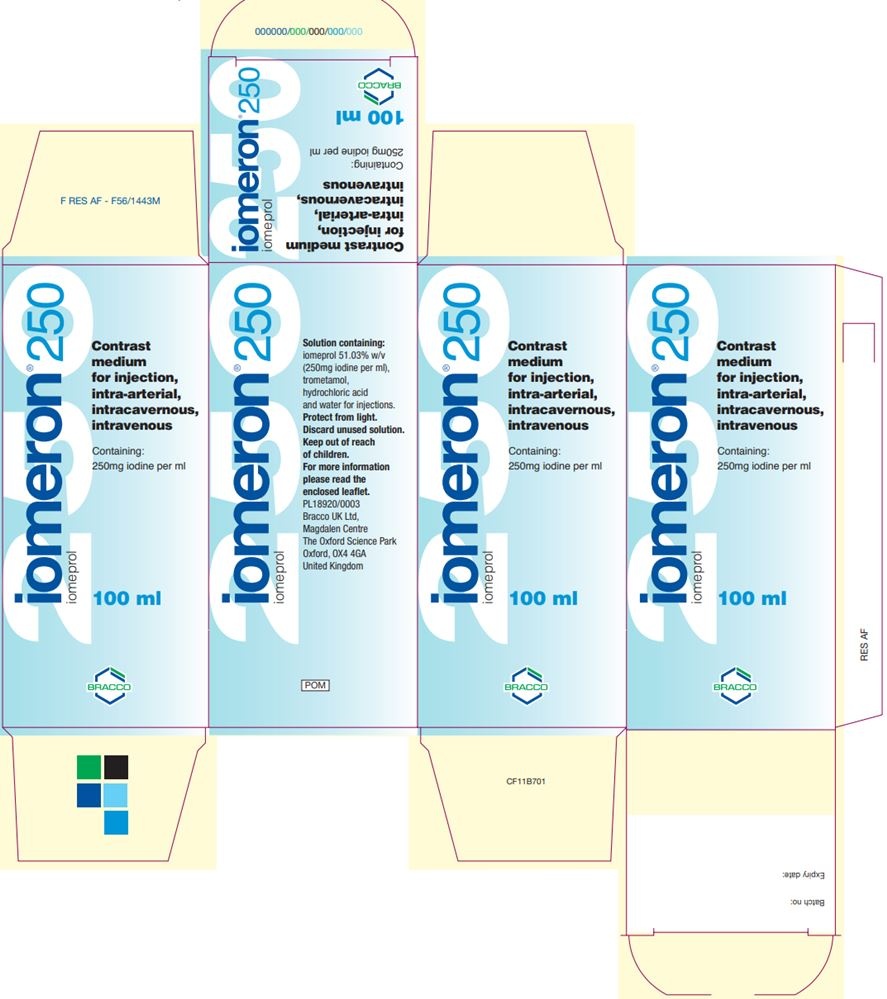
Aspecto del producto y contenido del envase
Iomeron se envasa en frascos de vidrio cerrados con tapones de halobutilo y una cápsula de aluminio.
Frascos monodosis de 50 ml, 100 ml y 200 ml.
Puede que solamente estén comercializados algunos tamaños de envases.
Titular de la autorización de comercialización y responsable de la fabricación
Titular de la autorización de comercialización
Bracco Imaging s.p.a.
Via E. Folli 50
20134 (Milán – Italia)
Responsable de la fabricación
Patheon Italia s.p.a.
2º Trav. SX Vía Morolense, 5
03013 Ferentino (Italia)
BIPSO GmbH
Robert-Gerwig-Strasse 4
78224 Singen (Alemania)
Bracco Imaging S.p.A.
Bioindustry Park - Via Ribes, 5
10010 Colleretto Giacosa (TO) (Italia)
Puede solicitar más información respecto a este medicamento dirigiéndose al representante local del titular de la autorización de comercialización:
Laboratorios Farmacéuticos ROVI, S.A.
Julián Camarillo, 35
28037 Madrid
Tel: 913756230
Fecha de la última revisión de este prospecto:septiembre 2023
La información detallada y actualizada de este medicamento está disponible en la página web de la Agencia Española de Medicamentos y Productos Sanitarios (AEMPS) http://www.aemps.gob.es/
<-------------------------------------------------------------------------------------------------------------->
Esta información está destinada únicamente a profesionales del sector sanitario:
Iomeron 250 mg Iodo/ml es una solución inyectable para administración por vía intravenosa, intraarterial e intratecal.
Siempre que sea posible, la administración intravascular de los medios de contraste debería hacerse con el paciente acostado. Mantener al paciente bajo observación al menos durante 30 minutos después de la administración.
Indicación | Vía de administración | Dosificaciones propuestas | |
Urografía intravenosa | Intravenosa | Adultos:50 - 150 ml Neonatos:3 - 4,8 ml Niños: < 1 año: 2,5 - 4 ml/kg > 1 año: 1 - 2,5 ml/kg | |
Tomografía computarizada de cabeza | Intravenosa | Adultos:50 - 200 ml Niñosa | |
Tomografía computarizada de cuerpo | Intravenosa | Adultos:100 - 200 ml Niñosa | |
Angiografía convencional | |||
Flebografía periférica | Intravenosa | Adultos:10 - 100 ml, repetir si es necesariob (10 - 50 ml extremidades superiores; 50 - 100 ml extremidades inferiores) | |
Arteriografía por sustracción digital | |||
Abdomen | Intraarterial | Adultosc | |
Arteriografía periférica | Intraarterial | Adultos:5 - 10 ml para inyecciones selectivas, hasta 250 ml Niñosa | |
Flebografía por sustracción digital | Intravenosa | Adultos:100 - 250 mlb Niñosa | |
Mielografía | Intratecal | Adultos:10 - 18 ml | |
a Según el peso corporal y la edad, y queda establecida por el médico responsable de la prueba. b No superar los 250 ml. El volumen de cada inyección única depende del área vascular a examinar. c No superar los 350 ml. |
Antes de usar, la solución debe ser inspeccionada visualmente. Sólo se usarán las soluciones sin signos visibles de deterioro o partículas.
La eliminación del medicamento no utilizado y de todos los materiales que hayan estado en contacto con él, se realizará de acuerdo con la normativa local.
Precauciones
- Respecto al paciente:
Hidratación- Se debe corregir cualquier alteración grave del equilibrio hidroelectrolítico. Antes del examen médico asegurar una hidratación adecuada, sobre todo en pacientes con deterioro grave funcional de los riñones, mieloma múltiple u otras paraproteinemias, anemia de células falciformes, diabetes mellitus, poliuria, oliguria, hiperuricemia, así como también en neonatos, niños y pacientes de edad avanzada.
Sugerencias dietéticas- Si no existen particulares instrucciones específicas del médico, se puede seguir una dieta normal. Confirmar una adecuada ingestión de líquidos. Sin embargo, el paciente deberá abstenerse de ingerir alimentos en las dos horas anteriores al examen.
Hipersensibilidad- En pacientes con predisposición a las alergias, con hipersensibilidad conocida a los medios de contraste iodados y con historia de asma, se puede considerar la premedicación con antihistamínicos y/o con corticoides con el fin de prevenir posibles reacciones anafilactoides.
Reacciones adversas cutáneas graves- Se han notificado reacciones adversas cutáneas graves (RACG), incluyendo síndrome de Stevens-Johnson (SSJ), necrólisis epidérmica tóxica (NET), pustulosis exantemática generalizada aguda (PEGA), y reacción a fármaco con eosinofilia y síntomas sistémicos (DRESS), que pueden llegar a ser mortales o potencialmente mortales, en pacientes a los que se les administraron medios de contraste iodados por vía intravascular. En el momento de la administración, se debe advertir a los pacientes de los signos y síntomas, y vigilar atentamente la aparición de reacciones cutáneas. Si aparecen signos y síntomas que sugieran la aparición de estas reacciones, se debe suspender la administración de Iomeron inmediatamente. Si el paciente ha desarrollado una reacción grave como SSJ, NET, PEGA o DRESS con el uso de Iomeron, no se debe volver a administrar Iomeron a ese paciente en ningún momento.
Ansiedad- Estados de excitación, ansiedad y dolor pueden ser causa de efectos secundarios o pueden intensificar las reacciones relacionadas con el medio de contraste. En estos casos se puede administrar un sedante.
Tratamientos concomitantes- Considerar la interrupción del tratamiento con fármacos que reduzcan el umbral convulsivo hasta 24 horas después de la intervención, en caso de uso intratecal, y en pacientes con trastornos de la barrera hematoencefálica (ver “Síntomas neurológicos”).
- Respecto al procedimiento:
Coagulación, cateterismo- Una propiedad de los medios de contraste no iónicos es la escasa interferencia con las funciones fisiológicas. Como consecuencia, los medios de contraste no iónicos tienen, in vitro, una actividad anticoagulante menor que la de los medios de contraste iónicos. El personal médico y paramédico que realice el cateterismo vascular debe estar informado de esto y debe prestar particular atención a la técnica angiográfica. Los medios de contraste no iónicos no deben entrar en contacto con la sangre en la jeringa y se deben limpiar con frecuencia los catéteres intravasculares para minimizar el riesgo de tromboembolias relacionadas con el procedimiento.
Observación del paciente- Siempre que sea posible, la administración intravascular de los medios de contraste debería hacerse con el paciente acostado. Mantener al paciente bajo observación al menos durante 30 minutos después de la administración.
Prueba de sensibilidad- Una prueba de sensibilidad es prácticamente inútil, ya que la aparición de reacciones graves o fatales debidas a medios de contraste no se pueden predecir con dicha prueba.
Riesgo de inflamación yextravasación- Se recomienda tener precaución durante la inyección de medios de contraste para evitar la extravasación.
Advertencias
- Común para todas las formas de administración
Considerando los posibles efectos secundarios graves, el uso de los medios de contraste con iodo orgánico debería limitarse a necesidades concretas de exploraciones contrastográficas.
Dicha necesidad deberá considerarse según las condiciones clínicas del paciente, sobre todo en relación con patologías del sistema cardiovascular, urinario y hepatobiliar.
Los medios de contraste para exploraciones angiocardiográficas deben ser utilizados en hospitales o en clínicas que cuenten con el personal competente y con el equipo necesario para los debidos cuidados intensivos en caso de emergencia. En los centros donde se realizan otros exámenes diagnósticos más comunes que requieran el uso de medios de contraste iodados, es necesario que los servicios de radiología donde se practiquen estos exámenes cuenten con las medidas terapéuticas y con los equipos de reanimación que la experiencia ha confirmado idóneos (balón Ambu, oxígeno, antihistamínicos, vasoconstrictores, etc.).
Uso en:
Población pediátrica- Los niños de edad inferior a un año y sobre todo los neonatos son particularmente susceptibles a desequilibrios electrolíticos y a alteraciones hemodinámicas. Es necesario prestar atención a las dosis a usar, a la técnica del procedimiento y al estado del paciente. Puede observarse hipotiroidismo o supresión transitoria de la tiroides tras la exposición a medios de contraste iodados. Se debe prestar especial atención a los pacientes pediátricos menores de 3 años ya que un episodio de baja actividad tiroidea durante los primeros años de vida puede ser perjudicial para el desarrollo motor, auditivo y cognitivo y puede requerir tratamiento sustitutivo temporal con T4. La incidencia de hipotiroidismo en pacientes menores de 3 años expuestos a medios de contraste iodados se ha notificado entre el 1,3% y el 15%, dependiendo de la edad de los sujetos y de la dosis del medio de contraste iodado, observándose con mayor frecuencia en neonatos y prematuros. Debe evaluarse la función tiroidea en todos los pacientes pediátricos menores de 3 años después de la exposición a medios de contraste iodados. Si se detecta hipotiroidismo, se debe considerar la necesidad de tratamiento y se debe vigilar la función tiroidea hasta que se normalice.
Ancianos- Los pacientes de edad avanzada se deben considerar de riesgo especial a reacciones debidas a una dosificación demasiado elevada del medio de contraste. La frecuente asociación de trastornos neurológicos y patologías vasculares constituye un factor agravante.
Pacientes con particulares condiciones patológicas
- Hipersensibilidad a medios de contraste iodados- La hipersensibilidad o reacciones precedentes a medios de contraste iodados aumentan también el riesgo de recurrencia de una reacción grave, incluso con medios de contraste no iónicos.
- Predisposición alérgica- Se sabe que reacciones adversas a medios de contraste iodados son más comunes en pacientes que tienen antecedentes de alergia: fiebre del heno, urticaria y alergias alimenticias.
- Pacientes asmáticos- Los pacientes que toman bloqueantes beta-adrenérgicos, en particular los pacientes asmáticos, pueden tener un umbral más bajo para broncoespasmo y una menor respuesta al tratamiento con beta-agonistas y adrenalina, lo que puede requerir el uso de dosis más altas.
- Función tiroidea y pruebas de función tiroidea- En los medios de contraste pueden estar presentes pequeñas cantidades de ioduro inorgánico libre que podrían tener efectos sobre la función tiroidea. Estos efectos son más evidentes en pacientes con hipertiroidismo latente o manifiesto, o bocio. Se ha notificado hipertiroidismo, o incluso, crisis tiroideas tras la administración de medios de contrastes iodados.
- Administración intraarterial e intravenosa
Uso en pacientes con especiales condiciones patológicas
Deterioro renal- En los pacientes con función renal comprometida, la administración de medios de contraste puede provocar episodios de insuficiencia renal. Las medidas de prevención incluyen: la identificación de pacientes de alto riesgo; garantizar una adecuada hidratación antes de la administración del medio de contraste, preferiblemente manteniendo la infusión intravenosa antes, durante el procedimiento y hasta que el medio de contraste haya sido eliminado por los riñones; evitar, si es posible, la administración de fármacos nefrotóxicos y someter al paciente a intervenciones quirúrgicas importantes o a procedimientos como la angioplastia renal, hasta que el medio de contraste haya sido eliminado completamente; posponer un nuevo examen con medio de contraste hasta que la función renal vuelva a los niveles pre-examen. Los pacientes en diálisis pueden recibir medios de contraste, como el iomeprol, que sean dializables sin dificultad.
Diabetes mellitus- La presencia de daño renal en pacientes diabéticos es uno de los factores que predispone a disfunciones renales como consecuencia de la administración de medios de contraste.
El deterioro renal puede provocar lactoacidosis en pacientes diabéticos con daño renal tratados con biguanidas (metformina). Para prevenirlo, se deberá suspender el tratamiento con biguanidas en los siguientes casos: antes de la administración intraarterial de un medio de contraste con exposición renal de primer paso, en pacientes con eGFR inferior a 30 ml/min/1,73 m2 que reciban un medio de contraste por vía intravenosa o un medio de contraste por vía intraarterial con exposición renal de segundo paso, o en pacientes con lesión renal aguda, y solamente deberá ser reanudada después de 48 horas, siempre y cuando la función renal no haya cambiado significativamente.
Feocromocitoma- Estos pacientes pueden desarrollar graves crisis hipertensivas (raramente incontrolables) después de utilizar medio de contraste intravascular durante los procedimientos radiológicos.
En pacientes con feocromocitoma, se aconseja premedicación con bloqueadores de los receptores alfa, debido al riesgo de crisis hipertensivas.
Miastenia gravis- La administración de medios de contraste iodados puede agravar los signos y síntomas de miastenia.
Enfermedadcardiaca e hipertensión pulmonar- Existe un elevado riesgo de reacciones graves en pacientes que presentan una patología cardiovascular grave, particularmente en aquellos con insuficiencia cardiaca y arteriopatías coronarias. La inyección intravascular de medios de contraste puede provocar edema pulmonar en pacientes con descompensación cardiaca manifiesta o incipiente, mientras que la administración del medio de contraste en casos de hipertensión pulmonar y de valvulopatías puede favorecer alteraciones hemodinámicas. La aparición de signos de isquemia en el ECG y de graves arritmias es más común en los pacientes más ancianos y en aquellos con cardiopatías previas: su frecuencia y gravedad parecen estar relacionadas con la gravedad de la patología cardiaca.
Síntomas neurológicos- Se debe prestar particular atención cuando se administra un medio de contraste a pacientes con infarto cerebral agudo, hemorragia intracraneal y que presenten alteraciones de la barrera hematoencefálica, edema cerebral o desmielinización aguda. La presencia de tumores intracraneales o metástasis y antecedentes de epilepsia puede aumentar la probabilidad de aparición de crisis convulsivas. La administración de medios de contraste puede agudizar los síntomas neurológicos debidos a patologías cerebrovasculares degenerativas, isquémicas, inflamatorias o neoplásicas. Estos pacientes tienen un mayor riesgo de complicaciones neurológicas transitorias. Las inyecciones intravasculares de medios de contraste pueden causar fenómenos de angiospasmo y episodios de isquemia cerebral.
Alcoholismo- Se ha demostrado, experimental y clínicamente, que el alcoholismo agudo o crónico aumenta la permeabilidad de la barrera hematoencefálica. Facilita el paso de los agentes iodados al tejido cerebral que pueden producir trastornos del SNC. Hay que tener presente una posible reducción del umbral epiléptico en los alcohólicos.
Encefalopatía inducida por contraste– Se ha notificado encefalopatía con el uso de iomeprol.
La encefalopatía inducida por contraste puede manifestarse con síntomas y signos de disfunción neurológica como dolor de cabeza, alteraciones visuales, ceguera cortical, confusión, convulsiones, pérdida de coordinación, hemiparesia, afasia, inconsciencia, coma y edema cerebral en los minutos a las horas posteriores a la administración de iomeprol, y por lo general desaparece en unos días.
El producto se debe emplear con precaución en pacientes con enfermedades que afectan a la integridad de la barrera hematoencefálica (BHE), que pudieran causar una mayor permeabilidad del contraste a través de la BHE y aumentar el riesgo de encefalopatía. Si se sospecha de una encefalopatía inducida por contraste, se debe suspender la administración de iomeprol e iniciar un control médico adecuado.
Toxicomanía- Los pacientes toxicómanos requieren una particular atención debido a la posible reducción del umbral convulsivo.
Se recomienda realizar una fluoroscopia para minimizar la extravasación durante la inyección.
Sobredosis
En caso de que el médico responsable diagnostique una sobredosis intravascular accidental del medio de contraste, se debe controlar la hidratación y el equilibrio electrolítico del paciente, y corregirlos si fuera necesario. En esta situación, la función renal debe ser monitorizada durante al menos tres días.
En caso de sobredosis accidental intratecal, el paciente debe ser monitorizado cuidadosamente durante al menos 24 horas, para detectar signos y síntomas de trastornos del Sistema Nervioso Central. Dichos signos pueden ser: aumento de la hiperreflexia o espasmos tónico-clónicos, e incluso convulsiones generalizadas, hipertermia, estupor y depresión respiratoria.
- País de registro
- Disponibilidad en farmacias
Problema de suministro reportado
Los datos de la Agencia Española de Medicamentos y Productos Sanitarios (AEMPS) indican un problema de suministro que afecta a este medicamento.<br><br>La disponibilidad puede ser limitada en algunas farmacias.<br><br>Para actualizaciones o alternativas, consulte a su farmacéutico. - Principio activo
- Requiere recetaSí
- Fabricante
- Esta información es de carácter general y no sustituye la consulta con un profesional sanitario.
- Alternativas a IOMERON 250 MG IODO/ML SOLUCIÓN INYECTABLEForma farmacéutica: INYECTABLE, 30,62 g/100 mlPrincipio activo: IomeprolFabricante: Bracco Imaging S.P.A.Requiere recetaForma farmacéutica: INYECTABLE, 40,82 g/100 mlPrincipio activo: IomeprolFabricante: Bracco Imaging S.P.A.Requiere recetaForma farmacéutica: INYECTABLE, 61,24 g iomeprol/100 mlPrincipio activo: IomeprolFabricante: Bracco Imaging S.P.A.Requiere receta
Médicos online para IOMERON 250 MG IODO/ML SOLUCIÓN INYECTABLE
Comenta la dosis, los posibles efectos secundarios, interacciones, contraindicaciones o la revisión de receta de IOMERON 250 MG IODO/ML SOLUCIÓN INYECTABLE, sujeto a valoración médica y a la normativa local.
Preguntas frecuentes















