
AIDESSIA 0,15 MG/0,03 MG COMPRIMIDOS RECUBIERTOS CON PELICULA EFG

Cómo usar AIDESSIA 0,15 MG/0,03 MG COMPRIMIDOS RECUBIERTOS CON PELICULA EFG
Traducción generada por IA
Este contenido ha sido traducido automáticamente y se ofrece solo con fines informativos. No sustituye la consulta con un profesional sanitario.
Ver originalContenido del prospecto
Introducción
Prospecto: Información para el usuario
aidessia0,15mg /0,03 mg, comprimidos recubiertos con película EFG
desogestrel/etinilestradiol
Cosas importantes que debe saber acerca de los anticonceptivos hormonales combinados (AHCs):
- Estos métodos uno de los métodos anticonceptivos reversibles más fiables si se utilizan correctamente.
- Aumentan ligeramente el riesgo de sufrir un coágulo de sangre en las venas y arterias, especialmente en el primer año o cuando se reinicia el uso de un anticonceptivo hormonal combinado tras una pausa de 4 semanas o más.
- Esté alerta y consulte a su médico si cree que puede tener síntomas de un coágulo de sangre (ver sección 2 “Coágulos de sangre”).
Lea todo el prospecto detenidamente antes de empezar a usar este medicamento, porque contiene información importante para usted.
- Conserve este prospecto, ya que puede tener que volver a leerlo.
- Si tiene alguna duda, consulte a su médico o farmacéutico.
- Este medicamento se le ha recetado solamente a usted, y no debe dárselo a otras personas. Puede perjudicarles, incluso si sus signos de enfermedad son los mismos que los suyos.
- Si experimenta efectos adversos mencionados en la sección 4 o si sufre algún efecto adverso no mencionado en este prospecto, consulte a su médico, o farmacéutico.
Contenido del prospecto:
- Qué es aidessia y para qué se utiliza
- Qué necesita saber antes de empezar a tomar aidessia
- Cómo tomar aidessia
- Posibles efectos adversos
- Conservación de aidessia
- Contenido del envase e información adicional
1. Qué es aidessia y para qué se utiliza
Composición y tipo de medicamento anticonceptivo
Este medicamento es un anticonceptivo oral combinado, también llamado píldora.
Cada uno de los 21 comprimidos blancos contiene una pequeña cantidad de dos hormonas femeninas diferentes, desogestrel (una hormona que funciona de manera similar a un progestágeno) y etinilestradiol (una hormona que funciona de manera similar a un estrógeno). Debido a las pequeñas cantidades de hormonas, aidessia se considera un anticonceptivo de dosis baja. Dado que la cantidad de cada hormona es la misma en todos los comprimidos del blíster, se llama píldora combinada.
Para qué se utiliza
Tome Aidessia para prevenir el embarazo.
Cuando lo toma correctamente (sin olvidar comprimidos) la probabilidad de quedar embarazada es muy baja.
2. Qué necesita saber antes de empezar a tomar aidessia
Consideraciones generales Antes de empezar a usar aidessia debe leer la información acerca de los coágulos de sangre en la sección 2. Es particularmente importante que lea los síntomas de un coágulo de sangre (ver sección 2 “Coágulos de sangre”). En este prospecto se describen varias situaciones en las que usted debería de interrumpir el uso de la píldora o en la que el efecto de la píldora puede disminuir. En dichas situaciones usted no debería tener relaciones sexuales o debería tomar precauciones anticonceptivas adicionales no hormonales, por ejemplo, uso de preservativo u otro método de barrera. No utilice el método del ritmo o el de la temperatura. Estos métodos pueden no ser fiables puesto que píldora altera los cambios mensuales de la temperatura corporal y del moco cervical. aidessiaal igual que otros anticonceptivos hormonales, no protege frente a la infección por VIH (SIDA) o cualquier otra enfermedad de transmisión sexual (ETSs). |
No tomeaidessia:
No debe usar aidessia si tiene alguna de las afecciones enumeradas a continuación. Informe a su médico si tiene alguna de las afecciones enumeradas a continuación. Su médico comentará con usted qué otra forma de anticoncepción sería más adecuada.
- Si tiene (o ha tenido alguna vez) un coágulo de sangre en un vaso sanguíneo de las piernas (trombosis venosa profunda, TVP), en los pulmones (embolia pulmonar, EP) o en otros órganos.
- Si sabe que padece un trastorno que afecta a la coagulación de la sangre: por ejemplo, deficiencia de proteína C, deficiencia de proteína S, deficiencia de antitrombina III, factor V Leiden o anticuerpos antifosfolípidos.
- Si necesita una operación o si pasa mucho tiempo sin ponerse de pie (ver sección “Coágulos de sangre”).
- Si ha sufrido alguna vez un ataque al corazón o un ictus.
- Si tiene (o ha tenido alguna vez) una angina de pecho (una afección que provoca fuerte dolor en el pecho y puede ser el primer signo de un ataque al corazón) o un accidente isquémico transitorio (AIT, síntomas temporales de ictus).
- Si tiene alguna de las siguientes enfermedades que pueden aumentar su riesgo de formación de un coágulo en las arterias:
- Diabetes grave con lesión de los vasos sanguíneos.
- Tensión arterial muy alta.
- Niveles muy altos de grasa en la sangre (colesterol o triglicéridos).
- Una afección llamada hiperhomocisteinemia.
- Si tiene (o ha tenido alguna vez) un tipo de migraña llamada “migraña con aura”.
- Si usted tiene (o ha tenido alguna vez) pancreatitis (una inflamación del páncreas) asociado con altos niveles de sustancias grasas en la sangre.
- Si usted tiene (o ha tenido alguna vez) ictericia (color amarillento de la piel o los ojos) o enfermedad hepática grave.
- Si usted tiene (o ha tenido alguna vez) cáncer afectado por hormonas sexuales, (cáncer de mama o cáncer de los órganos sexuales).
- Si usted tiene (o ha tenido alguna vez) un tumor hepático.
- Si usted tiene hemorragias vaginales, que no han sido explicadas por su médico.
- Si tiene una inflamación anormal del endometrio.
- Si usted es alérgica a etinilestradiol, a desogestrel, o a alguno de los demás componentes de este medicamento (incluidos en la sección 6). Esto puede manifestarse con picor, erupción o inflamación.
- Si es alérgica a los cacahuetes o a la soja.
- Si usted tiene Hepatitis C y está tomando medicamentos que contienen ombistavir / paritaprevir / ritonavir y dasabuvir, glecaprevir / pibrentasvir o sofosbuvir/velpatasvir/voxilaprevir (ver sección Toma de aidessia con otros medicamentos).
Si sufre alguno de estos síntomas o los tiene por primera vez mientras toma aidessia, deje de tomarlo inmediatamente y comuníquese con su médico lo antes posible. Mientras tanto, utilice otro método anticonceptivo no hormonal. Consulte también las "Consideraciones generales" al comienzo de la sección 2.
Cuándo debe tener especial cuidado conaidessia
¿Cuándo debe consultar a su médico? Busque asistencia médica urgente
Para obtener una descripción de los síntomas de estos efectos adversos graves, consulte “Cómo reconocer un coágulo de sangre”. |
Informe a su médico si alguna de las siguientes condiciones le aplica a usted
Si se da alguno de los siguientes casos o si alguna de las afecciones se desarrolla o empeora mientras está usando aidessia, también debe informar a su médico:
- Si usted fuma;
- Si usted padece diabetes;
- Si tiene sobrepeso;
- si tiene presión arterial alta;
- si tiene un problema con las válvulas de su corazón o una cierta alteración del ritmo;
- si tiene una inflamación de las venas debajo de la piel (tromboflebitis superficial).
- si tiene varices.
- Si algún familiar cercano ha tenido alguna vez una trombosis, un ataque al corazón o un derrame cerebral.
- Si alguna vez ha tenido migrañas.
- si sufre epilepsia
- si tiene niveles elevados de grasa en la sangre (hipertrigliceridemia) o antecedentes familiares positivos para esta afección. La hipertrigliceridemia se ha asociado con un mayor riesgo de desarrollar pancreatitis (inflamación del páncreas);
- si necesita una operación o no puede ponerse de pie durante mucho tiempo (ver en la sección 2 “Coágulos de sangre”).
- si acaba de dar a luz, tiene un mayor riesgo de coágulos sanguíneos. Debe preguntar a su médico cuánto tiempo después del parto puede empezar a tomar aidessia.
- si algún familiar cercano ha tenido cáncer de mama
- si tiene alguna enfermedad del hígado o de la vesícula biliar
- Si tiene enfermedad de Crohn o colitis ulcerosa (enfermedad intestinal inflamatoria crónica).
- Si tiene lupus eritematoso sistémico (LES, una enfermedad que afecta a su sistema natural de defensa).
- Si tiene síndrome urémico hemolítico (SUH, un trastorno de la coagulación de la sangre que provoca insuficiencia en el riñón).
- Si tiene anemia de células falciformes (una enfermedad hereditaria de los glóbulos rojos).
- Si usted tiene alguna enfermedad que apareciera por primera vez o empeorará durante el embarazo o durante un anterior uso de hormonas sexuales(por ejemplo, pérdida de audición, una enfermedad metabólica llamada porfiria, una enfermedad de la piel que causa vesículas durante el embarazo llamada herpes gestacional, una enfermedad neurológica llamada corea de Sydenham que causa movimientos involuntarios del cuerpo.
- Si usted tiene o ha tenido alguna vez cloasma (manchas de color pardo dorado, también llamadas “manchas del embarazo”, especialmente en la cara o cuello). En ese caso, hay que evitar la exposición directa al sol o a los rayos ultravioleta.
- Si experimenta síntomas de angioedema, tales como hinchazón de la cara, lengua y/o garganta, y/o dificultad para tragar o urticaria con posible dificultad para respirar, contacte con un médico de forma inmediata. Los productos que contienen estrógenos pueden causar o empeorar los síntomas del angioedema hereditario y adquirido.
aidessiay coágulos de sangre (Trombosis)
COAGULOS DE SANGRE (TROMBOSIS)
El uso de un anticonceptivo hormonal combinado como aidessia aumenta su riesgo de sufrir un coágulo de sangre en comparación con no usarlo. En raras ocasiones un coágulo de sangre puede bloquear vasos sanguíneos y provocar problemas graves.
Se pueden formar coágulos de sangre:
- En las venas (lo que se llama “trombosis venosa”, “tromboembolismo venoso” o TEV).
- En las arterias (lo que se llama “trombosis arterial”, “tromboembolismo arterial” o TEA).
La recuperación de los coágulos de sangre no es siempre completa. En raras ocasiones puede haber efectos graves duraderos o, muy raramente, pueden ser mortales.
Es importante recordar que el riesgo global de un coágulo de sangre perjudicial debido a aidessiaes pequeño.
CÓMO RECONOCER UN COÁGULO DE SANGRE
Busque asistencia médica urgente si nota alguno de los siguientes signos o síntomas.
¿Experimenta alguno de estos signos? | ¿Qué es posible que esté sufriendo? |
| Trombosis venosa profunda |
Si no está segura, consulte a un médico, ya que algunos de estos síntomas como la tos o la falta de aliento se pueden confundir con una afección más leve como una infección respiratoria (por ejemplo un catarro común) | Embolia pulmonar |
Síntomas que se producen con más frecuencia en un ojo:
| Trombosis de las venas retinianas (coágulo de sangre en el ojo). |
| Ataque al corazón |
A veces los síntomas de un ictus pueden ser breves, con una recuperación casi inmediata y completa, pero de todos modos debe buscar asistencia médica urgente ya que puede correr riesgo de sufrir otro ictus. | Ictus |
| Coágulos de sangre que bloquean otros vasos sanguíneos. |
COÁGULOS DE SANGRE EN UNA VENA
¿Qué puede ocurrir si se forma un coágulo de sangre en una vena?
- El uso de anticonceptivos hormonales combinados se ha relacionado con un aumento del riesgo de coágulos de sangre en las venas (trombosis venosa). No obstante, estos efectos adversos son raros. Se producen con más frecuencia en el primer año de uso de un anticonceptivo hormonal combinado.
- Si se forma un coágulo de sangre en una vena de la pierna o del pie, puede provocar trombosis venosa profunda (TVP).
- Si un coágulo de sangre se desplaza desde la pierna y se aloja en el pulmón puede provocar una embolia pulmonar.
- En muy raras ocasiones se puede formar un coágulo en una vena de otro órgano como el ojo (trombosis de las venas retinianas)
¿Cuándo es mayor el riesgo de presentar un coágulo de sangre en una vena?
El riesgo de presentar un coágulo de sangre en una vena es mayor durante el primer año en el que se toma un anticonceptivo hormonal combinado por primera vez. El riesgo puede ser mayor también si vuelve a empezar a tomar un anticonceptivo hormonal combinado (el mismo medicamento o un medicamento diferente) después de una interrupción de 4 semanas o más.
Después del primer año, el riesgo disminuye, pero siempre es algo mayor que si no estuviera tomando un anticonceptivo hormonal combinado.
Cuando deja de tomar aidessia, su riesgo de presentar un coágulo de sangre regresa a la normalidad en pocas semanas.
¿Cuál es el riesgo de presentar un coágulo de sangre?
El riesgo depende de su riesgo natural de TEV y del tipo de anticonceptivo hormonal combinado que esté tomando.
El riesgo global de presentar un coágulo de sangre en la pierna o en el pulmón (TVP o EP) con aidessia es pequeño.
- De cada 10.000 mujeres que no usan un anticonceptivo hormonal combinado y que no están embarazadas, unas 2 presentarán un coágulo de sangre en un año.
- De cada 10.000 mujeres que usan un anticonceptivo hormonal combinado que contiene levonorgestrel, noretisterona o norgestimato, unas 5-7 presentarán un coágulo de sangre en un año.
- De cada 10.000 mujeres que usan un anticonceptivo hormonal combinado que contiene desogestrel como aidessia, entre 9 y 12 mujeres presentarán un coágulo de sangre en un año.
- El riesgo de presentar un coágulo de sangre dependerá de sus antecedentes personales (ver “Factores que aumentan su riesgo de un coágulo sanguíneo” más adelante)
Riesgo de presentar un coágulo de sangre en un año | |
Mujeres que no utilizanun comprimido/parche/anillo hormonal combinado y que no están embarazadas | Unas 2 de cada 10.000 mujeres |
Mujeres que utilizan un comprimido anticonceptivo hormonal combinado que contiene levonorgestrel, noretisterona o norgestimato | Unas 5 -7 de cada 10.000 mujeres |
Mujeres que utilizan aidessia | Unas 9 -12 de cada 10.000 mujeres |
Factores que aumentan su riesgo de un coágulo de sangre en una vena
El riesgo de tener un coágulo de sangre con aidessia es pequeño, pero algunas afecciones aumentan el riesgo. Su riesgo es mayor:
- Si tiene exceso de peso (índice de masa corporal o IMC superior a 30 kg/m2).
- Si alguno de sus parientes próximos ha tenido un coágulo de sangre en la pierna, pulmón u otro órgano a una edad temprana (es decir, antes de los 50 años aproximadamente). En este caso podría tener un trastorno hereditario de la coagulación de la sangre.
- Si necesita operarse o si pasa mucho tiempo sin ponerse de pie debido a una lesión o enfermedad o si tiene la pierna escayolada. Tal vez haya que interrumpir el uso de aidessia varias semanas antes de la intervención quirúrgica o mientras tenga menos movilidad. Si necesita interrumpir el uso de aidessia pregúntele a su médico cuándo puede empezar a usarlo de nuevo.
- Al aumentar la edad (en especial por encima de unos 35 años).
- Si ha dado a luz hace menos de unas semanas.
El riesgo de presentar un coágulo de sangre aumenta cuantas más afecciones tenga.
Los viajes en avión (más de 4 horas) pueden aumentar temporalmente el riesgo de un coágulo de sangre, en especial si tiene alguno de los demás factores de riesgo enumerados.
Es importante informar a su médico si sufre cualquiera de las afecciones anteriores, aunque no esté segura. Su médico puede decidir que hay que interrumpir el uso de aidessia.
Si alguna de las afecciones anteriores cambia mientras está utilizando aidessia, por ejemplo un pariente próximo experimenta una trombosis sin causa conocida o usted aumenta mucho de peso, informe a su médico.
COÁGULOS DE SANGRE EN UNA ARTERIA
¿Qué puede ocurrir si se forma un coágulo de sangre en una arteria?
Al igual que un coágulo de sangre en una vena, un coágulo en una arteria puede provocar problemas graves. Por ejemplo, puede provocar un ataque al corazón o un ictus.
Factores que aumentan su riesgo de un coágulo de sangre en una arteria
Es importante señalar que el riesgo de un ataque al corazón o un ictus por utilizar aidessia es muy pequeño, pero puede aumentar:
- Con la edad (por encima de unos 35 años).
- Si fuma.Cuando utiliza un anticonceptivo hormonal combinado como aidessia se le aconseja que deje de fumar. Si no es capaz de dejar de fumar y tiene más de 35 años, su médico puede aconsejarle que utilice un tipo de anticonceptivo diferente.
- Si tiene sobrepeso.
- Si tiene la tensión alta.
- Si algún pariente próximo ha sufrido un ataque al corazón o un ictus a una edad temprana (menos de unos 50 años). En este caso usted también podría tener mayor riesgo de sufrir un ataque al corazón o un ictus.
- Si usted o alguno de sus parientes próximos tiene un nivel elevado de grasa en la sangre (colesterol o triglicéridos).
- Si padece migrañas, especialmente migrañas con aura.
- Si tiene un problema de corazón (trastorno de las válvulas, alteración del ritmo cardíaco llamado fibrilación auricular).
- Si tiene diabetes.
Si tiene una o más de estas afecciones o si alguna de ellas es especialmente grave, el riesgo de presentar un coágulo de sangre puede verse incrementado aún más.
Si alguna de las afecciones anteriores cambia mientras está utilizando aidessia, por ejemplo empieza a fumar, un pariente próximo experimenta una trombosis sin causa conocida o usted aumenta mucho de peso, informe a su médico.
La píldora y el cáncer
La píldora aumenta ligeramente el cáncer de mama en comparación con las mujeres que no usan la píldora. No se encuentra ninguna diferencia 10 años después de dejar de usar la Píldora. No se sabe si esta diferencia es causada por la Píldora. Puede ser que las mujeres que usan la Píldora fueran examinadas con más frecuencia, de modo que el cáncer de mama se detectó antes.
En raras ocasiones se han comunicado tumores benignos en el hígado, y más raramente incluso tumores malignos, en usuarias de anticonceptivos. Acuda a su médico si usted sufre un fuerte dolor abdominal repentino.
La infección crónica por el Virus del Papiloma Humano (VPH) es el factor de riesgo más importante para el cáncer de cuello uterino. En las mujeres que usan la Píldora durante mucho tiempo, la probabilidad de contraer cáncer de cuello uterino puede ser ligeramente mayor. Es posible que este hallazgo no sea causado por la píldora en sí, pero puede estar relacionado con el comportamiento sexual y otros factores (como mejores controles del cuello uterino).
Trastornos psiquiátricos:
Algunas mujeres que utilizan anticonceptivos hormonales como aidessia han notificado depresión o un estado de ánimo deprimido. La depresión puede ser grave y a veces puede inducir pensamientos suicidas. Si experimenta alteraciones del estado de ánimo y síntomas depresivos, póngase en contacto con su médico para obtener asesoramiento médico adicional lo antes posible.
aidessia y uso de otros medicamentos
Informe siempre al médico que le haya prescrito aidessia sobre los medicamentos o preparados a base de hierbas que esté tomando, ha tomado recientemente o podría tener que tomar. También informe a cualquier otro médico o dentista que le recete otro medicamento (o a su farmacéutico) de que usted usa aidessia. Ellos pueden indicarle si usted necesita tomar precauciones anticonceptivas adicionales (por ejemplo, preservativos) y, si es así, durante cuánto tiempo.
No tome aidessia si usted tiene Hepatitis C y está tomando medicamentos que contienen ombistavir / paritaprevir / ritonavir y dasabuvir, glecaprevir / pibrentasvir o sofosbuvir/velpatasvir/voxilaprevir, ya que estos medicamentos pueden producir aumentos en los resultados de pruebas hepáticas (aumento de la enzima hepática ALT).
Su médico le prescribirá otro tipo de anticonceptivo antes de comenzar el tratamiento con estos medicamentos.
aidessia se puede volver a usar aproximadamente 2 semanas después de la finalización de este tratamiento. Consulte la sección “No utilice aidessia”.
Algunos medicamentos:
- pueden tener influencia en los niveles de aidessia en sangre
- pueden hacer que sea menos efectivo en la prevención del embarazo
- pueden causar sangrados inesperados.
Esto incluye a los medicamentos utilizados en el tratamiento de:
- La epilepsia (p.ej., primidona, fenitoína, fenobarbital, carbamazepina, oxcarbazepina, topiramato, felbamato).
- La tuberculosis (p.ej., rifampicina, rifabutina).
- Las infecciones por el VIH (p.ej., ritonavir, nelfinavir, nevirapina, efavirenz)
- Hepatitis C (p. Ej., boceprevir, telaprevir)
- Otra enfermedad infecciosa (griseofulvina).
- Tensión sanguínea alta en vasos sanguíneos de los pulmones (bosentan).
- Estados de ánimo depresivos (la planta medicinal hierba de San Juan).
Si está tomando medicamentos o productos a base de hierbas que pueden hacer que aidessia sea menos eficaz, también debe utilizar un método anticonceptivo de barrera. Dado que el efecto de otro medicamento en aidessia puede durar hasta 28 días después de suspender el medicamento, es necesario utilizar el método anticonceptivo de barrera adicional durante ese tiempo.
aidessia puede influir en el efecto de otros medicamentos, por ejemplo:
- Los que contienen ciclosporina.
- El antiepiléptico lamotrigina (esto puede llevar a un aumento de los ataques).
Pruebas de laboratorio
Si se va a realizar una prueba de laboratorio, comente con su médico o con el personal del laboratorio que está tomando la píldora, ya que los anticonceptivos hormonales pueden influir en los resultados de algunas pruebas.
Embarazo y lactancia
Embarazo
No tome aidessiasi está embarazada o cree que podría estarlo.Si cree que podría estar embarazada mientras usa aidessia, comuníquese con su médico lo antes posible.
Lactancia
No se recomienda el uso de aidessia durante la lactancia. Póngase en contacto con su médico si aún desea utilizar aidessia durante la lactancia.
Conducción y uso de máquinas
aidessia no tiene efectos conocidos sobre la capacidad para conducir o utilizar máquinas.
aidessiacontiene lactosa y aceite de soja
Si su médico le ha indicado que padece una intolerancia a ciertos azúcares, consulte con él antes de tomar este medicamento.
Si usted es alérgico al cacahuete o a la soja, no utilice este medicamento.
Niños y adolescentes
No se dispone de datos clínicos sobre eficacia y seguridad en adolescentes menores de 18 años.
¿Cuándo debe contactar a su médico?
Revisiones regulares
Es posible que su médico le aconseje que haga citas regularmente para un chequeo de la píldora. Su situación personal determinará con qué frecuencia debe regresar para las revisiones y qué pruebas se realizarán.
Póngase en contacto con su médico lo antes posible si:
- nota posibles signos que podrían indicar que tiene un coágulo de sangre. Esto podría significar que tiene un coágulo de sangre en un vaso sanguíneo de la pierna (trombosis venosa profunda), un coágulo de sangre en un vaso sanguíneo del pulmón (embolia pulmonar), un infarto de miocardio o un accidente cerebrovascular (consulte la sección " aidessia y coágulos de sangre").
- Para obtener una descripción de los síntomas de estos efectos secundarios graves, consulte "Cómo reconocer un coágulo de sangre".
- nota algún cambio en su propia salud, especialmente relacionado con cualquiera de los elementos mencionados en este prospecto (ver también “¿Cuándo no debe usar aidessia?” y “Cuándo debe tener especial cuidado con aidessia”); no se olvide de los temas relacionados con su familia cercana;
- siente un bulto en el seno
- experimenta síntomas de angioedema como hinchazón de la cara, lengua y/o garganta y/o dificultad para tragar o urticaria potencialmente con dificultad para respirar (ver también la sección “Cuándo tener mucho cuidado con aidessia”)
- va a utilizar otros medicamentos (ver también “Uso de otros medicamentos”)
- su capacidad de moverse está limitada durante un largo período de tiempo o va a someterse a una cirugía (consulte a su médico al menos con 4 semanas de antelación)
- experimenta irregularidades de sangrado sostenidas o que empeoran
- olvidó los comprimidos en la primera semana del blíster y tuvo relaciones sexuales en los siete días
- tiene diarrea severa
- pierde su período dos veces seguidas. No comience el siguiente blíster hasta que su médico se lo indique.
3. Cómo tomar aidessia
Tome siempre este medicamento exactamente como le haya indicado su médico o farmacéutico. Si duda de estar usándolo correctamente, consulte a su médico o farmacéutico.
Cuándo y cómo tomar los comprimidos
Cada blíster contiene 21 comprimidos. En el blíster, cada comprimido está marcado con el día de la semana en que debe tomarse. Tome su comprimido aproximadamente a la misma hora todos los días, con un poco de líquido si es necesario.
Siga la dirección de las flechas en el blíster hasta que haya tomado los 21 comprimidos. No tome ningún comprimido durante los próximos 7 días. A lo largo de estos 7 días debe comenzar el periodo (el sangrado por deprivación). Por lo general, comenzará el día 2-3 después del último comprimido de aidessia.
Empiece a tomar el siguiente blíster de aidessia el octavo día, aunque siga sangrando. Esto quiere decir que siempre comenzará los nuevos blísteres el mismo día de la semana, y también significa que tendrá su menstruación aproximadamente los mismos días todos los meses.
¿Cuándo puede empezar con el primer blíster?
- Cuando no se ha usado un tratamiento anticonceptivo hormonal en el mes anterior.Empiece a tomar los comprimidos el primer día del ciclo, es decir, el primer día de su sangrado menstrual. El medicamento funcionará inmediatamente, no es necesario utilizar un método anticonceptivo adicional. También puede comenzar los días 2-5 del ciclo, pero en ese caso, asegúrese de usar un método anticonceptivo adicional, cómo un preservativo, durante los primeros 7 días.
- Al cambiar desde otro anticonceptivo hormonal combinado, o un anillo o parche vaginal.
Puede comenzar a tomar su tratamiento el día después de tomar el último comprimido de su actual blíster (es decir, sin interrupción). Si su blíster de tratamiento anticonceptivo hormonal anterior contenía comprimidos inactivos, puede comenzar su tratamiento con aidessia el día después de tomar el último comprimido activo (si no está seguro de cuál es, consulte a su médico o farmacéutico). También puede comenzar tarde, pero nunca más tarde del día siguiente a la pausa sin comprimidos de su anticonceptivo anterior (o el día posterior a los últimos comprimidos inactivos de su tratamiento anterior).
En caso de que use un anillo vaginal o un parche, debe comenzar a usar este medicamento el día de la extracción. También puede empezar a usar este medicamento más adelante, pero como máximo siete días después de quitarse el anillo o el último parche.
Si ha usado comprimidos anticonceptivos, parche o anillo completamente de acuerdo con las prescripciones y está segura de que no está embarazada, también puede dejar de usarlos o quitarse el anillo o el parche cualquier día de su ciclo actual y cambiar de inmediato a usar este medicamento.
Si sigue estas indicaciones, no necesita utilizar un método anticonceptivo adicional, como un preservativo.
- Al cambiar desde un método de progestágeno solo (minipíldora)
Puede dejar de tomar la minipíldora cualquier día y empezar a tomar este medicamento al día siguiente, en cualquier momento. Pero asegúrese de utilizar también un método anticonceptivo adicional, como un preservativo, durante los primeros 7 días de toma de comprimidos.
- Al cambiar de un dispositivo intrauterino (DIU) inyectable, implantado o liberador de progestágenos.
Empiece a tomar este medicamento cuando le corresponda la próxima inyección o el día en que se extraiga el implante o el DIU. Asegúrese de utilizar un método anticonceptivo adicional, como un preservativo, durante los primeros 7 días que esté tomando aidessia.
- Tras tener un niño.
Si acaba de tener un bebé, es posible que su médico le indique que espere hasta después de su primer período normal antes de comenzar a tomar este medicamento. A veces es posible empezar antes. Tu médico te aconsejará. Lo mismo se aplica en caso de que esté dando el pecho y quiera tomar aidessia.
- Tras un aborto espontáneo o aborto
Siga el consejo de su médico.
Si toma másaidessiadel que debe
No se han comunicado casos en los que la ingestión de una sobredosis de este medicamento haya causado daños graves.
Si toma demasiados comprimidos, puede sentirse mal, vomitar o tener sangrado vaginal.
Si usted descubre que un niño ha tomado este medicamento, consulte con su médico.
Qué hacer si:
Olvidó tomarsus comprimidos
- Si la píldora olvidada se toma dentro de las12 horas,la protección anticonceptiva no se reducirá. Tome el comprimido tan pronto como se acuerde y los comprimidos siguientes a la hora habitual.
- Si se retrasa más de 12 horas en la toma de algún comprimido, la fiabilidad del tratamiento puede verse reducida. Cuantos más comprimidos consecutivos haya olvidado, mayor será el riesgo de que disminuya la eficacia anticonceptiva.
Existe un riesgo particularmente alto de quedarse embarazada si se olvida tomar los comprimidos al principio o al final del blíster. Por ello, debe seguir las siguientes reglas que se detallan a continuación (ver diagrama):
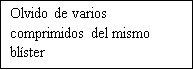
Olvido de más de un comprimido del blíster
Consulte con su médico.
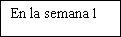
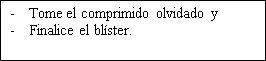
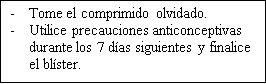
Olvido de un comprimido en la semana 1
Tome el comprimido olvidado tan pronto como se acuerde, incluso si esto significa que tenga que tomar dos comprimidos al mismo tiempo. Tome los siguientes comprimidos a la hora habitual. Utilice precauciones anticonceptivas adicionalesdurante los próximos 7 días. Si usted ha mantenido relaciones sexuales en la semana previa al olvido del comprimido, debe saber que existe la posibilidad de quedarse embarazada. En ese caso, consulte a su médico inmediatamente.
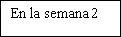
Olvido de un comprimido en la semana 2
Tome el comprimido olvidado tan pronto como se acuerde, incluso si esto significa que tenga que tomar dos comprimidos al mismo tiempo. Tome los siguientes comprimidos a la hora habitual. La fiabilidad de la píldora se mantiene. No es necesario utilizar precauciones anticonceptivas adicionales.
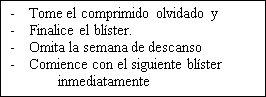
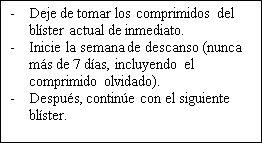
Olvido de un comprimido en la semana 3
Puede elegir cualquiera de las siguientes opciones, sin necesidad de precauciones anticonceptivas adicionales:
- Tome el comprimido olvidado tan pronto como se acuerde, incluso si esto significa que tenga que tomar dos comprimidos al mismo tiempo. Tome los siguientes comprimidos a la hora habitual. Cuando termine el blíster de comprimidos, comience el siguiente blíster al día siguiente sin interrupción. Es posible que no tenga una hemorragia por deprivación hasta el final del segundo blíster, pero puede tener manchado o sangrado intermenstrual durante el segundo blíster.
- Deje de tomar el blíster actual. Deje el descanso habitual de 7 días o menos (anote siempre el día en que olvidó tomar el comprimido). Luego continúe con el siguiente blíster.
Al seguir este método, siempre puede comenzar su próximo blíster el mismo día de la semana como lo hace habitualmente.
- Si usted ha olvidado tomar alguno de los comprimidos en un blíster y no sangra durante el periodo de descanso, es posible que esté embarazada. En ese caso, póngase en contacto con su médico antes de seguir con el siguiente blíster.



Si tiene trastornos gastrointestinales (por ejemplo, vómitos, diarrea intensa)
Si se encuentra enferma (vomita) o tiene diarrea muy fuerte, es posible que su cuerpo no obtenga la dosis habitual de hormonas de la píldora. Si vomita dentro de las 3 a 4 horas posteriores a la toma de la píldora, es como si se hubiera saltado una píldora. Debe seguir los consejos dados anteriormente para las píldoras olvidadas. Hable con su médico si sufre de diarrea intensa.
Si quiere retrasar su periodo
Puede posponer su período, aunque no es recomendable. Puede retrasar su período en casos excepcionales comenzando el siguiente blíster de aidessia al día siguiente sin interrupción. Puede continuar con este blíster durante el tiempo que desee, hasta que este blíster esté vacío. Mientras usa el segundo blíster, es posible que tenga un sangrado o manchado intermenstrual. Comience su próximo blíster después del período habitual de 7 días sin comprimidos.
Si quiere cambiar el día de inicio de su período
Si usted toma los comprimidos según las indicaciones, tendrá su período aproximadamente el mismo día. Si desea cambiar esto, simplemente acorte (nunca alargue) el período sin comprimidos entre dos blíster. Por ejemplo, si su período generalmente comienza un viernes y en el futuro desea que comience el martes (3 días antes), deberá comenzar su próximo blíster 3 días antes de lo habitual. Si hace que su período sin comprimidos sea muy corto (por ejemplo, 3 días o menos), es posible que no tenga sangrado durante el intervalo. Es posible que tenga sangrado intermenstrual o manchado durante el uso del siguiente blíster del medicamento .
Si tiene un sangrado inesperado
Con la toma de cualquier comprimido anticonceptivo, durante los primeros meses, puede tener un sangrado vaginal irregular (manchado o hemorragia intermenstrual) entre periodos. Puede que necesite utilizar productos de protección higiénica femenina, pero continue utilizando sus comprimidos como normalmente. El sangrado vaginal irregular normalmente se detiene una vez su cuerpo se ha adaptado al tratamiento (normalmente después de unos 3 blísters). Contacte con su médico si el sangrado continua, aumenta o empieza de nuevo.
Si no aparece el periodo
Si ha tomado todos los comprimidos en el momento adecuado, y no ha vomitado, o tenido diarrea intensa o usado otros medicamentos, es bastante improbable que esté embarazada. Empiece su próximo blíster como normalmente.
Si tiene dos faltas seguidas, puede que esté embarazada. Contacte con su médico inmediatamente. No empiece el siguiente blíster de este medicamento hasta que su médico haya confirmado que no está embarazada.
Si quiere interrumpir el tratamiento con aidessia
Usted puede dejar de tomar este medicamento en cualquier momento que desee. Si no quiere quedarse embarazada, consulte con su médico para que le aconseje sobre el uso de otros métodos anticonceptivos fiables. Si lo deja porque quiere quedarse embarazada, generalmente se recomienda que espere hasta que haya tenido un período natural antes de intentar concebir. Esto le ayuda a saber cuándo nacerá el bebé.
Si tiene cualquier otra duda sobre el uso de este medicamento, pregunte a su médico o farmacéutico.
4. Posibles efectos adversos
Al igual que todos los medicamentos, este medicamento puede producir efectos adversos, aunque no todas las personas los sufran. Si sufre cualquier efecto adverso, especialmente si es grave y persistente, o tiene algún cambio de salud que cree que puede deberse a aidessia, consulte a su médico.
Todas las mujeres que toman anticonceptivos hormonales combinados corren mayor riesgo de presentar coágulos de sangre en las venas (tromboembolismo venoso (TEV)) o coágulos de sangre en las arterias (tromboembolismo arterial (TEA)). Para obtener información más detallada sobre los diferentes riesgos de tomar anticonceptivos hormonales combinados, ver sección 2 “Qué necesita saber antes de empezar a usar aidessia”.
Contacte con un médico de forma inmediata si experimenta cualquiera de los siguientes síntomas de angioedema: hinchazón de la cara, lengua y/o garganta, y/o dificultad para tragar o urticaria con posible dificultad para respirar (ver también sección “Advertencias y precauciones”).
Al igual que con todas las píldoras, durante los primeros meses, el patrón de sus períodos puede cambiar. Esta diferencia puede manifestarse en la frecuencia del sangrado (si no aparece, con menos frecuencia, con más frecuencia o de forma continua), la cantidad de sangrado o la duración del sangrado.
Frecuentes(pueden afectar hasta 1 de cada 10 mujeres):
- Depresión o cambios de humor.
- Dolor de cabeza.
- Náuseas.
- Dolores abdominales.
- Senos sensibles o dolorosos.
- Aumento de peso.
Poco frecuentes(pueden afectar hasta 1 de cada 100 mujeres):
- Retención de líquidos.
- Disminución de la apetencia sexual.
- Migraña.
- Vómitos.
- Diarreas.
- Erupción cutánea o urticaria.
- Aumento de las mamas.
Raros(pueden afectar hasta 1 de cada 1.000 mujeres):
- Coágulos de sangre perjudiciales en una vena o arteria, por ejemplo:
- En una pierna o pie (es decir, TVP).
- En un pulmón (es decir, EP).
- Ataque al corazón.
- Ictus.
- Ictus leve o síntomas temporales similares a los de un ictus, lo que se llama accidente isquémico transitorio (AIT).
- Coágulos de sangre en el hígado, estómago/intestino, riñones u ojo.
Las posibilidades de tener un coágulo de sangre pueden ser mayores si tiene cualquier otra afección que aumente este riesgo (ver sección 2 para obtener más información sobre las afecciones que aumentan el riesgo de padecer coágulos de sangre y los síntomas de un coágulo de sangre).
- Reacciones hipersensibilidad
- aumento de la líbido
- Molestias en los ojos si usa lentes de contacto
- Eritema nodoso (hinchazón similar a un hematoma en las espinillas), eritema multiforme (erupción con úlceras o manchas rojas e irregulares)
- Mamas que producen un líquido lechoso de los pezones, cambios en las secreciones vaginales
- Disminución de peso
Notificación de efectos adversos
Si experimenta cualquier tipo de efecto adverso, consulte a su médico o farmacéutico, incluso si se trata de posibles efectos adversos que no aparecen en este prospecto. También puede comunicarlos directamente a través del Sistema Español de Farmacovigilancia de Medicamentos de Uso Humano https:// www.notificaram.es. Mediante la comunicación de efectos adversos usted puede contribuir a proporcionar más información sobre la seguridad de este medicamento.
5. Conservación de aidessia
Mantener este medicamento fuera de la vista y del alcance de los niños.
No conservar a una temperatura superior a 30ºC. Conservar en el envase original para protegerlo de la luz.
No utilice este medicamento después de la fecha de caducidad que aparece en el envase, después de ‘CAD’. La fecha de caducidad es el último día del mes que se indica.
No utilice aidessia si observa un cambio de color, comprimidos rotos o cualquier signo visible de deterioro.
Los medicamentos no se deben tirar por los desagües ni a la basura. Deposite los envases y los medicamentos que no necesita en el Punto SIGRE de su farmacia. En caso de duda pregunte a su farmacéutico cómo deshacerse de los envases y de los medicamentos que no necesita. De esta forma, ayudará a proteger el medio ambiente.
6. Contenido del envase e información adicional
Composición de aidessia
- Los principios activos son: desogestrel y etinilestradiol. Cada comprimido contiene 0,150 miligramos de desogestrel y 0,030 miligramos de etinilestradiol.
- Los otros componentes son: lactosa monohidrato, almidón de maíz, povidona K-30 (E1201), alfa-tocoferol (E307), aceite de soja, sílice coloidal hidratada (E551), sílice coloidal anhidra (E551), ácido esteárico (E570), hipromelosa 2910 (E464), triacetina (E1518), polisorbato, dióxido de titanio (E171).
Aspecto de aidessiay contenido del envase
Comprimidos recubiertos con película, de color blanco, redondos y marcados con “C” en una cara y “7” en la otra.
Disponible en cajas de 1, 3, 6 y 13 blísteres, cada uno con 21 comprimidos.
Puede que solamente estén comercializados algunos tamaños de envases.
Titular de la autorización de comercialización
Laboratorios Cinfa, S.A.
Carretera Olaz-Chipi, 10 – Polígono Industrial Areta
31620 Huarte (Navarra)
España
Responsable de fabricación
Laboratorios León Farma, S.A.
Pol. Ind. Navatejera; La Vallina s/n,
24008 - Villaquilambre, León.
España
Este medicamento está autorizado en los estados miembros del Espacio Económico Europeo con los siguientes nombres:
Países Bajos: Ethinylestradiol/Desogestrel 0,03 mg/0,15 mg Focus, fimomhulde tabletten
Bélgica: Desolina 150/30 microgram, comprimé pelliculé
Luxemburgo Desolina 30 0,150 mg/0,030 mg, comprimés pelliculés
España: aidessia 0,15 mg/0,03 mg, comprimidos recubiertos con película EFG
Fecha de la última revisión de este prospecto:Marzo 2024
La información detallada y actualizada de este medicamento está disponible en la página Web de la Agencia Española de Medicamentos y Productos Sanitarios (AEMPS)http://www.aemps.gob.es/.
Puede acceder a información detallada y actualizada sobre este medicamento escaneando con su teléfono móvil (smartphone) el código QR incluido en prospecto y cartonaje. También puede acceder a esta información en la siguiente dirección de internet: https://cima.aemps.es/cima/dochtml/p/77783/P_77783.html
Código QR a: https://cima.aemps.es/cima/dochtml/p/77783/P_77783.html
- País de registro
- Precio medio en farmacia2.93 EUR
- Principio activo
- Requiere recetaSí
- Fabricante
- Esta información es de carácter general y no sustituye la consulta con un profesional sanitario.
- Alternativas a AIDESSIA 0,15 MG/0,03 MG COMPRIMIDOS RECUBIERTOS CON PELICULA EFGForma farmacéutica: COMPRIMIDO, 0,15 mg/0,02 mgPrincipio activo: desogestrel and ethinylestradiolFabricante: Laboratorios Cinfa S.A.Requiere recetaForma farmacéutica: COMPRIMIDO, 0,150/0,02 mg/mgPrincipio activo: desogestrel and ethinylestradiolFabricante: Gedeon Richter Plc.Requiere recetaForma farmacéutica: COMPRIMIDO, 150 mcg Desogestrel/30 mcg EtinilestradiolPrincipio activo: desogestrel and ethinylestradiolFabricante: Exeltis Healthcare S.L.Requiere receta
Médicos online para AIDESSIA 0,15 MG/0,03 MG COMPRIMIDOS RECUBIERTOS CON PELICULA EFG
Comenta la dosis, los posibles efectos secundarios, interacciones, contraindicaciones o la revisión de receta de AIDESSIA 0,15 MG/0,03 MG COMPRIMIDOS RECUBIERTOS CON PELICULA EFG, sujeto a valoración médica y a la normativa local.
Preguntas frecuentes






