

ROPSINE 2 mg/ml SOLUÇÃO INJETÁVEL

Pergunte a um médico sobre a prescrição de ROPSINE 2 mg/ml SOLUÇÃO INJETÁVEL

Como usar ROPSINE 2 mg/ml SOLUÇÃO INJETÁVEL
Introdução
Prospecto: informação para o utilizador
Ropsine2 mg/ml solução injetável EFG
Ropivacaína, hidrocloruro
Leia todo o prospecto atentamente antes de começar a usar o medicamento.
- Conserva este prospecto, pois pode ter que voltar a lê-lo.
- Se tiver alguma dúvida, consulte o seu médico ou farmacêutico.
- Este medicamento foi prescrito apenas para si, e não deve dá-lo a outras pessoas, mesmo que tenham os mesmos sintomas que si, pois pode prejudicá-las.
- Se experimentar efeitos adversos, consulte o seu médico ou farmacêutico, mesmo que se trate de efeitos adversos que não aparecem neste prospecto. Ver seção 4.
Conteúdo do prospecto:
- O que é Ropsine e para que é utilizado
- O que necessita saber antes de começar a usar Ropsine
- Como usar Ropsine
- Efeitos adversos possíveis
- Conservação de Ropsine
- Conteúdo do envase e informação adicional
1. O que é Ropsine e para que é utilizado
Ropsine contém o princípio ativo hidrocloruro de ropivacaína, que pertence a uma classe de medicamentos denominados anestésicos locais.
Ropsine 2 mg/ml solução injetável é utilizado em adultos e crianças de todas as idades para o tratamento da dor aguda. Insensibiliza (anestesia) uma parte do corpo, por exemplo, após cirurgia.
2. O que necessita saber antes de começar a usar Ropsine
Não useRopsine
- se é alérgico(hipersensível) ao hidrocloruro de ropivacaína, a qualquer outro anestésico de tipo amida ou a qualquer um dos outros componentes de Ropsine (incluídos na seção 6),
- se apresenta um volume de sangue diminuído(hipovolemia). Isso será medido por pessoal sanitário,
- para injetá-lo em um vaso sanguíneopara insensibilizar uma zona específica do seu corpo,
- para injetá-lo no colo do úteropara aliviar a dor durante o parto.
Advertências e precauções
Consulte o seu médico ou farmacêutico antes de começar a usar Ropsine
- Nas crianças recém-nascidas, pois são mais suscetíveis à Ropsine.
- Nas crianças menores de 12 anos, pois não se estabeleceu o uso de injeções de Ropsine com a finalidade de insensibilizar uma parte do corpo.
Deve ter um cuidado especial para evitar qualquer injeçãode Ropsine diretamente em um vaso sanguíneopara prevenir qualquer efeito tóxico imediato. A injeção não deve ser realizada em uma área inflamada.
Informar ao seu médico:
- se tem uma má condição geraldevido à idade ou a outros fatores,
- se tem problemas de coração(bloqueio da condução cardíaca parcial ou completa),
- se tem um problemade fígadoavançado,
- se tem problemasde rimseveros.
Informar ao seu médico se tem algum desses problemas, pois o seu médico deverá ajustar a dose de Ropsine.
Informar ao seu médico:
- se padece porfiria aguda(problemas com a geração dos pigmentos vermelhos do sangue, às vezes resulta em sintomas neurológicos).
Informar ao seu médico se você ou alguém da sua família padece porfiria, pois o seu médico pode necessitar utilizar outro anestésico.
Uso deRopsinecom outros medicamentos
Informar ao seu médico ou farmacêutico se está utilizando, utilizou recentemente ou pode ter que utilizar qualquer outro medicamento.
Deve ter precaução se está recebendo:
- Outros anestésicos locais(por exemplo, lidocaína) ou agentes estruturalmente relacionados com os anestésicos locais de tipo amida, por exemplo, certos medicamentos utilizados para tratar batimentos do coração irregulares (arritmia), tais como a mexiletina ou a amiodarona,
- Anestésicos geraisou opioides, tais como a morfina ou a codeína,
- Medicamentos utilizados para tratar a depressão(por exemplo, fluvoxamina),
- Certos antibióticos(por exemplo, enoxacina).
Gravidez e lactação
Se está grávida ou em período de lactação, acredita que possa estar grávida ou tem intenção de engravidar, consulte o seu médico ou farmacêutico antes de utilizar este medicamento. Desconhece-se se o hidrocloruro de ropivacaína afeta a gravidez ou se passa para o leite materno.
Condução e uso de máquinas
Ropsine pode produzir sonolência e afetar a velocidade das suas reações. Não conduza nem utilize ferramentas ou máquinas após tomar Ropsine, até o dia seguinte.
Consulte o seu médico ou farmacêutico se tiver dúvidas.
Informação importante sobre alguns dos componentes deRopsine
Este medicamento contém 3,39 mg de sódio (componente principal do sal de mesa/para cozinhar) em cada ml. Isso equivale a 0,2% da ingestão diária máxima de sódio recomendada para um adulto.
3. Como usar Ropsine
Método de administração
Ropsine será administrado pelo seu médico. Será administrado mediante uma injeção.
Dose
A dose recomendada dependerá de para que é utilizado e também da sua saúde, idade e peso.
Deve utilizar a dose mais pequena que possa produzir um efeito insensibilizador (anestesia) da zona requerida.
A dose usual
- para adultose adolescentes maiores de 12 anosestá entre 2 mg e 300 mgde hidrocloruro de ropivacaína.
- em lactentes e crianças(de 0 até os 12 anos, ambos incluídos)está entre 1-3 mg por cada quilogramade peso corporal.
Duração do tratamento
A administração de hidrocloruro de ropivacaína por lo geral dura entre2 e 10 horasem caso de anestesiaantes de certas cirurgias e pode tardar até 72 horasem caso de alívio da dordurante ou após a cirurgia.
Se lhe for administrada maisRopsinedo que deve
Os primeiros sintomas de que lhe foi administrada mais hidrocloruro de ropivacaína do que devia, normalmente são problemas relacionados com:
- ouvido e vista,
- adormecimento ao redor da boca,
- tonturas ou desmaios,
- formigamento,
- distúrbio do falar caracterizado por uma pobre articulação (disartria),
- rigidez muscular, espasmos musculares, ataques (convulsões),
- pressão arterial baixa,
- ritmo cardíaco lento ou irregular.
Estes sintomas podem preceder um paro cardíaco, paro respiratório ou convulsões graves.
Se você experimenta algum destes sintomas ou acredita que pode ter recebido demasiadaRopsine, informe ao seu médico ou pessoal sanitário imediatamente.
Em caso de toxicidade aguda, imediatamente serão tomadas as medidas corretivas apropriadas pelo pessoal sanitário.
Se tiver alguma outra dúvida sobre o uso deste produto, pergunte ao seu médico ou farmacêutico.
4. Efeitos adversos possíveis
Como todos os medicamentos, Ropsine pode produzir efeitos adversos, embora nem todas as pessoas os sofram.
Efeitos adversos importantes que se devem ter em conta:
As reações alérgicas repentinas e potencialmente mortais (p. ex., anafilaxia, incluído o choque anafilático) são raras e afetam de 1 a 10 pessoas de cada 10 000. Os possíveis sintomas incluem:
- início repentino de erupção, picazão ou habão (urticária);
- picazão ou erupção com inchação (urticária);
- inchação da face, dos lábios, da língua ou de outras partes do corpo;
- falta de ar, sibilância ou dificuldade para respirar;
- e uma sensação de perda da consciência.
Se acredita queRopsinelhe está provocando uma reação alérgica, informe ao seu médico ou pessoal sanitário imediatamente.
Outros efeitos adversos possíveis:
Muito frequentes(pode afetar mais de 1 de cada 10 pessoas)
- Pressão arterial baixa (hipotensão). Isso pode fazer com que se sinta tonto ou atordoado.
- Sensação de mal-estar (náuseas).
Frequentes(pode afetar até 1 de cada 10 pessoas)
- Dor de cabeça, formigamento (parestesias), sensação de tontura.
- Batimento do coração lento ou rápido (bradicardia, taquicardia).
- Pressão arterial alta (hipertensão).
- Sensação de mal-estar (vômitos).
- Dificuldades para urinar (retenção urinária).
- Dor de costas, temperatura alta, rigidez muscular.
Pouco frequentes(pode afetar até 1 de cada 100 pessoas)
- Ansiedade.
- Alguns sintomas podem aparecer se a injeção foi realizada por erro em um vaso sanguíneo, ou se lhe foi administrada mais Ropsine do que devia (ver também seção 3 “Se lhe for administrada mais Ropsine do que deve” anteriormente). Estes incluem ataques (convulsões, crises), sensação de tontura ou atordoamento, entumecimento dos lábios e ao redor da boca, entumecimento da língua, problemas de audição, problemas com a vista (visão), problemas com o falar (disartria), rigidez dos músculos e tremor, diminuição do sentido do tato (hipoestesia).
- Desmaio (síncope).
- Dificuldade ao respirar (dispnéia).
- Temperatura do corpo baixa.
Raros(pode afetar até 1 de cada 1000 pessoas)
- Ataque ao coração, batimento irregular do coração (arritmias).
Efeitos adversos possíveis observados com outros anestésicos locais que podem também ser produzidos porRopsineincluem:
- Entumecimento, devido à irritação dos nervos produzida pela agulha ou pela injeção. Isso, normalmente, não dura muito.
- Dano nos nervos. Raramente, pode produzir problemas permanentes.
- Se for administrada demasiada Ropsine no líquido espinal, pode adormecer todo o corpo (anestesiado).
Efeitos adversos adicionais em crianças
Em crianças, os efeitos adversos são os mesmos que em adultos, à exceção da pressão arterial baixa, que é menos frequente em crianças (afeta menos de 1 de cada 10 crianças) e sensação de mal-estar, que são mais frequentes em crianças (afetam mais de 1 de cada 10 crianças).
Se considera que algum dos efeitos adversos que sofre é grave ou se aprecia qualquer efeito adverso não mencionado neste prospecto, informe ao seu médico ou farmacêutico.
Comunicação de efeitos adversos
Se experimenta qualquer tipo de efeito adverso, consulte o seu médico ou farmacêutico, mesmo que se trate de possíveis efeitos adversos que não aparecem neste prospecto. Também pode comunicá-los diretamente através do Sistema Espanhol de Farmacovigilância de medicamentos de Uso Humano: https://www.notificaram.es. Mediante a comunicação de efeitos adversos, você pode contribuir para fornecer mais informações sobre a segurança deste medicamento.
5. Conservação de Ropsine
Mantenha este medicamento fora da vista e do alcance das crianças.
Não utilize Ropsine após a data de validade que aparece na ampola ou caixa. A data de validade é o último dia do mês que se indica.
Não congele.
Não utilize Ropsine se observar alguma precipitação na solução para injeção.
Normalmente, o seu médico ou o hospital conservarão Ropsine e são responsáveis pela qualidade do produto se, uma vez aberto, não for utilizado imediatamente. Também são responsáveis por descartar corretamente toda a Ropsine não utilizada.
Os medicamentos não devem ser jogados nos esgotos, nem na lixeira. Pergunte ao seu farmacêutico como se livrar dos envases e dos medicamentos que não precisa. Dessa forma, ajudará a proteger o meio ambiente.
6. Conteúdo do envase e informação adicional
Composição deRopsine
- O princípio ativo é hidrocloruro de ropivacaína 2 mg/ml. Cada ampola de polipropileno de 10 ml contém 20 mg de ropivacaína (como hidrocloruro).
Cada ampola de polipropileno de 20 ml contém 40 mg de ropivacaína (como hidrocloruro).
- Os demais componentes são cloruro de sódio, hidróxido de sódio (para o ajuste de pH) e água para preparações injetáveis.
Aspecto do produto e conteúdo do envase
Ropsine solução injetável é uma solução injetável aquosa transparente, incolor, estéril, isotónica, isobárica.
Ropsine 2 mg/ml solução injetável EFG está disponível em ampolas de 10 ml e 20 ml transparentes de polipropileno.
Tamanho do envase:
10 ampolas estéreis em blister de plástico.
Titular da autorização de comercialização e responsável pela fabricação
Titular da autorização de comercialização:
Sintetica GmbH
Albersloher Weg 11
48155 Münster
Alemanha
Responsável pela fabricação:
Sintetica GmbH
Albersloher Weg 11
48155 Münster
Alemanha
Data da última revisão deste prospecto: Setembro 2018
A informação detalhada e atualizada deste medicamento está disponível na página Web da Agência Española de Medicamentos e Produtos Sanitários (AEMPS) http://www.aemps.gob.es/.
-----------------------------------------------------------------------------------------------------------------------
Esta informação está destinada unicamente a médicos ou profissionais do setor sanitário:
Manipulação
Ropsine deve ser usado por, ou sob a supervisão de, médicos experientes em anestesia regional (ver seção 3)
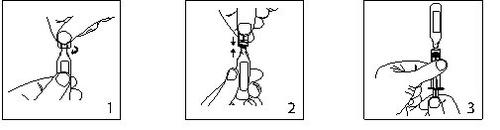
- Mantenha a ampola em posição vertical e gire o pescoço para eliminar qualquer resíduo de solução.
Abrir torcendo bruscamente a parte superior da ampola.
- A ampola pode ser conectada diretamente à seringa como se mostra na fig.2.
As ampolas se ajustam tanto às seringas Luerfit como às LuerLock.
- Segure a seringa com a ampola para cima. Sem apertar a ampola, retire a solução. Mantenha a pressão para baixo no êmbolo da seringa uma vez que a solução seja retirada e até que a ampola vazia seja descartada.
Período de validade antes da abertura
3 anos
Período de validade após a abertura
Desde o ponto de vista microbiológico, o produto deve ser empregado de forma imediata. Se não for utilizado imediatamente, a conservação durante a utilização e as condições antes de seu emprego são responsabilidade do usuário e geralmente não devem ultrapassar as 24 horas a 2-8ºC.
Os medicamentos Ropsine são produtos sem conservantes e estão destinados para um único uso. Descarte qualquer solução não utilizada.
O medicamento deve ser inspecionado visualmente antes de seu uso. A solução deve ser utilizada unicamente se a solução for transparente, praticamente livre de partículas e se o envase estiver intacto.
O envase intacto não deve ser re-introduzido no autoclave.
Posologia
Adultos e adolescentes maiores de 12 anos de idade
A tabela que se segue é uma guia sobre as doses mais habitualmente empregadas nos diferentes tipos de bloqueio. Deverá ser empregada a dose mais pequena requerida para produzir um bloqueio eficaz. A experiência clínica e o conhecimento da condição clínica do paciente são fatores importantes ao decidir a dose.
Indicação | Concentração mg/ml | Volume ml | Dose mg | Início da ação minutos | Duração horas |
Administração epidural lombar | |||||
Bolo | 2,0 | 10-20 | 20-40 | 10-15 | 0,5-1,5 |
Injeções intermitentes (repetidas) (por exemplo tratamento da dor no parto) | 2,0 | 10-15 (intervalo mínimo 30 minutos) | 20-30 | -- | -- |
Perfusão contínua por exemplo dor do parto | 2,0 | 6-10 ml/h | 12-20 mg/h | -- | -- |
Tratamento da dor pós-operatória | 2,0 | 6-14ml/h | 12-28 mg/h | -- | -- |
Administração epidural torácica | |||||
Perfusão contínua (tratamento da dor pós-operatória) | 2,0 | 6-14 ml/h | 12-28 mg/h | -- | -- |
Bloqueio periférico | |||||
(por exemplo bloqueio de nervos menores e infiltração) | 2,0 | 1-100 | 2,0-200 | 1-5 | 2-6 |
Bloqueio nervioso periférico (Bloqueio femoral ou interescaleno) | |||||
Perfusão contínua ou injeções intermitentes (por exemplo tratamento da dor pós-operatória) | 2,0 | 5-10 ml/h | 10-20 mg/h | -- | -- |
As doses expostas na tabela devem ser consideradas como recomendações de uso em adultos. Têm lugar variações individuais no início e duração da ação. As cifras da coluna “Dose” refletem o intervalo de dose promedio necessária esperado. Se consultará bibliografia adequada para os fatores que afetam as técnicas de bloqueio específicas e os requerimentos de cada um dos pacientes. |
Geralmente, a anestesia em cirurgia (por exemplo administração epidural) requer o uso de concentrações e doses mais altas. Para os processos quirúrgicos nos quais é necessário um bloqueio motor profundo, se recomenda a anestesia epidural empregando a formulação de Ropsine 10 mg/ml. Para a analgesia (por exemplo a administração epidural para o tratamento da dor aguda) se aconselham as concentrações e doses mais baixas.
Forma de administração
Administração perineural e epidural por injeção.
Antes e durante a injeção se recomenda realizar uma aspiração cuidadosa para prevenir uma injeção intravascular. Quando se vai injetar uma dose mais alta, se aconselha uma dose de teste 3-5 ml de lidocaína 2% (lignocaína) com adrenalina (epinefrina) 1:200.000. Uma injeção intravascular acidental pode ser reconhecida por um incremento temporário na frequência cardíaca e uma injeção intratecal acidental por sinais de bloqueio espinal.
Se realizará uma aspiração antes e durante a administração da dose principal, que se injetará de forma lenta ou em doses crescentes, a uma velocidade de 25-50 mg/minuto, enquanto se vigilam constantemente as funções vitais do paciente e se mantém o contato verbal com ele. Se aparecerem sintomas tóxicos, a administração do fármaco deverá ser interrompida imediatamente.
No bloqueio epidural para cirurgia, se empregaram doses únicas de até 250 mg de hidrocloruro de ropivacaína que foram bem toleradas.
No bloqueio do plexo braquial em um número limitado de pacientes se utilizou uma dose única de 300 mg que resultou ser bem tolerada.
Quando se requerem bloqueios prolongados, mediante uma perfusão contínua ou a administração em bolo repetida, deverá ter-se em conta os riscos de alcançar uma concentração plasmática tóxica ou a possibilidade de induzir lesão neural local. Doses acumuladas de até 675 mg de hidrocloruro de ropivacaína para cirurgia e analgesia pós-operatória administradas durante 24 horas foram bem toleradas em adultos, assim como as perfusões epidurais contínuas pós-operatórias a velocidades de até 28 mg/hora durante 72 horas. Em um número limitado de pacientes se administraram doses superiores de até 800 mg/dia com relativamente poucas reações adversas.
Para o tratamento da dor pós-operatória, se recomenda a seguinte técnica: A não ser que se inicie o tratamento com Ropivacaína previamente à intervenção, se induz um bloqueio epidural com esta a uma concentração de 7,5 mg/ml empregando um catéter epidural. A analgesia se mantém com uma perfusão de Ropsine 2 mg/ml. Velocidades de perfusão de 6-14 ml (12-28 mg) por hora proporcionam uma analgesia adequada com apenas um ligeiro e não progressivo bloqueio motor na maioria dos casos com dor pós-operatória e caráter de moderado a severo. A duração máxima do bloqueio epidural é de 3 dias. No entanto, deverá realizar-se um seguimento estreito do efeito analgésico com o fim de extrair o catéter tão pronto quanto a dor o permita. Com esta técnica se observou uma redução significativa da necessidade de utilizar opiáceos.
Em estudos clínicos, se administraram perfusões epidurais de 2 mg/ml de hidrocloruro de ropivacaína sozinho ou misturado com 1-4 μg/ml de fentanilo para o tratamento da dor pós-operatória durante um período de até 72 horas. Esta combinação de hidrocloruro de ropivacaína e fentanilo proporcionou um melhor alívio da dor mas causou efeitos secundários de tipo opiáceo; se investigou dita combinação apenas para hidrocloruro de ropivacaína 2 mg/ml.
Quando se aplicam bloqueios nerviosos periféricos prolongados, bem através de uma perfusão contínua ou mediante injeções repetidas, se devem considerar os riscos de alcançar uma concentração plasmática tóxica ou de induzir lesão neural local. Em estudos clínicos, se estabeleceu um bloqueio nervioso femoral com 300 mg de hidrocloruro de ropivacaína 7,5 mg/ml e um bloqueio interescaleno com 225 mg de hidrocloruro de ropivacaína 7,5 mg/ml, respectivamente, antes da cirurgia; mantendo-se então a analgesia com hidrocloruro de ropivacaína 2 mg/ml. Velocidades de perfusão ou injeções intermitentes de 10-20 mg por hora durante 48 horas, provocaram uma analgesia adequada e foram corretamente toleradas.
Pacientes pediátricos de0 até 12 anos de idade inclusive
Indicação | Concentração mg/ml | Volume ml/kg | Dose mg/kg |
Bloqueio epidural caudal único | 2,0 | 1 | 2 |
Bloqueios inferiores a T12, em crianças com um peso corporal de até 25 kg | |||
Perfusão epidural contínuaEm crianças com um peso corporal de até 25 kg | |||
0 até 6 meses | |||
Dose em bolo | 2,0 | 0,5-1 | 1-2 |
Perfusão de até 72 horas | 2,0 | 0,1 ml/kg/h | 0,2 mg/kg/h |
6 até 12 meses | |||
Dose em bolo | 2,0 | 0,5-1 | 1-2 |
Perfusão de até 72 horas | 2,0 | 0,2 ml/kg/h | 0,4 mg/kg/h |
1 a12 anos | |||
Dose em bolus | 2,0 | 1 | 2 |
Perfusão de até 72 horas | 2,0 | 0,2 ml/kg/h | 0,4 mg/kg/h |
As doses incluídas na tabela devem ser consideradas como diretrizes para o emprego em pediatria. Existem variações individuais. Em crianças com um peso corporal elevado, a menudo é necessária uma redução gradual da dose, que deverá basear-se no peso corporal ideal. O volume para o bloqueio epidural caudal único e o volume para as doses epidurais em bolo não devem ultrapassar os 25 ml em nenhum paciente. Se consultará bibliografia adequada em quanto aos fatores que afetam as técnicas de bloqueio específicas e aos requerimentos individuais do paciente. |
- Se recomenda empregar doses no limite inferior do intervalo de dose para os bloqueios epidurais torácicos, enquanto que para os bloqueios epidurais lombares ou caudais se recomenda administrar doses no limite superior.
- Recomendada para o bloqueio epidural lombar. É apropriado reduzir a dose em bolo para a analgesia epidural torácica.
Lactentes a partir de 1 ano e crianças de até 12 anos:
As doses de ropivacaína hidrocloruro propostas para o bloqueio do periférico em lactantes e crianças proporcionam diretrizes para o uso em crianças sem doença grave. Para crianças com doenças graves se recomenda uma dose mais conservadora e uma estreita monitorização.
As injeções únicas para o bloqueio nervioso periférico (por exemplo, bloqueio do nervo ilioinguinal, bloqueio do plexo braquial) não devem exceder de 2,5-3,0 mg / kg.
A perfusão contínua para bloqueio nervioso periférico se recomenda a 0,2-0,6 mg/kg/h (0,1-0,3 ml/kg/h) até as 72 h.
O emprego de hidrocloruro de ropivacaína em crianças prematuras não se documentou.
Forma de administração
Administração epidural por injeção.
Se recomenda uma aspiração cuidadosa antes e durante a injeção para prevenir a injeção intravascular. Se observarão estreitamente as funções vitais do paciente durante a injeção. Se se produzirem sintomas tóxicos, a injeção deverá ser interrompida imediatamente.
Uma injeção epidural caudal única de 2 mg/ml de hidrocloruro de ropivacaína produz uma analgesia pós-quirúrgica idónea por debaixo de T12 na maioria dos pacientes quando se emprega uma dose de 2 mg/kg em um volume de 1 ml/kg. Se pode ajustar o volume da injeção epidural caudal para obter uma distribuição diferente do bloqueio sensorial, tal como se recomenda na bibliografia. Se estudaram doses de até 3 mg/kg de uma concentração de hidrocloruro de ropivacaína de 3 mg/ml em crianças maiores de 4 anos; no entanto, esta concentração se associa a uma maior incidência de bloqueio motor.
Se recomenda fracionar a dose de anestésico local calculada, independentemente da via de administração.
Em caso que se recomende a infusão de hidrocloruro de ropivacaína, pode utilizar-se Ropsine solução injetável.
Incompatibilidades
Não se investigaram compatibilidades com outras soluções, por lo que este medicamento não deve ser misturado com outros medicamentos.
Pode produzir-se precipitação em soluções alcalinas já que o hidrocloruro de ropivacaína mostra escassa solubilidade a pH > 6,0.
Eliminação
A eliminação do medicamento não utilizado e de todos os materiais que tenham estado em contato com ele, se realizará de acordo com a normativa local.
- País de registo
- Substância ativa
- Requer receita médicaSim
- Fabricante
- Esta informação é apenas para referência e não constitui aconselhamento médico. Consulte sempre um médico antes de tomar qualquer medicamento. A Oladoctor não se responsabiliza por decisões médicas baseadas neste conteúdo.
- Alternativas a ROPSINE 2 mg/ml SOLUÇÃO INJETÁVELForma farmacêutica: INJETÁVEL, 100 mgSubstância ativa: ropivacaineFabricante: Altan Pharmaceuticals SaRequer receita médicaForma farmacêutica: PERFURAÇÃO INJETÁVEL, 2 mg/mlSubstância ativa: ropivacaineFabricante: Altan Pharmaceuticals SaRequer receita médicaForma farmacêutica: INJETÁVEL, 75 mgSubstância ativa: ropivacaineFabricante: Altan Pharmaceuticals SaRequer receita médica
Alternativas a ROPSINE 2 mg/ml SOLUÇÃO INJETÁVEL noutros países
As melhores alternativas com o mesmo princípio ativo e efeito terapêutico.
Alternativa a ROPSINE 2 mg/ml SOLUÇÃO INJETÁVEL em Polónia
Alternativa a ROPSINE 2 mg/ml SOLUÇÃO INJETÁVEL em Ukraine
Médicos online para ROPSINE 2 mg/ml SOLUÇÃO INJETÁVEL
Avaliação de posologia, efeitos secundários, interações, contraindicações e renovação da receita de ROPSINE 2 mg/ml SOLUÇÃO INJETÁVEL – sujeita a avaliação médica e regras locais.














