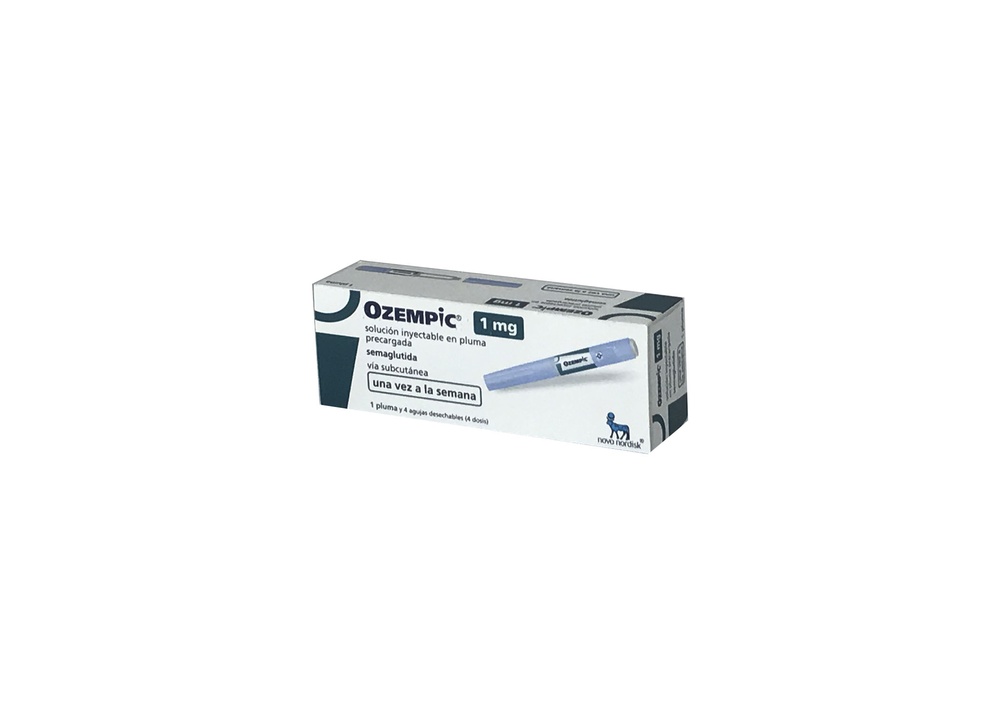
OZEMPIC 1 mg SOLUÇÃO INJETÁVEL EM CANETA PREENCHIDA
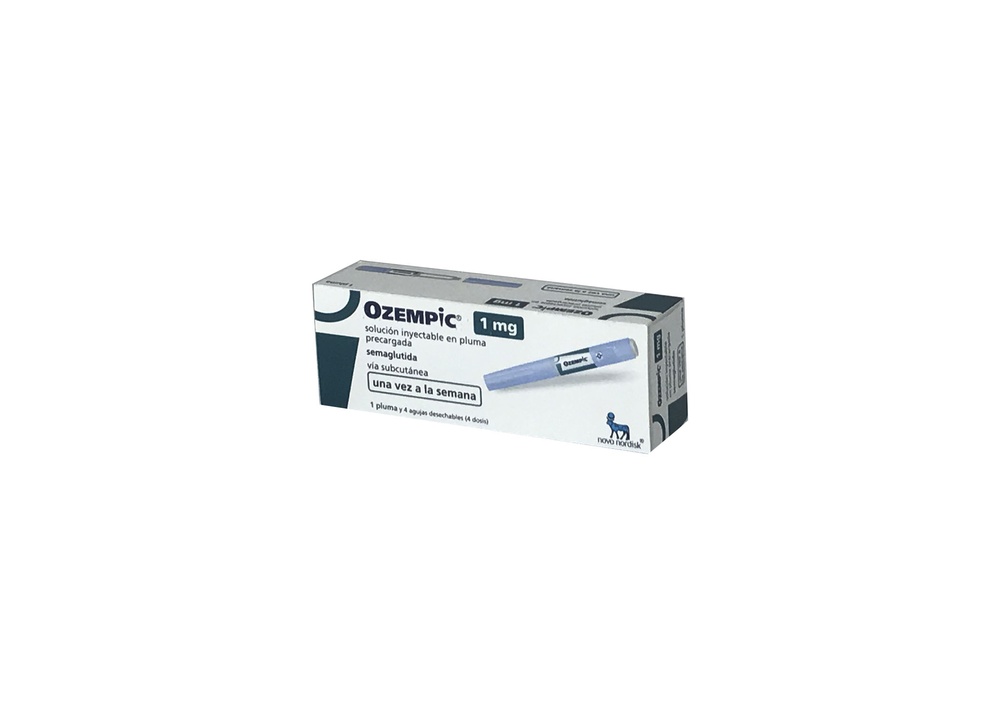
Pergunte a um médico sobre a prescrição de OZEMPIC 1 mg SOLUÇÃO INJETÁVEL EM CANETA PREENCHIDA

Como usar OZEMPIC 1 mg SOLUÇÃO INJETÁVEL EM CANETA PREENCHIDA
Introdução
Prospecto: informação para o paciente
Ozempic 1mg solução injetável em caneta pré-carregada
semaglutida
Leia todo o prospecto atentamente antes de começar a usar este medicamento, porque contém informações importantes para si.
- Conserva este prospecto, porque pode ter que relê-lo.
- Se tiver alguma dúvida, consulte o seu médico, farmacêutico ou enfermeiro.
- Este medicamento foi prescrito apenas para si, e não deve dá-lo a outras pessoas, mesmo que tenham os mesmos sintomas que si, porque pode prejudicá-las.
- Se experimentar efeitos adversos, consulte o seu médico, farmacêutico ou enfermeiro, mesmo que se trate de efeitos adversos que não aparecem neste prospecto. Ver seção 4.
Conteúdo do prospecto
- O que é Ozempic e para que é utilizado
- O que precisa saber antes de começar a usar Ozempic
- Como usar Ozempic
- Possíveis efeitos adversos
- Conservação de Ozempic
- Conteúdo do envase e informações adicionais
1. O que é Ozempic e para que é utilizado
Ozempic contém o princípio ativo semaglutida. Ajuda ao seu corpo a reduzir o nível de açúcar no sangue apenas quando este nível de açúcar está demasiado elevado e pode ajudar a prevenir uma doença cardíaca em pacientes com diabetes mellitus tipo 2 (DMT2). Também ajuda a retardar o deterioro da função renal em pacientes com DMT2 por meio de um mecanismo à parte da redução da glicemia.
Ozempic é utilizado para tratar adultos (a partir dos 18 anos de idade) com DMT2 quando a dieta e o exercício não são suficientes:
- como medicamento antidiabético único quando não pode utilizar metformina (outro medicamento para a diabetes) ou
- com outros medicamentos para a diabetes: quando estes não são suficientes para controlar os níveis de açúcar no sangue. Estes podem ser medicamentos que se tomam por via oral ou se injetam, como a insulina.
É importante que continue com a dieta e o plano de exercício que o seu médico, farmacêutico ou enfermeiro lhe indicou.
2. O que precisa saber antes de começar a usar Ozempic
Não use Ozempic
- se é alérgico a semaglutida ou a algum dos outros componentes deste medicamento (incluídos na seção 6).
Advertências e precauções
Consulte o seu médico, farmacêutico ou enfermeiro antes de começar a usar este medicamento.
Este medicamento não é o mesmo que a insulina e não deve usá-lo se:
- sofre de diabetes tipo 1, uma doença na qual o corpo não produz nada de insulina
- desenvolve cetoacidose diabética, uma complicação da diabetes que se caracteriza por um alto nível de açúcar no sangue, dificuldade para respirar, confusão, sede excessiva, hálito de odor doce ou sabor doce ou metálico na boca.
Ozempic não é uma insulina e, portanto, não se deve usá-lo como um substituto de insulina.
Se sabe que vai ser submetido a uma intervenção cirúrgica na qual será submetido a anestesia (estado de sono), informe o seu médico de que está tomando Ozempic.
Efeitos no sistema digestivo
Durante o tratamento com este medicamento, é possível que tenha náuseas, vômitos ou diarreia. Estes efeitos adversos podem causar desidratação (perda de líquidos). É importante que beba muito líquido para evitar a desidratação. Isso é especialmente importante se tiver problemas renais. Se tiver alguma dúvida, consulte o seu médico.
Dor de estômago intenso e contínuo que pode ser devido a pancreatite aguda
Se tiver uma dor intensa e contínua na zona do estômago, acuda ao médico imediatamente, porque pode ser um sintoma de pancreatite aguda (inflamação do pâncreas). Consulte a seção 4 para conhecer os sintomas de aviso da inflamação do pâncreas.
Nível baixo de açúcar no sangue (hipoglicemia)
A combinação de uma sulfonilureia ou insulina com este medicamento pode aumentar o risco de experimentar níveis baixos de açúcar no sangue (hipoglicemia). Consulte a seção 4 para conhecer os sintomas de aviso de um nível baixo de açúcar no sangue. É possível que o seu médico lhe peça que meça os níveis de açúcar no sangue. Isso ajudará o seu médico a decidir se é necessário mudar a dose de sulfonilureia ou insulina para reduzir o risco de nível baixo de açúcar no sangue.
Doença ocular diabética (retinopatia)
Se sofre de uma doença ocular diabética e está usando insulina, este medicamento pode provocar um pioramento da sua visão, pelo que pode precisar de tratamento. Informe o seu médico se sofre de doença ocular diabética ou experimenta problemas oculares durante o tratamento com este medicamento. No caso de ter doença ocular diabética potencialmente instável, não se recomenda o uso de Ozempic 2 mg.
Crianças e adolescentes
Este medicamento não é recomendado em crianças e adolescentes menores de 18 anos de idade, porque a segurança e eficácia não foram estabelecidas ainda nestes grupos de idade.
Outros medicamentos e Ozempic
Informe o seu médico, farmacêutico ou enfermeiro se está tomando, tomou recentemente ou pode ter que tomar qualquer outro medicamento, incluindo medicamentos à base de plantas ou outros medicamentos adquiridos sem receita.
Em particular, informe o seu médico, farmacêutico ou enfermeiro se está utilizando medicamentos que contenham algum dos seguintes componentes:
- Varfarina ou outros medicamentos semelhantes orais para reduzir a coagulação do sangue (anticoagulantes orais). Pode precisar de análises de sangue frequentes para verificar como o sangue coagula.
- Se está utilizando insulina, o seu médico lhe informará como reduzir a dose de insulina e lhe recomendará fazer seguimento dos níveis de açúcar no sangue de forma mais frequente, com o objetivo de evitar uma hiperglicemia (nível alto de açúcar no sangue) e cetoacidose diabética (uma complicação da diabetes que ocorre quando o corpo não pode decompor a glicose porque não há suficiente insulina).
Gravidez e amamentação
Se está grávida ou em período de amamentação, acha que pode estar grávida ou tem intenção de engravidar, consulte o seu médico antes de utilizar este medicamento.
Este medicamento não deve ser utilizado durante a gravidez, porque não se sabe se afeta o feto. Portanto, o uso de métodos anticoncepcionais é recomendado durante o uso deste medicamento. Se deseja engravidar, consulte com o seu médico sobre como mudar o tratamento, porque deve interromper o uso deste medicamento pelo menos 2 meses antes. Se engravidar enquanto usa este medicamento, consulte com o seu médico imediatamente, porque será necessário mudar o tratamento.
Não use este medicamento durante o período de amamentação, porque não se sabe se passa para o leite materno.
Condução e uso de máquinas
É pouco provável que Ozempic afete a sua capacidade de conduzir e utilizar máquinas. Se utiliza este medicamento em combinação com uma sulfonilureia ou insulina, é possível que experimente um nível baixo de açúcar no sangue (hipoglicemia), o que pode reduzir a sua capacidade de concentração. Não conduza ou use máquinas se experimentar algum sintoma de nível baixo de açúcar no sangue. Consulte a seção 2, “Advertências e precauções” para obter informações sobre o aumento do risco de experimentar um nível baixo de açúcar no sangue e a seção 4 para conhecer os sintomas de aviso de um nível baixo de açúcar no sangue. Consulte o seu médico para mais informações.
Conteúdo de sódio
Este medicamento contém menos de 1 mmol de sódio (23 mg) por dose; isto é, é essencialmente “isento de sódio”.
3. Como usar Ozempic
Siga exatamente as instruções de administração deste medicamento indicadas pelo seu médico. Em caso de dúvida, consulte novamente o seu médico, farmacêutico ou enfermeiro.
Quanto usar
- A dose inicial é 0,25 mg uma vez por semana durante quatro semanas.
- Depois de quatro semanas, o seu médico aumentará a dose para 0,5 mg uma vez por semana.
- É possível que o seu médico aumente a dose para 1 mg uma vez por semana se o nível de açúcar no sangue não estiver controlado adequadamente com uma dose de 0,5 mg uma vez por semana.
- É possível que o seu médico aumente a dose para 2 mg uma vez por semana se o nível de açúcar no sangue não estiver controlado adequadamente com uma dose de 1 mg uma vez por semana.
Não mude a dose a menos que o seu médico o indique.
Como administrar Ozempic
Ozempic é administrado como uma injeção sob a pele (injeção subcutânea). Não se injeta em uma veia nem em um músculo.
- As melhores zonas para a injeção são a parte frontal da coxa, a parte frontal da cintura (abdomen) ou a parte superior do braço.
- Antes de utilizar a caneta pela primeira vez, o seu médico ou enfermeiro lhe mostrará como utilizá-la.
No outro lado deste prospecto, encontrará instruções detalhadas sobre o seu uso.
Quando usar Ozempic
- Deve usar este medicamento uma vez por semana, no mesmo dia da semana, se possível.
- Pode colocar a injeção a qualquer momento do dia, independentemente das refeições.
Para ajudá-lo a lembrar que se injeta este medicamento apenas uma vez por semana, é conveniente que anote na caixa o dia da semana escolhido (por exemplo, quarta-feira), bem como a data de cada vez que o injeta.
Se necessário, pode mudar o dia da injeção semanal deste medicamento, desde que tenham passado pelo menos 3 dias desde a última injeção. Uma vez selecionado o novo dia de administração, deve prosseguir com o esquema de dosificação semanal.
Se usar mais Ozempic do que deve
Se usar mais Ozempic do que deve, consulte o seu médico imediatamente. É possível que experimente efeitos adversos como náuseas.
Se esquecer de usar Ozempic
Se esquecer de se injetar uma dose e:
- passaram 5 dias ou menos desde que deveria ter usado Ozempic, use-o assim que se lembrar. Depois, administre a próxima dose como de costume, no dia programado.
- passaram mais de 5 dias desde que deveria ter usado Ozempic, salte a dose esquecida. Depois, administre a próxima dose como de costume, no dia programado.
Não use uma dose dupla para compensar a dose esquecida.
Se interromper o tratamento com Ozempic
Não interrompa o tratamento com este medicamento sem consultar o seu médico. Se o interromper, pode que aumentem os níveis de açúcar no sangue.
Se tiver alguma outra dúvida sobre o uso deste medicamento, pergunte ao seu médico, farmacêutico ou enfermeiro.
4. Possíveis efeitos adversos
Como todos os medicamentos, este medicamento pode produzir efeitos adversos, embora nem todas as pessoas os sofram.
Efeitos adversos graves
Frequentes(podem afetar até 1 de cada 10 pessoas)
- complicações da doença ocular diabética (retinopatia); se tiver problemas oculares, como mudanças na visão durante o tratamento com este medicamento, deve comunicá-los ao seu médico.
Pouco frequentes(podem afetar até 1 de cada 100 pessoas)
- Pâncreas inflamado (pancreatite aguda) que pode causar uma dor intensa que não desaparece no estômago e nas costas. Se apresentar tais sintomas, acuda imediatamente ao médico.
Raros(podem afetar até 1 de cada 1.000 pessoas)
- reações alérgicas graves (reações anafiláticas, angioedema). Deve obter ajuda médica e informar o seu médico imediatamente se experimentar sintomas como problemas respiratórios, inchaço do rosto, lábios, língua e/ou garganta com dificuldade para engolir e palpitações.
Frequência não conhecida(não pode ser estimada a partir dos dados disponíveis)
- Obstrução intestinal. Uma forma grave de constipação com outros sintomas como dor de estômago, inchaço abdominal, vômitos, etc.
Outros efeitos adversos
Muito frequentes(podem afetar mais de 1 de cada 10 pessoas)
- náuseas; este efeito desaparece normalmente com o tempo
- diarreia; este efeito desaparece normalmente com o tempo
- nível baixo de açúcar no sangue (hipoglicemia) quando este medicamento é usado com medicamentos que contêm sulfonilureia ou insulina
Frequentes(podem afetar até 1 de cada 10 pessoas)
- vômitos
- nível baixo de açúcar no sangue (hipoglicemia), quando este medicamento é usado com medicamentos orais para a diabetes que não sejam sulfonilureias ou insulina
Os sintomas de aviso de um nível baixo de açúcar no sangue podem aparecer repentinamente. Alguns destes sintomas são: suor frio, pele fria e pálida, dor de cabeça, palpitações, náuseas ou apetite excessivo, mudanças na visão, sonolência ou sensação de fraqueza, nervosismo, ansiedade ou confusão, dificuldade de concentração ou tremores.
O seu médico lhe indicará como tratar o nível baixo de açúcar no sangue e o que tem que fazer no caso de observar estes sintomas de aviso.
Este nível baixo de açúcar no sangue é mais provável que ocorra se também utilizar uma sulfonilureia ou insulina. Pode que o seu médico reduza a dose destes medicamentos antes de começar a usar este medicamento.
- indigestão
- estômago inflamado (gastrite); os sintomas incluem dor de estômago, náuseas ou vômitos
- refluxo ou ardor de estômago; também se denomina “doença de refluxo gastroesofágico” (ERGE)
- dor de estômago
- inchaço de estômago
- constipação
- arrotos
- pedras na vesícula
- tontura
- cansaço
- perda de peso
- diminuição do apetite
- gases (flatulência)
- aumento das enzimas pancreáticas (como lipase e amilase)
- dor de cabeça.
Pouco frequentes(podem afetar até 1 de cada 100 pessoas)
- mudanças no sabor das comidas e bebidas
- pulso rápido
- reações no local da injeção, como hematomas, dor, irritação, picazón e erupção cutânea
- reações alérgicas como erupção cutânea, picazón ou urticária
- um atraso no esvaziamento do estômago.
Comunicação de efeitos adversos
Se experimentar qualquer tipo de efeito adverso, consulte o seu médico, farmacêutico ou enfermeiro, mesmo que se trate de possíveis efeitos adversos que não aparecem neste prospecto. Também pode comunicá-los diretamente através do sistema nacional de notificação incluído no Apêndice V. Mediante a comunicação de efeitos adversos, você pode contribuir para fornecer mais informações sobre a segurança deste medicamento.
5. Conservação de Ozempic
Mantenha este medicamento fora da vista e do alcance das crianças.
Não use este medicamento após a data de validade que aparece na etiqueta da caneta e no envase após CAD. A data de validade é o último dia do mês que se indica.
Antes de abrir:
Conservar na geladeira (entre 2 °C e 8 °C). Não congelar. Manter longe do componente de refrigeração da geladeira. Conservar a caneta com o capuchão colocado para protegê-la da luz.
Depois da primeira abertura:
Ozempic 1 mg (caneta de 4 doses)
- Pode conservar a caneta durante 6 semanas se for armazenada abaixo de 30 °C ou na geladeira (entre 2 °C e 8 °C), longe do componente de refrigeração da geladeira. Não congelar Ozempic e não utilize se foi congelado.
Ozempic 1 mg (caneta de 8 doses)
- Pode conservar a caneta durante 8 semanas se for armazenada abaixo de 30 °C ou na geladeira (entre 2 °C e 8 °C), longe do componente de refrigeração da geladeira. Não congelar Ozempic e não utilize se foi congelado.
- Quando não for utilizado, conservar a caneta com o capuchão colocado para protegê-la da luz.
Não use este medicamento se observar que a solução não é transparente e incolor ou quase incolor.
Os medicamentos não devem ser jogados nos esgotos nem na lixeira. Pergunte ao seu farmacêutico como se livrar dos envases e dos medicamentos que já não precisa. Dessa forma, ajudará a proteger o meio ambiente.
6. Conteúdo do frasco e informações adicionais
Composição de Ozempic
- O princípio ativo é semaglutida.
- 1 ml de solução injetável contém 1,34 mg de semaglutida. Uma caneta pré-carregada contém 4 mg de semaglutida em 3 ml de solução. Cada dose contém 1 mg de semaglutida em 0,74 ml.
- 1 ml de solução injetável contém 2,68 mg de semaglutida. Uma caneta pré-carregada contém 8 mg de semaglutida em 3 ml de solução. Cada dose contém 1 mg de semaglutida em 0,37 ml.
- Os outros componentes são: fosfato dissódico di-hidratado, propilenoglicol, fenol, água para preparações injetáveis, hidróxido de sódio/ácido clorídrico (para ajuste do pH). Consulte também a seção 2 “Conteúdo de sódio”.
Aspecto do produto e conteúdo do frasco
Ozempic é uma solução injetável transparente e incolor ou quase incolor em uma caneta pré-carregada.
Cada caneta pré-carregada contém 3 ml de solução, podendo administrar 4 doses de 1 mg.
Cada caneta pré-carregada contém 3 ml de solução, podendo administrar 8 doses de 1 mg.
Ozempic 1 mg solução injetável está disponível nos seguintes tamanhos de embalagem:
1 caneta e 4 agulhas descartáveis NovoFine Plus.
1 caneta e 8 agulhas descartáveis NovoFine Plus.
3 canetas e 12 agulhas descartáveis NovoFine Plus.
Pode ser que apenas alguns tamanhos de embalagens estejam comercializados.
Título da autorização de comercialização
Novo Nordisk A/S
Novo Allé
DK-2880 Bagsværd
Dinamarca
Responsável pela fabricação
Ozempic 1 mg (4 e 8 doses)
Novo Nordisk A/S
Novo Allé
DK-2880 Bagsværd
Dinamarca
Ozempic 1 mg (4 doses)
Novo Nordisk Production SAS
45, Avenue d’Orléans
28000 Chartres
França
Data da última revisão deste prospecto:
Outras fontes de informação
A informação detalhada deste medicamento está disponível no site da Agência Europeia de Medicamentos: http://www.ema.europa.eu.
Instruções de uso
Ozempic 1mg solução injetável em caneta pré-carregada podendo administrar 4 doses
semaglutida
Instruções de uso de Ozempic 1mg solução injetável em caneta pré-carregada | |
Leia atentamente estas instruçõesantes de utilizar sua caneta pré-carregada Ozempic. Pergunte ao seu médico, enfermeiro ou farmacêutico como injetar Ozempic corretamente. Comece verificando a caneta para certificar-se de que contém Ozempic1mge depois observe as seguintes imagens para familiarizar-se com as diferentes partes da caneta e da agulha. Se você é cego ou tem visão reduzida e não pode ler o contador de dose da caneta, não use esta caneta sem ajuda.Busque ajuda de uma pessoa que veja bem e saiba como usar a caneta pré-carregada Ozempic. Sua caneta é uma caneta pré-carregada dosificadora. Contém 4 mg de semaglutida e pode selecionar apenas doses de 1 mg. Uma caneta não usada contém quatro doses de 1 mg. Use a tabela que se encontra dentro da tampa da caixa para registrar quantas injeções você deu e quando as deu. A caneta está projetada para ser usada com agulhas descartáveis de 30G, 31G e 32G de até 8 mm de comprimento. A embalagem inclui agulhas NovoFine Plus. |
|
Informação importante Preste atenção especial a estas notas, pois são importantes para o uso seguro da caneta. | |
| |
|
|
|
|
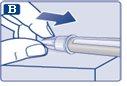
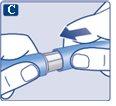
Verifique se a língua de papel e o capuchinho exterior da agulha não apresentam danos que possam afetar a esterilidade. Se observar qualquer dano, use uma agulha nova.
|
|
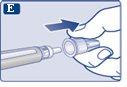
Certifique-se de colocar a agulha corretamente.
|
|
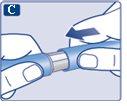
A agulha está coberta por dois capuchinhos. Você deve remover ambos os capuchinhos.Se esquecer de remover ambos os capuchinhos, nãoinjetará solução.
|
|
Pode aparecer uma gota de solução na ponta da agulha. Isso é normal, mas, apesar disso, você deve verificar o fluxo se for uma caneta nova e for a primeira vez que a usa. Consulte o passo 2 “Verificação do fluxo com cada caneta nova”. Nunca coloque uma agulha novana caneta até que esteja pronto para se injetar. |
|
Use sempre uma agulha nova para cada injeção. Isso pode evitar que as agulhas fiquem entupidas, contaminação, infecção e dosagem inexata. | |
Nunca use uma agulha dobrada ou danificada. | |
| |
|
|
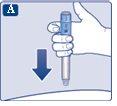
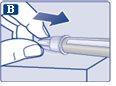
Pressione e mantenha pressionado o botãoaté que o contador de dose volte a ‘0’. O ‘0’ deve estar alinhado com o marcador de dose. Uma gota de solução deve aparecer na ponta da agulha. |
|
Pode ser que uma pequena gota fique na ponta da agulha, mas não será injetada. Se nenhuma gota aparecer,repita o passo 2 “Verificação do fluxo com cada caneta nova” um máximo de 6 vezes. Se ainda nenhuma gota for vista, troque a agulha e repita o passo 2 “Verificação do fluxo com cada caneta nova” uma vez mais. Descarte a caneta e use uma nova se, apesar de tudo, nenhuma gota de solução aparecer. | |
Certifique-se sempre de que uma gotaapareça na ponta da agulha antes de usar uma caneta nova pela primeira vez. Isso garante que a solução flui. Se nenhuma gota aparecer, nãose injetará medicamento, embora o contador de dose se mova. Isso pode indicar que a agulha está obstruída ou danificada. Se você não verificar o fluxo antes da primeira injeção com cada caneta nova, é possível que não receba a dose prescrita nem obtenha o efeito previsto de Ozempic. | |
| |
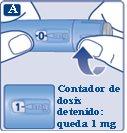
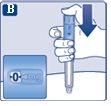
Continue girando até que o contador de dose pare e mostre 1 mg. |
|
Apenas o contador de dose e o marcador de dose mostrarão que 1 mg foi selecionado. Você só pode selecionar 1 mg por dose. Quando sua caneta contiver menos de 1 mg, o contador de dose parará antes de mostrar um 1. O seletor de dose emite um clique diferente quando gira para a frente, para trás ou ultrapassa 1 mg. Não conte os cliques da caneta. | |
Antes de se injetar este medicamento, use sempre o contador de dose e o marcador de dose para verificar que selecionou 1mg. Não conte os cliques da caneta. Devem ser selecionadas apenas doses de 1mg com o seletor de dose.1 mg deve estar alinhado exatamente com o marcador de dose para garantir que você recebe a dose correta. | |
Quanto de solução resta | |
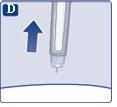
Se mostrar 1, resta ao menos 1mgna caneta. Se o contador de dose parar antes de 1mg,não resta solução suficiente para uma dose completa de 1 mg. |
|
Se não restar solução suficiente na caneta para uma dose completa, não a use. Em vez disso, use uma nova caneta Ozempic. | |
| |
|
|
|
|
|
|
Se aparecer sangue no local de injeção, pressione levemente. |
|
Pode aparecer uma gota de solução na ponta da agulha após a injeção. Isso é normal e não afeta sua dose. | |
Como detectar se a agulha está obstruída ou danificada
O que fazer se a agulha está obstruída Troque a agulha como descrito no passo 5 “Após a injeção” e repita todos os passos desde o passo 1 “Preparação da caneta com uma agulha nova”. Certifique-se de selecionar a dose completa que precisa. Nunca toque o contador de dose durante a injeção.Isso pode interromper a injeção. | |
| |
Descarte sempre a agulha após cada injeçãopara garantir que as injeções sejam administradas corretamente e evitar que as agulhas fiquem entupidas. Se a agulha estiver obstruída, nãose injetará nada de medicamento.
|
|
|
|
|
|
Quando a caneta estiver vazia, descarte-a sema agulha, seguindo as instruções do seu médico, enfermeiro, farmacêutico ou autoridades locais. | |
Nunca tente colocar novamente o capuchinho interior na agulha.Pode se picar com a agulha. Retire sempre a agulha da caneta imediatamente após cada injeção. Isso pode evitar que as agulhas fiquem entupidas, contaminação, infecção, perda de solução e dosagem inexata. | |
Outra informação importante | |
| |
Manutenção da sua caneta | |
Trate a caneta com cuidado. A manipulação brusca ou o uso indevido podem causar uma dosagem inexata. Se isso acontecer, é possível que não obtenha o efeito previsto deste medicamento. | |
|
Instruções de uso
Ozempic 1mg solução injetável em caneta pré-carregada podendo administrar 8 doses
semaglutida
Instruções de uso de Ozempic 1mg solução injetável em caneta pré-carregada | |
Leia atentamente estas instruçõesantes de utilizar sua caneta pré-carregada Ozempic. Pergunte ao seu médico, enfermeiro ou farmacêutico como injetar Ozempic corretamente. Comece verificando a caneta para certificar-se de que contém Ozempic1mge depois observe as seguintes imagens para familiarizar-se com as diferentes partes da caneta e da agulha. Se você é cego ou tem visão reduzida e não pode ler o contador de dose da caneta, não use esta caneta sem ajuda.Busque ajuda de uma pessoa que veja bem e saiba como usar a caneta pré-carregada Ozempic. Sua caneta é uma caneta pré-carregada dosificadora. Contém 8 mg de semaglutida e pode selecionar apenas doses de 1 mg. Uma caneta não usada contém oito doses de 1 mg. Após ter se injetado as doses previstas, ainda restará solução na caneta. A caneta deve ser descartada. Use a tabela que se encontra dentro da tampa da caixa para registrar quantas injeções você deu e quando as deu. A caneta está projetada para ser usada com agulhas descartáveis de 30G, 31G e 32G de até 8 mm de comprimento. A embalagem inclui agulhas NovoFine Plus. |
|
Informação importante Preste atenção especial a estas notas, pois são importantes para o uso seguro da caneta. | |
| |
|
|
|
|
Verifique que a língua de papel e o capuchão exterior da agulha não apresentam danos que possam afetar a esterilidade. Se observar qualquer dano, use uma agulha nova.
|
|
Certifique-se de colocar a agulha corretamente.
|
|
A agulha está coberta por dois capuchões. Deve remover ambos os capuchões.Se esquecer de remover ambos os capuchões, nãoinjetará solução.
|
|
Pode aparecer uma gota de solução na ponta da agulha. Isso é normal, mas, apesar disso, você deve verificar o fluxo se for uma caneta nova e for a primeira vez que a utiliza. Consulte o passo 2 “Verificação do fluxo com cada caneta nova”. Não coloque uma agulha novana caneta até que esteja pronto para se aplicar a injeção. |
|
Use sempre uma agulha nova para cada injeção. Isso pode evitar que as agulhas se obstruam, contaminação, infecção e dosagem inexata. | |
Nunca use uma agulha dobrada ou danificada. | |
| |
|
|
Pressione e mantenha pressionado o botãoaté que o contador de dose volte a ‘0’. O ‘0’ deve estar alinhado com o marcador de dose. Uma gota de solução deve aparecer na ponta da agulha. |
|
Pode ser que uma pequena gota fique na ponta da agulha, mas não se injetará. Se nenhuma gota aparecer,repita o passo 2 “Verificação do fluxo com cada caneta nova” um máximo de 6 vezes. Se ainda não vir nenhuma gota, troque a agulha e repita o passo 2 “Verificação do fluxo com cada caneta nova” uma vez mais. Descarte a caneta e use uma nova se, apesar de tudo, nenhuma gota de solução aparecer. | |
Certifique-se sempre de que apareça uma gotana ponta da agulha antes de usar uma caneta nova pela primeira vez. Isso garante que a solução flui. Se nenhuma gota aparecer, nãose injetará medicamento, embora o contador de dose se mova. Isso pode indicar que a agulha está obstruída ou danificada. Se não verificar o fluxo antes da primeira injeção com cada caneta nova, é possível que não receba a dose prescrita nem alcance o efeito previsto de Ozempic. | |
| |
Continue girando até que o contador de dose pare e mostre 1 mg. |
|
Apenas o contador de dose e o marcador de dose mostrarão que se selecionou 1 mg. Você só pode selecionar 1 mg por dose. Quando sua caneta contiver menos de 1 mg, o contador de dose parará antes de mostrar um 1. O seletor de dose emite um clique diferente quando gira para a frente, para trás ou ultrapassa 1 mg. Não conte os cliques da caneta. | |
Antes de se injetar este medicamento, use sempre o contador de dose e o marcador de dose para ver que selecionou 1mg. Não conte os cliques da caneta. Devem ser selecionadas apenas doses de 1mg com o seletor de dose.1 mg deve estar alinhado de maneira exata com o marcador de dose para garantir que você recebe a dose correta. | |
Quanta solução resta | |
Se mostrar 1, resta ao menos 1mgna caneta. Se o contador de dose parar antes de 1mg,não resta solução suficiente para uma dose completa de 1 mg. |
|
Se não restar solução suficiente na caneta para uma dose completa, não a use. Em vez disso, use uma nova caneta Ozempic. | |
| |
|
|
|
|
|
|
Se aparecer sangue no local de injeção, pressione levemente. |
|
Pode aparecer uma gota de solução na ponta da agulha após a injeção. Isso é normal e não afeta sua dose. | |
Como detectar se a agulha está obstruída ou danificada
O que fazer se a agulha está obstruída Troque a agulha como descrito no passo 5 “Depois da injeção” e repita todos os passos desde o passo 1 “Preparação da caneta com uma agulha nova”. Certifique-se de selecionar a dose completa que precisa. Nunca toque o contador de dose durante a injeção.Isso pode interromper a injeção. | |
| |
Descarte sempre a agulha após cada injeçãopara garantir que as injeções sejam administradas corretamente e evitar que as agulhas se obstruam. Se a agulha estiver obstruída, nãose injetará nada de medicamento.
|
|
|
|
|
|
Quando a caneta estiver vazia, descarte-a sema agulha, seguindo as instruções de seu médico, enfermeiro, farmacêutico ou autoridades locais. | |
Nunca tente colocar novamente o capuchão interior na agulha.Pode se picar com a agulha. Retire sempre a agulha da caneta imediatamente após cada injeção. Isso pode evitar que as agulhas se obstruam, contaminação, infecção, perda de solução e dosagem inexata. | |
Outra informação importante | |
| |
Manutenção de sua caneta | |
Trate a caneta com cuidado. A manipulação brusca ou o uso indevido podem causar uma dosagem inexata. Se isso acontecer, é possível que não alcance o efeito previsto deste medicamento. | |
|

Quanto custa o OZEMPIC 1 mg SOLUÇÃO INJETÁVEL EM CANETA PREENCHIDA em Espanha em 2025?
O preço médio do OZEMPIC 1 mg SOLUÇÃO INJETÁVEL EM CANETA PREENCHIDA em dezembro de 2025 é de cerca de 128.15 EUR. Os valores podem variar consoante a região, a farmácia e a necessidade de receita. Confirme sempre com uma farmácia local ou fonte online para obter informações atualizadas.
- País de registo
- Preço médio em farmácia128.15 EUR
- Substância ativa
- Requer receita médicaSim
- Fabricante
- Esta informação é apenas para referência e não constitui aconselhamento médico. Consulte sempre um médico antes de tomar qualquer medicamento. A Oladoctor não se responsabiliza por decisões médicas baseadas neste conteúdo.
- Alternativas a OZEMPIC 1 mg SOLUÇÃO INJETÁVEL EM CANETA PREENCHIDAForma farmacêutica: INJETÁVEL, 0,25 mgSubstância ativa: semaglutideFabricante: Novo Nordisk A/SRequer receita médicaForma farmacêutica: INJETÁVEL, 0.5 mgSubstância ativa: semaglutideFabricante: Novo Nordisk A/SRequer receita médicaForma farmacêutica: COMPRIMIDO, 1,5 mgSubstância ativa: semaglutideFabricante: Novo Nordisk A/SRequer receita médica
Alternativas a OZEMPIC 1 mg SOLUÇÃO INJETÁVEL EM CANETA PREENCHIDA noutros países
As melhores alternativas com o mesmo princípio ativo e efeito terapêutico.
Alternativa a OZEMPIC 1 mg SOLUÇÃO INJETÁVEL EM CANETA PREENCHIDA em Ukraine
Médicos online para OZEMPIC 1 mg SOLUÇÃO INJETÁVEL EM CANETA PREENCHIDA
Avaliação de posologia, efeitos secundários, interações, contraindicações e renovação da receita de OZEMPIC 1 mg SOLUÇÃO INJETÁVEL EM CANETA PREENCHIDA – sujeita a avaliação médica e regras locais.