LUCENTIS 10 mg/ml Solução injetável em seringa pré-carregada

Pergunte a um médico sobre a prescrição de LUCENTIS 10 mg/ml Solução injetável em seringa pré-carregada

Como usar LUCENTIS 10 mg/ml Solução injetável em seringa pré-carregada
Introdução
Prospecto:informação para o paciente
Lucentis 10mg/ml solução injetável em seringa pré-carregada
ranibizumab
Leia todo o prospecto detenidamente antes deque lhe administrem este medicamento, porque contém informações importantes para si.
- Conserva este prospecto, porque pode ter que voltar a lê-lo.
- Se tiver alguma dúvida, consulte o seu médico.
- Se experimentar efeitos adversos, consulte o seu médico, mesmo que se trate de efeitos adversos que não aparecem neste prospecto. Ver secção 4.
Conteúdo do prospecto
- O que é Lucentis e para que é utilizado
- O que precisa saber antes de que lhe administrem Lucentis
- Como é administrado Lucentis
- Posíveis efeitos adversos
- Conservação de Lucentis
- Conteúdo do envase e informações adicionais
1. O que é Lucentis e para que é utilizado
O que é Lucentis
Lucentis é uma solução que se injeta no olho. Lucentis pertence a um grupo de medicamentos denominados agentes anti-angiogénese. Contém o princípio ativo denominado ranibizumab.
Para que é utilizado Lucentis
Lucentis é utilizado em adultos para tratar várias doenças oculares que causam alteração da visão.
Estas doenças são o resultado de uma lesão na retina (camada sensível à luz na parte posterior do olho) provocada por:
- O crescimento de vasos sanguíneos anormais, que perdem líquido. Isto é observado em doenças como a degeneração macular associada à idade (DMAI) e a retinopatia diabética proliferativa (RDP, uma doença provocada pelo diabetes). Também pode estar associado à neovascularização coroide (NVC) devida à miopia patológica (MP), estrías angioides, corioretinopatia serosa central ou NVC inflamatória.
- Edema macular (inchação do centro da retina). A causa desta inchação pode ser o diabetes (uma doença conhecida como edema macular diabético (EMD)) ou um bloqueio das veias retinianas da retina (uma doença conhecida como oclusão da veia da retina (OVR)).
Como actua Lucentis
Lucentis reconhece e une-se de forma específica a uma proteína denominada factor de crescimento endotelial vascular A (VEGF-A) humano presente nos olhos. Em excesso, o VEGF-A causa o crescimento de vasos sanguíneos anormais e inchação no olho que pode ocasionar uma alteração da visão em doenças como DMAI, EMD, RDP, OVP, MP e NVC. Mediante a união ao VEGF-A, Lucentis pode impedir que actue e prevenir dito crescimento e inchação anormais.
Nestas doenças, Lucentis pode ajudar a estabilizar e, em muitos casos, melhorar a sua visão.
2. O que precisa saber antes de que lhe administrem Lucentis
Não lhe devem administrar Lucentis
- Se é alérgico ao ranibizumab ou a algum dos outros componentes deste medicamento (incluídos na secção 6).
- Se tem uma infecção no olho ou à volta do mesmo.
- Se tem dor ou vermelhidão (inflamação intraocular grave) no olho.
Advertências e precauções
Consulte o seu médico antes de que lhe administrem Lucentis
- Lucentis é administrado mediante uma injeção no olho. Ocasionalmente, após o tratamento com Lucentis pode aparecer uma infecção na parte interna do olho, dor ou vermelhidão (inflamação), desprendimento ou desgarro de uma das camadas situadas no fundo do olho (desprendimento ou desgarro da retina e desprendimento ou desgarro do epitélio pigmentário da retina), ou enturbiação do cristalino (catarata). É importante identificar e tratar tal infecção ou desprendimento de retina o mais cedo possível. Informe imediatamente o seu médico se nota sinais como dor no olho ou aumento das molestias no olho, se piora a vermelhidão no olho, visão borrosa ou diminuição da visão, um aumento do número de pequenas manchas na visão ou aumento da sensibilidade à luz.
- Em alguns pacientes, após a injeção a pressão no olho pode aumentar durante um curto período de tempo. É possível que você não se aperceba disso, por isso pode que o seu médico lhe faça um seguimento da pressão ocular após cada injeção.
- Informe o seu médico se teve doenças nos olhos ou recebeu algum tratamento nos olhos anteriormente, ou se sofreu um acidente vascular cerebral ou teve sinais passageiros de acidente vascular cerebral (debilidade ou paralisia de um membro ou face, dificuldade na fala ou na compreensão). Esta informação será tida em consideração para avaliar se Lucentis é o tratamento apropriado para si.
Para consultar informações mais detalhadas sobre os efeitos adversos que poderiam ocorrer durante o tratamento com Lucentis, ver secção 4 (“Posíveis efeitos adversos”).
Crianças e adolescentes (menores de 18anos)
Não se recomenda o uso de Lucentis em crianças e adolescentes, pois não foi estabelecido nestes grupos de idade.
Outros medicamentos e Lucentis
Informe o seu médico se está utilizando, utilizou recentemente ou poderia ter que utilizar qualquer outro medicamento.
Gravidez e amamentação
- As mulheres que pudessem ficar grávidas devem utilizar um método anticonceptivo eficaz durante o tratamento e durante pelo menos os três meses posteriores à última injeção de Lucentis.
- Não há experiência no uso de Lucentis em mulheres grávidas. Lucentis não deve ser usado durante a gravidez salvo que o benefício potencial supere o risco potencial para o feto. Se está grávida, acredita que possa estar grávida ou tem intenção de ficar grávida, consulte o seu médico antes do tratamento com Lucentis.
- Pequenas quantidades de Lucentis podem passar para o leite materno, por isso não se recomenda o uso de Lucentis durante a amamentação. Consulte o seu médico ou farmacêutico antes do tratamento com Lucentis.
Condução e uso de máquinas
Após o tratamento com Lucentis você pode experimentar visão borrosa temporariamente. Se isso lhe ocorrer, não conduza nem use máquinas até que este sintoma desapareça.
3. Como é administrado Lucentis
Lucentis é administrado pelo oftalmologista em forma de injeção única no olho sob anestesia local. A dose habitual de uma injeção é 0,05 ml (que contém 0,5 mg de princípio ativo). A seringa pré-carregada contém mais quantidade do que a dose recomendada de 0,5 mg. O volume extraível não será administrado na totalidade. O excesso de volume deve ser expulsado antes da injeção. Se for injetado todo o volume da seringa pré-carregada pode dar origem a uma sobredose.
O intervalo entre duas doses aplicadas no mesmo olho deve ser como mínimo de quatro semanas. Todas as injeções serão administradas por um oftalmologista.
Para prevenir uma infecção, antes da injeção o seu médico lavará o olho cuidadosamente. O seu médico também lhe administrará um anestésico local para reduzir ou prevenir qualquer dor que possa sentir com a injeção.
O tratamento é iniciado com uma injeção de Lucentis cada mês. O seu médico controlará a doença do seu olho e dependendo de como responde ao tratamento, decidirá se precisa ou não receber mais tratamento e quando precisa ser tratado.
No final do prospecto, na secção “Como preparar e administrar Lucentis” são dadas instruções detalhadas de uso.
Pacientes de idade avançada (65anos e mais)
Lucentis pode ser utilizado em pessoas de 65 anos de idade ou mais, e não é necessário um ajuste da dose.
Antes de interromper o tratamento com Lucentis
Se você está considerando interromper o tratamento com Lucentis, acuda à próxima consulta e comente antes com o seu médico. O seu médico aconselhará e decidirá durante quanto tempo deverá ser tratado com Lucentis.
Se tiver alguma outra dúvida sobre o uso deste medicamento, pergunte ao seu médico.
4. Posíveis efeitos adversos
Como todos os medicamentos, este medicamento pode produzir efeitos adversos, embora não todas as pessoas os sofram.
Os efeitos adversos associados à administração de Lucentis devem-se ou ao próprio medicamento ou ao procedimento de injeção e a maioria afeta o olho.
A seguir são descritos os efeitos adversos mais graves:
Efeitos adversos graves frequentes(podem afetar até 1 de cada 10 pacientes): Desprendimento ou desgarro de uma camada na parte interna do olho (desprendimento ou desgarro da retina), que dá origem a destellos de luz com partículas flutuantes que progridem para uma perda de visão transitoria ou para uma enturbiação do cristalino (catarata).
Efeitos adversos graves pouco frequentes(podem afetar até 1 de cada 100 pacientes): Cegueira, infecção do globo ocular (endoftalmite) com inflamação da parte interna do olho.
Os sintomas que poderia experimentar são dor ou aumento das molestias no olho, se piora a vermelhidão no olho, visão borrosa ou diminuição da visão, um aumento do número de pequenas manchas na visão ou aumento da sensibilidade à luz. Informe o seu médico imediatamente se apresentar algum destes efeitos adversos.
A seguir são descritos os efeitos adversos comunicados mais frequentemente:
Efeitos adversos muito frequentes(podem afetar mais de 1 de cada 10 pacientes)
Os efeitos adversos oculares incluem: Inflamação do olho, sangramento na parte posterior do olho (hemorragia na retina), alterações visuais, dor no olho, pequenas partículas ou manchas na visão (partículas flutuantes), sangue no olho, irritação do olho, sensação de ter algo dentro do olho, aumento da produção de lágrima, inflamação ou infecção no bordo das pálpebras, olho seco, vermelhidão ou picor no olho e aumento da pressão no olho.
Os efeitos adversos não oculares incluem: Dor de garganta, congestão nasal, gotejamento nasal, dor de cabeça e dor nas articulações.
A seguir são descritos outros efeitos adversos que podem ocorrer após o tratamento com Lucentis:
Efeitos adversos frequentes
Os efeitos adversos oculares incluem: Diminuição da nitidez da visão, inchação de uma secção do olho (úvea, córnea), inflamação da córnea (parte frontal do olho), pequenas marcas na superfície do olho, visão borrosa, sangramento no local de injeção, sangramento no olho, secreção do olho com picor, vermelhidão e inchação (conjuntivite), sensibilidade à luz, molestias no olho, inchação da pálpebra, dor na pálpebra.
Os efeitos adversos não oculares incluem: Infecção das vias urinárias, contagem de glóbulos vermelhos baixa (com sintomas tais como cansaço, dificuldade ao respirar, tontura, palidez), ansiedade, tosse, náuseas, reações alérgicas tais como erupção, urticária, picor e vermelhidão da pele.
Efeitos adversos pouco frequentes
Os efeitos adversos oculares incluem: Inflamação e sangramento na parte anterior do olho, acúmulo de pus no olho, mudanças na parte central da superfície ocular, dor ou irritação no local de injeção, sensação anormal no olho, irritação da pálpebra.
Comunicação de efeitos adversos
Se experimentar qualquer tipo de efeito adverso, consulte o seu médico, mesmo que se trate de possíveis efeitos adversos que não aparecem neste prospecto. Também pode comunicá-los directamente através do sistema nacional de notificação incluído no Apêndice V. Mediante a comunicação de efeitos adversos, você pode contribuir para fornecer mais informações sobre a segurança deste medicamento.
5. Conservação de Lucentis
- Mantenha este medicamento fora da vista e do alcance das crianças.
- Não utilize este medicamento após a data de validade que aparece na caixa após CAD e na etiqueta da seringa pré-carregada após EXP. A data de validade é o último dia do mês que se indica.
- Conservar em frigorífico (entre 2°C e 8°C). Não congelar.
- Antes de usar, a bandeja selada pode ser conservada a temperatura ambiente (25°C) durante um máximo de 24 horas.
- Conservar a seringa pré-carregada na sua bandeja sem abrir na caixa para protegê-la da luz.
- Não utilize nenhum envase que esteja danificado.
6. Conteúdo do envase e informação adicional
Composição de Lucentis
- O princípio ativo é ranibizumab. Cada ml contém 10 mg de ranibizumab. Uma seringa pré-carregada contém 0,165 ml, equivalente a 1,65 mg de ranibizumab. Isso fornece uma quantidade utilizável que proporciona uma dose única de 0,05 ml, que contém 0,5 mg de ranibizumab.
- Os demais componentes são α,α-trealosa diidratado; cloridrato de histidina monoidratado; histidina; polissorbato 20; água para injetáveis.
Aspecto do produto e conteúdo do envase
Lucentis é uma solução injetável contida em uma seringa pré-carregada. A seringa pré-carregada contém 0,165 ml de uma solução aquosa, estéril, transparente, de incolora a amarelo pardacento pálido. A seringa pré-carregada contém mais quantidade do que a dose recomendada de 0,5 mg. O volume extraível não será administrado em sua totalidade. O excesso de volume deve ser expulsado antes da injeção. Se todo o volume da seringa pré-carregada for injetado, pode dar origem a uma sobredose.
O tamanho do envase é de uma seringa pré-carregada, envasada em uma bandeja contenedora selada. A seringa pré-carregada é para uso único.
Título da autorização de comercialização
Novartis Europharm Limited
Edifício Vista
Elm Park, Merrion Road
Dublin 4
Irlanda
Responsável pela fabricação
Novartis Pharma GmbH
Roonstrasse 25
90429 Nuremberga
Alemanha
Novartis Manufacturing NV
Rijksweg 14
2870 Puurs-Sint-Amands
Bélgica
Novartis Pharma GmbH
Sophie-Germain-Strasse 10
90443 Nuremberga
Alemanha
Pode solicitar mais informações sobre este medicamento dirigindo-se ao representante local do titular da autorização de comercialização:
Bélgica Novartis Pharma N.V. Tel: +32 2 246 16 11 | Lituânia SIA Novartis Baltics Lietuvos filialas Tel: +370 5 269 16 50 |
Novartis Bulgaria EOOD Tel: +359 2 489 98 28 | Luxemburgo Novartis Pharma N.V. Tel: +32 2 246 16 11 |
República Tcheca Novartis s.r.o. Tel: +420 225 775 111 | Hungria Novartis Hungária Kft. Tel: +36 1 457 65 00 |
Dinamarca Novartis Healthcare A/S Tel: +45 39 16 84 00 | Malta Novartis Pharma Services Inc. Tel: +356 2122 2872 |
Alemanha Novartis Pharma GmbH Tel: +49 911 273 0 | Países Baixos Novartis Pharma B.V. Tel: +31 88 04 52 111 |
Estônia SIA Novartis Baltics Eesti filiaal Tel: +372 66 30 810 | Noruega Novartis Norge AS Tel: +47 23 05 20 00 |
Grécia Novartis (Hellas) A.E.B.E. Tel: +30 210 281 17 12 | Áustria Novartis Pharma GmbH Tel: +43 1 86 6570 |
Espanha Novartis Farmacéutica, S.A. Tel: +34 93 306 42 00 | Polônia Novartis Poland Sp. z o.o. Tel: +48 22 375 4888 |
França Novartis Pharma S.A.S. Tel: +33 1 55 47 66 00 | Portugal Novartis Farma - Produtos Farmacêuticos, S.A. Tel: +351 21 000 8600 |
Croácia Novartis Hrvatska d.o.o. Tel: +385 1 6274 220 | Romênia Novartis Pharma Services Romania SRL Tel: +40 21 31299 01 |
Irlanda Novartis Ireland Limited Tel: +353 1 260 12 55 | Eslovênia Novartis Pharma Services Inc. Tel: +386 1 300 75 50 |
Islândia Vistor hf. Tel: +354 535 7000 | República Eslovaca Novartis Slovakia s.r.o. Tel: +421 2 5542 5439 |
Itália Novartis Farma S.p.A. Tel: +39 02 96 54 1 | Finlândia Novartis Finland Oy Tel: +358 (0)10 6133 200 |
Chipre Novartis Pharma Services Inc. Tel: +357 22 690 690 | Suécia Novartis Sverige AB Tel: +46 8 732 32 00 |
Letônia SIA Novartis Baltics Tel: +371 67 887 070 |
Data da última revisão deste prospecto:
Outras fontes de informação
A informação detalhada sobre este medicamento está disponível no site da Agência Europeia de Medicamentos: http://www.ema.europa.eu
Esta informação é destinada apenas a profissionais de saúde:
Ver também a seção 3 “Como administrar Lucentis”.
Como preparar e administrar Lucentis
Seringa pré-carregada para uso único. Apenas para via intravítrea.
Lucentis deve ser administrado por um oftalmologista que tenha experiência na administração de injeções intravítreas.
Na DMAE exsudativa, na NVC, na RDP e na alteração visual devida a EMD ou a edema macular secundário a OVR, a dose recomendada de Lucentis é 0,5 mg administrada em forma de injeção intravítrea única. Isso corresponde a um volume de injeção de 0,05 ml. O intervalo entre duas doses injetadas no mesmo olho deve ser de pelo menos quatro semanas.
O tratamento é iniciado com uma injeção por mês até alcançar a acuidade visual máxima e/ou não haja sinais de atividade da doença, ou seja, nenhum cambio na acuidade visual nem em outros sinais e sintomas da doença sob tratamento contínuo. Em pacientes com DMAE exsudativa, EMD, RDP e OVR, inicialmente podem ser necessárias três ou mais injeções consecutivas administradas mensalmente.
A partir desse momento, os intervalos de monitorização e tratamento devem ser determinados de acordo com o critério médico e com base na atividade da doença, avaliada mediante a acuidade visual e/ou parâmetros anatômicos.
Deve-se interromper o tratamento com Lucentis se, de acordo com o critério do médico, os parâmetros visuais e anatômicos indicam que o paciente não está se beneficiando do tratamento contínuo.
A monitorização para determinar a atividade da doença pode incluir exame clínico, controle funcional ou técnicas de imagem (p. ex. tomografia de coerência óptica ou angiografia com fluoresceína).
Se os pacientes estiverem sendo tratados de acordo com um regime de tratar e estender, uma vez que a acuidade visual máxima tenha sido alcançada e/ou não haja sinais de atividade da doença, os intervalos de tratamento podem ser espaçados gradualmente até que os sinais de atividade da doença ou alteração visual voltem a aparecer. No caso da DMAE exsudativa, o intervalo de tratamento não deve ser espaçado em mais de duas semanas cada vez, e no caso do EMD, pode ser espaçado até um mês cada vez. Para a RDP e a OVR, os intervalos de tratamento também podem ser espaçados gradualmente, no entanto, os dados disponíveis não são suficientes para determinar a duração desses intervalos. Se a atividade da doença voltar a aparecer, o intervalo de tratamento deve ser encurtado de forma consecutiva.
O tratamento da alteração visual devida a NVC deve ser determinado para cada paciente de forma individualizada com base na atividade da doença. Alguns pacientes podem necessitar apenas de uma injeção durante os primeiros 12 meses; outros podem necessitar de tratamento com maior frequência, incluindo uma injeção mensal. No caso de NVC secundária a miopia patológica (MP), muitos pacientes podem necessitar apenas de uma ou duas injeções durante o primeiro ano.
Lucentis e fotocoagulação com laser em EMD e edema macular secundário a oclusão da ramo venosa retiniana (OVR)
Existe alguma experiência com Lucentis administrado concomitantemente com fotocoagulação com laser. Quando administrados no mesmo dia, Lucentis deve ser administrado pelo menos 30 minutos após a fotocoagulação com laser. Lucentis pode ser administrado em pacientes que receberam fotocoagulação com laser previamente.
Lucentis e a terapia fotodinâmica com verteporfina na NVC secundária a MP
Não há experiência na administração concomitante de Lucentis e verteporfina.
Antes da administração de Lucentis, deve-se verificar visualmente a ausência de partículas e decoloração.
O procedimento de injeção deve ser realizado sob condições assépticas, que incluem o lavado quirúrgico das mãos, o uso de luvas estéreis, um campo estéril, um blefarostato estéril para as pálpebras (ou equivalente) e a disponibilidade de uma paracentese estéril (se necessário). Antes de realizar o procedimento de injeção intravítrea, deve-se avaliar detalhadamente a história clínica do paciente em relação a reações de hipersensibilidade. Antes da injeção, deve-se administrar uma anestesia adequada e um microbicida tópico de amplo espectro para desinfetar a pele da zona periocular, pálpebra e superfície ocular, de acordo com a prática local.
A seringa pré-carregada é para uso único. A seringa pré-carregada é estéril. Não use o produto se o envase estiver deteriorado. A esterilidade da seringa pré-carregada apenas pode ser garantida se a bandeja for mantida selada. Não use a seringa pré-carregada se a solução tiver mudado de cor, estiver turva ou contiver partículas.
A seringa pré-carregada contém mais quantidade do que a dose recomendada de 0,5 mg. O volume extraível da seringa pré-carregada (0,1 ml) não será administrado em sua totalidade. O excesso de volume deve ser expulsado antes da injeção. Se todo o volume da seringa pré-carregada for injetado, pode dar origem a uma sobredose. Para expulsar as bolhas de ar e o excesso de medicamento, pressione lentamente o êmbolo até que o bordo inferior da cúpula que forma o extremo do tapão de borracha fique alinhado com a linha negra de dosagem da seringa (equivalente a 0,05 ml, ou seja, 0,5 mg de ranibizumab).
Para a injeção intravítrea, deve-se usar uma agulha para injeção estéril 30G x ½″.
Para a preparação de Lucentis para administração intravítrea, siga as instruções de uso:
Introdução | Leia todas as instruções atentamente antes de usar a seringa pré-carregada. A seringa pré-carregada é para uso único. A seringa pré-carregada é estéril. Não use o produto se o envase estiver deteriorado. A abertura da bandeja selada e os passos subsequentes devem ser realizados sob condições assépticas. Nota: A dose a administrar deve ser ajustada para 0,05 ml. | |
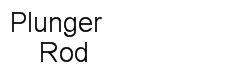
Descrição da seringa pré-carregada |
| |
Preparar |
| |
Verificar a seringa |
| |
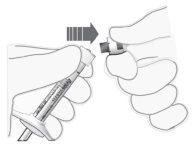
Remover a cápsula de fechamento da seringa |
|
Figura 2
Figura 3 |
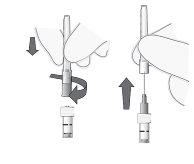
Conectar a agulha |
Nota: Não seque a agulha em nenhum momento. |
Figura 4Figura 5 |
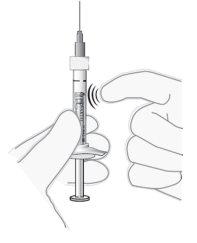
Remover as bolhas de ar |
|
Figura 6 |
Ajustar a dose |
Nota: O êmbolo não está unido ao tapão de borracha – isso é para evitar a entrada de ar na seringa. |
Figura 7 |
Injeção | O procedimento de injeção deve ser realizado sob condições assépticas.
|
- País de registo
- Substância ativa
- Requer receita médicaSim
- Fabricante
- Esta informação é apenas para referência e não constitui aconselhamento médico. Consulte sempre um médico antes de tomar qualquer medicamento. A Oladoctor não se responsabiliza por decisões médicas baseadas neste conteúdo.
- Alternativas a LUCENTIS 10 mg/ml Solução injetável em seringa pré-carregadaForma farmacêutica: INJETÁVEL, 10 mg/mLSubstância ativa: ranibizumabFabricante: Samsung Bioepis Nl B.V.Requer receita médicaForma farmacêutica: INJETÁVEL, 10 mg/mLSubstância ativa: ranibizumabFabricante: Novartis Europharm LimitedRequer receita médicaForma farmacêutica: INJETÁVEL, 10 mg/mlSubstância ativa: ranibizumabFabricante: Midas Pharma GmbhRequer receita médica
Alternativas a LUCENTIS 10 mg/ml Solução injetável em seringa pré-carregada noutros países
As melhores alternativas com o mesmo princípio ativo e efeito terapêutico.
Alternativa a LUCENTIS 10 mg/ml Solução injetável em seringa pré-carregada em Ukraine
Médicos online para LUCENTIS 10 mg/ml Solução injetável em seringa pré-carregada
Avaliação de posologia, efeitos secundários, interações, contraindicações e renovação da receita de LUCENTIS 10 mg/ml Solução injetável em seringa pré-carregada – sujeita a avaliação médica e regras locais.