XULTOPHY 100 U/mL + 3.6 mg/mL INJECTABLE SOLUTION

How to use XULTOPHY 100 U/mL + 3.6 mg/mL INJECTABLE SOLUTION
Translated with AI
This page provides general information and does not replace a doctor’s consultation. Always consult a doctor before taking any medication. Seek urgent medical care if symptoms are severe.
Show originalContents of the leaflet
Introduction
Package Leaflet:information for the patient
Xultophy 100units/ml + 3.6mg/ml solution for injection
insulin degludec + liraglutide
Read all of this leaflet carefully before you start using this medicine because it contains important information for you.
- Keep this leaflet, you may need to read it again.
- If you have any further questions, ask your doctor, pharmacist, or nurse.
- This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours.
- If you get any side effects, talk to your doctor, pharmacist, or nurse. This includes any possible side effects not listed in this leaflet. See section 4.
Contents of the pack
- What is Xultophy and what is it used for
- What you need to know before you use Xultophy
- How to use Xultophy
- Possible side effects
- Storing Xultophy
- Contents of the pack and other information
1. What is Xultophy and what is it used for
What Xultophy is used for
Xultophy is used to improve blood sugar levels in adults with type 2 diabetes mellitus. You have diabetes because your body:
- does not produce enough insulin to control your blood sugar levels or
- cannot use insulin properly.
How Xultophy works
Xultophy contains two active substances that help your body control your blood sugar levels:
- Insulin degludec - a long-acting basal insulin that reduces your blood sugar levels.
- Liraglutide - a "GLP-1 receptor agonist" that helps your body produce more insulin during meals and reduces the amount of sugar produced by your body.
Xultophy and oral anti-diabetic medicines
Xultophy is used together with oral anti-diabetic medicines (such as metformin, pioglitazone, and sulfonylurea). It is prescribed when these medicines (used alone or with GLP-1 receptor agonist or basal insulin treatment) are not enough to control your blood sugar levels.
If you are using GLP-1 receptor agonist treatment
Before you start using Xultophy, you must stop your GLP-1 receptor agonist treatment.
If you are using insulin
Before you start using Xultophy, you must stop your insulin treatment.
2. What you need to know before you use Xultophy
Do not use Xultophy
- if you are allergic to insulin degludec, liraglutide, or any of the other ingredients of this medicine (listed in section 6).
Warnings and precautions
Talk to your doctor, pharmacist, or nurse before you start using Xultophy:
- If you are also taking a sulfonylurea (such as glimepiride or glibenclamide), your doctor may tell you to reduce your sulfonylurea dose, based on your blood sugar levels.
- Do not use Xultophy if you have type 1 diabetes mellitus or if you have "ketoacidosis" (a disease characterized by the accumulation of acid in the blood).
- Xultophy is not recommended for use in patients with inflammatory bowel disease or delayed emptying of the stomach (diabetic gastroparesis).
- If you know you are going to have surgery where you will be under anesthesia (put to sleep), tell your doctor that you are taking Xultophy.
It is important that you know the following information when you use Xultophy:
- Low blood sugar levels (hypoglycemia) - if your blood sugar level is low, follow the advice in section 4 "Low blood sugar levels (hypoglycemia)".
- High blood sugar levels (hyperglycemia) - if your blood sugar level is high, follow the advice in section 4 "High blood sugar levels (hyperglycemia)".
- Make sure you use the correct medicine - always check the label on the pen before each injection to avoid accidental mix-ups between Xultophy and other products.
Important information you should know before using this medicine:
Tell your doctor if:
- you have vision problems. A sudden improvement in blood sugar control may cause a temporary worsening of vision problems due to diabetes. Long-term improvements in blood sugar control may reduce vision problems;
- you have or have had thyroid disease.
Important information you should know while using this medicine:
- you may get dehydrated (lose body fluids) if you have nausea or vomiting or if you have diarrhea; it is important to drink plenty of fluids to stop dehydration.
Changes in the skin at the injection site
You should rotate the injection site to help avoid changes in the fatty tissue, such as thickening of the skin, shrinking of the skin, or lumps under the skin. Insulin may not work well if it is injected into a thickened, shrunk, or lumped area (see section 3 "How to use Xultophy"). Tell your doctor if you notice any changes at the injection site. Tell your doctor if you are currently injecting into these affected areas before you start injecting into a different area. Your doctor may tell you to check your blood sugar levels more closely and adjust your insulin or the dose of your other anti-diabetic medicines.
Children and adolescents
Do not give this medicine to children or adolescents. There is no experience with the use of Xultophy in children and adolescents under 18 years of age.
Other medicines and Xultophy
Tell your doctor, pharmacist, or nurse if you are using, have recently used, or might use any other medicines. Some medicines affect your blood sugar levels, and you may need to adjust your Xultophy dose.
The following are the main medicines that may affect your treatment with Xultophy.
Your blood sugar levels may decrease if you take:
- other anti-diabetic medicines (tablets or injectables)
- sulfonylureas, to treat infections
- anabolic steroids, such as testosterone
- beta-blockers, to treat high blood pressure. These may make it harder to recognize the warning signs of a low blood sugar level (see section 4 "Warning signs of a low blood sugar level, which can appear suddenly")
- acetylsalicylic acid (and medicines called "salicylates"), to relieve pain and reduce fever
- monoamine oxidase inhibitors (MAOIs), to treat depression
- angiotensin-converting enzyme (ACE) inhibitors, to treat certain heart problems or high blood pressure.
Your blood sugar levels may increase if you take:
- danazol, a medicine that affects ovulation
- oral contraceptives (birth control pills)
- thyroid hormones, to treat thyroid gland diseases
- growth hormone, to treat low levels of this hormone
- medicines called "glucocorticoids", such as cortisone, to treat inflammation
- medicines called "sympathomimetics", such as epinephrine (adrenaline), salbutamol, or terbutaline, to treat asthma
- diuretics called "thiazides", to treat high blood pressure or if your body retains too much fluid (fluid retention).
Octreotide and lanreotide- used to treat acromegaly (a rare disorder characterized by excessive production of growth hormone). They may increase or decrease your blood sugar levels.
Pioglitazone- tablets used to treat type 2 diabetes mellitus. Some patients with type 2 diabetes mellitus of long duration and previous heart disease or stroke who were treated with pioglitazone and insulin developed heart failure. Tell your doctor immediately if you have signs of heart failure such as unusual shortness of breath, rapid weight gain, or localized swelling (edema).
Warfarin or other anticoagulants- medicines used to prevent blood clotting. Tell your doctor if you are using warfarin or other anticoagulants, as you may need to have blood tests more often to measure the thickness of your blood (this is known as "International Normalized Ratio" or INR tests).
Using Xultophy with alcohol
If you drink alcohol, it may change your need for Xultophy, as your blood sugar levels may increase or decrease. Therefore, you should check your blood sugar levels more often than usual.
Pregnancy and breast-feeding
Do not use Xultophy if you are pregnant or plan to become pregnant. Tell your doctor if you are pregnant, think you may be pregnant, or plan to become pregnant. It is not known if Xultophy may affect your baby.
Do not use Xultophy during breast-feeding. It is not known if Xultophy passes into breast milk.
Driving and using machines
Low or high blood sugar levels may affect your ability to drive or use tools or machines. If your blood sugar level is low or high, your ability to concentrate and react may be impaired. This could put your life or the lives of others at risk. Ask your doctor if you can drive if:
- you have frequent episodes of low blood sugar;
- you find it hard to recognize the warning signs of low blood sugar.
Important information about some of the ingredients of Xultophy
Xultophy contains less than 1 mmol of sodium (23 mg) per dose; this is essentially "sodium-free".
3. How to use Xultophy
Follow the instructions for administration of this medicine exactly as told by your doctor. If you are not sure, ask your doctor, pharmacist, or nurse again.
If you are blind or have reduced vision and cannot read the dose counter on the pen, do not use this pen without help. Ask for help from a person with no vision problems and who is trained in the use of the Xultophy pre-filled pen.
Your doctor will tell you:
- how much Xultophy you need to use each day
- when to check your blood sugar levels
- how to adjust your dose.
The dose of Xultophy is given in "dose units". The dose counter on the pen shows the number of dose units.
Dosing time
- Use Xultophy once a day, preferably at the same time every day. Choose a time of day that suits you.
- If you cannot use Xultophy at the same time every day, you can use it at a different time of day. Make sure that at least 8 hours pass between doses.
- You do not need to use Xultophy with a meal.
- Always follow your doctor's advice about dose and dose adjustment.
- If you want to change your usual diet, talk to your doctor, pharmacist, or nurse first, as a change in your diet may change your need for Xultophy.
How to handle Xultophy
Xultophy is a pre-filled pen.
- Xultophy is given in "dose units". The dose counter on the pen shows the number of dose units.
- One dose unit contains 1 unit of insulin degludec and 0.036 mg of liraglutide.
- The maximum daily dose of Xultophy is 50 dose units (50 units of insulin degludec and 1.8 mg of liraglutide).
Read the "Instructions for use" carefully on the other side of this leaflet and use the pen as described.
Always check the label on the pen before you inject the medicine to make sure you are using the correct pen.
How to inject
Before you use Xultophy for the first time, your doctor or nurse will show you how to inject it.
- Xultophy is injected under the skin (subcutaneous injection). Do not inject it into a vein or muscle.
- The best areas for injection are the front of your thigh, the top of your arm, and the front of your waist (abdomen).
- Change the injection site every day within the area you are using to reduce the risk of developing lumps or pits in the skin (see section 4).
- Always use a new needle for each injection. Reusing needles can increase the risk of blocked needles, leading to inaccurate dosing. Dispose of the needle safely after each use.
- Do not use a syringe to withdraw the solution from the pen to avoid dosing errors and possible overdoses.
Detailed instructions for use are on the other side of this leaflet.
Do not use Xultophy:
- if the pen is damaged or has not been stored correctly (see section 5).
- if the liquid in the pen window is not clear and colorless.
Use in elderly patients (65 years or older)
Xultophy can be used in elderly patients, but if you are elderly, you may need to check your blood sugar levels more often. Talk to your doctor about possible changes in your dose.
If you have kidney or liver problems
If you have kidney or liver problems, you may need to check your blood sugar levels more often. Talk to your doctor about possible changes in your dose.
If you use more Xultophy than you should
If you use more Xultophy than you should, your blood sugar levels may become too low (hypoglycemia) or you may feel sick or vomit. If your blood sugar levels become too low, follow the advice in section 4 "Low blood sugar levels (hypoglycemia)".
If you forget to use Xultophy
If you forget to inject a dose, inject the missed dose when you discover the mistake, making sure that at least 8 hours pass between doses. If you discover that you missed a dose at the time you are supposed to inject the next dose, do not inject a double dose.
If you stop using Xultophy
Do not stop using Xultophy without talking to your doctor. Stopping Xultophy may cause your blood sugar levels to become too high; follow the advice in section 4 "High blood sugar levels (hyperglycemia)".
If you have any other questions about the use of this medicine, ask your doctor, pharmacist, or nurse.
4. Possible Adverse Effects
Like all medicines, this medicine can cause adverse effects, although not all people suffer from them. This medicine can cause the following serious adverse effects:
- Low blood sugar level (very common: may affect more than 1 in 10 people).
If your blood sugar level decreases, you may faint (lose consciousness). Severe hypoglycemia can cause brain damage and be potentially fatal. If you have signs of low blood sugar, take immediate action to increase your blood sugar level. See tips in "Low blood sugar level (hypoglycemia)" later in this section.
- Severe allergic reaction (anaphylactic reaction) (frequency not known: cannot be estimated from the available data).
If you experience a severe allergic reaction to any of the components of Xultophy, discontinue treatment with Xultophy and consult your doctor immediately. The signs of a severe allergic reaction are:
- local reactions spread to other parts of the body
- you suddenly feel sick with sweating
- you have difficulty breathing
- you have palpitations or feel dizzy.
Changes in the skin at the injection site:
If you inject insulin in the same place, the fatty tissue may shrink (lipoatrophy) or become thicker (lipohypertrophy) (may affect up to 1 in 100 people). Lumps under the skin can also occur due to the accumulation of a protein called amyloid (cutaneous amyloidosis; the frequency of this is not known). Insulin may not work very well if injected into a lumpy, shrunken, or thickened area. Change the injection site to help avoid these skin changes.
Other adverse effects include:
Frequent(may affect up to 1 in 10 people)
- Dizziness.
- Decreased appetite, nausea or vomiting, diarrhea, constipation, indigestion (dyspepsia), inflammation of the stomach lining (gastritis), stomach pain, heartburn or bloating - usually disappear after a few days or weeks.
- Reactions at the injection site. The signs may include bruising (bruises), bleeding, pain, redness, rash, swelling or itching - usually disappear after a few days. If the symptoms do not disappear after a few weeks, consult your doctor. If the reactions worsen, discontinue treatment with Xultophy and consult your doctor immediately. Increased pancreatic enzymes, such as lipase and amylase.
Uncommon(may affect up to 1 in 100 people)
- Rash (red lumps on the skin, sometimes with itching).
- Allergic reactions (hypersensitivity) such as rash, itching and swelling of the face.
- Dehydration (loss of body fluids) - it is essential to drink plenty of fluids to stop dehydration.
- Belching and gas (flatulence).
- Rash.
- Itching.
- Increased heart rate.
- Gallstones.
- Inflamed gallbladder.
- Change in the taste of things.
Frequency not known(cannot be estimated from the available data)
- Pancreatitis (inflammation of the pancreas).
- Delayed emptying of the stomach.
- Swelling of arms or legs (peripheral edema) - when starting to use the medicine, the body may retain more fluid than it should. This causes swelling of the ankles and other joints. This effect usually disappears quickly.
- Intestinal obstruction. A severe form of constipation with other symptoms such as stomach pain, bloating, vomiting, etc.
General effects of diabetes treatment
- Low blood sugar level (hypoglycemia)
Low blood sugar levels may occur if:
- you drink alcohol
- you exercise more than usual
- you eat very little or skip a meal
- you inject too much Xultophy.
Warning signs of low blood sugar that may appear suddenly
Headache, difficulty speaking, palpitations, cold sweat, cold and pale skin, nausea, excessive hunger, tremors, nervousness or anxiety, unusual fatigue, weakness and drowsiness or confusion, difficulty concentrating and temporary changes in vision.
What to do if your blood sugar level is low:
- Take glucose tablets or a sugary product - such as sweets, biscuits or fruit juice (always carry glucose tablets or sugary products with you, just in case you need them).
- Measure your blood sugar level if possible and then rest. You may need to measure your blood sugar level more than once. This is because the improvement in your blood sugar level may not occur immediately.
- Wait until the signs of hypoglycemia have disappeared or your blood sugar level has stabilized. Then continue with your treatment as usual.
What others should do if you lose consciousness:
Inform the people you spend time with that you have diabetes. Tell them what the consequences of low blood sugar might be, including the risk of losing consciousness.
Tell them that if you become unconscious, they should do the following:
- lay you on your side
- seek immediate medical attention
- do notgive you anything to eat or drink, as you may choke.
You may regain consciousness more quickly if you receive glucagon. This should only be administered by someone who knows how to do it.
- If you are given glucagon, you should take glucose or a sugary product as soon as you regain consciousness.
- If you do not respond to glucagon treatment, you should be treated in a hospital.
- If severe hypoglycemia is not treated, it can cause brain damage over time. This can be temporary or permanent. It can lead to death.
Talk to your doctor if:
- you have had low blood sugar levels that have caused you to lose consciousness
- you have used glucagon
- you have had several episodes of low blood sugar recently.
You may need to adjust the dose of Xultophy, your diet or exercise.
- High blood sugar level (hyperglycemia)
High blood sugar levels may occur if:
- you drink alcohol
- you exercise less than usual
- you eat more than usual
- you have an infection or fever
- you do not inject enough Xultophy, repeatedly inject less Xultophy than you need, forget to inject Xultophy or stop treatment with Xultophy without talking to your doctor.
Warning signs of high blood sugar that usually appear gradually
Dry and reddened skin, drowsiness or fatigue, dry mouth, fruity breath odor (acetone), increased need to urinate, thirst, loss of appetite, nausea or vomiting.
These can be symptoms of a very serious condition called "ketoacidosis". This is a buildup of acid in the blood because the body is metabolizing fat instead of sugar. If left untreated, it can cause diabetic coma and death.
What to do if your blood sugar level is high:
- Check your blood sugar level.
- Check your ketone levels in your blood or urine.
- Seek immediate medical attention.
Reporting adverse effects
If you experience any adverse effects, consult your doctor, pharmacist or nurse, even if they are possible adverse effects not listed in this leaflet. You can also report them directly through the national reporting system included in Appendix V. By reporting adverse effects, you can help provide more information on the safety of this medicine.
5. Storage of Xultophy
Keep this medicine out of the sight and reach of children.
Do not use this medicine after the expiry date stated on the label of the pen and on the carton after EXP. The expiry date is the last day of the month indicated.
Before opening
Store in a refrigerator (between 2°C and 8°C). Keep away from the freezer. Do not freeze.
During use
Do not freeze. You can carry Xultophy with you and store it at room temperature (not above 30°C) or in a refrigerator (between 2°C and 8°C) for a maximum of 21 days. The medicine must be discarded 21 days after opening.
Always keep the pre-filled pen with the cap on when not in use to protect it from light.
Medicines should not be disposed of via wastewater or household waste. Ask your pharmacist how to dispose of the packaging and any unused medicine. This will help protect the environment.
6. Container Contents and Additional Information
Xultophy Composition
- The active substances are insulin degludec and liraglutide. Each ml of solution contains 100 units of insulin degludec and 3.6 mg of liraglutide. Each unused pre-filled pen (3 ml) contains 300 units of insulin degludec and 10.8 mg of liraglutide.
- The other components are glycerol, phenol, zinc acetate, hydrochloric acid, and sodium hydroxide (for pH adjustment) and water for injections. See also section 2 "Important information about some of the ingredients of Xultophy" for information on sodium.
Appearance and Container Contents of the Product
Xultophy is a clear and colorless solution.
Container sizes of 1, 3, 5, and a multiple pack with 10 (2 packs of 5) 3 ml pens. Not all pack sizes may be marketed.
Marketing Authorization Holder and Manufacturer
Novo Nordisk A/S
Novo Allé
DK-2880 Bagsværd, Denmark
Instructions for use of your pre-filled pen are included on the back.
Date of last revision of this leaflet:
Other sources of information
Detailed information on this medicine is available on the European Medicines Agency website: http://www.ema.europa.eu.
Xultophy 100 units/ml + 3.6 mg/ml solution for injection Instructions for use
Read these instructions carefullybefore using your Xultophy pre-filled pen. Do not use the pen without proper trainingfrom your doctor or nurse. Start by checking the pen to make sure it contains Xultophy 100 units/ml + 3.6 mg/ml, then look at the illustrations to familiarize yourself with the different parts of the pen and needle. If you are blind or have low vision and cannot read the dose counter on the pen, do not use this pen without help.Seek help from a person who can see well and is trained in the use of the Xultophy pre-filled pen. Xultophy is a medicine that contains insulin degludec and liraglutide.Xultophy is administered in "dose units".One dose unit contains 1 unit of insulin degludec + 0.036 mg of liraglutide. Your pen is a pre-filled dosing pen. It contains 3 ml of Xultophy solution. It delivers doses from:
Your pen delivers doses in increments of 1 dose unit. Do not perform any dose conversion.The selected dose units are equivalent to the number that appears on the dose counter. The pen is designed to be used with NovoTwist or NovoFine disposable needles up to 8 mm in length and 32 G in thickness. Needles are not included in the pack. Important information Pay special attention to these notes because they are important for the safe use of the pen. |
|
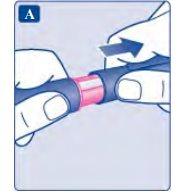
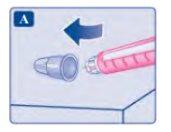
1 Preparing the pen with a new needle
This is especially important if you use more than one type of injectable medicine. Administering the wrong medicine can be harmful to your health.
|
|
|
|
|
A drop of solution may appear at the tip of the needle. This is normal, but you must still check the flow. Do not put a new needle on the penuntil you are ready to take the injection. Always use a new needle for each injection. This will help you avoid blocked needles, contamination, infection, and inaccurate dosing. Never use bent or damaged needles.
|
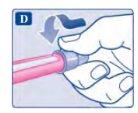
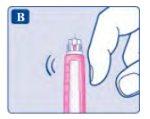
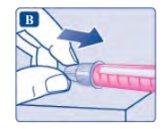
2 Checking the flow
|
|
If no drop appears, do notinject, even if the dose counter moves. This may indicate that the needle is blocked or damaged.
|
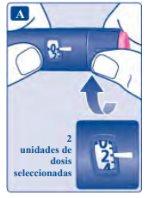
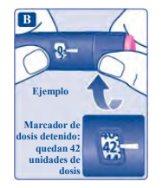
3 Selecting the dose
The dose counter shows the dose in dose units. If you have selected a wrong dose, you can turn the dose selector forward or backward until you reach the correct dose. The pen can select up to a maximum of 50 dose units. The dose selector changes the number of dose units. Only the dose counter and dose indicator show how many dose units you have selected for each administration. You can select up to 50 dose units for each administration. When the pen contains less than 50 dose units, the dose counter stops when it reaches the number of dose units left. The dose selector clicks differently when turned forward, backward, or when passing the number of dose units left. Do not count the pen clicks. Always use the dose counter and dose indicator to see how many dose units you have selected before injecting the medicine. Do not count the pen clicks. If you select a wrong dose and inject it, your blood sugar level may rise or fall. Do not use the pen scale, as it only shows the approximate amount of solution left in the pen.
|
How much solution is left?
|
the dose between two pens. If you divide the dose, be very careful to calculate it correctly. If you are unsure, inject the full dose with a new pen. If you divide the dose incorrectly, you may inject too much or too little medicine. Consequently, your blood sugar level may rise or fall.
|
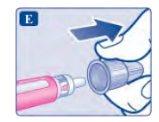
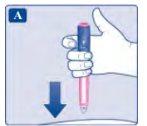
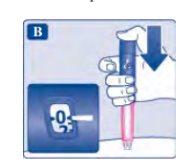
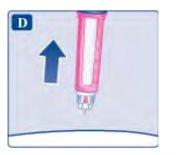
4 Injecting the dose
|
The 0must be aligned with the dose indicator. You may hear or feel a click.
|
|
If blood appears at the injection site, press lightly. Do not rub the area. A drop of solution may appear at the tip of the needle after the injection. This is normal and does not affect the dose. Always check the dose counterto see how many dose units you have injected. Press and hold the dose button until the dose counter shows 0.If the dose counter does not return to 0,it means that the full dose has not been administered, which could lead to high blood sugar levels. How to detect if the needle is blocked or damaged?
What to do if the needle is blocked? Change the needle as described in section 5 and repeat all the steps from section 1: Preparing the pen with a new needle. Make sure to select the full dose you need. Never touch the dose counterwhile injecting. This could interrupt the injection.
|
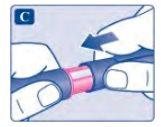
5 After the injection
|
|
Always discard the needleafter each injection, so you can use a sharp needle and avoid blockage. If the needle is blocked, you will not injectany medicine. When the pen is empty, discard it withoutthe needle attached, following the instructions of your doctor, nurse, pharmacist, or local authorities. Never try to put the inner needle cap back on.You could stick yourself with it. Always remove the needle from the penafter each injection. This will help you avoid blocked needles, contamination, infection, solution loss, and inaccurate dosing.
|
More important information
|
Care of the pen
|
- Country of registration
- Active substance
- Prescription requiredYes
- Manufacturer
- This information is for reference only and does not constitute medical advice. Always consult a doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to XULTOPHY 100 U/mL + 3.6 mg/mL INJECTABLE SOLUTIONDosage form: INJECTABLE, 100 U/mlActive substance: insulin glargineManufacturer: Eli Lilly Nederland B.V.Prescription requiredDosage form: INJECTABLE, UnknownActive substance: insulin glargineManufacturer: Sanofi-Aventis Deutschland GmbhPrescription requiredDosage form: INJECTABLE, UnknownActive substance: insulin glargineManufacturer: Sanofi-Aventis Deutschland GmbhPrescription required
Online doctors for XULTOPHY 100 U/mL + 3.6 mg/mL INJECTABLE SOLUTION
Discuss questions about XULTOPHY 100 U/mL + 3.6 mg/mL INJECTABLE SOLUTION, including use, safety considerations and prescription review, subject to medical assessment and local regulations.
Frequently Asked Questions