
SIMPONI 50 mg SOLUTION FOR INJECTION IN PRE-FILLED PEN

How to use SIMPONI 50 mg SOLUTION FOR INJECTION IN PRE-FILLED PEN
Translated with AI
This page provides general information and does not replace a doctor’s consultation. Always consult a doctor before taking any medication. Seek urgent medical care if symptoms are severe.
Show originalContents of the leaflet
Introduction
Package Leaflet: Information for the User
Simponi 50mg solution for injection in pre-filled pen
golimumab
Read all of this leaflet carefully before you start using this medicine because it contains important information for you.
- Keep this leaflet, you may need to read it again.
- If you have any further questions, ask your doctor, pharmacist, or nurse.
- This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours.
- If you get any side effects, talk to your doctor, pharmacist, or nurse. This includes any possible side effects not listed in this leaflet. See section 4.
In addition, your doctor will give you a Patient Alert Card, which contains important safety information that you need to know before and during treatment with Simponi.
Contents of the pack
- What is Simponi and what is it used for
- What you need to know before you use Simponi
- How to use Simponi
- Possible side effects
- Storage of Simponi
- Contents of the pack and further information
1. What is Simponi and what is it used for
Simponi contains the active substance golimumab.
Simponi belongs to a group of medicines called “TNF blockers”. It is used in adultsfor the treatment of the following inflammatory diseases:
- Rheumatoid arthritis
- Psoriatic arthritis
- Axial spondyloarthritis, which includes ankylosing spondylitis and non-radiographic axial spondyloarthritis
- Ulcerative colitis
Simponi is used for the treatment of polyarticular juvenile idiopathic arthritis in childrenfrom 2 years of age.
Simponi works by blocking the action of a protein called “tumor necrosis factor alpha” (TNF-α). This protein is involved in the inflammatory processes of the body, and its blockade can reduce inflammation in your body.
Rheumatoid Arthritis
Rheumatoid arthritis is an inflammatory disease of the joints. If you have active rheumatoid arthritis, you will first be given other medicines. If you do not respond well to these medicines, you may be given Simponi in combination with another medicine called methotrexate to:
- Reduce the signs and symptoms of your disease.
- Slow down the damage to bones and joints.
- Improve your physical condition.
Psoriatic Arthritis
Psoriatic arthritis is an inflammatory disease of the joints, usually accompanied by psoriasis, an inflammatory disease of the skin. If you have active psoriatic arthritis, you will first be given other medicines. If you do not respond well to these medicines, you may be given Simponi to:
- Reduce the signs and symptoms of your disease.
- Slow down the damage to bones and joints.
- Improve your physical condition.
Ankylosing Spondylitis and Non-Radiographic Axial Spondyloarthritis
Ankylosing spondylitis and non-radiographic axial spondyloarthritis are inflammatory diseases of the spine. If you have ankylosing spondylitis or non-radiographic axial spondyloarthritis, you will first be given other medicines. If you do not respond well to these medicines, you may be given Simponi to:
- Reduce the signs and symptoms of your disease
- Improve your physical condition.
Ulcerative Colitis
Ulcerative colitis is an inflammatory disease of the intestine. If you have ulcerative colitis, you will first be given other medicines. If you do not respond well to these medicines, you may be given Simponi to treat your disease.
Polyarticular Juvenile Idiopathic Arthritis
Polyarticular juvenile idiopathic arthritis is an inflammatory disease that causes swelling and pain in the joints of children. If you have polyarticular juvenile idiopathic arthritis, you will first be given other medicines. If you do not respond well to these medicines, you may be given Simponi in combination with methotrexate to treat the disease.
2. What you need to know before you use Simponi
Do not use Simponi
- If you are allergic (hypersensitive) to golimumab or any of the other ingredients of this medicine (listed in section 6).
- If you have tuberculosis (TB) or any other severe infection.
- If you have moderate or severe heart failure.
If you are not sure if any of the above applies to you, talk to your doctor, pharmacist, or nurse before using Simponi.
Warnings and precautions
Talk to your doctor, pharmacist, or nurse before you start using Simponi.
Infections
Tell your doctor immediately if you already have or develop any symptoms of an infection during or after treatment with Simponi. Symptoms of infection include fever, cough, difficulty breathing, flu-like symptoms, diarrhea, wounds, dental problems, or a burning sensation when urinating.
- While you are using Simponi, you may get infections more easily.
- Infections can progress faster and can be more severe. Also, some previous infections may come back.
Tuberculosis (TB)
Tell your doctor immediately if you develop symptoms of TB during or after treatment. Symptoms of TB include persistent cough, weight loss, tiredness, fever, or night sweats.
- There have been reports of tuberculosis in patients treated with Simponi, and in rare cases even in patients who have been treated for TB. Your doctor will do tests to see if you have TB. Your doctor will record these tests on your Patient Alert Card.
- It is very important that you tell your doctor if you have ever had TB or if you have had close contact with someone who has had or has TB.
- If your doctor thinks you are at risk of getting TB, you may be treated with TB medicines before you start treatment with Simponi.
Hepatitis B Virus (HBV)
- Tell your doctor if you are a carrier or if you have had hepatitis B before you are given Simponi
- Tell your doctor if you think you may be at risk of getting HBV
- Your doctor will do HBV tests
- Treatment with TNF blockers like Simponi may cause the hepatitis B virus to become active again in people who carry this virus, which in some cases can be life-threatening.
Invasive Fungal Infections
Tell your doctor immediately if you have lived in or traveled to an area where certain types of fungal infections are common, which can affect the lungs or other parts of your body (called histoplasmosis, coccidioidomycosis, or blastomycosis). If you are not sure if these infections are common in the area you have lived in or traveled to, talk to your doctor.
Cancer and Lymphoma
Tell your doctor if you have ever been diagnosed with lymphoma (a type of blood cancer) or any other cancer before using Simponi.
- If you use Simponi or another TNF blocker, the risk of developing lymphoma or another cancer may be increased.
- Patients with severe rheumatoid arthritis and other inflammatory diseases who have had the disease for a long time may have a higher than average risk of developing lymphoma.
- In children and adolescents treated with TNF blockers, there have been cases of cancer, some of which were rare and sometimes fatal.
- In rare cases, a serious and specific type of lymphoma called hepatosplenic T-cell lymphoma has been observed in patients taking other TNF blockers. Most of these patients were male adolescents or young adults. This type of cancer is usually fatal. Almost all of these patients had also received medicines such as azathioprine or 6-mercaptopurine. Tell your doctor if you are taking azathioprine or 6-mercaptopurine with Simponi.
- Patients with severe persistent asthma, chronic obstructive pulmonary disease (COPD), or heavy smokers may have a higher risk of developing cancer when treated with Simponi. If you have severe persistent asthma, COPD, or are a heavy smoker, you should discuss with your doctor whether treatment with a TNF blocker is suitable for you.
- Some patients treated with golimumab have developed certain types of skin cancer. Tell your doctor if you notice any changes in the appearance of your skin or abnormal skin growth during or after treatment.
Heart Failure
Tell your doctor immediately if you develop new symptoms of heart failure or if the symptoms you already have get worse. Symptoms of heart failure include difficulty breathing or swelling of the feet.
- During treatment with TNF blockers, including Simponi, there have been reports of new or worsening heart failure. Some of these patients died.
- If you have mild heart failure and are being treated with Simponi, your doctor will monitor you closely.
Nervous System Disease
Tell your doctor immediately if you have ever been diagnosed with or have developed symptoms of a demyelinating disease such as multiple sclerosis. Symptoms may include changes in your vision, weakness in your arms or legs, or numbness or tingling in any part of your body. Your doctor will decide if you should receive Simponi.
Surgical or Dental Procedures
- Tell your doctor if you are going to have any surgery or dental procedure.
- Tell the surgeon or dentist who is going to perform the procedure that you are being treated with Simponi, and show them your Patient Alert Card.
Autoimmune Disease
Tell your doctor if you develop symptoms of a disease called lupus. Symptoms include persistent rash, fever, joint pain, and tiredness.
- In rare cases, people treated with TNF blockers have developed lupus.
Blood Disease
In some patients, the body may stop producing enough blood cells that help the body fight infections or stop bleeding. If you develop persistent fever, bruising, or bleeding easily, or if you look pale, tell your doctor immediately. Your doctor may decide to stop treatment.
If you are not sure if any of the above applies to you, talk to your doctor or pharmacist before using Simponi.
Vaccines
Tell your doctor if you have been vaccinated or are going to be vaccinated.
- You should not be vaccinated with certain vaccines (live vaccines) while you are using Simponi.
- Some vaccines may cause infections. If you have received treatment with Simponi during pregnancy, your baby may have a higher risk of getting these infections until about 6 months after your last dose of Simponi. It is important that you inform your baby's doctors and other healthcare professionals about your treatment with Simponi so that they can decide when your baby should be vaccinated.
Tell your child's doctor about the vaccines your child has received. If possible, your child should be up to date with all the vaccines they are due before starting treatment with Simponi.
Therapeutic Infectious Agents
Tell your doctor if you have recently received or are going to receive treatment with therapeutic infectious agents (such as BCG instillation used for cancer treatment).
Allergic Reactions
Tell your doctor immediately if you develop symptoms of an allergic reaction after your treatment with Simponi. Symptoms of an allergic reaction can be swelling of the face, lips, mouth, or throat which may cause difficulty in swallowing or breathing, skin rash, hives, swelling of the hands, feet, or ankles.
- Some of these reactions can be serious or, in rare cases, life-threatening.
- Some of these reactions occurred after the first administration of Simponi.
Children
Simponi is not recommended in children under 2 years of age with polyarticular juvenile idiopathic arthritis, as it has not been studied in this age group.
Other medicines and Simponi
- Tell your doctor or pharmacist if you are using, have recently used, or might use any other medicines, including other medicines for treating rheumatoid arthritis, polyarticular juvenile idiopathic arthritis, psoriatic arthritis, ankylosing spondylitis, non-radiographic axial spondyloarthritis, or ulcerative colitis.
- You must not use Simponi with medicines that contain the active substance anakinra or abatacept. These medicines are used for the treatment of rheumatic diseases.
- Tell your doctor or pharmacist if you are using any other medicine that affects your immune system.
- You must not receive certain vaccines (live vaccines) while you are being treated with Simponi.
If you are not sure if you are using any of the medicines mentioned above, talk to your doctor or pharmacist before using Simponi.
Pregnancy and breast-feeding
Ask your doctor or pharmacist for advice before using Simponi if:
- You are pregnant or planning to become pregnant while using Simponi. There is limited information on the effects of this medicine in pregnant women. If you are treated with Simponi, you should avoid becoming pregnant by using adequate contraceptive methods during your treatment and for at least 6 months after your last injection of Simponi. You should only use Simponi during pregnancy if it is strictly necessary for you.
- Before you start breast-feeding, at least 6 months must have passed since your last treatment with Simponi. You must stop breast-feeding if you are given Simponi.
- If you have received treatment with Simponi during pregnancy, your baby may have a higher risk of getting an infection. It is important that you inform your baby's doctors and other healthcare professionals about your treatment with Simponi before your baby is vaccinated (for more information, see the section on vaccines).
If you are pregnant or breast-feeding, think you may be pregnant, or are planning to have a baby, ask your doctor or pharmacist for advice before using this medicine.
Driving and using machines
Simponi has a minor influence on your ability to drive and use tools or machines. However, you may feel dizzy after receiving Simponi. If this happens, do not drive or use any tools or machines.
Simponi contains latex and sorbitol
Latex Sensitivity
A part of the pre-filled pen, the needle cap, contains latex. As latex can cause severe allergic reactions, talk to your doctor before using Simponi if you or your caregiver are allergic to latex.
Sorbitol Intolerance
This medicine contains 20.5 mg of sorbitol (E-420) in each pre-filled pen.
3. How to use Simponi
Follow exactly the administration instructions of this medication as indicated by your doctor or pharmacist. In case of doubt, consult your doctor or pharmacist again.
What quantity of Simponi is administered
Rheumatoid arthritis, psoriatic arthritis, and axial spondyloarthritis, including ankylosing spondylitis and non-radiographic axial spondyloarthritis:
- The recommended dose is 50 mg (the contents of 1 pre-filled pen) administered once a month, on the same day of each month.
- Consult your doctor before the fourth dose is administered. Your doctor will determine if you should continue treatment with Simponi.
- If you weigh more than 100 kg, the dose may be increased to 100 mg (the contents of 2 pre-filled pens) administered once a month, on the same day of each month.
Polyarticular juvenile idiopathic arthritis in children from 2 years of age:
- In patients who weigh at least 40 kg, the recommended dose is 50 mg administered once a month, on the same day of each month. In patients with a weight below 40 kg, a 45 mg/0.45 ml pre-filled pen is available. Your doctor will inform you of the correct dose to use.
- Consult your doctor before the fourth dose is administered. Your doctor will determine if you should continue treatment with Simponi.
Ulcerative colitis
- The following table shows how you will usually use this medication.
Initial treatment | An initial dose of 200 mg (the contents of 4 pre-filled pens) followed by 100 mg (the contents of 2 pre-filled pens) 2 weeks later. |
Maintenance treatment |
|
How Simponi is administered
- Simponi is administered via a subcutaneous injection.
- Initially, your doctor or nurse may inject Simponi. However, you and your doctor may decide that you can self-inject Simponi. In this case, you will be instructed on how to self-inject Simponi.
Consult your doctor if you have any doubts about how to self-administer an injection. At the end of this leaflet, you will find detailed "Instructions for Use".
If you use more Simponi than you should
If you have used or been administered too much Simponi (by injecting too much at one time or using it too frequently), consult your doctor or pharmacist immediately. Always carry the outer packaging with you, even if it is empty, and this leaflet.
If you forget to use Simponi
If you forget to use Simponi on the scheduled date, inject the missed dose as soon as you remember.
Do not administer a double dose to make up for missed doses.
When to inject the next dose:
- If the dose is delayed by less than 2 weeks, inject the missed dose as soon as you remember and maintain your original schedule.
- If the dose is delayed by more than 2 weeks, inject the missed dose as soon as you remember and consult your doctor or pharmacist when the next dose should be administered.
If you are unsure what to do, consult your doctor or pharmacist.
If you interrupt treatment with Simponi
If you are thinking of interrupting treatment with Simponi, consult your doctor or pharmacist first.
If you have any other doubts about the use of this medication, ask your doctor, pharmacist, or nurse.
4. Possible side effects
Like all medications, this medication can cause side effects, although not all people experience them. Some patients may experience serious side effects and may require treatment. The risk of certain side effects is higher with the 100 mg dose compared to the 50 mg dose. Side effects may appear up to several months after the last injection.
Inform your doctor immediately if you notice any of the serious side effects of Simponi, including:
- allergic reactions that can be serious, or rarely, potentially life-threatening (rare).Symptoms of an allergic reaction may include swelling of the face, lips, mouth, or throat that may cause difficulty swallowing or breathing, skin rash, hives, swelling of the hands, feet, or ankles. Some of these reactions occurred after the first administration of Simponi.
- serious infections (including tuberculosis, bacterial infections that include serious blood infections and pneumonia, serious fungal infections, and other opportunistic infections) (frequent).Symptoms of an infection may include fever, fatigue, cough (persistent), difficulty breathing, flu-like symptoms, weight loss, night sweats, diarrhea, wounds, dental problems, and a burning sensation when urinating.
- reactivation of hepatitis B virus if you are a carrier or have had hepatitis B previously (rare).Symptoms may include yellowing of the eyes and skin, dark brown urine, abdominal pain on the right side, fever, dizziness, vomiting, and extreme fatigue.
- nervous system disease such as multiple sclerosis (rare).Symptoms of nervous system disease may include vision problems, weakness in arms or legs, numbness or tingling of any part of your body.
- lymph node cancer (lymphoma) (rare).Symptoms of lymphoma may include swelling of the lymph nodes, weight loss, or fever.
- heart failure (rare).Symptoms of heart failure may include difficulty breathing or swelling of your feet.
- signs of immune system disorders called:
- lupus (rare).Symptoms may include joint pain or a skin rash on the cheeks or arms that is sensitive to the sun.
- sarcoidosis (rare).Symptoms may include persistent cough, shortness of breath, chest pain, fever, swelling of the lymph nodes, weight loss, skin rashes, and blurred vision.
- swelling of small blood vessels (vasculitis) (rare).Symptoms may include fever, headache, weight loss, night sweats, skin rash, and nerve problems such as numbness and tingling.
- skin cancer (uncommon).Symptoms of skin cancer may include changes in the appearance of the skin or abnormal skin growth.
- blood disease (frequent).Symptoms of blood disease may include persistent fever, bruising or easy bleeding, or pallor.
- blood cancer (leukemia) (rare).Symptoms of leukemia may include fever, fatigue, frequent infections, easy bruising, and night sweats.
Inform your doctor immediately if you notice any of the above symptoms.
The following additional side effects have been observed with Simponi:
Very common side effects (may affect more than 1 in 10 patients):
- Upper respiratory tract infections, sore throat or hoarseness, runny nose
Common side effects (may affect up to 1 in 10 patients):
- Liver test alterations (increase in liver enzymes) detected during blood tests requested by your doctor
- Dizziness
- Headache
- Numbness or tingling
- Superficial fungal infections
- Abscess
- Bacterial infections (such as cellulitis)
- Low red blood cell count
- Low white blood cell count
- Positive lupus test in blood
- Allergic reactions
- Indigestion
- Stomach pain
- Dizziness (nausea)
- Flu
- Bronchitis
- Sinusitis
- Herpes
- High blood pressure
- Fever
- Asthma, shortness of breath, difficulty breathing
- Stomach and intestine disorders, including inflammation of the stomach lining and colon that may cause fever
- Pain and sores in the mouth
- Injection site reactions (including redness, hardness, pain, bruising, itching, tingling, and irritation)
- Hair loss
- Skin rash and itching
- Difficulty sleeping
- Depression
- Weakness
- Bone fractures
- Chest discomfort
Uncommon side effects (may affect up to 1 in 100 patients):
- Kidney infection
- Cancers, such as skin cancer and non-cancerous tumors or lumps, including moles
- Blistering of the skin
- Severe whole-body infection (sepsis), which sometimes includes low blood pressure (septic shock)
- Psoriasis (including on the palms of the hands and/or soles of the feet and/or of the type that presents with blisters on the skin)
- Low platelet count
- Low combined platelet, red blood cell, and white blood cell count
- Thyroid disorders
- Increased blood sugar levels
- Increased blood cholesterol levels
- Balance disorders
- Visual disturbances
- Eye inflammation (conjunctivitis)
- Eye allergy
- Irregular heartbeat
- Narrowing of the heart blood vessels
- Blood clots
- Flushing
- Constipation
- Chronic inflammatory lung disease
- Reflux
- Gallstones
- Liver disorders
- Breast disorders
- Menstrual cycle disorders
Rare side effects (may affect up to 1 in 1,000 patients):
- Failure of the bone marrow to produce blood cells
- Severe decrease in the number of white blood cells in the blood
- Infection of the joints or the tissue surrounding them
- Healing problems
- Inflammation of blood vessels in internal organs
- Leukemia
- Melanoma (a type of skin cancer)
- Merkel cell carcinoma (a type of skin cancer)
- Lichenoid reactions (pruritic reddish-purple skin rash and/or thick grayish-white lines on the mucous membranes)
- Scaly and flaky skin
- Immune system disorders that may affect the lungs, skin, and lymph nodes (usually presented as sarcoidosis).
- Pain and discoloration in the fingers or toes
- Taste disorders
- Bladder disorders
- Kidney disorders
- Inflammation of blood vessels in the skin that causes a rash
Side effects with unknown frequency:
- A rare blood cancer that mainly affects young people (hepatosplenic T-cell lymphoma)
- Kaposi's sarcoma, a rare cancer related to human herpesvirus 8 infection. Kaposi's sarcoma usually manifests more frequently as purple skin lesions
- Worsening of a disease called dermatomyositis (which manifests as a skin rash accompanied by muscle weakness)
Reporting side effects
If you experience any side effects, consult your doctor, pharmacist, or nurse, even if it is a possible side effect not listed in this leaflet. You can also report them directly through the national reporting system included in Appendix V. By reporting side effects, you can help provide more information on the safety of this medication.
5. Storage of Simponi
- Keep this medication out of sight and reach of children.
- Do not use this medication after the expiration date stated on the label and on the packaging after "EXP". The expiration date is the last day of the month indicated.
- Store in a refrigerator (between 2°C and 8°C). Do not freeze.
- Keep the pre-filled pen in the outer packaging to protect it from light.
- This medication can also be stored at room temperature up to a maximum of 25°C for a single period of up to 30 days, but not beyond the initial expiration date printed on the box. Write the new expiration date on the box, including day/month/year (not more than 30 days after the medication is removed from the refrigerator). If it has reached room temperature, do not return this medication to the refrigerator. Discard this medication if it has not been used by the new expiration date or the expiration date printed on the box, whichever occurs first.
- Do not use this medication if you notice that the liquid is not transparent or clear yellow, cloudy, or contains foreign particles.
- Medications should not be disposed of via wastewater or household waste. Ask your doctor or pharmacist how to dispose of the packaging and any unused medication. This will help protect the environment.
6. Container Contents and Additional Information
Composition ofSimponi
The active substance is golimumab. A 0.5 ml pre-filled pen contains 50 mg of golimumab.
The other ingredients are sorbitol (E-420), histidine, histidine hydrochloride monohydrate, polysorbate 80, and water for injections. For more information on sorbitol (E-420), see section 2.
Appearance and Container Contents of the Product
Simponi is presented as a solution for injection in a single-use pre-filled pen. Simponi is available in packs containing 1 pre-filled pen and multiple packs containing 3 pre-filled pens (3 packs of 1). Only some pack sizes may be marketed.
The solution is between transparent and slightly opalescent (with a pearlescent sheen), colorless to light yellow, and may contain a few small translucent or white protein particles. Do not use Simponi if the solution changes color, is cloudy, or if foreign particles are observed in it.
Marketing Authorization Holder and Manufacturer
Janssen Biologics B.V.
Einsteinweg 101
2333 CB Leiden
Netherlands
You can request more information about this medicinal product by contacting the local representative of the marketing authorization holder:
Belgium/Belgique/Belgien MSD Belgium Tel: +32(0)27766211 | Lithuania UAB Merck Sharp & Dohme Tel: + 370 5 278 02 47 |
Bulgaria Merck Sharp & Dohme Bulgaria EOOD Tel: +359 2 819 3737 | Luxembourg/Luxemburg MSD Belgium Tel: (+32(0)27766211) |
Czech Republic Merck Sharp & Dohme s.r.o. Tel: +420 233 010 111 | Hungary MSD Pharma Hungary Kft. Tel: +36 1 888 5300 |
Denmark MSD Danmark ApS Tlf: + 45 4482 4000 | Malta Merck Sharp & Dohme Cyprus Limited Tel: 8007 4433 (+356 99917558) |
Germany MSD Sharp & Dohme GmbH Tel: 0800 673 673 673 (+49 (0) 89 4561 0) | Netherlands Merck Sharp & Dohme B.V. Tel: 0800 9999000 (+31 23 5153153) |
Estonia Merck Sharp & Dohme OÜ Tel: +372 6144 200 | Norway MSD (Norge) AS Tlf: +47 32 20 73 00 |
Greece MSD Α.Φ.Β.Ε.Ε. Τηλ: +30 210 98 97 300 | Austria Merck Sharp & Dohme Ges.m.b.H. Tel: +43 (0) 1 26 044 |
Spain Merck Sharp & Dohme de España, S.A. Tel: +34 91 321 06 00 | Poland MSD Polska Sp. z o.o. Tel: +48 22 549 51 00 |
France MSD France Tél: + 33 (0) 1 80 46 40 40 | Portugal Merck Sharp & Dohme, Lda Tel: +351 21 4465700 |
Croatia Merck Sharp & Dohme d.o.o. Tel: + 385 1 6611 333 | Romania Merck Sharp & Dohme Romania S.R.L. Tel: +40 21 529 29 00 |
Ireland Merck Sharp & Dohme Ireland (Human Health) Limited Tel: +353 (0)1 2998700 | Slovenia Merck Sharp & Dohme, inovativna zdravila d.o.o. Tel: +386 1 5204 201 |
Iceland Vistor hf. Sími: + 354 535 7000 | Slovak Republic Merck Sharp & Dohme, s. r. o. Tel: +421 2 58282010 |
Italy MSD Italia S.r.l. Tel: 800 23 99 89 (+39 06 361911) | Finland MSD Finland Oy Puh/Tel: +358 (0)9 804 650 |
Cyprus Merck Sharp & Dohme Cyprus Limited Τηλ: 800 00 673 (+357 22866700) | Sweden Merck Sharp & Dohme (Sweden) AB Tel: +46 77 5700488 |
Latvia SIA Merck Sharp & Dohme Latvija Tel: + 371 67364224 | United Kingdom (Northern Ireland) Merck Sharp & Dohme Ireland (Human Health) Limited Tel: +35312998700 |
Date of Last Revision of this Leaflet:
Detailed information on this medicinal product is available on the European Medicines Agency web site: http://www.ema.europa.eu.
INSTRUCTIONS FOR USE
If you want to inject Simponi yourself, you must have a healthcare professional teach you how to prepare the injection and inject yourself. If you have not been taught, contact your doctor, nurse, or pharmacist to schedule a training session.
In these instructions:
- Preparation for using the pre-filled pen
- Selection and preparation of the injection site
- Injection of the medicine
- After the injection
The following diagram (see Figure 1) shows what the pre-filled pen "SmartJect" looks like.
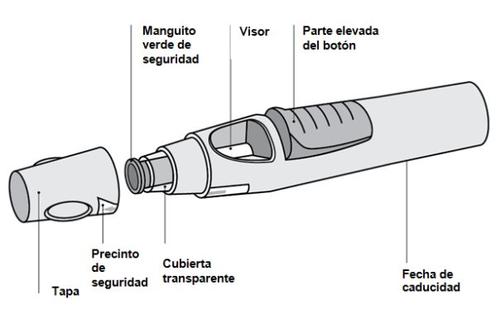
Figure 1
- Preparation for using the pre-filled pen
- Do not shake the pre-filled pen at any time.
- Do not remove the cap from the pre-filled pen until immediately before injection.
- Do not replace the cap on the pre-filled pen if you have removed it, to avoid bending the needle.
Check the number of pre-filled pens
Check the pre-filled pens to ensure that
- The number of pre-filled pens and the dose is correct
- If your dose is 50 mg, you will receive one 50 mg pre-filled pen
- If your dose is 100 mg, you will receive two 50 mg pre-filled pens and you will need to administer two injections yourself. Choose two different injection sites (e.g., one injection in the right thigh and the other injection in the left thigh) and administer the injections one after the other.
- If your dose is 200 mg, you will receive four 50 mg pre-filled pens and you will need to administer four injections yourself. Choose different injection sites and administer the injections one after the other.
Check the expiration date
- Check the expiration date printed or written on the carton.
- Check the expiration date (indicated by "EXP") on the pre-filled pen.
- Do not use the pre-filled pen if the expiration date has passed. The printed expiration date is the last day of the month indicated. Consult your doctor or pharmacist.
Check the safety seal
- Check the safety seal around the cap of the pre-filled pen.
- Do not use the pre-filled pen if the seal is broken. Consult your doctor or pharmacist.
Wait for 30 minutes to allow the pre-filled pen to reach room temperature
- To ensure the injection is correct, leave the pre-filled pen at room temperature outside of the carton for 30 minutes, out of the reach of children.
- Do not use any other method to heat the pre-filled pen (e.g., do not heat it in the microwave or in hot water).
- Do not remove the cap from the pre-filled pen while waiting for it to reach room temperature.
Prepare the rest of the materials
- While waiting, prepare the rest of the materials you need, such as alcohol swabs, a cotton ball or gauze, and a sharps container.
Check the liquid in the pre-filled pen
- Look through the viewer to check that the liquid in the pre-filled pen is transparent to slightly opalescent (with a pearlescent sheen) and colorless to light yellow. The solution can be used if it contains a few small translucent or white protein particles.
- You will also see an air bubble, which is normal.
- Do not use the pre-filled pen if the liquid has an abnormal color, is cloudy, or contains large particles. In such cases, inform your doctor or pharmacist.
- Selection and preparation of the injection site (see Figure 2)
- The medicine can be injected into the middle of the thigh.
- It can be injected into the abdomen below the navel, except for the area of about 5 cm immediately below the navel.
- Do not inject into areas where the skin is sensitive, bruised, red, scaly, hard, or has scars or stretch marks.
- If multiple injections are needed for a single dose, the injections will be administered in different injection sites.

Figure 2
DO NOTinject into the arm to avoid failure of the pre-filled pen and/or accidental needlestick injuries.
Wash your hands and cleanthe injection site
- Wash your hands well with soap and warm water.
- Clean the injection site with an alcohol swab.
- Let the skin dry before injection. Do not fan or blow on the cleaned area.
- Do not touch that area again until you put the injection.
- Injection of the medicine
- Do not remove the cap until you are ready to inject the medicine.
- The medicine must be injected within 5 minutes of removing the cap.
Remove the cap (Figure 3)
- When you are ready, gently twist the cap to break the safety seal.
- Remove the cap and dispose of it after injection.
- Do not replace the cap because it may damage the needle inside the pre-filled pen.
- Do not use the pre-filled pen if it has fallen without the cap. If this happens, inform your doctor or pharmacist.
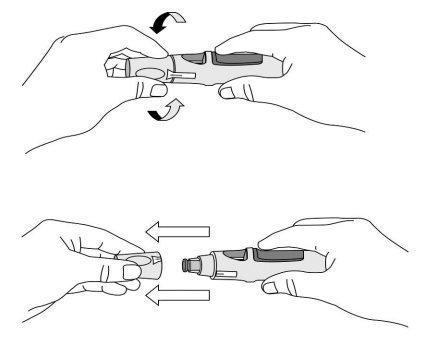
Figure 3
Push the pre-filled pen against the skin (see Figures 4 and 5) without pinching the skin.

Figure 4
- Hold the pre-filled pen relaxedly with one hand above the blue button
- Make sure the green safety sleeve is stable and as flat as possible against your skin. If the pre-filled pen is not stable during injection, you risk bending the needle.
- DO NOTpinch the skin to avoid accidental needlestick injuries.
- DO NOTtouch or press the blue button while placing the pre-filled pen against your skin.
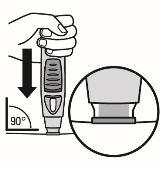
Figure 5
- Push the open end of the pre-filled pen against the skin at a 90-degree angle. Press until the green safety sleeve slides up and stays inside the transparent cover. Only the wider part of the green safety sleeve remains outside the transparent cover.
- DO NOTpress the blue button until the safety sleeve is slid inside the transparent cover. Pressing the blue button before the safety sleeve is retracted may cause the pen to fail.
- Perform the injection without pinching the skin.
Press the injection button (see Figures 6 and 7)
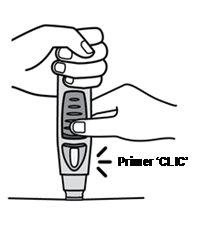

Figure 6 Figure 7
- Keep the pre-filled pen pressed against the skin.To start the injection, use your other handto press the raised part of the blue button. Do not press the button unless the pre-filled pen is pressed against the skinand the safety sleeve is slid inside the transparent cover.
- Once the button is pressed, it will remain pressed and does not need to be pressed further.
- If it seems difficult to press the button, do not press the button with more force. Release the button, lift the pre-filled pen, and start again. Make sure there is no pressure on the button until the green safety sleeve is completely retracted against the skin, then press the raised part of the blue button.
- You will hear a loud sound, a "click" - do not be alarmed.The first "click" indicates that the needle has been inserted and the injection has started. You may not feel the needle prick at this time.
Do not lift the pre-filled pen from the skin. If you remove the pre-filled pen from the skin, you may not receive the full dose.
Continue to hold until the second "click" (see Figure 8), this usually takes between 3 and 6 seconds, but it may take up to 15 seconds until you hear the second "click".

Figure 8
- Keep the pre-filled pen against the skin until you hear a second "click" (which indicates that the injection is complete and the needle has retracted into the pre-filled pen).
- Lift the pre-filled pen from the injection site.
- Note: If you do not hear the second "click", wait 15 seconds from the moment you first pressed the button and then lift the autoinjector from the injection site.
- After the injection
Use a cotton ball or gauze
- You may see a little blood or liquid at the injection site. This is normal.
- With a cotton ball or gauze, press on the injection site for 10 seconds.
- If necessary, cover the injection site with a small adhesive bandage.
- Do not rub the skin.
Check the viewer - a yellow indicator confirms adequate administration (see Figure 9)
- The yellow indicator is connected to the plunger of the pre-filled pen. If the yellow indicator does not appear in the viewer, the plunger has not moved adequately, and the injection has not occurred.
- The yellow indicator will fill almost half of the viewer. This is normal.
- If the yellow indicator does not appear in the viewer, or if you suspect that you may not have received a full dose, inform your doctor or pharmacist. Do not administer a second dose without consulting your doctor.
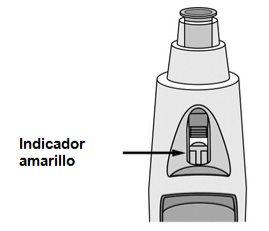
Figure 9
Dispose of the pre-filled pen (see Figure 10)
- Then, place the pen in a sharps container. Follow the doctor's or nurse's instructions for disposing of the container when it is full.
If you think something has gone wrong during the injection or have any doubts, inform your doctor or pharmacist.

Figure 10
- Country of registration
- Active substance
- Prescription requiredYes
- Manufacturer
- This information is for reference only and does not constitute medical advice. Always consult a doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to SIMPONI 50 mg SOLUTION FOR INJECTION IN PRE-FILLED PENDosage form: INJECTABLE, 100 mg/1mlActive substance: golimumabManufacturer: Janssen Biologics B.V.Prescription requiredDosage form: INJECTABLE, 20 mgActive substance: adalimumabManufacturer: Amgen Europe B.V.Prescription requiredDosage form: INJECTABLE, 20 mgActive substance: adalimumabManufacturer: Amgen Europe B.V.Prescription required
Online doctors for SIMPONI 50 mg SOLUTION FOR INJECTION IN PRE-FILLED PEN
Discuss questions about SIMPONI 50 mg SOLUTION FOR INJECTION IN PRE-FILLED PEN, including use, safety considerations and prescription review, subject to medical assessment and local regulations.
Frequently Asked Questions






