PELMEG 6 mg INJECTABLE SOLUTION IN PRE-FILLED SYRINGE


How to use PELMEG 6 mg INJECTABLE SOLUTION IN PRE-FILLED SYRINGE
Translated with AI
This page provides general information and does not replace a doctor’s consultation. Always consult a doctor before taking any medication. Seek urgent medical care if symptoms are severe.
Show originalContents of the leaflet
Introduction
Package Leaflet: Information for the User
Pelmeg 6 mg solution for injection in pre-filled syringe
pegfilgrastim
Read all of this leaflet carefully before you start using this medicine because it contains important information for you.
- Keep this leaflet, you may need to read it again.
- If you have any further questions, ask your doctor, pharmacist or nurse.
- This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours.
- If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in this leaflet. See section 4.
Contents of the pack
- What is Pelmeg and what is it used for
- What you need to know before you use Pelmeg
- How to use Pelmeg
- Possible side effects
- Storage of Pelmeg
- Contents of the pack and other information
1. What is Pelmeg and what is it used for
Pelmeg contains the active substance pegfilgrastim. Pegfilgrastim is a protein produced by biotechnology in the bacterium E. coli. Pegfilgrastim belongs to a group of proteins called cytokines and is very similar to a natural protein (granulocyte colony-stimulating factor) produced by our body.
Pelmeg is used in adult patients to reduce the duration of neutropenia (low white blood cell count) and the incidence of febrile neutropenia (low white blood cell count and fever) that can occur as a result of cytotoxic chemotherapy (medicines that destroy rapidly dividing cells). White blood cells are important cells that help fight infections. These cells are sensitive to the effects of chemotherapy, which can cause their numbers to decrease. If the number of white blood cells decreases too much, there may not be enough to fight off bacteria, which can lead to a higher risk of infection.
Your doctor has prescribed Pelmeg to stimulate your bone marrow (the part of the bone where blood cells are produced) to produce more white blood cells to help you fight infections.
2. What you need to know before you use Pelmeg
Do not use Pelmeg
- if you are allergic to pegfilgrastim, filgrastim, proteins produced in E. colior any of the other ingredients of this medicine.
Warnings and precautions
Talk to your doctor, pharmacist or nurse before starting Pelmeg:
- if you experience an allergic reaction that includes weakness, low blood pressure, difficulty breathing, swelling of the face (anaphylaxis), redness and flushing, skin rash and itching.
- if you experience cough, fever and difficulty breathing. This may be a sign of acute respiratory distress syndrome (ARDS).
- if you experience any or a combination of the following side effects:
- swelling that may be associated with decreased frequency of urination, difficulty breathing, abdominal swelling and a feeling of fullness and a general feeling of tiredness.
These may be symptoms of a condition called "capillary leak syndrome" that causes blood to leak from small blood vessels into other parts of your body. See section 4.
- if you have pain in the upper left abdomen or pain in the tip of the shoulder. This may be a sign of a problem with the spleen (splenomegaly).
- if you have recently had a severe lung infection (pneumonia), fluid in the lungs (pulmonary edema), inflammation of the lungs (interstitial lung disease) or an abnormal chest X-ray (pulmonary infiltration).
- if you are aware of any changes in your blood cell count (e.g. increased white blood cell count or anemia) or a decrease in your platelet count, which can reduce the ability of your blood to clot (thrombocytopenia). Your doctor may want to monitor you more closely.
- if you have sickle cell anemia. Your doctor may monitor your condition more closely.
- if you are a cancer patient, the combined treatment of Pelmeg with chemotherapy and/or radiotherapy may increase the risk of developing a pre-cancerous hematological condition called myelodysplastic syndrome (MDS) or a hematological malignancy called acute myeloid leukemia (AML). Symptoms may include tiredness, fever, easy bruising or bleeding.
- if you have sudden signs of allergy, such as rash, itching or hives on the skin, swelling of the face, lips, tongue or other parts of the body, shortness of breath, wheezing or difficulty breathing. These may be signs of a severe allergic reaction.
- if you have symptoms of inflammation of the aorta (the large blood vessel that carries blood from the heart to the rest of the body), this has rarely been reported in cancer patients and healthy donors. Symptoms may include fever, abdominal pain, general malaise, back pain and increased inflammatory markers. Inform your doctor if you experience these symptoms.
Your doctor will perform regular blood and urine tests as Pelmeg may damage the small filters inside the kidneys (glomerulonephritis).
With the use of Pelmeg, serious skin reactions (Stevens-Johnson syndrome) have been reported. Stop using Pelmeg and seek medical attention immediately if you notice any of the symptoms described in section 4.
You should discuss with your doctor the risk of developing blood cancer. If you develop or may develop blood cancer, you should not use Pelmeg, unless your doctor advises you to.
Loss of response to pegfilgrastim
If you experience a loss of response or if you are unable to maintain a response to treatment with pegfilgrastim, your doctor will investigate the causes, including whether you have developed antibodies that neutralize the activity of pegfilgrastim.
Other medicines and Pelmeg
Tell your doctor or pharmacist if you are using, have recently used or might use any other medicines.
Pregnancy and breastfeeding
Ask your doctor or pharmacist for advice before taking any medicine. Pelmeg has not been studied in pregnant women. It is important that you inform your doctor if:
- you are pregnant;
- you think you may be pregnant; or
- you plan to become pregnant.
If you become pregnant during treatment with Pelmeg, inform your doctor.
Unless your doctor tells you otherwise, you must stop breastfeeding if you use Pelmeg.
Driving and using machines
Pelmeg has no or negligible influence on the ability to drive and use machines.
Pelmeg contains sorbitol (E 420) and sodium acetate
This medicine contains 30 mg of sorbitol in each pre-filled syringe equivalent to 50 mg/ml.
This medicine contains less than 1 mmol of sodium (23 mg) per 6 mg, i.e. it is essentially "sodium-free".
3. How to use Pelmeg
Pelmeg is indicated for adults 18 years of age or older.
Follow exactly the instructions for administration of this medicine given by your doctor. If you are unsure, consult your doctor or pharmacist again. The usual dose is a single subcutaneous injection of 6 mg (under the skin) using a pre-filled syringe, which should be administered at the end of each chemotherapy cycle at least 24 hours after your last dose of chemotherapy.
Do not shake Pelmeg vigorously as this may affect its activity.
Self-injection of Pelmeg
Your doctor may consider it more convenient for you to inject Pelmeg yourself. Your doctor or nurse will teach you how to do this. Do not attempt to do it if you have not been taught.
For further instructions on how to inject Pelmeg yourself, read the section at the end of this leaflet.
If you use more Pelmeg than you should
If you use more Pelmeg than you should, tell your doctor, pharmacist or nurse.
If you forget to inject Pelmeg
If you have forgotten to administer a dose of Pelmeg, contact your doctor to decide when you should inject the next dose.
If you have any further questions on the use of this medicine, ask your doctor, pharmacist or nurse.
4. Possible side effects
Like all medicines, this medicine can cause side effects, although not everybody gets them.
Tell your doctor immediately if you experience any or a combination of the following side effects:
- swelling that may be associated with decreased frequency of urination, difficulty breathing, abdominal swelling and a feeling of fullness and a general feeling of tiredness. These symptoms usually develop rapidly.
These may be symptoms of a condition called "capillary leak syndrome" that causes blood to leak from small blood vessels into other parts of your body and requires urgent medical attention.
Very common side effects(may affect more than 1 in 10 patients):
- bone pain. Your doctor will inform you about what you can take to relieve the pain;
- nausea and headache.
Common side effects(may affect up to 1 in 10 patients):
- injection site pain;
- general pain and pain in the joints and muscles;
- some changes in your blood may occur, which will be detected by regular blood tests. You may have an increased white blood cell count for a short period. You may have a decreased platelet count, which can cause bruising.
Uncommon side effects(may affect up to 1 in 100 patients):
- allergic reactions, including redness and flushing, rash, and skin inflammation with itching;
- severe allergic reactions, including anaphylaxis (weakness, low blood pressure, difficulty breathing, facial swelling);
- enlargement of the spleen;
- splenic rupture. Some cases of splenic rupture were fatal. It is important that you contact your doctor immediately if you notice pain in the upper left abdomen or in the left shoulder as these may be related to a problem with your spleen;
- respiratory problems. If you have cough, fever and difficulty breathing, consult your doctor. Cases of Sweet's syndrome (painful, inflamed, purple-colored lesions on the extremities and sometimes on the face and neck, accompanied by fever) have been reported, but may be related to other factors;
- cutaneous vasculitis (inflammation of the skin blood vessels);
- damage to the small filters inside the kidneys (glomerulonephritis);
- redness at the injection site;
- bloody cough (hemoptysis).
- hematological disorders (myelodysplastic syndrome [MDS] or acute myeloid leukemia [AML]).
Rare side effects(may affect up to 1 in 1,000 patients):
- inflammation of the aorta (the large blood vessel that carries blood from the heart to the rest of the body), see section 2;
- bleeding in the lungs (pulmonary hemorrhage).
- Stevens-Johnson syndrome, which can appear as red, circular, or concentric patches, often with central blisters on the trunk, exfoliation, ulcers in the mouth, throat, nose, genitals, and eyes; and may be preceded by fever and flu-like symptoms. Stop using Pelmeg if you develop these symptoms and contact your doctor or seek medical attention immediately. See section 2.
Reporting of side effects
If you experience any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in this leaflet. You can also report side effects directly via the national reporting system listed in Appendix V. By reporting side effects, you can help provide more information on the safety of this medicine.
5. Storage of Pelmeg
Keep this medicine out of the sight and reach of children.
Do not use this medicine after the expiry date which is stated on the carton and on the label of the pre-filled syringe after EXP. The expiry date is the last day of the month shown.
Store in a refrigerator (2°C - 8°C).
Pelmeg can be stored at room temperature (below 30°C) for a maximum of 4 days. Once a pre-filled syringe has been removed from the refrigerator and reached room temperature (below 30°C), it must be used within 4 days or discarded.
Do not freeze. Pelmeg can be used if it has been accidentally frozen for two periods of less than 72 hours each.
Keep the container in the outer packaging to protect it from light.
Do not use this medicine if you notice that the solution is cloudy or contains particles.
Medicines should not be disposed of via wastewater or household waste. Ask your pharmacist how to dispose of medicines no longer required. This will help protect the environment.
6. Container Contents and Additional Information
Pelmeg Composition
- The active ingredient is pegfilgrastim. Each pre-filled syringe contains 6 mg of pegfilgrastim in 0.6 ml of solution.
- The other components are sodium acetate, sorbitol (E 420), polysorbate 20, and water for injectable preparations. See section 2.
Product Appearance and Container Contents
Pelmeg is a clear and colorless injectable solution in a pre-filled syringe (6 mg/0.6 ml).
Each container contains 1 glass pre-filled syringe with a stainless steel needle and a needle cap. The syringe is supplied with an automatic needle guard.
Marketing Authorization Holder
Mundipharma Corporation (Ireland) Limited,
United Drug House Magna Drive, Magna Business Park,
Citywest Road, Dublin 24,
Ireland
Manufacturer
PharmaKorell GmbH
Georges-Köhler-Str. 2,
79539 Lörrach
Germany
You can request more information about this medication by contacting the local representative of the marketing authorization holder:
Belgium Mundipharma BV Tel: +32 2 358 54 68 | Lithuania EGIS Pharmaceuticals PLC representative Tel: +370 5 231 4658 |
| Luxembourg Mundipharma BV Tel: +32 2 358 54 68 [email protected] |
Czech Republic Mundipharma Gesellschaft m.b.H., organizational unit Tel: +420 296 188 338 | Hungary Medis Hungary Kft Tel: +36 23 801 028 |
Denmark Mundipharma A/S Tel: +45 45 17 48 00 | Malta Mundipharma Corporation (Ireland) Limited Tel: +353 1 206 3800 |
Germany Mundipharma GmbH Tel: +49 (0)69 506029-000 | Netherlands Mundipharma Pharmaceuticals B.V. Tel: +31 (0)33 450 82 70 [email protected] |
Estonia Medis Pharma Lithuania UAB Tel: +370 68735006 | Norway Mundipharma AS Tel: +47 67 51 89 00 |
Greece Mundipharma Corporation (Ireland) Limited Tel: +353 1 206 3800 | Austria Mundipharma Gesellschaft m.b.H. Tel: +43 (0)1 523 25 05 [email protected] |
Spain Mundipharma Pharmaceuticals, S.L. Tel: +34 91 3821870 | Poland Mundipharma Polska Sp. z o.o. Tel: +48 22 3824850 |
France MUNDIPHARMA SAS Tel: +33 1 40 65 29 29 | Portugal Mundipharma Farmacêutica Lda Tel: +351 21 901 31 62 [email protected] |
Croatia Medis Adria d.o.o Tel: +385 (0)1 230 34 46 | Romania Medis RO S.R.L. Tel: +40 744 777 258 |
Ireland Mundipharma Pharmaceuticals Limited Tel: +353 1 206 3800 | Slovenia Medis, d.o.o. Tel: +386 158969 00 |
Iceland Icepharma hf. Tel: +354 540 8000 | Slovakia Mundipharma Ges.m.b.H.-o.z. Tel: +421 2 6381 1611 [email protected] |
Italy Mundipharma Pharmaceuticals Srl Tel: +39 02 3182881 | Finland Mundipharma Oy Tel: +358 (0)9 8520 2065 |
Cyprus Mundipharma Pharmaceuticals Ltd Tel: +357 22 815656 | Sweden Mundipharma AB Tel: +46 (0)31 773 75 30 |
Latvia Medis Pharma Lithuania UAB Tel: +370 68735006 |
Date of Last Revision of this Leaflet:
Other Sources of Information
Detailed information on this medication is available on the European Medicines Agency website: http://www.ema.europa.eu/.

Important |
Read this important information before using the Pelmeg pre-filled syringe with automatic needle guard:
Do notremove the needle cap from the pre-filled syringe until you are ready for injection. Do notuse the pre-filled syringe if it has been dropped onto a hard surface. Use a new pre-filled syringe and contact your doctor or healthcare professional. Do notattempt to activate the pre-filled syringe before injection. Do notattempt to remove the transparent safety guard from the pre-filled syringe. Do notattempt to remove the label from the syringe cylinder of the pre-filled syringe before administering the injection. If you have any doubts, contact your doctor or healthcare professional. |
Step 1: Preparation | |
A | Remove the pre-filled syringe container from the box and gather the materials you need for your injection: alcohol swabs, cotton balls or gauze, band-aids, and a sharps container (not included). |
To make the injection less painful, leave the pre-filled syringe at room temperature for about 30 minutes before the injection. Wash your hands carefully with soap and water. Place the new pre-filled syringe and other materials on a clean and well-lit surface. Do notattempt to heat the syringe using a heat source such as hot water or a microwave. Do notleave the pre-filled syringe exposed to direct sunlight. Do notshake the pre-filled syringe. Keeppre-filled syringes out of the sight and reach of children. |
B | Open the container by removing the cover. Hold the pre-filled syringe by the safety guard to remove it from the tray. |
For safety reasons: Do nothold it by the plunger. Do nothold it by the needle cap. |
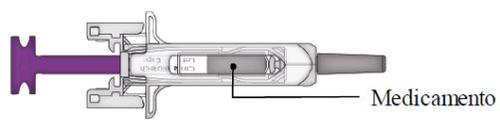
C | Examine the medication and the pre-filled syringe. |
| |
Do notuse the pre-filled syringe if:
In any of these cases, contact your doctor or healthcare professional. |
Step 2: Prepare | |
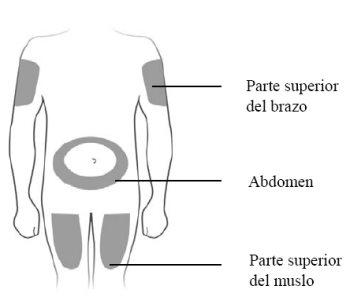
A | Wash your hands carefully. Prepare and clean the injection site. |
You can inject the medication into:
Clean the injection site with an alcohol swab. Let the skin dry. Do nottouch the injection site before injecting. Do notinject into areas where the skin is sensitive, bruised, red, or hardened. Avoid injecting into areas with scars or stretch marks. |
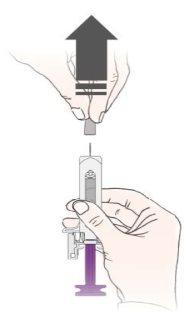
B | Carefully pull the needle cap straight off, keeping the syringe away from your body. |
|
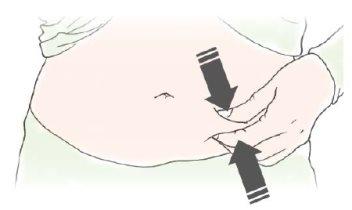
C | Pinch the injection site to create a firm surface. |
It is important to keep the skin pinched when injecting. |
Step 3: Inject | |
A | Keep the skin pinched. INSERT the needle into the skin. |
Do nottouch the clean area of the skin. |
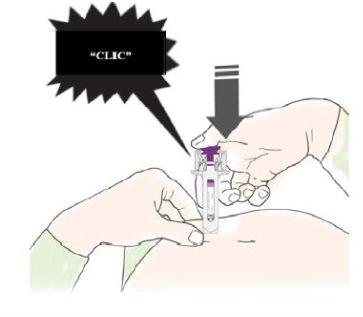
B | PRESS the plunger with gentle and constant pressure until you feel or hear a "click". Push all the way down until you hear the "click". |
It is important to press down until you hear the "click" to receive your full dose. |
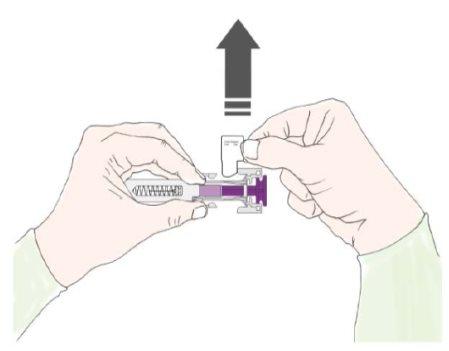
C | RELEASE the plunger. Then, REMOVE the syringe from the skin. |
After releasing the plunger, the pre-filled syringe's safety guard will safely cover the needle. Do notput the needle cap back on the used pre-filled syringe. |
For Healthcare Professionals Only The trade name and batch number of the administered medication must be clearly recorded in the patient's medical history. |
Remove and store the pre-filled syringe label.
Turn the plunger to move the syringe label to a position where you can remove it. |
Step 4: Finish | |
A | Discard the used pre-filled syringe and other materials in a sharps container. |
Medications should be disposed of in accordance with local regulations. Ask your pharmacist how to dispose of medications that are no longer needed. This will help protect the environment. Keep the syringe and sharps container out of the sight and reach of children. Do notreuse the pre-filled syringe. Do notrecycle pre-filled syringes or throw them in the trash. |
B | Examine the injection site. |
If you see blood, press a cotton ball or gauze over the injection site. Do notrub the injection site. If necessary, apply a band-aid. |
- Country of registration
- Active substance
- Prescription requiredYes
- Manufacturer
- This information is for reference only and does not constitute medical advice. Always consult a doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to PELMEG 6 mg INJECTABLE SOLUTION IN PRE-FILLED SYRINGEDosage form: INJECTABLE, 6 mgActive substance: pegfilgrastimManufacturer: Biosimilar Collaborations Ireland LimitedPrescription requiredDosage form: INJECTABLE, 6 mg of pegfilgrastim (10mg/ml)Active substance: pegfilgrastimManufacturer: Amgen Europe B.V.Prescription requiredDosage form: INJECTABLE, 6 mgActive substance: pegfilgrastimManufacturer: Amgen Europe B.V.Prescription required
Online doctors for PELMEG 6 mg INJECTABLE SOLUTION IN PRE-FILLED SYRINGE
Discuss questions about PELMEG 6 mg INJECTABLE SOLUTION IN PRE-FILLED SYRINGE, including use, safety considerations and prescription review, subject to medical assessment and local regulations.
Frequently Asked Questions