
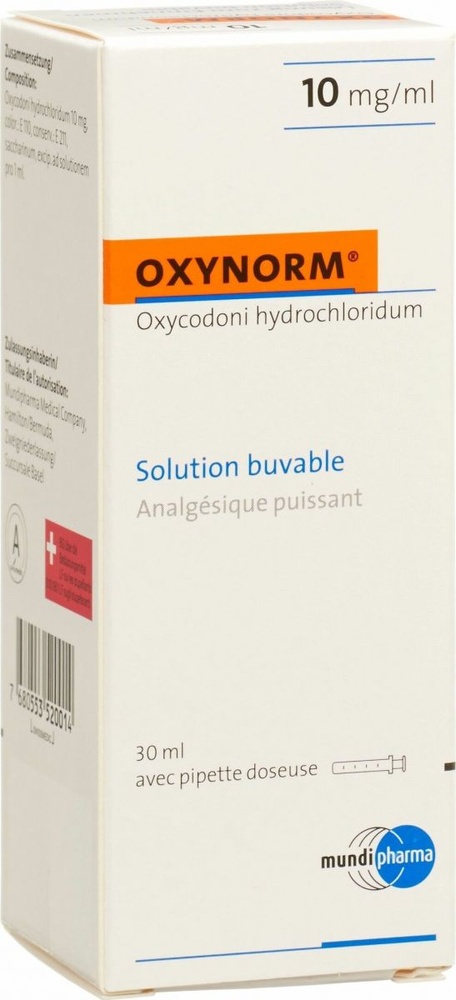
OXYNORM 10 mg/ml INJECTABLE SOLUTION AND PERFUSION SOLUTION

How to use OXYNORM 10 mg/ml INJECTABLE SOLUTION AND PERFUSION SOLUTION
Translated with AI
This page provides general information and does not replace a doctor’s consultation. Always consult a doctor before taking any medication. Seek urgent medical care if symptoms are severe.
Show originalContents of the leaflet
- Introduction
- What OxyNorm Solution for Injection and Infusion is and what it is used for
- What you need to know before you use OxyNorm Solution for Injection
- How to use OxyNorm Solution for Injection
- Possible Adverse Effects
- Storage of OxyNorm Injectable Solution
- Packaging Contents and Additional Information
Introduction
Package Leaflet: Information for the User
OxyNorm 10 mg/ml Solution for Injection and Infusion
Oxycodone, Hydrochloride
Read all of this leaflet carefully before you start taking this medicine because it contains important information for you.
- Keep this leaflet, you may need to read it again.
- If you have any further questions, ask your doctor or pharmacist.
- This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours.
- If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet. See section 4.
Contents of the pack and other information
- What OxyNorm Solution for Injection and Infusion is and what it is used for
- What you need to know before you use OxyNorm Solution for Injection and Infusion
- How to use OxyNorm Solution for Injection and Infusion
- Possible side effects
- Storage of OxyNorm Solution for Injection and Infusion
Contents of the pack and further information
1. What OxyNorm Solution for Injection and Infusion is and what it is used for
OxyNorm Solution for Injection is a strong pain reliever and belongs to the group of opioids.
OxyNorm Solution for Injection is used in adults and adolescents from 12 years of age for the relief of severe pain, which can only be adequately treated with opioid analgesics.
2. What you need to know before you use OxyNorm Solution for Injection
Do not use OxyNorm Solution for Injection if:
- you are allergic (hypersensitive) to any of the ingredients of the injection (listed in section 6 “Further information”) or have previously had an allergic reaction to taking other strong pain relievers (such as morphine or other opioids);
- you have breathing problems, such as chronic obstructive pulmonary disease, severe bronchial asthma, or respiratory depression. Symptoms may include shortness of breath, coughing, or slower or weaker breathing than expected;
- you have a head injury that causes severe headache or dizziness, as the injection may worsen these symptoms or mask the extent of the injury;
- you have a condition where your small intestine does not function properly (paralytic ileus), your stomach empties more slowly than it should (delayed gastric emptying), or you have sudden severe abdominal pain (acute abdomen);
- you have a heart problem following long-term lung disease (cor pulmonale);
Warnings and precautions
Consult your doctor or pharmacist before starting to use OxyNorm Solution for Injection if:
- you are elderly or debilitated;
- you have low thyroid activity (hypothyroidism);
- you have myxedema (a thyroid disorder, with dryness, coldness, and inflammation (swelling) of the skin, affecting the face and limbs);
- you have severe headache or dizziness, as this may indicate increased pressure in your skull;
- you have low blood pressure (hypotension);
- you have pancreatitis (which can cause severe abdominal and back pain) or problems with your gallbladder or bile duct;
- you have any obstructive or inflammatory bowel disease;
- you have colic-type abdominal pain or discomfort;
- you have an enlarged prostate gland and this causes difficulty urinating (in men);
- you have poor adrenal gland function (your adrenal gland does not work properly), for example, Addison's disease;
- you have breathing problems such as severely impaired respiratory function, chronic obstructive pulmonary disease, severe lung disease, or reduced respiratory capacity. Symptoms may include shortness of breath and coughing;
- you have kidney or liver problems;
- you have withdrawal symptoms such as agitation, anxiety, palpitations, tremors, or sweating when stopping alcohol or drug use;
- if you or a family member have a history of abuse or dependence on alcohol, prescription drugs, or illicit substances (“addiction”);
- if you smoke;
- if you have ever had problems with your mood (depression, anxiety, or personality disorder) or have received psychiatric treatment for other mental health disorders;
- if you suffer from spasms, seizures, or convulsions;
- if you suffer from dizziness or fainting;
- if you need to increase the dose of OxyNorm Solution for Injection to achieve the same level of pain relief (tolerance);
- if you are taking a type of medicine known as monoamine oxidase inhibitors (such as tranylcypromine, phenelzine, isocarboxazid, moclobemide, and linezolid), or if you have taken this type of medicine in the last two weeks;
- if you have constipation.
Breathing difficulties related to sleep
OxyNorm may cause breathing difficulties related to sleep, such as sleep apnea (pauses in breathing during sleep) and sleep-related hypoxemia (low oxygen levels in the blood). Symptoms may include pauses in breathing during sleep, nighttime awakenings due to difficulty breathing, difficulty maintaining sleep, or excessive daytime sleepiness. If you or someone else notices these symptoms, consult your doctor. Your doctor may consider reducing the dose.
If you are going to have surgery, inform the hospital doctor that you have been given this injection.
You may experience hormonal changes while taking this medicine. Your doctor may want to monitor these changes.
Opioids are not the first choice for treating non-cancer pain and are not recommended as the only treatment. In the treatment of chronic pain, other medications should be used along with opioids. Your doctor should closely monitor you and make the necessary adjustments to your dose while you are taking OxyNorm Solution for Injection and Infusion to prevent addiction and abuse.
Tolerance, dependence, and addiction
This medicine contains oxycodone, which is an opioid, and can cause dependence and/or addiction. |
This medicine contains oxycodone, which is an opioid medication. Repeated use of opioid analgesics can make the medicine less effective (you get used to it, which is known as tolerance). Repeated use of OxyNorm Solution for Injection can also cause dependence, abuse, and addiction, which can lead to a life-threatening overdose. The risk of these side effects may increase with higher doses and longer treatment duration.
Dependence or addiction can make you feel like you no longer have control over the amount of medicine you need to take or how often you need to take it. You may feel like you need to keep taking the medicine even when it no longer helps with your pain.
The risk of becoming dependent or addicted varies from person to person. You may have a higher risk of becoming dependent or addicted to OxyNorm Solution for Injection:
- if you or a family member have a history of abuse or dependence on alcohol, prescription drugs, or illicit substances (“addiction”).
- if you smoke.
- if you have ever had problems with your mood (depression, anxiety, or personality disorder) or have received psychiatric treatment for other mental health disorders.
If you notice any of the following signs while taking OxyNorm Solution for Injection, it could be a sign that you have become dependent or addicted.
- You need to take the medicine for a longer period than recommended by your doctor.
- You need to take more doses than recommended.
- You are using the medicine for reasons other than those prescribed, for example, “to calm down” or “to help you sleep”.
- You have made repeated unsuccessful attempts to stop or control the use of the medicine.
- You do not feel well when you stop taking the medicine and feel better once you take it again (“withdrawal symptoms”).
If you notice any of these signs, talk to your doctor to discuss the best treatment for you, including when it is appropriate to stop taking it and how to do so safely (see section 3, If you stop taking OxyNorm Solution for Injection).
Contact your doctor if you have severe abdominal pain that may radiate to your back, nausea, vomiting, or fever, as these may be symptoms associated with pancreatitis and biliary tract disease.
Using OxyNorm with other medicines
Concomitant use of opioids, including oxycodone, and sedative medicines, such as benzodiazepines or related drugs, increases the risk of drowsiness, respiratory difficulties (respiratory depression), coma, and can be potentially life-threatening. Therefore, concomitant use should only be considered when other treatment options are not possible.
However, if your doctor prescribes OxyNorm along with sedative medicines, the dose and duration of concomitant treatment should be limited by your doctor.
Please inform your doctor about all sedative medicines you are taking, and follow your doctor's dosage recommendations carefully. It may be useful to inform friends or family members to be aware of the signs and symptoms mentioned above. Contact your doctor if you experience such symptoms.
Tell your doctor or pharmacist if you are using, have recently used, or might use any other medicines, including those bought without a prescription. If you use this injection with other medicines, the effect of the injection or the other medicines may be altered.
The risk of side effects increases if you are taking antidepressants (such as citalopram, duloxetine, escitalopram, fluoxetine, fluvoxamine, paroxetine, sertraline, venlafaxine). These medicines may interact with oxycodone and may cause symptoms such as involuntary muscle contractions, agitation, excessive sweating, tremors, exaggerated reflexes, increased muscle tone, and body temperature above 38 °C. Contact your doctor if you experience such symptoms.
Tell your doctor or pharmacist if you are taking:
- medicines called monoamine oxidase inhibitors or have taken them in the last two weeks (see section 2 “Warnings and precautions”).
- medicines that help you sleep or stay calm (such as hypnotics or sedatives, including benzodiazepines);
- medicines for treating depression (such as paroxetine or fluoxetine);
- a herbal remedy called St. John's Wort (also known as Hypericum perforatum);
- medicines for treating psychiatric or mental disorders (such as phenothiazines or neuroleptics);
- medicines for treating epilepsy, pain, and anxiety, such as gabapentin and pregabalin;
- other strong pain relievers;
- muscle relaxants;
- medicines for treating high blood pressure;
- quinidine (a medicine for treating rapid heart rate);
- cimetidine (a medicine for stomach ulcers, indigestion, or heartburn);
- medicines for treating fungal infections (such as ketoconazole, voriconazole, itraconazole, or posaconazole);
- medicines used to treat bacterial infections (such as clarithromycin, erythromycin, or telithromycin);
- a specific type of medicine known as protease inhibitors for treating HIV (such as boceprevir, ritonavir, indinavir, nelfinavir, or saquinavir);
- rifampicin (a medicine for treating tuberculosis);
- carbamazepine (a medicine for treating spasms, seizures, or convulsions and certain pain conditions);
- phenytoin (a medicine for treating spasms, seizures, or convulsions).
- antihistamines;
- medicines for treating Parkinson's disease.
Also, tell your doctor if you have recently been given an anesthetic.
Using OxyNorm Solution for Injection with food, drinks, and alcohol
Drinking alcohol during treatment with this injection may cause drowsiness or increase the risk of serious side effects such as slow or shallow breathing and risk of respiratory arrest and loss of consciousness. It is recommended not to drink alcohol while taking OxyNorm.
You should avoid drinking grapefruit juice during treatment with this injection.
Pregnancy and breastfeeding
If you are pregnant or breastfeeding, think you may be pregnant, or plan to become pregnant, consult your doctor or pharmacist before using this medicine.
Pregnancy
You should not use this injection during pregnancy and childbirth unless your doctor has specifically told you to do so. Depending on the dose and duration of treatment with oxycodone, slow and shallow breathing (respiratory depression) or withdrawal syndrome may occur in the newborn.
Breastfeeding
This injection should not be used while breastfeeding because the active substance may pass into breast milk.
Driving and using machines
This injection may cause a number of side effects such as drowsiness that could affect your ability to drive or use machines (see section 4 for a more complete list of side effects). These are most noticeable when starting treatment with the injection or when the dose is increased. If affected, do not drive or use machines.
OxyNorm Solution for Injection contains sodium.
This medicine contains 2.78 mg of sodium (a major component of cooking salt) per milliliter. This is equivalent to 0.139% of the maximum daily intake of sodium recommended for an adult.
3. How to use OxyNorm Solution for Injection
Follow your doctor's instructions for using this medicine exactly.
Before starting treatment and periodically during treatment, your doctor will talk to you about what you can expect from using oxycodone solution for injection, when and for how long you should take it, when to contact your doctor, and when to stop taking it (see also “If you stop taking OxyNorm Solution for Injection”).
Your doctor will adjust the dose according to the intensity of your pain and your individual needs. Normally, a doctor or nurse will prepare and administer the medicine.
Do not exceed the dose recommended by your doctor. If in doubt, consult your doctor or pharmacist again.
Children under 12 years
The safety and efficacy of oxycodone solution for injection have not been sufficiently proven in children under 12 years of age. Therefore, treatment with oxycodone solution for injection is not recommended in children under 12 years of age.
Method of administration
For intravenous use, OxyNorm Solution for Injection should be diluted to a concentration of 1 mg/ml of oxycodone hydrochloride. The following solutions for infusion/injection can be used as diluents: sodium chloride 0.9% p/v solution, glucose 5% p/v solution, or water for injection.
For subcutaneous use, if necessary, OxyNorm Solution for Injection can be diluted with the following solutions for infusion/injection: sodium chloride 0.9% p/v solution, glucose 5% p/v solution, or water for injection.
Patients with liver or kidney problems
Please inform your doctor if you have liver or kidney problems so that they can prescribe alternative medication or reduce the dose depending on your situation.
If you use more OxyNorm Solution for Injection than you should, or if someone else uses your injection
In case of overdose or accidental ingestion, consult your doctor or pharmacist immediately or call the Toxicology Information Service, Telephone 91 562 04 20, indicating the medicine and the amount taken, or go to the hospital immediately.
An overdose can cause:
- a decrease in the size of your pupils
- slower and weaker breathing than normal (respiratory depression)
- drowsiness or loss of consciousness
- a decrease in muscle tone (hypotonia)
- a decrease in heart rate
- a drop in blood pressure
- difficulty breathing due to fluid in the lungs (pulmonary edema)
- a brain disorder (known as toxic leucoencephalopathy)
In severe cases, an overdose can lead to unconsciousness or even death. When you need medical attention, bring this leaflet and any remaining injection with you to show the doctor.
If you have received a high dose of the injection, under no circumstances should you engage in a situation that requires you to be alert, such as driving a car.
If you stop taking OxyNorm Solution for Injection
Do not stop using this medicine suddenly unless your doctor recommends it. If you want to stop treatment, talk to your doctor first. Your doctor will tell you how to do it, usually by gradually reducing the dose so that you do not experience unwanted effects. Withdrawal symptoms such as yawning, abnormal pupil dilation, lacrimation, nasal secretion, restlessness, anxiety, palpitations, tremors, or sweating may occur if you stop treatment with the injection abruptly.
If you have any further questions about the use of this medicine, ask your doctor or pharmacist.
4. Possible Adverse Effects
Like all medicines, this injectable can cause adverse effects, although not all people suffer from them.
This medicine may cause allergic reactions, although severe allergic reactions are rare. Inform your doctor immediately if you experience sudden shortness of breath, difficulty breathing, swelling of the eyelids, face, or lips, rash, or itching of the skin, especially if it covers your entire body.
The most serious adverse effect is when your breathing becomes slower or weaker than normal (respiratory depression, typical risk of opioid overdose).
Like all potent analgesics, there is a risk of addiction or dependence on this injectable.
Very Common
(may affect more than 1 in 10 patients)
- Constipation (your doctor will prescribe a laxative to treat this problem).
- Feeling dizzy (these symptoms should normally disappear in a few days; however, your doctor may prescribe medication to prevent dizziness if the problem continues).
- Drowsiness (this is more likely when starting to administer this medicine or when increasing the dose, but it should disappear in a few days).
- Dizziness.
- Headache.
- Itching of the skin.
Common
(may affect up to 1 in 10 patients)
- Dry mouth, loss of appetite, indigestion, abdominal pain or discomfort, diarrhea.
- Confusion, depression, feeling of unusual weakness, tremors, lack of energy, fatigue, anxiety, nervousness, difficulty sleeping, abnormal dreams and thoughts.
- Difficulty breathing, wheezing, interrupted breathing.
- Difficulty urinating.
- Rash.
- Sweating, high temperature.
Uncommon
(may affect up to 1 in 100 patients)
- A disorder in which your breathing is slower and weaker than normal (respiratory depression).
- Difficulty swallowing, belching, hiccups, gas, intestinal disorders in which the intestine does not function properly (ileus), stomach inflammation, alteration of taste, ulcers or sores in the mouth.
- Situations that may cause abnormal production of antidiuretic hormone (inappropriate antidiuretic hormone secretion syndrome).
- Feeling of dizziness or "spinning" (vertigo), hallucinations, mood changes, feeling of extreme happiness, agitation, feeling of general malaise, memory loss, difficulty speaking, decreased sensitivity to pain or touch, tingling or numbness, seizures, epileptic fits or convulsions, abnormal gait or walking style, feeling of detachment from oneself, being exceptionally hyperactive, fainting, reduced level of consciousness, unusual muscle stiffness or laxity, involuntary muscle contractions.
- Impotence, decreased sexual desire, low levels of sex hormones in the blood (hypogonadism, seen in blood tests).
- Redness of the skin.
- Dehydration, weight change, thirst, swelling of the hands, ankles, or feet.
- Dry skin.
- Disorders of tear production, blurred vision, reduction of pupil size.
- Need to increase the doses of the injectable to obtain the same level of analgesia (tolerance).
- Ringing or buzzing in the ears.
- Swelling and irritation inside the nose, nosebleeds, alteration of voice.
- Chills.
- Chest pain.
- Inability to empty the bladder completely.
- Worsening of liver function tests (observed in a blood test).
- Withdrawal symptoms (see section 3 "If you stop treatment with OxyNorm injectable solution").
Rare
(may affect up to 1 in 1,000 patients)
- Feeling of fainting, especially when standing up.
- Low blood pressure.
- Hives.
Not Known
(Frequency cannot be estimated from available data)
- Sudden whistling when breathing, difficulty breathing, swelling of the eyelids, face, or lips, skin rash or itching, especially those that cover the entire body.
- Tooth loss.
- Abdominal pain like colic or discomfort.
- A problem that affects a valve in the intestine, which can cause intense pain in the upper abdomen (Oddi's sphincter dysfunction).
- Blockage of bile flow from the liver. This can cause itching of the skin, yellowish skin, dark urine, and light-colored stools.
- Absence of menstrual periods.
- Increased sensitivity to pain.
- Aggression.
- Prolonged treatment with OxyNorm during pregnancy may produce withdrawal syndrome in newborns with a threat to their life. Symptoms seen in babies included irritability, hyperactivity, and abnormal sleep pattern, crying with high-pitched screams, tremors, sickly appearance, diarrhea, and no weight gain.
- Sleep apnea (interruptions of breathing during sleep).
Reporting of Adverse Effects
If you experience any type of adverse effects, consult your doctor, pharmacist, or nurse, even if they are possible adverse effects that do not appear in this prospectus. You can also report them directly through the Spanish Pharmacovigilance System for Human Use Medicines: www.notificaRAM.es.
By reporting adverse effects, you can contribute to providing more information on the safety of this medicine.
5. Storage of OxyNorm Injectable Solution
Keep out of sight and reach of children. Accidental overdose in a child is dangerous and can be fatal. Store this medicine in a safe and closed place, where other people cannot access it. It can cause serious harm and be fatal to people when not prescribed to them.
Do not use the injectable after the expiration date that appears on the packaging after CAD. The expiration date is the last day of the month indicated. For example, CAD 08 2020 means that you should not take the medicine after the last day of that month, i.e., August 2020.
This medicine does not require special temperature conditions for storage. Store in the original packaging to protect it from light. However, once the ampoule is opened, the injection should be administered immediately. Any unused part should be discarded immediately.
Medicines should not be thrown away through drains or into the trash. Deposit the packaging and medicines you no longer need at the SIGRE point in the pharmacy. In case of doubt, ask your pharmacist how to dispose of the packaging and medicines you no longer need. This way, you will help protect the environment.
6. Packaging Contents and Additional Information
Composition of OxyNorm Injectable Solution
The active ingredient is oxicodone hydrochloride. Each milliliter contains 10 mg of oxicodone hydrochloride.
The other components are:
- monohydrate citric acid,
- sodium citrate,
- sodium chloride,
- diluted hydrochloric acid,
- sodium hydroxide,
- water for injectable preparations.
Appearance of the Product and Packaging Contents
The injectable is a clear, colorless solution, presented in transparent glass ampoules. It is available in 1 ml, 2 ml, or 20 ml of solution (containing 10 mg, 20 mg, or 200 mg of oxicodone hydrochloride, respectively).
The ampoules are packaged in boxes.
Only some package sizes may be marketed.
Marketing Authorization Holder and Manufacturer
Marketing Authorization Holder
Mundipharma Pharmaceuticals, S.L.
Bahía de Pollensa, 11
28042 Madrid
Spain
Tel. 91 382 1870
Manufacturer
Mundipharma DC B.V.
Leusderend 16
3832 RC Leusden
Netherlands
or
Fidelio Healthcare Limburg GmbH
Mundipharmastrasse 2,
65549 Limburg
Germany
This medicine is authorized in the Member States of the European Economic Area under the name OxyNorm:
Austria OxyNorm Injektionslösung
Ireland OxyNorm solution for injection or infusion
Spain OxyNorm 10 mg/ml injectable and infusion solution
Date of the Last Revision of this Prospectus:March 2025.
Detailed information about this medicine is available on the website of the Spanish Agency for Medicines and Health Products (AEMPS) (http://www.aemps.gob.es/)
- Country of registration
- Average pharmacy price7.68 EUR
- Active substance
- Prescription requiredYes
- Manufacturer
- This information is for reference only and does not constitute medical advice. Always consult a doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to OXYNORM 10 mg/ml INJECTABLE SOLUTION AND PERFUSION SOLUTIONDosage form: MODIFIED-RELEASE TABLET, 10 mgActive substance: oxycodoneManufacturer: Sandoz Farmaceutica S.A.Prescription requiredDosage form: MODIFIED-RELEASE TABLET, 20 mgActive substance: oxycodoneManufacturer: Sandoz Farmaceutica S.A.Prescription requiredDosage form: MODIFIED-RELEASE TABLET, 40 mgActive substance: oxycodoneManufacturer: Sandoz Farmaceutica S.A.Prescription required
Online doctors for OXYNORM 10 mg/ml INJECTABLE SOLUTION AND PERFUSION SOLUTION
Discuss questions about OXYNORM 10 mg/ml INJECTABLE SOLUTION AND PERFUSION SOLUTION, including use, safety considerations and prescription review, subject to medical assessment and local regulations.
Frequently Asked Questions












