NIVESTIM 48 MU/0.5 ml INJECTABLE SOLUTION OR FOR INFUSION


How to use NIVESTIM 48 MU/0.5 ml INJECTABLE SOLUTION OR FOR INFUSION
Translated with AI
This page provides general information and does not replace a doctor’s consultation. Always consult a doctor before taking any medication. Seek urgent medical care if symptoms are severe.
Show originalContents of the leaflet
Introduction
Package Leaflet: Information for the User
Nivestim 12MU/0.2ml solution for injection and infusion
Nivestim 30MU/0.5ml solution for injection and infusion
Nivestim 48MU/0.5ml solution for injection and infusion
filgrastim
Read all of this leaflet carefully before you start using this medicine because it contains important information for you.
- Keep this leaflet, you may need to read it again.
- If you have any further questions, ask your doctor, pharmacist, or nurse.
- This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours.
- If you get any side effects, talk to your doctor, pharmacist, or nurse. This includes any possible side effects not listed in this leaflet. See section 4.
Contents of the pack
- What is Nivestim and what is it used for
- What you need to know before you use Nivestim
- How to use Nivestim
- Possible side effects
- Storage of Nivestim
- Contents of the pack and other information
1. What is Nivestim and what is it used for
Nivestim is a white blood cell growth factor (granulocyte-colony stimulating factor) and belongs to a group of medicines called cytokines. Growth factors are proteins that are produced naturally in the body, but can also be produced using genetic engineering for use as a medicine. Nivestim works by making the bone marrow produce more white blood cells.
A reduction in the number of white blood cells (neutropenia) can occur for several reasons and makes your body less able to fight infections. Nivestim stimulates the bone marrow to produce new white blood cells quickly.
Nivestim can be used:
- to increase the number of white blood cells after chemotherapy to help prevent infections;
- to increase the number of white blood cells after a bone marrow transplant to help prevent infections;
- before high-dose chemotherapy to make the bone marrow produce more stem cells, which can be collected and given back to you after treatment. These cells can be collected from you or a donor. The stem cells will then return to the bone marrow and produce blood cells;
- to increase the number of white blood cells if you have severe chronic neutropenia to help prevent infections;
- to help reduce the risk of infection in patients with advanced HIV infection.
2. What you need to know before you use Nivestim
Do not use Nivestim
- if you are allergic to filgrastim or any of the other ingredients of this medicine (listed in section 6).
Warnings and precautions
Talk to your doctor, pharmacist, or nurse before starting treatment with Nivestim.
Tell your doctor before starting treatment if you:
- have sickle cell anaemia, as Nivestim may cause sickle cell crisis;
- have osteoporosis (bone disease).
Tell your doctor immediately during treatment with Nivestim if:
- you have signs of a sudden allergic reaction, such as rash, itching, or hives on the skin, swelling of the face, lips, tongue, or other parts of the body, wheezing, or difficulty breathing, as these may be signs of a severe allergic reaction (hypersensitivity);
- you experience swelling of the face or ankles, blood in the urine, or brown-coloured urine, or if you notice that you are urinating less often than usual (glomerulonephritis);
- you experience pain in the upper left side of the abdomen (abdominal pain), pain under the left side of the rib cage or at the top of the left shoulder (these may be symptoms of an enlarged spleen [splenomegaly] or a possible rupture of the spleen);
- you notice unusual bleeding or bruising (these may be symptoms of a decrease in platelets in the blood [thrombocytopenia], with a reduced ability of the blood to clot).
- Rarely, inflammation of the aorta (the large blood vessel that carries blood from the heart to the rest of the body) has been reported in patients with cancer and in healthy donors. Symptoms may include fever, abdominal pain, general malaise, back pain, and increased inflammatory markers. Tell your doctor if you experience these symptoms.
Loss of response to filgrastim
If you experience a loss of response or if you do not achieve a response to treatment with filgrastim, your doctor will investigate the causes, including whether you have developed antibodies that may neutralize the activity of filgrastim.
Your doctor may want to closely monitor you, see section 4 of the package leaflet.
If you are a patient with severe chronic neutropenia, you may be at risk of developing blood cancer (leukaemia, myelodysplastic syndrome [MDS]). Talk to your doctor about the risks of developing blood cancer and the tests that should be performed. If you develop or are likely to develop blood cancers, you should not use Nivestim unless your doctor says so.
If you are a stem cell donor, you must be between 16 and 60 years old.
Be careful with other products that stimulate white blood cells
Nivestim belongs to a group of medicines that stimulate the production of white blood cells. Your doctor should always record the exact product you are using.
Using Nivestim with other medicines
Tell your doctor or pharmacist if you are taking, have recently taken, or might take any other medicines.
Pregnancy and breastfeeding
Nivestim has not been studied in pregnant or breastfeeding women.
Nivestim should not be used during pregnancy.
It is important that you tell your doctor:
- if you are pregnant or breastfeeding;
- if you think you may be pregnant; or
- if you plan to become pregnant.
If you become pregnant during treatment with Nivestim, tell your doctor.
Unless your doctor tells you otherwise, you must stop breastfeeding if you use Nivestim.
Driving and using machines
Nivestim has a minor influence on your ability to drive and use machines. This medicine may cause dizziness. It is recommended that you wait and see how you feel after administration of Nivestim before driving or operating machinery.
Nivestim contains sodium
This medicine contains less than 1 mmol of sodium (23 mg) per dose of 0.6 mg/ml or 0.96 mg/ml; i.e., it is essentially “sodium-free”.
Nivestim contains sorbitol
This medicine contains 50 mg of sorbitol in each ml.
Sorbitol is a source of fructose. If you (or your child) have hereditary fructose intolerance (HFI), a rare genetic disorder, you must not receive this medicine. Patients with HFI cannot break down fructose, which may cause serious side effects.
Talk to your doctor before receiving this medicine if you (or your child) have HFI or if your child cannot take sweet foods or drinks because they cause nausea, vomiting, or unpleasant effects such as bloating, stomach cramps, or diarrhoea.
3. How to use Nivestim
Follow the instructions for administration of this medicine exactly as told by your doctor. If you are unsure, consult your doctor, pharmacist, or nurse again.
How is Nivestim administered and how much should you take?
Nivestim is usually administered once a day as an injection into the tissue just under the skin (known as a subcutaneous injection). It can also be administered once a day as a slow injection into a vein (known as an intravenous infusion). The usual dose varies depending on your condition and weight. Your doctor will tell you how much Nivestim to take.
Patient with bone marrow transplant after chemotherapy:
You will usually receive your first dose of Nivestim at least 24 hours after chemotherapy and at least 24 hours after receiving your bone marrow transplant.
You or the people caring for you may be taught how to administer subcutaneous injections so that you can continue treatment at home. However, you should not attempt to do this unless you have been properly trained by a healthcare professional.
How long will you need to take Nivestim?
You will need to take Nivestim until your white blood cell count is normal. You will have regular blood tests to monitor the number of white blood cells in your body. Your doctor will tell you how long you need to take Nivestim.
Use in children
Nivestim is used to treat children who are receiving chemotherapy or who have a low white blood cell count (neutropenia). The dose in children receiving chemotherapy is the same as for adults.
If you use more Nivestim than you should
Do not increase the dose that your doctor has prescribed. If you think you have injected more than the dose that you should, contact your doctor as soon as possible.
If you forget to use Nivestim
If you have missed an injection, or if you have injected a lower dose, contact your doctor as soon as possible. Do not take a double dose to make up for missed doses.
If you have any further questions on the use of this product, ask your doctor, pharmacist, or nurse.
4. Possible side effects
Like all medicines, this medicine can cause side effects, although not everybody gets them.
Tell your doctor immediatelyduring treatment:
- if you experience an allergic reaction, including weakness, low blood pressure, difficulty breathing, swelling of the face (anaphylaxis), skin rash, itchy skin rash (urticaria), swelling of the face, lips, mouth, tongue, or throat (angioedema), and shortness of breath (dyspnoea);
- if you experience cough, fever, and difficulty breathing (dyspnoea), as this may be a sign of acute respiratory distress syndrome (ARDS);
- if you experience kidney damage (glomerulonephritis). Kidney damage has been observed in patients receiving filgrastim. Contact your doctor immediately if you notice swelling of the face or ankles, blood in the urine, or brown-coloured urine, or if you notice that you are urinating less often than usual;
- if you experience any of the following side effects or a combination of them:
- swelling, which may be related to urinating less often, difficulty breathing, swelling, and a feeling of fullness in the abdomen, and a general feeling of tiredness. These symptoms usually develop very quickly.
These may be symptoms of a condition called “capillary leak syndrome”, which causes blood to leak from small blood vessels into other parts of your body and requires urgent medical attention.
- If you experience a combination of the following symptoms:
- fever, or chills, or feeling very cold, rapid heartbeat, confusion or disorientation, difficulty breathing, severe pain or discomfort, and sweaty skin.
These could be symptoms of a condition called “sepsis” (also called “blood poisoning”), a severe infection with a systemic inflammatory response that can be life-threatening and requires urgent medical attention.
- if you experience pain in the upper left side of the abdomen (abdominal pain), pain under the left side of the rib cage or at the top of the left shoulder (these may be symptoms of an enlarged spleen [splenomegaly] or a possible rupture of the spleen);
- if you are being treated for severe chronic neutropenia and have blood in the urine (haematuria). Your doctor will perform regular urine tests if you experience this side effect or if protein is found in your urine (proteinuria).
A common side effect of using filgrastim is muscle or bone pain (musculoskeletal pain), which can be prevented by taking usual pain-relieving medicines (analgesics). In patients undergoing stem cell or bone marrow transplantation, graft-versus-host disease (GVHD) may occur. This is a reaction of the donor cells against the patient receiving the transplant; signs and symptoms include rashes on the palms of the hands or soles of the feet, and ulcers and sores in the mouth, gut, liver, skin, eyes, lungs, vagina, and joints.
In healthy donors of stem cells, an increase in white blood cells (leucocytosis) and a decrease in platelets (thrombocytopenia) may be observed. This reduces the ability of your blood to clot. These effects will be monitored by your doctor.
Very common side effects(may affect more than 1 in 10 people):
- decrease in platelets, which reduces the ability of the blood to clot (thrombocytopenia)
- low red blood cell count (anaemia)
- headache
- diarrhoea
- vomiting
- nausea
- unusual hair loss or thinning (alopecia)
- fatigue
- irritation and swelling of the lining of the digestive tract, which runs from the mouth to the anus (mucosal inflammation)
- fever (pyrexia)
Common side effects(may affect up to 1 in 10 people):
- inflammation of the lungs (bronchitis)
- infection of the upper respiratory tract
- infection of the urinary tract
- decreased appetite
- sleeping problems (insomnia)
- dizziness
- decreased sensitivity, especially in the skin (hypoesthesia)
- tingling or numbness of the hands or feet (paraesthesia)
- low blood pressure (hypotension)
- high blood pressure (hypertension)
- cough
- coughing up blood (haemoptysis)
- pain in the mouth and throat (oropharyngeal pain)
- nosebleeds (epistaxis)
- constipation
- mouth pain
- enlargement of the liver (hepatomegaly)
- rash
- redness of the skin (erythema)
- muscle cramp
- pain when urinating (dysuria)
- chest pain
- pain
- general weakness (asthenia)
- feeling unwell (malaise)
- swelling of the hands and feet (peripheral oedema)
- increase in certain enzymes in the blood
- changes in blood biochemistry tests
- transfusion reaction
Uncommon side effects(may affect up to 1 in 100 people):
- increase in white blood cells in the blood (leucocytosis)
- allergic reaction (hypersensitivity)
- rejection of the bone marrow transplant (graft-versus-host disease)
- high levels of uric acid in the blood, which can cause gout (hyperuricaemia)
- liver damage caused by blockage of the small veins of the liver (veno-occlusive disease)
- the lungs not working properly, causing shortness of breath (respiratory failure)
- swelling or fluid in the lungs (pulmonary oedema)
- inflammation of the lungs (interstitial lung disease)
- abnormal chest X-rays (pulmonary infiltrates)
- bleeding in the lungs (pulmonary haemorrhage)
- lack of oxygen in the lungs (hypoxia)
- irregular skin rash (maculopapular rash)
- a disease that causes bones to lose density, making them weaker, more fragile, and prone to breaking (osteoporosis)
- reaction at the injection site
Rare side effects(may affect up to 1 in 1,000 people):
- severe pain in the bones, chest, intestines, or joints (sickle cell crisis)
- sudden, life-threatening allergic reactions (anaphylactic reaction)
- swelling and pain in the joints, similar to gout (pseudogout)
- a change in the way your body regulates body fluids, which can result in swelling (fluid volume changes)
- inflammation of the blood vessels in the skin (cutaneous vasculitis)
- painful, inflamed, and dark red ulcers on the extremities and sometimes on the face and neck, accompanied by fever (Sweet's syndrome)
- worsening of rheumatoid arthritis
- unusual changes in urine
- decrease in bone density
- inflammation of the aorta (the large blood vessel that carries blood from the heart to the rest of the body), see section 2.
- formation of blood cells outside the bone marrow (extramedullary haematopoiesis).
Reporting of side effects
If you get any side effects, talk to your doctor, pharmacist, or nurse. This includes any possible side effects not listed in this leaflet. You can also report side effects directly via the national reporting system listed in Appendix V. By reporting side effects, you can help provide more information on the safety of this medicine.
5. Storage of Nivestim
Keep this medicine out of the sight and reach of children.
Do not use this medicine after the expiry date which is stated on the carton and on the label of the pre-filled syringe after EXP. The expiry date refers to the last day of the month shown.
Store and transport refrigerated (between 2°C and 8°C). Do not freeze. Keep the pre-filled syringe in the outer carton to protect it from light.
The syringe can be removed from the refrigerator and stored at room temperature for a single period of up to 15 days (but not above 25°C).
Do not use this medicine if you notice that the contents of the syringe are cloudy or contain particles.
Medicines should not be disposed of via wastewater or household waste. Ask your pharmacist how to dispose of medicines no longer required. These measures will help protect the environment.
6. Container Contents and Additional Information
Composition of Nivestim
- The active substance is filgrastim. Each ml contains 60 million units [MU] (600 µg) or 96 million units ([MU] (960 µg) of filgrastim.
- Nivestim 12 MU/0.2 ml solution for injection/infusion: each pre-filled syringe contains 12 million units (MU), 120 µg of filgrastim in 0.2 ml (corresponding to 0.6 mg/ml
- Nivestim 30 MU/0.5 ml solution for injection/infusion: each pre-filled syringe contains 30 million units (MU), 300 µg of filgrastim in 0.5 ml (corresponding to 0.6 mg/ml).
- Nivestim 48 MU/0.5 ml solution for injection/infusion: each pre-filled syringe contains 48 million units (MU), 480 µg of filgrastim in 0.5 ml (corresponding to 0.96 mg/ml
- The other components are glacial acetic acid, sodium hydroxide, sorbitol E420, polysorbate 80, and water for injectable preparations.
Appearance of the Product and Container Contents
Nivestim is a clear and colorless solution for injection/infusion supplied in a pre-filled syringe with a stainless steel needle and a needle shield. The needle shield contains epoxyprene, a derivative of natural rubber latex that may come into contact with the needle.
Nivestim is available in packs of 1, 5, 8, or 10 syringes per pack. Not all pack sizes may be marketed.
Marketing Authorisation Holder
Pfizer Europe MA EEIG
Boulevard de la Plaine 17
1050 Bruxelles
Belgium
Manufacturer
Hospira Zagreb d.o.o.
Prudnicka cesta 60
10291 Prigorje Brdovecko
Croatia
For further information on this medicinal product, please contact the local representative of the Marketing Authorisation Holder:
België/Belgique/Belgien Luxembourg/Luxemburg Pfizer NV/SA Tél/Tel: +32 (0)2 554 62 11 | Lietuva Pfizer Luxembourg SARL filialas Lietuvoje Tel: +370 52 51 4000 |
| Magyarország Pfizer Kft. Tel.: +36 1 488 37 00 |
Ceská republika Pfizer, spol. s r.o. Tel: +420-283-004-111 | Malta Drugsales Ltd Tel: +356 21 419 070/1/2 |
Danmark Pfizer ApS Tlf.: +45 44 20 11 00 | Nederland Pfizer bv Tel: +31 (0)800 63 34 636 |
Deutschland PFIZER PHARMA GmbH Tel: +49 (0)30 550055-51000 | Norge Pfizer AS Tlf: +47 67 52 61 00 |
Eesti Pfizer Luxembourg SARL Eesti filiaal Tel: +372 666 7500 | Österreich Pfizer Corporation Austria Ges.m.b.H. Tel: +43 (0)1 521 15-0 |
Ελλάδα Pfizer ΕΛΛ?Σ A.E. Τηλ: +30 210 6785 800 | Polska Pfizer Polska Sp. z o.o. Tel.: +48 22 335 61 00 |
España Pfizer, S.L. Tel: +34 91 490 99 00 | Portugal Laboratórios Pfizer, Lda. Tel: +351 21 423 55 00 |
France Pfizer Tél: +33 (0)1 58 07 34 40 | România Pfizer România S.R.L. Tel: +40 (0)21 207 28 00 |
Hrvatska Pfizer Croatia d.o.o. Tel: +385 1 3908 777 | Slovenija Pfizer Luxembourg SARL Pfizer, podružnica za svetovanje s podrocja farmacevtske dejavnosti, Ljubljana Tel: +386 (0)1 52 11 400 |
Ireland Pfizer Healthcare Ireland Unlimited Company Tel: +1800 633 363 (toll free) Tel: +44 (0) 1304 616161 | Slovenská republika Pfizer Luxembourg SARL, organizacná zložka Tel: +421–2–3355 5500 |
Ísland Icepharma hf. Sími: +354 540 8000 | Suomi/Finland Pfizer Oy Puh/Tel: +358 (0)9 430 040 |
Italia Pfizer S.r.l. Tel: +39 06 33 18 21 | Sverige Pfizer AB Tel: +46 (0)8 550 520 00 |
Κúπρος Pfizer ΕΛΛΑΣ Α.Ε. (Cyprus Branch) Τηλ: +357 22 817690 | Latvija Pfizer Luxembourg SARL filiale Latvija Tel: + 371 670 35 775 |
Date of Last Revision of this Leaflet: {MM/AAAA}.
Detailed information on this medicinal product is available on the European Medicines Agency web site: https://www.ema.europa.eu.
-------------------------------------------------------------------------------------------------------
Instructions for Self-administration by the Patient
This section contains information on how to administer Nivestim to yourself. It is essential that you do not attempt to administer the injection without your doctor or nurse having first explained how to do it. It is also crucial that you dispose of the syringes in a puncture-proof container. If you are unsure about self-administering the injection or have any questions, consult your doctor or nurse.
How do I inject Nivestim?
Nivestim is usually administered once a day by injection, typically into the tissue under the skin. This is known as a subcutaneous injection.
If you learn how to administer the injection yourself, you will no longer have to wait at home for a nurse to come or go to the hospital or clinic every day to have your injection administered.
You will need to administer your injection at approximately the same time each day. The most suitable places for injection are:
- The front of your thighs
- The abdomen, except for the area around the navel
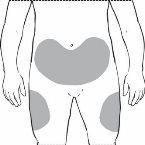
It is best to change the injection site every day to avoid the risk of painful sensation at any one site.
Equipment Required for Administration:
The following items are needed for subcutaneous injection:
- A new pre-filled syringe of Nivestim
- A puncture-proof container for safe disposal of used syringes
- Antiseptic wipes (if recommended by your doctor or nurse)
How to Administer the Subcutaneous Injection of Nivestim:
- Try to administer the injection at approximately the same time each day.
- Take the Nivestim pre-filled syringe out of the refrigerator.
- Take the blister pack containing the pre-filled syringe out of the carton. When the carton contains blister packs with more than one pre-filled syringe, cut the blister pack with one pre-filled syringe along the perforation, return the remaining blister packs with pre-filled syringes to the carton, and put the carton back in the refrigerator.
- Open the blister pack by removing the blister pack cover. Take the pre-filled syringe out of the blister pack by grasping the syringe body.
Check the syringe to ensure that the needle shield covers the syringe body. Do notpush the needle shield over the needle cap before injection. This may activate or lock the needle shield. If the needle shield covers the needle, it means it has been activated.
Check that the solution is clear, colorless, and practically free from visible particles. Do notinspect the product through the plastic of the safety device.
Check the expiration date on the label to ensure that the medicine has not passed its expiration date.
Make sure you have a puncture-proof container nearby.
Allow the pre-filled syringe to reach room temperature (approximately 25 °C). This will take 15-30 minutes.
- Do notremove the needle cap from the syringe while allowing the pre-filled syringe to reach room temperature.
- Do notshake the syringe.
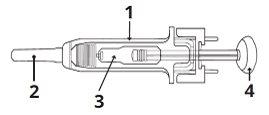
1 | Needle shield |
2 | Needle cap |
3 | Medicine |
4 | Piston |
- Do not use the Nivestim syringe if:
- The carton is open or damaged.
- The needle shield is missing, has been removed, or has been activated.
- The medicine is cloudy or has changed color or the liquid has particles floating in it.
- Any part of the pre-filled syringe appears cracked or broken or liquid has leaked from the syringe.
- The pre-filled syringe has been dropped. The pre-filled syringe may be broken even if you cannot see the break.
- The needle cap is missing or not properly positioned.
- The expiration date printed on the label has passed.
In all the above cases, discard the pre-filled syringe and use a new pre-filled syringe.
- Find a comfortable place to administer the injection and check the dose that you have been prescribed.
- Wash your hands thoroughly with soap and water.
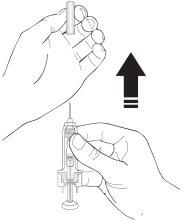
- Take the pre-filled syringe by the needle shield body with the needle cap pointing upwards.
- Remove the needle cap from the syringe by holding the syringe body and pulling the needle cap straight off and away from your body with care, without twisting it. Discard the needle cap. Do not attempt to put the needle cap back on the syringe. Do not push the piston, touch the needle, or shake the syringe.
- The syringe is now ready for use. You may see a small air bubble in the syringe. You do not need to expel the air bubble before injecting the solution. Injecting the solution with an air bubble is harmless.
- Decide where you will administer the injection - look for a place on the front of your abdomen or on the front of your thighs. Choose a different injection site each time. Do not choose an area that is sensitive, red, damaged, or has a scar. Clean this area of skin with an antiseptic wipe.
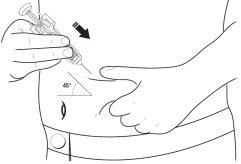
- Pinch a large area of skin, being careful not to touch the area you cleaned.
12 With your other hand, hold the pre-filled syringe like a pencil. Use a quick "dart-like" motion to insert the needle into the skin at an angle of approximately 45 degrees, as shown.
- Gently pull back the piston to check if you have accidentally injected into a blood vessel. If you see blood in the syringe, remove the needle and insert it into another location. Holding the skin pinched, slowly and evenly press the piston until the syringe is empty.
- After injecting the solution, remove the needle from your skin.
- Make sure the syringe shield covers the needle according to the instructions for the active or passive syringe shield as indicated below.
- Do not attempt to put the needle cap back on the syringe. Put the syringe in a puncture-proof container.
- Keep used syringes out of the reach and sight of children.
- Neverput used syringes in the normal household waste bin.
Remember
Most people can learn to administer the subcutaneous injection by themselves, but if you find it very difficult, do not hesitate to ask for help and advice from your doctor or nurse.
Using the Active UltraSafe Needle Guard forNivestim 12MU/0.2ml Solution for Injection and Infusion
The pre-filled syringes have an Active UltraSafe Needle Guard to protect you from needlestick injury. When handling a pre-filled syringe, keep your hands behind the needle.
- Administer the injection using the technique described above.
- After completing the injection, slide the needle into the safety shield until the needle is fully covered (it will click).

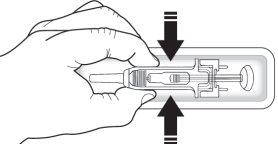
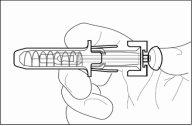
Using the Passive UltraSafe Needle Guard forNivestim 30MU/0.5ml Solution for Injection/Infusion and Nivestim 48MU/0.5ml Solution for Injection/Infusion
The pre-filled syringes have a Passive UltraSafe Needle Guard to protect you from needlestick injury. When handling a pre-filled syringe, keep your hands behind the needle.
- Administer the injection using the technique described above.
- Press the piston while holding the syringe with your fingers until the full dose has been administered. The passive syringe shield WILL NOT activate until the FULL dose has been administered.

- Remove the needle from your skin; the piston will move and allow the syringe to move up until the needle is covered and locked in place.
--------------------------------------------------------------------------------------------------------------------
This information is intended for healthcare professionals only:
Nivestim does not contain preservatives: in view of the possible risk of microbiological contamination, Nivestim syringes are for single use only.
Accidental exposure to freezing temperatures for up to 24 hours does not affect the stability of Nivestim. Frozen pre-filled syringes can be thawed and then refrigerated for future use. If exposure has been longer than 24 hours or if the pre-filled syringes have been frozen more than once, then Nivestim MUST NOT be used.
Nivestim must not be diluted with sodium chloride solutions. This medicinal product must not be mixed with other medicinal products except those mentioned below. Filgrastim diluted may be adsorbed to plastic or glass materials, except if diluted as mentioned below.
Nivestim can be diluted, if necessary, in a 5% glucose solution. It is not recommended to dilute to final concentrations below 0.2 MU (2 µg) per milliliter. The solution must be inspected visually before use. Only clear solutions without particles should be used. In patients treated with filgrastim diluted to concentrations below 1.5 MU/ml (15 µg) per milliliter, human serum albumin (HSA) must be added to a final concentration of 2 mg/ml.
Example: if the final injection volume is 20 ml and the total dose of filgrastim is below 30 MU (300 µg), 0.2 ml of a 20% human serum albumin solution (200 mg/ml) must be added. When diluted in a 5% glucose solution, Nivestim is compatible with glass and various plastics, including polyvinyl chloride, polyolefin (a copolymer of polypropylene and polyethylene), and polypropylene.
After dilution: it has been demonstrated that, during use, the diluted solution for infusion remains physically and chemically stable for 24 hours at 2 - 8°C. From a microbiological point of view, the product should be used immediately. If not used immediately, the in-use storage times and conditions are the responsibility of the user and normally should not exceed 24 hours at 2-8°C, unless the dilution has been made in validated and controlled aseptic conditions.
- Country of registration
- Active substance
- Prescription requiredYes
- Manufacturer
- This information is for reference only and does not constitute medical advice. Always consult a doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to NIVESTIM 48 MU/0.5 ml INJECTABLE SOLUTION OR FOR INFUSIONDosage form: INJECTABLE, 12 IU/0.2 mlActive substance: filgrastimManufacturer: Accord Healthcare S.L.U.Prescription requiredDosage form: INJECTABLE, 0.3 mg / prefilled syringeActive substance: filgrastimManufacturer: Accord Healthcare S.L.U.Prescription requiredDosage form: INJECTABLE, 0.3 mg / prefilled syringeActive substance: filgrastimManufacturer: Accord Healthcare S.L.U.Prescription required
Online doctors for NIVESTIM 48 MU/0.5 ml INJECTABLE SOLUTION OR FOR INFUSION
Discuss questions about NIVESTIM 48 MU/0.5 ml INJECTABLE SOLUTION OR FOR INFUSION, including use, safety considerations and prescription review, subject to medical assessment and local regulations.
Frequently Asked Questions