
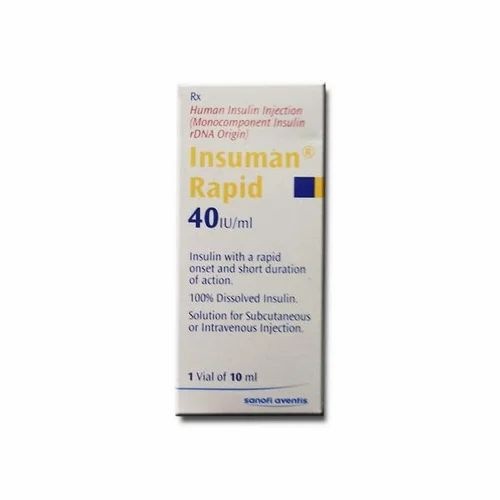
INSUMAN RAPID 40 U/ml INJECTABLE SOLUTION IN A VIAL

How to use INSUMAN RAPID 40 U/ml INJECTABLE SOLUTION IN A VIAL
Translated with AI
This page provides general information and does not replace a doctor’s consultation. Always consult a doctor before taking any medication. Seek urgent medical care if symptoms are severe.
Show originalContents of the leaflet
Introduction
Package Leaflet: Information for the User
Insuman Rapid 40 UI/ml Solution for Injection in a Vial
Human Insulin
Read all of this leaflet carefully before you start using this medicine because it contains important information for you.
- Keep this leaflet, you may need to read it again.
- If you have any further questions, ask your doctor, pharmacist, or nurse.
- This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours.
- If you get any side effects, talk to your doctor, pharmacist, or nurse. This includes any possible side effects not listed in this leaflet. See section 4.
Contents of the Package Leaflet:
- What is Insuman Rapid and what is it used for
- What you need to know before you use Insuman Rapid
- How to use Insuman Rapid
- Possible side effects
- Storage of Insuman Rapid
- Contents of the pack and other information
1. What is Insuman Rapid and what is it used for
Insuman Rapid contains human insulin as the active substance, which is produced by a biotechnological process and is identical to the insulin produced by the human body.
Insuman Rapid is a fast-acting and short-duration insulin solution.
Insuman Rapid is used to reduce high blood sugar levels in patients with diabetes mellitus who require insulin treatment. Diabetes mellitus is a disease in which your body does not produce enough insulin to control your blood sugar levels. Insuman Rapid can also be used to treat hyperglycemic coma (coma caused by very high blood sugar levels) and ketoacidosis (increase in blood acid levels because your body breaks down fat instead of sugar), as well as to control blood sugar levels before, during, and after surgery.
2. What you need to know before you use Insuman Rapid
Do not use Insuman Rapid
If you are allergic to insulin or any of the other ingredients of this medicine (listed in section 6).
Warnings and precautions
Consult your doctor, pharmacist, or nurse before starting to use Insuman Rapid.
Follow strictly the instructions on dosage, monitoring (blood and urine tests), diet, and physical activity (work and exercise) that you have established with your doctor.
Consult your doctor if you are allergic to this medicine or to human insulins.
Special patient groups
If you have liver or kidney problems or if you are elderly, consult your doctor, as you may need a lower dose of insulin.
Travel
Before traveling, consult your doctor. You may need to consult about:
- the availability of insulin in the country you are traveling to,
- insulin reserves, syringes, etc.,
- proper storage of insulin during travel,
- meal and insulin administration schedules during travel,
- possible effects of time zone changes,
- new health risks in the countries you will visit,
- what to do in emergency situations when you feel unwell or become ill.
Illnesses and injuries
The management of your diabetes may require special care in the following situations:
- If you are ill or suffer a severe injury, your blood sugar levels may rise (hyperglycemia).
- If you do not eat enough, your blood sugar levels may drop too low (hypoglycemia).
In most cases, you will need a doctor. Make sure to consult a doctor immediately.
If you have type 1 diabetes (insulin-dependent diabetes mellitus), do not stop taking your insulin and follow a sufficient carbohydrate diet. Always inform the people who care for you or treat you that you need insulin.
Some patients with long-standing type 2 diabetes mellitus and previous heart disease or stroke who were treated with pioglitazone and insulin developed heart failure. Inform your doctor as soon as possible if you experience symptoms of heart failure such as unusual shortness of breath or rapid weight gain or localized swelling (edema).
Other medicines and Insuman Rapid
Some medicines can change your blood sugar levels (either lowering or raising them, depending on the situation). In each case, it may be necessary to adjust your insulin dose to avoid blood sugar levels that are too low or too high. Be careful when starting to take another medicine and also when stopping it.
Tell your doctor or pharmacist if you are using, have recently used, or might use any other medicines.
Ask your doctor before using a medicine if it can affect your blood sugar levels and what measures you should take, if necessary.
Among the medicines that can cause a drop in your blood sugar levels (hypoglycemia) are:
- all other diabetes medicines,
- angiotensin-converting enzyme (ACE) inhibitors (used to treat certain heart diseases or high blood pressure),
- disopyramide (used to treat certain heart diseases),
- fluoxetine (used to treat depression),
- fibrates (used to lower blood lipid levels),
- monoamine oxidase inhibitors (MAOIs) (used to treat depression),
- pentoxifylline, propoxyphene, salicylates (such as aspirin, used to relieve pain and reduce fever),
- antibiotics of the sulfonamide group.
Among the medicines that can cause an increase in your blood sugar levels (hyperglycemia) are:
- corticosteroids (such as "cortisone", used to treat inflammation),
- danazol (a medicine that acts on ovulation),
- diazoxide (used to treat hypertension),
- diuretics (used to treat hypertension or excess fluid retention),
- glucagon (a pancreatic hormone used to treat severe hypoglycemia),
- isoniazid (used to treat tuberculosis),
- estrogens and progestogens (such as birth control pills used for contraception),
- phenothiazine derivatives (used to treat psychiatric diseases),
- somatotropin (growth hormone),
- sympathomimetic medicines (such as epinephrine [adrenaline], salbutamol, terbutaline used to treat asthma),
- thyroid hormones (used to treat thyroid gland dysfunction),
- protease inhibitors (used to treat HIV),
- atypical antipsychotic medicines (such as clozapine, olanzapine).
Your blood sugar levels may rise or fall if you use:
- beta-blockers (used to treat hypertension),
- clonidine (used to treat hypertension),
- lithium salts (used to treat psychiatric diseases).
Pentamidine (used to treat some parasitic infections) can cause hypoglycemia, which can sometimes be followed by hyperglycemia.
Beta-blockers, like other sympatholytic medicines (such as clonidine, guanethidine, and reserpine), can mask or completely suppress the early warning symptoms that could help you recognize hypoglycemia.
If you are not sure if you are using any of these medicines, ask your doctor or pharmacist.
Insuman Rapid with alcohol
Your blood sugar levels may rise or fall if you consume alcohol.
Pregnancy and breastfeeding
If you are pregnant or breastfeeding, or think you may be pregnant or are planning to have a baby, ask your doctor or pharmacist for advice before using this medicine.
Tell your doctor if you are planning to become pregnant or if you are already pregnant. Your insulin administration regimen may need to be changed during pregnancy and after delivery. Very careful control of your diabetes and prevention of hypoglycemia are important for the health of your baby. However, there is no experience with the use of Insuman Rapid in pregnant women.
If you are breastfeeding, you may need to adjust your insulin dose and diet.
Driving and using machines
Your ability to concentrate or react may be reduced if:
- you have hypoglycemia (low blood sugar levels)
- you have hyperglycemia (high blood sugar levels)
you have vision problems.
Be aware of this possible problem, considering all situations that may pose a risk to you or others (such as driving a vehicle or using machines). You should ask your doctor for advice about driving if:
- you have frequent episodes of hypoglycemia,
- the early warning symptoms of hypoglycemia have decreased or disappeared.
Important information about some of the ingredients of Insuman Rapid
This medicine contains less than 23 mg of sodium per dose; this is essentially "sodium-free".
3. How to use Insuman Rapid
Dose
Follow exactly the administration instructions of this medicine indicated by your doctor or pharmacist. In case of doubt, consult your doctor or pharmacist again.
Depending on your lifestyle and the results of your blood sugar (glucose) tests and previous insulin treatment, your doctor:
- will determine the dose of Insuman Rapid you need each day,
- will indicate when you should analyze your blood sugar levels and if you need to perform urine tests,
- will indicate when you may need to inject a higher or lower dose of Insuman Rapid.
Many factors can influence your blood sugar levels. You should know these factors so that you can react correctly to changes in your blood sugar levels and avoid them becoming too high or too low. See the box at the end of this leaflet for more information.
Frequency of administration
Insuman Rapid is injected under the skin 15 to 20 minutes before a meal.
Method of administration
Insuman Rapid is a solution for injection under the skin or, in exceptional circumstances, into a vein (blood vessel).
Your doctor will show you which area of the skin to inject Insuman Rapid into. With each injection, you should change the injection site within the specific area of skin you are using.
Administration of insulin into a vein, for example to treat severe hyperglycemia or ketoacidosis, requires experience and special safety precautions, so it should be performed in a hospital or similar setting.
Do not use Insuman Rapid in insulin pumps. There are special insulin preparations for use in these devices. Do not use it in peristaltic pumps with silicone tubes either.
How to handle the vials
Insuman Rapid contains 40 UI of insulin per ml. Only syringes for injection designed for this insulin concentration (40 UI per ml) should be used. The syringes for injection should not contain other medicines or residues of them (e.g., heparin residues).
Before extracting the first dose of insulin, you must remove the removable safety cap from the vial.
Do not use Insuman Rapid if the solution is not transparent, colorless, free of visible solid particles, and has a watery consistency.
Do not shake the vial vigorously, as foam may form. The foam can make it difficult to measure the correct dose.
Special precautions before injection
Before injection, eliminate all air bubbles. Make sure the insulin is not contaminated with alcohol or other disinfectants, or with other substances. Do not mix the insulin with any other medicine, except with human insulin preparations as detailed below.
Insuman Rapid can be mixed with all human insulin preparations, EXCEPT those specifically designed for insulin pumps. Similarly, it MUST NOT be mixed with animal insulins or insulin analogs.
Your doctor will tell you if you need to mix human insulin preparations. If you need to inject a mixture, put Insuman Rapid in the syringe for injection before putting the other insulin. Inject immediately after mixing. Do not mix insulins of different concentrations (e.g., 100 UI/ml and 40 UI/ml).
If you use more Insuman Rapid than you should
-If you have injected too much Insuman Rapid, your blood sugar levels may become very low (hypoglycemia). Check your blood sugar levels frequently. In general, to prevent hypoglycemia, you should eat more and control your blood sugar levels. For more information on treating hypoglycemia, see the box at the end of this leaflet.
If you forget to use Insuman Rapid
- If you have forgotten a dose of Insuman Rapid or if you have not injected enough insulin, your blood sugar levels may rise (hyperglycemia). Check your blood sugar levels frequently. For more information on treating hyperglycemia, see the box at the end of this leaflet.
- Do not take a double dose to make up for forgotten doses.
If you stop using Insuman Rapid
This could lead to severe hyperglycemia (very high blood sugar levels) and ketoacidosis (increase in blood acid levels because your body breaks down fat instead of sugar). Do not stop your treatment with Insuman Rapid without consulting a doctor; he will tell you what to do.
If you have any further questions on the use of this product, ask your doctor, pharmacist, or nurse.
Insulin confusion
You should always check the insulin label before each injection to avoid confusion between Insuman Rapid and other insulins.
4. Possible side effects
Like all medicines, this medicine can cause side effects, although not everybody gets them.
More serious side effects
Side effects reported rarely(may affect up to 1 in 100 people)
- Severe allergic reactions with low blood pressure(shock)
Side effects reported with an unknown frequency(frequency cannot be estimated from the available data)
- The most common side effect is hypoglycemia (low blood sugar levels).Severe hypoglycemia can cause brain damage and can be life-threatening. For more information on side effects due to low or high blood sugar levels, see the box at the end of this leaflet.
- Severe allergic reactions to insulinmay occur, which can be life-threatening. These reactions to insulin or excipients can cause widespread skin reactions (rash and itching all over the body), severe skin or mucous membrane swelling (angioedema), difficulty breathing, a drop in blood pressure with rapid heartbeat and sweating.
Other side effects
Side effects reported frequently(may affect up to 1 in 10 people)
- Edema
Treatment with insulin can cause temporary water retention in the body with swelling of the ankles and feet.
- Injection site reactions
Side effects reported rarely
- Urticaria at the injection site (itchy rash)
Other side effects reported with an unknown frequency
- Sodium retention
- Eye reactions
A significant change (improvement or worsening) in your blood sugar control may temporarily alter your vision. If you have proliferative retinopathy (an eye disease related to diabetes), severe hypoglycemic attacks can cause temporary loss of vision.
- Skin changes at the injection site (lipodystrophy)
If you inject insulin too frequently into the same skin area, the fatty tissue under that area may shrink or thicken. The insulin you inject into that area may not work well. Changing the injection site with each injection will help prevent these skin changes.
- Skin and allergic reactions
Moderate allergic reactions may occur at the injection site (such as redness, intense pain when injecting, itching, urticaria, swelling, or inflammation). These reactions can also spread around the injection site. Most mild reactions to insulins resolve on their own within a few days or weeks.
- Antibodies to insulin
Treatment with insulin can cause your body to produce antibodies against insulin (substances that act against insulin). However, this will only rarely require a change in your insulin dose.
Reporting of side effects
If you experience any side effects, talk to your doctor, pharmacist, or nurse, even if it is possible side effects not listed in this leaflet. You can also report side effects directly through the national reporting system listed in Appendix V. By reporting side effects, you can help provide more information on the safety of this medicine.
5. Storage of Insuman Rapid
Keep this medicine out of the sight and reach of children.
Do not use this medicine after the expiry date which is stated on the carton and on the label of the vial after "EXP". The expiry date refers to the last day of the month.
Unopened vials:
Store in a refrigerator (between 2°C and 8°C). Do not freeze. Do not place Insuman Rapid near the freezer compartment or next to a cooling pack.
Keep the vial in the outer carton to protect it from light.
Opened vials:
Once in use, the vial may be stored for a maximum of 4 weeks in the outer carton at a temperature not above 25°C and protected from direct heat (e.g. next to a heater) or direct light (direct sunlight or next to a lamp). Do not use the vial after this period. It is recommended to note the date of the first use on the label.
Medicines should not be disposed of via wastewater or household waste. Ask your pharmacist how to dispose of medicines no longer required. This will help to protect the environment.
6. Package Contents and Additional Information
Composition of Insuman Rapid
- The active substance is human insulin. One ml of Insuman Rapid contains 100 IU (International Units) of the active substance human insulin.
- The other ingredients are: metacresol, sodium dihydrogen phosphate dihydrate, glycerol, sodium hydroxide (see section 2, "Important information about some of the ingredients of Insuman Rapid"), hydrochloric acid (for pH adjustment) and water for injections.
Appearance and Packaging of the Product
Insuman Rapid is a clear, colorless, aqueous solution for injection, free from visible particles.
Insuman Rapid is available in vials containing 10 ml of solution (400 IU). It is available in packs of 1 and 5 vials of 10 ml. Not all pack sizes may be marketed.
Marketing Authorization Holder and Manufacturer
Sanofi-Aventis Deutschland GmbH
D-65926 Frankfurt am Main
Germany
For further information, please contact the local representative of the Marketing Authorization Holder.
Belgium/Belgique/Belgien Sanofi Belgium Tel: +32 (0)2 710 54 00 | Luxembourg/Luxemburg Sanofi Belgium Tel: +32 (0)2 710 54 00 (Belgique/Belgien) |
Bulgaria SANOFI BULGARIA EOOD Tel: +359 (0)2 970 53 00 | Hungary SANOFI-AVENTIS Zrt. Tel: +36 1 505 0050 |
Czech Republic sanofi-aventis, s.r.o. Tel: +420 233 086 111 | Malta Sanofi Malta Ltd. Tel: +356 21493022 |
Denmark Sanofi A/S Tel: +45 45 16 70 00 | Netherlands sanofi-aventis Netherlands B.V. Tel: +31 20 245 4000 |
Germany Sanofi-Aventis Deutschland GmbH Tel: 0800 52 52 010 Tel from abroad: +49 69 305 21 131 | Norway sanofi-aventis Norge AS Tel: +47 67 10 71 00 |
Estonia sanofi-aventis Estonia OÜ Tel: +372 627 34 88 | Austria sanofi-aventis GmbH Tel: +43 1 80 185 – 0 |
Greece sanofi-aventis AEBE Tel: +30 210 900 16 00 | Poland sanofi-aventis Sp. z o.o. Tel: +48 22 280 00 00 |
Spain sanofi-aventis, S.A. Tel: +34 93 485 94 00 | Portugal Sanofi - Produtos Farmacêuticos, Lda Tel: +351 21 35 89 400 |
France sanofi-aventis France Tel: 0 800 222 555 Call from abroad: +33 1 57 63 23 23 Croatia sanofi-aventis Croatia d.o.o. Tel: +385 1 600 34 00 | Romania Sanofi Romania SRL Tel: +40 (0) 21 317 31 36 |
Ireland sanofi-aventis Ireland Ltd. T/A SANOFI Tel: +353 (0) 1 403 56 00 | Slovenia sanofi-aventis d.o.o. Tel: +386 1 560 48 00 |
Iceland Vistor hf. Tel: +354 535 7000 | Slovakia sanofi-aventis Pharma Slovakia s.r.o. Tel: +421 2 33 100 100 |
Italy Sanofi S.p.A. Tel: 800 13 12 12 (technical inquiries) 800 536389 (other inquiries) | Finland Sanofi Oy Tel: +358 (0) 201 200 300 |
Cyprus sanofi-aventis Cyprus Ltd. Tel: +357 22 871600 | Sweden Sanofi AB Tel: +46 (0)8 634 50 00 |
Latvia sanofi-aventis Latvia SIA Tel: +371 67 33 24 51 | United Kingdom Sanofi Tel: +44 (0) 845 372 7101 |
Lithuania UAB “SANOFI-AVENTIS LIETUVA” Tel: +370 5 2755224 | |
The last revision of this leaflet was in
Other sources of information
Detailed information on this medicine is available on the European Medicines Agency web site: http://www.ema.europa.eu/
HYPERGLYCEMIA AND HYPOGLYCEMIA
Always carry some sugar (at least 20 grams) with you
Always carry some information that indicates you are diabetic
HYPERGLYCEMIA (high blood sugar levels)
If you have very high blood sugar levels (hyperglycemia),you may not have injected enough insulin.
Why do you get hyperglycemia?
Some examples are:
- you have not injected your insulin or have not injected enough, or if its effect has weakened, for example, due to incorrect storage,
- you are doing less exercise than usual, are under stress (emotional distress, nervousness), or are suffering from an injury, surgery, infection, or fever,
- you are using or have used certain medications (see section 2, "Other medications and Insuman Rapid").
Warning signs of hyperglycemia
Thirst, increased need to urinate, fatigue, dry skin, redness of the face, loss of appetite, low blood pressure, rapid heartbeat, and the presence of glucose and ketone bodies in the urine. Stomach pain, deep and rapid breathing, drowsiness, or even loss of consciousness may be signs of a serious condition (ketoacidosis) due to lack of insulin.
What to do if you have hyperglycemia
You should check your blood sugar and ketone levels in your urine as soon as you experience any of these symptoms.Severe hyperglycemia or ketoacidosis should always be treated by a doctor, usually in a hospital.
HYPOGLYCEMIA (low blood sugar levels)
If your blood sugar levels drop too low, you may lose consciousness. Severe hypoglycemia can cause a heart attack or brain damage and can be life-threatening. You should usually be able to recognize when your blood sugar levels are dropping too low to take the necessary measures.
Why do you get hypoglycemia?
Some examples are:
- you inject too much insulin,
225
- you miss meals or delay them,
- you do not eat enough, or eat foods that contain fewer carbohydrates than usual (sugar and substances similar to sugar are called carbohydrates; however, artificial sweeteners are NOT carbohydrates),
you lose carbohydrates due to vomiting or diarrhea,
- you drink alcohol, especially if you are not eating much,
- you are doing more exercise than usual or a different type of physical activity,
- you are recovering from an injury, surgery, or other types of stress,
- you are recovering from an illness or fever,
- you are using or have used certain medications (see section 2, "Other medications and Insuman Rapid").
It is also more likely to get hypoglycemia if:
- you have just started insulin treatment or changed to another insulin preparation,
- your blood sugar levels are almost normal or are unstable,
- you change the injection site (e.g., from the thigh to the upper arm),
or if you have a severe kidney or liver disease, or other diseases such as hypothyroidism.
Warning signs of hypoglycemia
- In your body
Examples of symptoms that indicate your blood sugar levels are dropping too low or too quickly: sweating, damp and sticky skin, anxiety, rapid heartbeat, high blood pressure, palpitations, and irregular heartbeat. These symptoms often occur before symptoms of low blood sugar in the brain appear.
- In your brain
Examples of symptoms that indicate low blood sugar in the brain: headaches, intense hunger, nausea, vomiting, fatigue, drowsiness, sleep disturbances, restlessness, aggressive behavior, concentration problems, altered reactions, depression, confusion, speech disorders (sometimes, complete loss of speech), visual disturbances, tremors, paralysis, tingling sensations (paresthesias), numbness and tingling sensations around the mouth, dizziness, loss of self-control, feeling of helplessness, convulsions, loss of consciousness.
The first warning signs of hypoglycemia ("warning symptoms") may change, weaken, or be absent if
- you are elderly, have had diabetes for a long time, or suffer from a certain type of nerve disease (autonomic diabetic neuropathy),
- you have recently experienced a hypoglycemic episode (e.g., the day before) or if it develops gradually,
- you have almost normal or at least much improved blood sugar levels,
- you have recently changed from an animal insulin to a human insulin like Insuman,
- you are using or have used certain medications (see section 2, "Other medications and Insuman Rapid").
In this case, you may experience severe hypoglycemia (and even lose consciousness) before you realize the problem. Always be familiar with your warning symptoms. If necessary, more frequent blood sugar testing can help identify mild hypoglycemic episodes that might otherwise go unnoticed. If you are not sure you can recognize your warning symptoms, avoid situations (such as driving a car) that could put you or others at risk due to hypoglycemia.
What to do if you have hypoglycemia?
- Do not inject insulin. Immediately consume 10 to 20 grams of sugar, such as glucose, sugar cubes, or a sugary drink. Note: Artificial sweeteners and sugar-free products do not help treat hypoglycemia.
- Then, eat something that will increase your blood sugar levels in the long term (such as bread or pasta). Your doctor or nurse should have discussed this with you beforehand.
- If hypoglycemia recurs, take another 10 to 20 grams of sugar.
- Consult a doctor immediately if you are unable to control hypoglycemia or if it recurs.
Tell your family, friends, or people close to you: If you are unable to swallow or lose consciousness, you will need an injection of glucose or glucagon (a medication that increases blood sugar levels). These injections are justified even if you are not sure you have hypoglycemia.
It is recommended to check your blood sugar levels immediately after consuming glucose to confirm that you actually have hypoglycemia.
- Country of registration
- Active substance
- Prescription requiredYes
- Manufacturer
- This information is for reference only and does not constitute medical advice. Always consult a doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to INSUMAN RAPID 40 U/ml INJECTABLE SOLUTION IN A VIALDosage form: INJECTABLE, 100 U/mlActive substance: insulin (human)Manufacturer: Novo Nordisk A/SPrescription requiredDosage form: INJECTABLE, 100 U/mlActive substance: insulin (human)Manufacturer: Novo Nordisk A/SPrescription requiredDosage form: INJECTABLE, 100 IU/mLActive substance: insulin (human)Manufacturer: Lilly S.A.Prescription required
Online doctors for INSUMAN RAPID 40 U/ml INJECTABLE SOLUTION IN A VIAL
Discuss questions about INSUMAN RAPID 40 U/ml INJECTABLE SOLUTION IN A VIAL, including use, safety considerations and prescription review, subject to medical assessment and local regulations.
Frequently Asked Questions















