
IMULDOSA 45 mg Injectable Solution in Pre-filled Syringe

How to use IMULDOSA 45 mg Injectable Solution in Pre-filled Syringe
Translated with AI
This page provides general information and does not replace a doctor’s consultation. Always consult a doctor before taking any medication. Seek urgent medical care if symptoms are severe.
Show originalContents of the leaflet
Introduction
Package Leaflet: Information for the Patient
IMULDOSA 45 mg solution for injection in pre-filled syringe
ustekinumab
This medicinal product is subject to additional monitoring, which will allow for quick identification of new safety information. Healthcare professionals are asked to report any suspected adverse reactions. See section 4.8, which includes information on how to report adverse reactions.
Read all of this leaflet carefully before you start using this medicine, because it contains important information for you.
This leaflet has been written for the person taking the medicine. If you are the parent or caregiver of a child who will be given IMULDOSA, please read this information carefully.
- Keep this leaflet, you may need to read it again.
- If you have any further questions, ask your doctor or pharmacist.
- This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours.
- If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet. See section 4.
Contents of the pack
- What is IMULDOSA and what is it used for
- What you need to know before you use IMULDOSA
- How to use IMULDOSA
- Possible side effects
- Storage of IMULDOSA
- Contents of the pack and other information
1. What is IMULDOSA and what is it used for
What is IMULDOSA
IMULDOSA contains the active substance “ustekinumab”, a monoclonal antibody. Monoclonal antibodies are proteins that identify and bind specifically to certain proteins in the body.
IMULDOSA belongs to a group of medicines called “immunosuppressants”. These medicines work by weakening part of the immune system.
What is IMULDOSA used for
IMULDOSA is used to treat the following inflammatory diseases:
- Plaque psoriasis - in adults and children aged 6 years and older
- Psoriatic arthritis - in adults
- Moderate to severe Crohn's disease - in adults
Plaque psoriasis
Plaque psoriasis is a skin disease that causes inflammation affecting the skin and nails. IMULDOSA reduces inflammation and other signs of the disease.
IMULDOSA is used in adults with moderate to severe plaque psoriasis who cannot use ciclosporin, methotrexate, or phototherapy, or where these treatments do not work.
IMULDOSA is used in children and adolescents aged 6 years and older with moderate to severe plaque psoriasis who are not able to tolerate phototherapy or other systemic therapies or where these treatments do not work.
Psoriatic arthritis
Psoriatic arthritis is an inflammatory disease of the joints, which is usually accompanied by psoriasis. If you have active psoriatic arthritis, you will first receive other medicines. If you do not respond well to these medicines, you may be treated with IMULDOSA to:
- Reduce the signs and symptoms of your disease.
- Improve your physical function.
- Reduce damage to your joints.
Crohn's disease
Crohn's disease is an inflammatory disease of the intestine. If you have Crohn's disease, you will first be given other medicines. If you do not respond adequately or do not tolerate these medicines, you may be given IMULDOSA to reduce the signs and symptoms of your disease.
2. What you need to know before you use IMULDOSA
Do not use IMULDOSA
- If you are allergic to ustekinumabor any of the other ingredients of this medicine (listed in section 6).
- If you have an active infectionthat your doctor thinks is important.
If you are not sure if anyof the above applies to you, talk to your doctor or pharmacist before using IMULDOSA.
Warnings and precautions
Talk to your doctor or pharmacist before starting IMULDOSA. Your doctor will check how you are before each treatment. Make sure you tell your doctor about any illness you have before each treatment. Your doctor will also ask if you have recently been near someone who may have tuberculosis. Your doctor will examine you and do a test to detect tuberculosis before you use IMULDOSA. If your doctor thinks you are at risk of tuberculosis, you may be given medicines to treat it.
Look out for serious side effects
IMULDOSA may cause serious side effects, including allergic reactions and infections. You should be aware of certain signs of illness while you are using IMULDOSA. See the complete list of these side effects in “Serious side effects” in section 4.
Tell your doctor before using IMULDOSA:
- If you have ever had an allergic reaction to IMULDOSA.Check with your doctor if you are not sure.
- If you have ever had any type of cancer– this is because immunosuppressants like IMULDOSA weaken part of the immune system. This may increase the risk of having cancer.
- If you have received treatment for psoriasis with other biologics (a medicine produced from a biological source and usually given by injection)– the risk of having cancer may be higher.
- If you have had a recent infection.
- If you have any new or changing lesionswithin the area of psoriasis or on intact skin.
- If you are taking any other treatment for psoriasis and/or psoriatic arthritis– such as any other immunosuppressant or phototherapy (when your body is treated with a type of ultraviolet light (UV)). These treatments may also weaken part of the immune system. It has not been studied whether these treatments can be used together with IMULDOSA. However, it may increase the likelihood of suffering from diseases related to a weaker immune system.
- If you are receiving or have ever received allergy shots– it is not known if IMULDOSA can affect these treatments.
- If you are 65 years of age or older– you are more likely to get infections.
If you are not sure if you have any of these conditions, talk to your doctor or pharmacist before using IMULDOSA.
Some patients have experienced lupus-like reactions during treatment with ustekinumab, including cutaneous lupus or lupus-like syndrome. Talk to your doctor immediately if you experience a red, raised, and scaly skin rash, sometimes with a darker border, in areas of skin exposed to the sun or if accompanied by joint pain.
Heart attacks and strokes
In a study in patients with psoriasis treated with ustekinumab, heart attacks and strokes have been observed. Your doctor will periodically check your risk factors for heart disease and stroke to ensure they are being treated properly. Seek medical attention immediately if you experience chest pain, weakness, or unusual sensation on one side of the body, facial paralysis, or abnormalities in speech or vision.
Children and adolescents
IMULDOSA is not recommended for use in children under 6 years of age with psoriasis or in children under 18 years of age with psoriatic arthritis, Crohn's disease, or ulcerative colitis, as it has not been studied in this age group.
Using IMULDOSA with other medicines, vaccines
Tell your doctor or pharmacist:
- If you are using, have recently used, or might use other medicines.
- If you have been vaccinated recently or are going to have a vaccination.Certain types of vaccines (live vaccines) must not be given while you are using IMULDOSA.
- If you received IMULDOSA during pregnancy, inform your baby's doctor about your treatment with IMULDOSA before your baby receives any vaccination, including live vaccines such as the BCG vaccine (used to prevent tuberculosis).Live vaccines are not recommended for your baby in the first 12 months after birth if you received IMULDOSA during pregnancy, unless your baby's doctor recommends otherwise.
Pregnancy and breastfeeding
- If you are pregnant or think you may be pregnant or are planning to have a baby, ask your doctor for advice before taking this medicine.
- No increased risk of birth defects has been observed in babies exposed to Imuldosa in the womb.However, there is limited experience with Imuldosa in pregnant women. Therefore, it is preferable to avoid the use of Imuldosa during pregnancy.
- If you are a woman of childbearing age, you are advised to avoid becoming pregnant and to use adequate contraceptive measures while using Imuldosa and for at least 15 weeks after the last treatment with Imuldosa.Imuldosa may pass through the placenta to the fetus. If you received Imuldosa during pregnancy, your baby may have a higher risk of getting an infection.
- It is important that you inform your baby's doctors and other healthcare professionals if you received Imuldosa during your pregnancy before your baby receives any vaccination.Live vaccines, such as the BCG vaccine (used to prevent tuberculosis), are not recommended for your baby in the first 12 months after birth if you received Imuldosa during pregnancy, unless your baby's doctor recommends otherwise.
- Ustekinumab may be excreted in breast milk in very small amounts.If you are breastfeeding or plan to breastfeed, talk to your doctor. You and your doctor will decide whether you should breastfeed or use Imuldosa. Do not do both.
Driving and using machines
IMULDOSA has no or negligible influence on the ability to drive and use machines.
IMULDOSA contains polisorbate
IMULDOSA contains 0.02 mg of polysorbate 80 per unit volume, equivalent to 0.02 mg per 45 mg dose.
Polysorbates may cause allergic reactions. Tell your doctor if you have known allergies.
3. How to use IMULDOSA
IMULDOSA should be used under the guidance and supervision of a doctor with experience in the treatment of the conditions for which IMULDOSA is indicated.
Always follow exactly the administration instructions of this medicine given by your doctor. If you are not sure, ask your doctor. Ask your doctor when you should have the injections and about follow-up appointments.
How much IMULDOSA is given
Your doctor will decide how much IMULDOSA you need to use and the duration of treatment.
Adults aged 18 years and older
Psoriasis or psoriatic arthritis
- The recommended starting dose is 45 mg of IMULDOSA.Patients who weigh more than 100 kilograms (kg) may start with a dose of 90 mg instead of 45 mg.
- After the initial dose, you will take the next dose 4 weeks later and then every 12 weeks.The following doses are usually the same as the starting dose.
Crohn's disease
- During treatment, your doctor will give you the first dose of approximately 6 mg/kg of IMULDOSA through a vein in your arm (intravenous infusion).After the initial dose, you will receive the next dose of 90 mg of IMULDOSA 8 weeks later and then every 12 weeks, by injection under the skin (“subcutaneously”).
- In some patients, after the first injection under the skin, 90 mg of IMULDOSA will be given every 8 weeks.Your doctor will decide when you should receive the next dose.
Children and adolescents aged 6 years and older
Psoriasis
- Your doctor will tell you the correct dose for you, including the amount (volume) of IMULDOSA to inject to give the correct dose.The correct dose for you will depend on your body weight at the time of each dose.
- If you weigh less than 60 kg, there is no dosage form of IMULDOSA for children with a body weight below 60 kg, and you should use other ustekinumab products.
- If you weigh between 60 kg and 100 kg, the recommended dose is 45 mg of IMULDOSA.
- If you weigh more than 100 kg, the recommended dose is 90 mg of IMULDOSA.
- After the initial dose, you will receive the next dose 4 weeks later, and then every 12 weeks.
How IMULDOSA is given
- IMULDOSA is given by injection under the skin (“subcutaneously”).At the start of your treatment, medical staff or nurses may inject IMULDOSA for you.
- However, you and your doctor may decide that you can inject IMULDOSA yourself.In this case, you will be trained on how to inject IMULDOSA yourself.
- For instructions on how to inject IMULDOSA, see “Administration instructions” at the end of this leaflet.
Talk to your doctor if you have any questions about how to inject yourself.
If you use more IMULDOSA than you should
If you have used or been given too much IMULDOSA, talk to your doctor or pharmacist immediately. Always carry the medicine box with you, even if it is empty.
If you forget to use IMULDOSA
If you miss a dose, talk to your doctor or pharmacist. Do not take a double dose to make up for forgotten doses.
If you stop using IMULDOSA
Stopping IMULDOSA is not dangerous. However, if you stop using it, your symptoms may come back.
If you have any other questions about using this medicine, ask your doctor or pharmacist.
4. Possible Adverse Effects
Like all medicines, this medicine can cause adverse effects, although not all people suffer from them.
Severe Adverse Effects
Some patients may have severe adverse effects that may require urgent treatment.
Allergic Reactions – these may require urgent treatment. Contact your doctor or get emergency medical help immediately if you notice any of the following signs.
- Severe allergic reactions ("anaphylaxis") are rare in the population using IMULDOSA (may affect up to 1 in 1,000 people). The signs include:
- difficulty breathing and swallowing
- low blood pressure, which can cause dizziness or mild headaches
- swelling of the face, lips, mouth, or throat.
- Common signs of an allergic reaction include skin rash and hives (these may affect up to 1 in 100 people).
In rare cases, allergic reactions at the lung level and lung inflammation have been reported in patients treated with ustekinumab. Inform your doctor immediately if you have symptoms such as cough, difficulty breathing, and fever.
If you have a severe allergic reaction, your doctor may decide that you should not use IMULDOSA again.
Infections – these may require urgent treatment. Contact your doctor immediately if you notice any of these signs.
- Nose or throat infections and the common cold are frequent (may affect up to 1 in 10 people).
- Chest infections are uncommon (may affect up to 1 in 100 people).
- Inflammation of the tissues under the skin ("cellulitis") is uncommon (may affect up to 1 in 100 people).
- Herpes (a type of painful rash with blisters) are uncommon (may affect up to 1 in 100 people).
IMULDOSA may affect your ability to fight infections. Some of them could become serious and be caused by viruses, fungi, bacteria (including tuberculosis) or parasites, and include infections that occur mainly in people with a weakened immune system (opportunistic infections). Opportunistic infections of the brain (encephalitis, meningitis), lungs, and eyes have been reported in patients receiving treatment with ustekinumab.
You should watch for signs of infection while using IMULDOSA. These include:
- fever, flu-like symptoms, night sweats, weight loss
- feeling tired or having difficulty breathing; cough that does not go away
- having hot, red, and painful skin or having a painful skin rash with blisters
- burning when urinating
- diarrhea
- visual impairment or loss of vision
- headache, neck stiffness, photosensitivity, nausea, or confusion.
Contact your doctor immediately if you notice any of these signs of infection, as they may be signs of infections such as chest infections, skin infections, herpes, or opportunistic infections that could have serious complications. You should also inform your doctor if you have any type of infection that does not go away or comes back. Your doctor may decide that you should not use IMULDOSA until the infection goes away. Also, contact your doctor if you have any open cuts or ulcers that could become infected.
Shedding of the skin – increased redness and shedding of the skin on a large surface of the body may be symptoms of erythrodermic psoriasis or exfoliative dermatitis, which are serious skin disorders. If you notice any of these symptoms, you should inform your doctor immediately.
Other Adverse Effects
Frequent Adverse Effects(may affect up to 1 in 10 people)
- Diarrhea
- Nausea
- Vomiting
- Feeling tired
- Feeling dizzy
- Headache
- Itching ("pruritus")
- Back, muscle, or joint pain
- Sore throat
- Redness and pain at the injection site
- Sinusitis
Uncommon Adverse Effects(may affect up to 1 in 100 people)
- Dental infections
- Vaginal yeast infections
- Depression
- Nasal congestion or stuffiness
- Bleeding, bruising, hardening, swelling, and itching at the injection site
- Feeling weak
- Drooping eyelid and sinking of the muscles on one side of the face ("facial paralysis" or "Bell's palsy"), which is normally temporary
- A change in psoriasis with redness and new small, yellow or white skin blisters, sometimes accompanied by fever (pustular psoriasis)
- Shedding of the skin (skin exfoliation)
- Acne
Rare Adverse Effects(may affect up to 1 in 1,000 people)
- Redness and shedding of the skin on a large surface of the body, which can cause itching or pain (exfoliative dermatitis). Similar symptoms may develop as a natural change in psoriasis symptoms (erythrodermic psoriasis)
- Inflammation of small blood vessels, which can cause a skin rash with small red or purple bumps, fever, or joint pain (vasculitis)
Very Rare Adverse Effects(may affect up to 1 in 10,000 people)
- Blisters on the skin, which can be red and cause itching and pain (bullous pemphigoid).
- Lupus-like syndrome (red, raised, and scaly skin rash in sun-exposed areas, possibly accompanied by joint pain).
Reporting of Adverse Effects
If you experience any type of adverse effect, consult your doctor or pharmacist, even if it is a possible adverse effect that is not listed in this leaflet. You can also report them directly through the national reporting system included in Appendix V. By reporting adverse effects, you can help provide more information on the safety of this medicine.
5. Storage of IMULDOSA
- Keep this medicine out of the sight and reach of children.
- Store in a refrigerator (2°C – 8°C). Do not freeze.
- Store the pre-filled syringe in the outer packaging to protect it from light.
- If necessary, individual IMULDOSA pre-filled syringes can also be stored at room temperature up to 30°C for a single period of up to 30 days in their original carton to protect them from light. Write the date when the pre-filled syringe is first removed from the refrigerator and the date when it should be discarded on the spaces provided on the outer packaging. The discard date should not exceed the original expiry date printed on the carton. Once a syringe has been stored at room temperature (up to a maximum of 30°C), it should not be refrigerated again. Discard the syringe if it is not used within 30 days of storage at room temperature or from the original expiry date, whichever comes first.
- Do not shake the IMULDOSA pre-filled syringes. Prolonged vigorous shaking can damage the product.
Do not use this medicine:
- after the expiry date which is stated on the label and carton after "EXP". The expiry date is the last day of the month shown.
- if the liquid changes color, is cloudy or contains foreign particles floating in it (see section 6 "Appearance of IMULDOSA and package contents").
- if you know or think that it has been exposed to extreme temperatures (such as accidental heating or freezing).
- if the product has been vigorously shaken.
IMULDOSA is for single use. You should discard any unused product left in the syringe. Medicines should not be disposed of via wastewater or household waste. Ask your pharmacist how to dispose of medicines no longer required. This will help protect the environment.
6. Package Contents and Additional Information
Composition of IMULDOSA
- The active substance is ustekinumab. Each pre-filled syringe contains 45 mg of ustekinumab in 0.5 ml.
- The other ingredients are L-histidine, L-histidine monohydrochloride, polysorbate 80 (E433), sucrose, and water for injections.
Appearance of IMULDOSA and Package Contents
IMULDOSA is a clear to slightly opalescent, colorless to slightly yellowish injectable solution. It is presented in a pack containing 1 pre-filled syringe of 1 ml glass. Each pre-filled syringe contains 45 mg of ustekinumab in 0.5 ml of injectable solution.
Marketing Authorization Holder
Accord Healthcare S.L.U.
World Trade Center, Moll de Barcelona, s/n
Edifici Est, 6a Planta
08039 Barcelona
Spain
Manufacturer
Accord Healthcare Polska Sp. z.o.o.
ul. Lutomierska 50,
95-200, Pabianice, Poland
Accord Healthcare B.V.
Winthontlaan 200,
3526 KV Utrecht, Netherlands
You can request more information about this medicine by contacting the local representative of the marketing authorization holder:
AT / BE / BG / CY / CZ / DE / DK / EE / ES / FI / FR / HR / HU / IE / IS / IT / LT / LV / LU / MT / NL / NO / PL / PT / RO / SE / SI / SK
Accord Healthcare S.L.U.
Tel: +34 93 301 00 64
EL
Win Medica Α.Ε.
Tel: +30 210 74 88 821
Date of the last revision of this leaflet: {MM/AAAA}
Detailed information on this medicine is available on the European Medicines Agency website: http://www.ema.europa.eu/.
Administration Instructions
At the start of treatment, your healthcare professional will help you with your first injection. However, you and your doctor may decide that you can inject IMULDOSA yourself. In this case, they will teach you how to inject IMULDOSA. Talk to your doctor if you have any questions about administering the injections.
- Do not mix IMULDOSA with other injectable liquids.
- Do not shake the IMULDOSA pre-filled syringes. The medicine may deteriorate if shaken vigorously. Do not use the medicine if it has been shaken vigorously.
Figure 1 shows what the pre-filled syringe looks like.
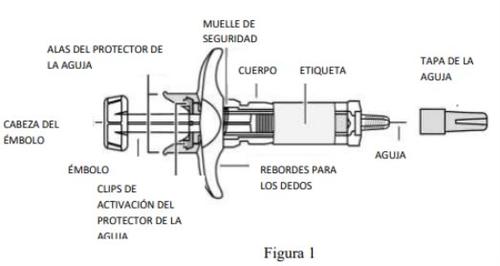
- Check the number of pre-filled syringes and prepare the materials:
Preparation to use the pre-filled syringe
- Remove the pre-filled syringe(s) from the refrigerator. Let the pre-filled syringe sit outside the carton for 30 minutes. This will allow the liquid to reach a comfortable temperature for injection (room temperature). Do not remove the needle cap while waiting for the syringe to reach room temperature.
- Hold the pre-filled syringe by the body with the needle cap pointing upwards.
- Do not hold the pre-filled syringe by the plunger, plunger head, needle protector wings, or needle cap.
- Do not remove the plunger at any time.
- Do not remove the pre-filled syringe cap until instructed to do so.
- Do not touch the activation clips on the needle protector to avoid covering the needle prematurely.
Check the pre-filled syringe(s) to ensure that
- the number of pre-filled syringes and concentration are correct
- If your dose is 45 mg, you will have one 45 mg IMULDOSA pre-filled syringe.
- If your dose is 90 mg, you will have two 45 mg IMULDOSA pre-filled syringes and you will need to administer two injections. Choose two different sites for these injections (e.g., one in the right thigh and one in the left thigh), and inject one after the other.
- it is the correct medicine.
- the expiry date has not passed.
- the pre-filled syringe is not damaged.
- the solution in the pre-filled syringe is clear to slightly opalescent and colorless to slightly yellowish.
- the solution in the pre-filled syringe does not have an abnormal color, is not cloudy, or contains foreign particles.
- the solution in the pre-filled syringe is not frozen.
Prepare all the materials you need and place them on a clean surface, including antiseptic wipes, cotton or gauze, and a container for sharp objects.
- Choose and prepare the injection site:
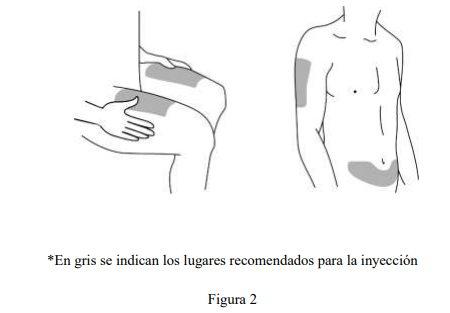
Choose the injection site (see Figure 2).
- IMULDOSA is administered by injection under the skin (subcutaneously).
- Some suitable injection sites are the upper thigh or the abdomen, at least 5 cm from the navel.
- As much as possible, do not use skin areas that show signs of psoriasis.
- If someone else is administering the injection, they can also choose the upper arm as an injection site.
Prepare the injection site
- Wash your hands thoroughly with soap and warm water.
- Clean the skin at the injection site with an antiseptic wipe.
- Do not touch this area again before injecting.
- Remove the needle cap (see Figure 3):
- The needle cap should notbe removed until you are ready to inject.
- Hold the pre-filled syringe and hold the body of the pre-filled syringe with one hand.
- Remove the needle cap and dispose of it. Do not touch the plunger while doing this.
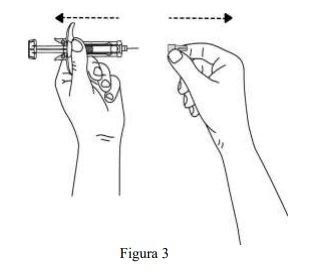
- You may notice an air bubble in the pre-filled syringe or a drop of liquid at the end of the needle. Both are normal and do not need to be removed.
- Do not touch the needle or let it touch any surface.
- Do not use the pre-filled syringe if it has been dropped without the needle cap. If this happens, inform your doctor or pharmacist.
- Inject the dose immediately after removing the needle cap.
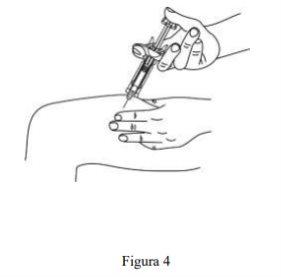
- Inject the dose:
- Hold the pre-filled syringe with one hand between the index and middle fingers, place your thumb on the plunger head, and with your other hand gently pinch a fold of disinfected skin between your thumb and index finger. Do not squeeze.
- Do not remove the plunger at any time.
- With a single quick motion, insert the needle through the skin until it reaches as far as it can go (see Figure 4).
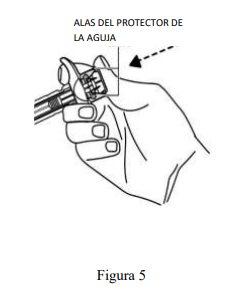
- Inject all the medicine by pushing the plunger until the plunger head is fully between the wings of the needle protector (see Figure 5).
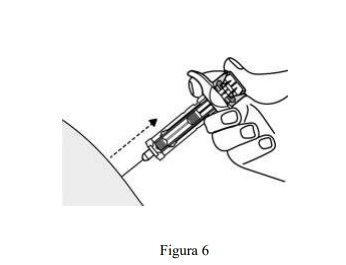
- When you have pushed the plunger as far as it will go, maintain pressure on the plunger head, remove the needle, and release the skin (see Figure 6).
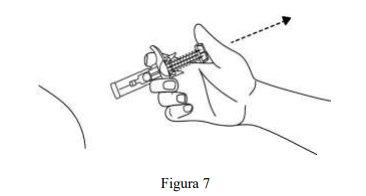
- Slowly remove your thumb from the plunger head to allow the empty syringe to move forward until the needle is completely covered by the needle protector, as shown in Figure 7
- After the injection:
- Press the injection site with an antiseptic wipe for a few seconds after the injection.
- A small amount of blood or liquid may appear at the injection site. This is normal.
- You can press the injection site with a cotton ball or gauze and hold it for 10 seconds.
- Do not rub the skin at the injection site. You can cover the injection site with a band-aid if necessary.
- Disposal:
- Used syringes should be placed in a puncture-resistant container, similar to a sharps container (see Figure 8). For your safety and health and the safety of others, never reuse the syringe. Dispose of your sharps container according to local regulations.
- Antiseptic wipes and other materials can be disposed of in the trash.

- Country of registration
- Active substance
- Prescription requiredYes
- Manufacturer
- This information is for reference only and does not constitute medical advice. Always consult a doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to IMULDOSA 45 mg Injectable Solution in Pre-filled SyringeDosage form: INJECTABLE PERFUSION, 130 mgActive substance: ustekinumabManufacturer: Accord Healthcare S.L.U.Prescription requiredDosage form: INJECTABLE, 45 mgActive substance: ustekinumabManufacturer: Accord Healthcare S.L.U.Prescription requiredDosage form: INJECTABLE, 90 mgActive substance: ustekinumabManufacturer: Accord Healthcare S.L.U.Prescription required
Online doctors for IMULDOSA 45 mg Injectable Solution in Pre-filled Syringe
Discuss questions about IMULDOSA 45 mg Injectable Solution in Pre-filled Syringe, including use, safety considerations and prescription review, subject to medical assessment and local regulations.
Frequently Asked Questions






