HUMIRA 80 mg SOLUTION FOR INJECTION IN PRE-FILLED PEN


How to use HUMIRA 80 mg SOLUTION FOR INJECTION IN PRE-FILLED PEN
Translated with AI
This page provides general information and does not replace a doctor’s consultation. Always consult a doctor before taking any medication. Seek urgent medical care if symptoms are severe.
Show originalContents of the leaflet
Introduction
Patient Information: Summary of Product Characteristics
Humira 80mg solution for injection in pre-filled pen
adalimumab
Read all of this leaflet carefully before you start using this medicine because it contains important information for you.
- Keep this leaflet, you may need to read it again.
- Your doctor will give you a patient information card, which contains important safety information that you need to know before and during treatment with Humira. Keep this patient information card.
- If you have any further questions, ask your doctor or pharmacist.
- This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours.
- If you experience any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet. See section 4.
Contents of the pack
- What is Humira and what is it used for
- What you need to know before you use Humira
- How to use Humira
- Possible side effects
- Storing Humira
- Package contents and further information
- How to inject Humira
1. What is Humira and what is it used for
Humira contains the active substance adalimumab.
Humira is used to treat
- Rheumatoid arthritis
- Plaque psoriasis
- Hidradenitis suppurativa
- Crohn's disease
- Ulcerative colitis
- Non-infectious uveitis
The active substance in Humira, adalimumab, is a human monoclonal antibody. Monoclonal antibodies are proteins that target specific targets.
The target of adalimumab is a protein called tumor necrosis factor (TNFα), which is involved in the immune system (defense) and is found in high levels in the inflammatory diseases described above. By targeting TNFα, Humira reduces the inflammation process in these diseases.
Rheumatoid Arthritis
Rheumatoid arthritis is an inflammatory disease of the joints.
Humira is used to treat moderate to severe rheumatoid arthritis in adults. You may have been given other medicines that modify the disease, such as methotrexate, before. If you do not respond well enough to these medicines, you will be given Humira.
Humira can also be used to treat severe, active, and progressive rheumatoid arthritis without prior treatment with methotrexate.
Humira can reduce the damage to the joints caused by the inflammatory disease and can help you move more freely.
Your doctor will decide if Humira should be used with methotrexate or as monotherapy.
Plaque Psoriasis
Plaque psoriasis is a skin disease that causes red, scaly, crusty, and silvery-scaled areas. Plaque psoriasis can also affect the nails, causing them to deteriorate, thicken, and lift off the nail bed, which can be painful.
Humira is used to treat moderate to severe chronic plaque psoriasis in adults.
Hidradenitis Suppurativa
Hidradenitis suppurativa (also known as inverse acne) is a chronic and often painful inflammatory skin disease. Symptoms can include painful nodules (lumps) and abscesses (boils) that can secrete pus. It usually affects specific areas of the skin, such as under the breast, armpits, inner thighs, groin, and buttocks. There may also be scarring in the affected areas.
Humira is used to treat
- moderate to severe hidradenitis suppurativa in adults and
- moderate to severe hidradenitis suppurativa in adolescents from 12 to 17 years.
Humira can reduce the number of nodules and abscesses caused by the disease and the pain that is usually associated with this disease. You may have received other medicines before. If you do not respond well enough to these medicines, you will be given Humira.
Crohn's Disease
Crohn's disease is an inflammatory disease of the digestive tract.
Humira is used to treat
- moderate to severe Crohn's disease in adults and
- moderate to severe Crohn's disease in children and adolescents from 6 to 17 years.
You may have received other medicines before. If you do not respond well enough to these medicines, you will be given Humira.
Ulcerative Colitis
Ulcerative colitis is an inflammatory disease of the large intestine.
Humira is used to treat
- moderate to severe ulcerative colitis in adults and
- moderate to severe ulcerative colitis in children and adolescents from 6 to 17 years.
You may have received other medicines before. If you do not respond well enough to these medicines, you will be given Humira.
Non-infectious Uveitis
Non-infectious uveitis is an inflammatory disease that affects certain parts of the eye.
Humira is used to treat
- adults with non-infectious uveitis with inflammation that affects the back of the eye.
- children from 2 years of age with chronic non-infectious uveitis with inflammation that affects the front of the eye.
This inflammation can lead to a decrease in vision and/or the presence of floaters in the eye (black dots or thin lines that move across the field of vision). Humira works by reducing this inflammation. You may have received other medicines before. If you do not respond well enough to these medicines, you will be given Humira.
2. What you need to know before you use Humira
Do not use Humira:
- If you are allergic to adalimumab or any of the other ingredients of this medicine (listed in section 6).
- If you have active tuberculosis or other severe infections (see "Warnings and precautions"). If you have symptoms of any infection, such as fever, wounds, fatigue, dental problems, it is important that you inform your doctor.
- If you have moderate to severe heart failure. It is important that you tell your doctor if you have had or have any serious heart problems (see "Warnings and precautions").
Warnings and precautions
Talk to your doctor or pharmacist before you start using Humira.
Allergic reactions
- If you notice an allergic reaction with symptoms such as chest tightness, difficulty breathing, dizziness, swelling, or rash, stop using Humira and contact your doctor immediately, as these reactions can be life-threatening.
Infections
- If you have any infection, including chronic infections, or a localized infection in any part of your body (e.g., a leg ulcer), talk to your doctor before starting treatment with Humira. If you are not sure, contact your doctor.
- With Humira treatment, you may be more likely to get infections. This risk may be higher if you have damaged lungs. These infections can be serious and include:
- tuberculosis
- infections caused by viruses, fungi, parasites, or bacteria
- severe blood infection (sepsis)
In rare cases, these infections can be life-threatening. For this reason, it is important that if you have symptoms such as fever, wounds, fatigue, or dental problems, you tell your doctor. Your doctor may decide to stop your Humira treatment for a while.
- Tell your doctor if you live or travel in areas where fungal infections (e.g., histoplasmosis, coccidioidomycosis, or blastomycosis) are common.
- Tell your doctor if you have had recurrent infections or other diseases that increase the risk of infection.
- If you are over 65 years old, you may be more likely to get infections during Humira treatment. You and your doctor should pay special attention to signs of infection while you are receiving Humira treatment. It is important that you tell your doctor if you have symptoms of infection, such as fever, wounds, fatigue, or dental problems.
Tuberculosis
- Since cases of tuberculosis have been reported in patients treated with Humira, your doctor will examine you for signs or symptoms of tuberculosis before starting your Humira treatment. This will include a thorough medical examination, including your medical history and appropriate diagnostic tests (e.g., chest X-ray and tuberculin test). The results of these tests should be recorded on your patient information card.
- Tuberculosis can develop during treatment, even if you have received treatment to prevent tuberculosis.
- If you develop symptoms of tuberculosis (such as persistent cough, weight loss, lack of energy, low-grade fever) or any other infection during or after treatment, contact your doctor immediately.
Hepatitis B
- Tell your doctor if you are a carrier of the hepatitis B virus (HBV), if you have had active HBV infections, or if you think you may be at risk of getting HBV.
- Your doctor should do a blood test for HBV. In people who are HBV carriers, Humira can cause the virus to become active again.
- In rare cases, especially if you are taking other medicines that suppress the immune system, HBV reactivation can be life-threatening.
Surgery or dental procedures
- If you are going to have surgery or dental procedures, tell your doctor that you are taking Humira. Your doctor may recommend that you temporarily stop Humira treatment.
Demyelinating disease
- If you have or develop a demyelinating disease (a disease that affects the insulation layer around the nerves, such as multiple sclerosis), your doctor will decide whether you should be treated or continue treatment with Humira. Tell your doctor immediately if you experience symptoms such as changes in vision, weakness in arms or legs, or numbness or tingling in any part of your body.
Vaccines
- Certain vaccines may cause infections and should not be given if you are taking Humira.
- Talk to your doctor before getting any vaccine.
- If possible, it is recommended that you get all the vaccines you need before starting Humira treatment.
- If you get Humira while you are pregnant, your baby may have a higher risk of getting infections for about 5 months after the last Humira dose you received during pregnancy. It is important that you tell your doctor and other healthcare professionals about your use of Humira during pregnancy, so they can decide when your baby should get any vaccines. For more information on vaccines, see the "Warnings and precautions" section.
Heart failure
- If you have mild heart failure and are taking Humira, you may be closely monitored by your doctor. It is important that you tell your doctor if you have had or have any serious heart problems. If you develop new symptoms or your symptoms get worse (difficulty breathing, or swelling of your feet), contact your doctor immediately. Your doctor will decide whether you should continue taking Humira.
Fever, bruising, bleeding, or pale appearance
- In some patients, the body may not be able to produce enough of the type of blood cells that help the body fight infections or stop bleeding. Your doctor may decide to stop your Humira treatment. If you develop persistent fever, easy bruising, or bleeding, or if you look pale, call your doctor immediately.
Cancer
- In very rare cases, certain types of cancer have been reported in children and adults treated with Humira or other TNF blockers.
- People with rheumatoid arthritis who have had the disease for a long time may have a higher-than-average risk of developing lymphoma (a cancer that affects the lymphatic system) and leukemia (a cancer that affects the blood and bone marrow).
- If you are taking Humira, your risk of getting lymphoma, leukemia, or other types of cancer may increase. A rare and serious type of lymphoma has been reported in patients taking Humira. Some of these patients were also taking azathioprine or 6-mercaptopurine.
- Tell your doctor if you are taking azathioprine or 6-mercaptopurine with Humira.
- Cases of non-melanoma skin cancer have been reported in patients taking Humira.
- Tell your doctor if you get new skin lesions or if existing lesions change during or after treatment.
- Cancers, other than lymphoma, have been reported in patients with a certain lung disease, called Chronic Obstructive Pulmonary Disease (COPD), treated with another TNF blocker. If you have COPD, or if you smoke heavily, you should talk to your doctor about whether treatment with a TNF blocker is right for you.
Autoimmune disease
- In rare cases, Humira treatment may cause a condition similar to lupus. Contact your doctor if you have symptoms such as unexplained persistent rash, fever, joint pain, or fatigue.
Children and adolescents
- Vaccines: if possible, your child should be up-to-date with all vaccines before using Humira.
Using Humira with other medicines
Tell your doctor or pharmacist if you are taking, have recently taken, or might take any other medicines.
Do not use Humira with medicines that contain the following active substances, due to an increased risk of serious infections:
- anakinra
- abatacept
Humira can be taken with:
- methotrexate
- certain disease-modifying antirheumatic drugs (such as sulfasalazine, hydroxychloroquine, leflunomide, and injectable gold salts)
- corticosteroids or painkillers, including non-steroidal anti-inflammatory drugs (NSAIDs).
If you have any doubts, talk to your doctor.
Pregnancy and breastfeeding
- You should consider using adequate contraceptive methods to avoid becoming pregnant and continue using them for at least 5 months after the last Humira treatment.
- If you are pregnant, think you may be pregnant, or plan to have a baby, ask your doctor for advice before taking this medicine.
- Humira should only be used during pregnancy if necessary.
- According to a pregnancy study, there was no increased risk of congenital malformations when the mother had received Humira treatment during pregnancy compared to mothers with the same disease who did not receive Humira treatment.
- Humira can be used during breastfeeding.
- If you use Humira while you are pregnant, your baby may have a higher risk of getting infections.
- It is important that you tell the pediatrician and other healthcare professionals about your use of Humira during pregnancy before your baby gets any vaccines. For more information on vaccines, see the "Warnings and precautions" section.
Driving and using machines
Humira has a minor influence on the ability to drive, ride a bike, or use machines. You may feel dizzy and have vision problems after using Humira.
3. How to use Humira
Follow your doctor's administration instructions for this medication exactly. If in doubt, consult your doctor again.
The recommended doses of Humira for each of its authorized uses are shown in the following table. Your doctor may prescribe a different presentation of Humira if you need a different dose.
Rheumatoid Arthritis | ||
Age or Body Weight | How much and how often to take | Notes |
Adults | 40 mg every other week | In rheumatoid arthritis, continue treatment with methotrexate during the use of Humira. If your doctor decides that methotrexate is inappropriate, Humira may be administered as monotherapy. If you have rheumatoid arthritis and are not receiving methotrexate with your Humira treatment, your doctor may decide to administer 40 mg of Humira every week or 80 mg every two weeks. |
Plaque Psoriasis | ||
Age or Body Weight | How much and how often to take | Notes |
Adults | The initial dose is 80 mg (one 80 mg injection), followed by 40 mg every other week starting one week after the first dose. | If you obtain an inadequate response, your doctor may increase your dose to 40 mg weekly or 80 mg every two weeks. |
Hiddenitis Suppurativa | ||
Age or Body Weight | How much and how often to take | Notes |
Adults | The initial dose is 160 mg (two 80 mg injections on the same day or one 80 mg injection per day for two consecutive days), followed by an 80 mg dose (one 80 mg injection) two weeks later. After two more weeks, continue with a dose of 40 mg every week or 80 mg every two weeks, as prescribed by your doctor. | It is recommended to use a daily antiseptic liquid on the affected areas. |
Adolescents from 12 to 17 years of age with a weight of 30 kg or more | The initial dose is 80 mg (one 80 mg injection), followed by 40 mg every other week starting one week later. | If you obtain an inadequate response with Humira 40 mg every other week, your doctor may increase your dose to 40 mg every week or 80 mg every two weeks. It is recommended to use a daily antiseptic liquid on the affected areas. |
Crohn's Disease | ||
Age or Body Weight | How much and how often to take | Notes |
Children, adolescents, and adults from 6 to 17 years of age who weigh 40 kg or more | The initial dose is 80 mg (one 80 mg injection), followed by 40 mg two weeks later. If a faster response is needed, the doctor may prescribe an initial dose of 160 mg (two 80 mg injections on the same day or one 80 mg injection per day for two consecutive days), followed by 80 mg (one 80 mg injection) two weeks later. From then on, the usual dose is 40 mg every other week. | Your doctor may increase your dose to 40 mg every week or 80 mg every two weeks. |
Children and adolescents from 6 to 17 years of age who weigh less than 40 kg | The initial dose is 40 mg, followed by 20 mg two weeks later. If a faster response is needed, the doctor may prescribe an initial dose of 80 mg (one 80 mg injection), followed by 40 mg two weeks later. From then on, the usual dose is 20 mg every other week. | Your doctor may increase the frequency of administration to 20 mg every week. |
Ulcerative Colitis | ||
Age or Body Weight | How much and how often to take | Notes |
Adults | The initial dose is 160 mg (two 80 mg injections on the same day or one 80 mg injection per day for two consecutive days), followed by 80 mg (one 80 mg injection) two weeks later. From then on, the usual dose is 40 mg every other week. | Your doctor may increase your dose to 40 mg every week or 80 mg every two weeks. |
Children and adolescents from 6 years of age with a weight less than 40 kg | Initial dose of 80 mg (one 80 mg injection), followed by 40 mg (one 40 mg injection) two weeks later. From then on, the usual dose is 40 mg every other week. | You should continue using Humira at the usual dose, even after turning 18 years old. |
Children and adolescents from 6 years of age with a weight of 40 kg or more | Initial dose of 160 mg (two 80 mg injections on the same day or one 80 mg injection per day for two consecutive days), followed by 80 mg (one 80 mg injection) two weeks later. From then on, the usual dose is 80 mg every other week. | You should continue using Humira at the usual dose, even after turning 18 years old. |
Non-infectious Uveitis | ||
Age or Body Weight | How much and how often to take | Notes |
Adults | The initial dose is 80 mg (one 80 mg injection), followed by 40 mg every other week starting one week after the first dose. | Corticosteroids or other medications that affect the immune system can continue to be used during treatment with Humira. Humira can also be administered as monotherapy. |
Children and adolescents from 2 years of age with a weight less than 30 kg | 20 mg every other week | Your doctor may prescribe an initial dose of 40 mg that can be administered one week before starting the usual schedule of 20 mg every other week. The use of Humira in combination with methotrexate is recommended. |
Children and adolescents from 2 years of age with a weight of 30 kg or more | 40 mg every other week | Your doctor may prescribe an initial dose of 80 mg that can be administered one week before starting the usual schedule of 40 mg every other week. The use of Humira in combination with methotrexate is recommended. |
Form and route of administration
Humira is injected under the skin (subcutaneously).
In section 7 "How to inject Humira" you will find detailed instructions on how to inject Humira.
If you use more Humira than you should
If you accidentally inject Humira more frequently than scheduled by your doctor or pharmacist, you should report it. Always carry the medication box with you, even if it's empty.
If you forget to use Humira
If you forget to administer an injection, you should inject the next dose of Humira as soon as you remember. Then, the next dose will be administered as usual, as if you had not forgotten a dose.
If you stop treatment with Humira
The decision to stop using Humira should be discussed with your doctor. Your symptoms may return if you stop using Humira.
If you have any other questions about the use of this medication, ask your doctor or pharmacist.
4. Possible side effects
Like all medications, this medication can cause side effects, although not everyone gets them. Most side effects are mild to moderate. However, some can be serious and require treatment. Side effects can appear up to 4 months after the last injection of Humira.
Contact your doctor immediately if you notice any of the following effects
- severe rash, hives, or other signs of allergic reaction
- swelling of the face, hands, feet
- difficulty breathing, swallowing
- shortness of breath with physical activity or when lying down or swelling of feet
Contact your doctor as soon as possible if you notice any of the following effects
- signs of infection such as fever, nausea, wounds, dental problems, burning sensation when urinating
- feeling of weakness or fatigue
- cough
- tingling
- numbness
- double vision
- weakness in arms or legs
- a lump or an open wound that does not heal
- signs and symptoms of blood disorders such as persistent fever, bruising, bleeding, paleness
The symptoms described above may be signs of the following side effects, which have been observed with Humira.
Very common(may affect more than 1 in 10 people)
- reactions at the injection site (including pain, swelling, redness, or itching)
- respiratory tract infections (including colds, runny nose, sinusitis, pneumonia)
- headache
- abdominal pain
- nausea and vomiting
- rash
- muscle pain
Common(may affect up to 1 in 10 people)
- serious infections (including sepsis and flu)
- intestinal infections (including gastroenteritis)
- skin infections (including cellulitis and herpes)
- ear infections
- oral infections (including dental infection and cold sore)
- infections of the reproductive system
- urinary tract infections
- fungal infections
- joint infections
- benign tumors
- skin cancer
- allergic reactions (including seasonal allergy)
- dehydration
- mood changes (including depression)
- anxiety
- difficulty sleeping
- sensory disturbances such as tingling, prickling, or numbness
- migraine
- nerve root compression (including lower back pain and leg pain)
- visual disturbances
- eye inflammation
- eyelid inflammation and eye swelling
- vertigo (feeling of dizziness or spinning)
- feeling of rapid heartbeat
- high blood pressure
- flushing
- bruising (accumulation of blood outside blood vessels)
- cough
- asthma
- difficulty breathing
- gastrointestinal bleeding
- indigestion (indigestion, bloating, and heartburn)
- acid reflux
- dry eye syndrome (including dry eyes and mouth)
- itching
- itchy rash
- bruising
- skin inflammation (such as eczema)
- breaking of fingernails and toenails
- increased sweating
- hair loss
- new or worsening psoriasis
- muscle spasms
- blood in urine
- kidney problems
- chest pain
- edema (swelling)
- fever
- decrease in platelet count in blood, which increases the risk of bleeding or bruising
- wound healing problems
Uncommon(may affect up to 1 in 100 people)
- opportunistic infections (including tuberculosis and other infections that occur when disease resistance decreases)
- neurological infections (including viral meningitis)
- eye infections
- bacterial infections
- diverticulitis (inflammation and infection of the large intestine)
- cancer
- cancer affecting the lymphatic system
- melanoma
- immune system disorders that can affect the lungs, skin, and lymph nodes (the most common presentation is sarcoidosis)
- vasculitis (inflammation of blood vessels)
- tremor (feeling shaky)
- neuropathy (disorder of the nervous system)
- stroke
- hearing loss, tinnitus
- feeling of irregular heartbeat like skips
- heart problems that can cause difficulty breathing or swelling of ankles
- heart attack
- aneurysm of a major artery, inflammation, and clotting in a vein, blockage of a blood vessel
- lung diseases that can cause difficulty breathing (including inflammation)
- pulmonary embolism (blockage of a pulmonary artery)
- pleural effusion (abnormal fluid accumulation in the pleural space)
- pancreatitis that causes severe abdominal and back pain
- difficulty swallowing
- facial edema (swelling of the face)
- inflammation of the gallbladder; gallstones
- fatty liver
- night sweats
- scars
- abnormal muscle crisis
- systemic lupus erythematosus (including skin inflammation, heart, lungs, joints, and other organs)
- sleep disturbances
- impotence
- inflammations
Rare(may affect up to 1 in 1000 people)
- leukemia (cancer that affects the blood and bone marrow)
- severe allergic reaction with shock
- multiple sclerosis
- nerve disorders (such as optic neuritis and Guillain-Barré syndrome that can cause muscle weakness, abnormal sensations, tingling in the arms and upper body)
- cardiac arrest
- pulmonary fibrosis (scarring in the lungs)
- intestinal perforation (hole in the intestine)
- hepatitis
- reactivation of hepatitis B virus
- autoimmune hepatitis (inflammation of the liver caused by the body's own immune system)
- cutaneous vasculitis (inflammation of blood vessels in the skin)
- Stevens-Johnson syndrome (early symptoms include discomfort, fever, headache, and rash)
- facial edema (swelling of the face) associated with allergic reactions
- erythema multiforme (inflammatory rash on the skin)
- lupus-like syndrome
- angioedema (localized skin inflammation)
- lichenoid skin reaction (purplish-red rash with itching)
Frequency not known(cannot be estimated from the available data)
- hepatosplenic T-cell lymphoma (a rare and often fatal blood cancer)
- Merkel cell carcinoma (a type of skin cancer)
- Kaposi's sarcoma, a rare cancer related to human herpesvirus 8 infection. Kaposi's sarcoma usually occurs more frequently as purple skin lesions
- liver failure
- worsening of a disease called dermatomyositis (seen as a skin rash accompanied by muscle weakness)
- weight gain (for most patients, weight gain was reduced)
Some side effects observed with Humira may not have symptoms and can only be identified through a blood test. These include:
Very common(may affect more than 1 in 10 people)
- low white blood cell count
- low red blood cell count
- increased lipids in blood
- increased liver enzymes
Common(may affect up to 1 in 10 people)
- high white blood cell count
- low platelet count
- increased uric acid in blood
- abnormal sodium levels in blood
- low calcium levels in blood
- low phosphate levels in blood
- high blood sugar
- high lactate dehydrogenase levels in blood
- presence of autoantibodies in blood
- low potassium levels in blood
Uncommon(may affect up to 1 in 100 people)
- high bilirubin levels (liver function test)
Rare(may affect up to 1 in 1000 people)
- low counts in blood for white blood cells, red blood cells, and platelets
Reporting of side effects
If you experience any type of side effect, consult your doctor or pharmacist, even if it is a possible side effect that does not appear in this leaflet. You can also report them directly through the national reporting system included in Appendix V. By reporting side effects, you can help provide more information on the safety of this medication.
5. Storage of Humira
Keep this medication out of sight and reach of children.
Do not use this medication after the expiration date that appears on the packaging after "EXP".
Store in a refrigerator (between 2°C and 8°C). Do not freeze.
Keep the pre-filled pen in the outer packaging to protect it from light.
Alternative storage:
When necessary (for example, when traveling), you can store a single Humira pre-filled pen at room temperature (up to 25°C) for a maximum period of 14 days - make sure to protect it from light. Once you have removed the pen from the refrigerator to store it at room temperature, you must use it within the next 14 days or discard it, even if you put it back in the refrigerator.
You should note the date you removed the pen from the refrigerator and the date after which you must discard the pen.
Medicines should not be disposed of via wastewater or household waste. Ask your doctor or pharmacist how to dispose of the packaging and any unused medication. This will help protect the environment.
6. Container Contents and Additional Information
Composition of Humira
The active substance is adalimumab.
The other components are: mannitol, polysorbate 80, and water for injectable preparations.
Appearance of the Product and Container Contents
Humira 80 mg solution for injection in a pre-filled pen is supplied as a sterile solution of 80 mg of adalimumab dissolved in 0.8 ml of solution.
The Humira pre-filled pen is a single-use, gray/purple pen that contains a glass syringe with Humira. It has two caps: one is gray and has a "1" printed on it, and the other is purple and has a "2" printed on it. It has a window on each side of the pen through which you can see the Humira solution contained in the syringe.
The Humira pre-filled pen is available in packs containing:
- 1 pre-filled pen for patient use with 2 alcohol swabs (1 spare).
- 3 pre-filled pens for patient use with 4 alcohol swabs (1 spare).
Only some pack sizes may be marketed.
Humira may be available in a vial, pre-filled syringe, and/or pre-filled pen.
Marketing Authorization Holder
AbbVie Deutschland GmbH & Co. KG
Knollstrasse
67061 Ludwigshafen
Germany
Manufacturer
AbbVie Biotechnology GmbH
Knollstrasse
67061 Ludwigshafen
Germany
You can request more information about this medicinal product from the local representative of the marketing authorization holder.
België/Belgique/Belgien AbbVie SA Tél/Tel: +32 10 477811 | Lietuva AbbVie UAB Tel: +370 5 205 3023 |
България AbbVie Bulgaria EOOD Тел.: +359 2 90 30 430 | Luxembourg/Luxemburg AbbVie SA Belgique/Belgien Tél/Tel: +32 10 477811 |
Česká republika AbbVie s.r.o. Tel: +420 233 098 111 | Magyarország AbbVie Kft. Tel.: +36 1 455 8600 |
Danmark AbbVie A/S Tlf: +45 72 30-20-28 | Malta V.J.Salomone Pharma Limited Tel: +356 21220174 |
Deutschland AbbVie Deutschland GmbH & Co. KG Tel: 00800 222843 33 (gebührenfrei) Tel: +49 (0) 611 / 1720-0 | Nederland AbbVie B.V. Tel: +31 (0)88 322 2843 |
Eesti AbbVie OÜ Tel: +372 623 1011 | Norge AbbVie AS Tlf: +47 67 81 80 00 |
Ελλάδα AbbVie ΦΑΡΜΑΚΕΥΤΙΚΗ Α.Ε. Τηλ: +30 214 4165 555 | Österreich AbbVie GmbH Tel: +43 1 20589-0 |
España AbbVie Spain, S.L.U. Tel: +34 91 384 09 10 | Polska AbbVie Polska Sp. z o.o. Tel.: +48 22 372 78 00 |
France AbbVie Tél: +33 (0) 1 45 60 13 00 | Portugal AbbVie, Lda. Tel: +351 (0)21 1908400 |
Hrvatska AbbVie d.o.o. Tel + 385 (0)1 5625 501 | România AbbVie S.R.L. Tel: +40 21 529 30 35 |
Ireland AbbVie Limited Tel: +353 (0)1 4287900 | Slovenija AbbVie Biofarmacevtska družba d.o.o. Tel: +386 (1)32 08 060 |
Ísland Vistor hf. Tel: +354 535 7000 | Slovenská republika AbbVie s.r.o. Tel: +421 2 5050 0777 |
Italia AbbVie S.r.l. Tel: +39 06 928921 | Suomi/Finland AbbVie Oy Puh/Tel: +358 (0)10 2411 200 |
Κύπρος Lifepharma (Z.A.M.) Ltd Τηλ.: +357 22 34 74 40 | Sverige AbbVie AB Tel: +46 (0)8 684 44 600 |
Latvija AbbVie SIA Tel: +371 67605000 |
Date of Last Revision of this Leaflet
Detailed information on this medicinal product is available on the European Medicines Agency website: http://www.ema.europa.eu.
To Request a Copy of this Leaflet in
- How to Inject Humira
- The following instructions explain how to inject Humira yourself using the pre-filled pen. Read all the instructions carefully before starting and follow them step by step.
- Your doctor, nurse, or pharmacist will show you the technique for injecting yourself.
- Do not attempt to inject yourself until you are sure you understand how to prepare and administer the injection.
- After you have been properly trained, you or another person, such as a family member or friend, can give the injection.
- Use each pre-filled pen for only one injection.
Humira Pre-filled Pen
Gray Cap1 White Needle Shield Arrow White Purple Cap2
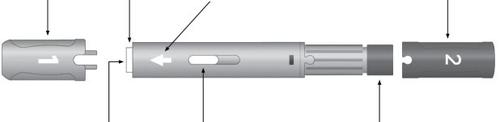
Needle Inspection Window Activation Button
Do not use the pre-filled pen and contact your doctor or pharmacist if
- the liquid is cloudy, discolored, or contains flakes or particles
- the expiration date (EXP) has passed
- the liquid has been frozen or exposed to direct sunlight
- the pre-filled pen has been dropped or crushed
Do not remove all caps until just before injection. Keep out of sight and reach of children.
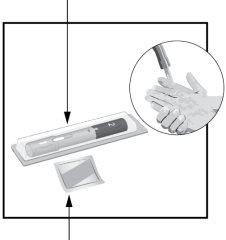
STEP1 Take Humira out of the refrigerator. Let Humira reach room temperature for 15 to 30minutesbefore injection.
| |
STEP2 Pen
Alcohol Swab | Check the expiration date (EXP). Do notuse the pre-filled pen if the expiration date (EXP) has passed. On a flat surface, place
Wash your hands and dry them. |
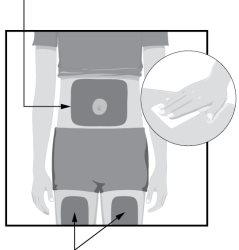
STEP3 Injectable Areas
Injectable Areas | Choose an injection site on your body:
Clean the injection site with the alcohol swab in a circular motion.
|
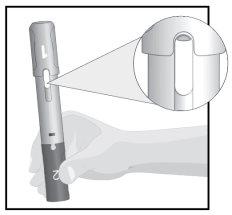
STEP4
| Hold the pre-filled pen with the gray cap 1 facing up. Check the inspection window.
|
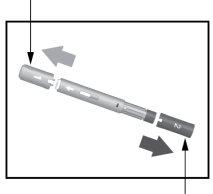
STEP5 Cap 1
Cap2 | Pull the gray cap 1 straight off and throw it away. Do notput it back on.
Pull the purple cap 2 straight off and throw it away. Do notput it back on. The pre-filled pen is now ready for use. Turn the pre-filled pen so that the white arrow points towards the injection site. |
STEP6
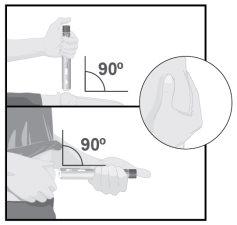
| Pinch the skin at the injection site with your other hand to raise it and hold it firmly until you have finished administering the injection. Point the white arrow towards the injection site (thigh or abdomen). Place the white needle shield straight (at a 90° angle)against the injection site. Hold the pre-filled pen so that you can see the inspection window. Do notpress the purple activation button until you are ready to administer the injection. |
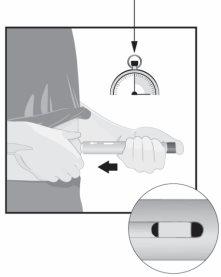
STEP7 15seconds
| Pressthe pre-filled penfirmlyagainst the injection site before starting the injection. Continue to pressto prevent the pre-filled pen from coming out of the skin during the injection. Pressthe purple activation button and count slowly to 15seconds.
The injection is complete when the yellow indicator has stopped moving. |
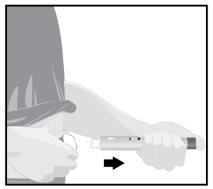
STEP8
| When the injection is complete, slowly pull the pre-filled pen away from the skin. The white needle shield will cover the needle tip.
If there is more than a few drops of liquid at the injection site, contact your doctor, nurse, or pharmacist. After completing the injection, place a cotton ball or gauze on the skin at the injection site.
|
STEP9 Throw the pre-filled pen away in a special sharps container as instructed by your doctor, nurse, or pharmacist.
The caps, alcohol swab, cotton ball or gauze, blister, and packaging can be thrown away in the household trash. |
- Country of registration
- Active substance
- Prescription requiredYes
- Manufacturer
- This information is for reference only and does not constitute medical advice. Always consult a doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to HUMIRA 80 mg SOLUTION FOR INJECTION IN PRE-FILLED PENDosage form: INJECTABLE, 20 mgActive substance: adalimumabManufacturer: Amgen Europe B.V.Prescription requiredDosage form: INJECTABLE, 20 mgActive substance: adalimumabManufacturer: Amgen Europe B.V.Prescription requiredDosage form: INJECTABLE, 40 mgActive substance: adalimumabManufacturer: Amgen Europe B.V.Prescription required
Online doctors for HUMIRA 80 mg SOLUTION FOR INJECTION IN PRE-FILLED PEN
Discuss questions about HUMIRA 80 mg SOLUTION FOR INJECTION IN PRE-FILLED PEN, including use, safety considerations and prescription review, subject to medical assessment and local regulations.
Frequently Asked Questions