HUKYNDRA 40 mg Injectable Solution in Pre-filled Syringe


How to use HUKYNDRA 40 mg Injectable Solution in Pre-filled Syringe
Translated with AI
This page provides general information and does not replace a doctor’s consultation. Always consult a doctor before taking any medication. Seek urgent medical care if symptoms are severe.
Show originalContents of the leaflet
Introduction
Package Leaflet: Information for the Patient
Hukyndra 40mg solution for injection in pre-filled syringe
adalimumab
- This medicinal product is subject to additional monitoring, which will allow for quick identification of new safety information. You can help by reporting any side effects you may get. The last section of this leaflet includes information on how to report side effects.
Read all of this leaflet carefully before you start using this medicine, because it contains important information for you.
- Keep this leaflet, you may need to read it again.
- Your doctor will give you a patient information card, which contains important safety information that you need to know before you start using and during treatment with Hukyndra. Keep this patient information card during your treatment and for 4 months after your last Hukyndra injection.
- If you have any further questions, ask your doctor or pharmacist.
- This medicine has been prescribed for you only. Do not pass it on to others, even if they have the same symptoms as you, as it may harm them.
- If you experience any side effects, talk to your doctor or pharmacist, even if they are not listed in this leaflet. See section 4.
Contents of the package leaflet
- What is Hukyndra and what is it used for
- What you need to know before you start using Hukyndra
- How to use Hukyndra
- Possible side effects
- Storage of Hukyndra
- Contents of the pack and further information
- Instructions for use
1. What is Hukyndra and what is it used for
Hukyndra contains the active substance adalimumab.
Hukyndra is used to treat:
- Rheumatoid arthritis
- Polyarticular juvenile idiopathic arthritis
- Enthesitis-related arthritis
- Ankylosing spondylitis
- Non-radiographic axial spondyloarthritis
- Psoriatic arthritis
- Plaque psoriasis
- Hidradenitis suppurativa
- Crohn's disease
- Ulcerative colitis
- Non-infectious uveitis
The active substance of Hukyndra, adalimumab, is a human monoclonal antibody. Monoclonal antibodies are proteins that target a specific target.
The target of adalimumab is a protein called tumor necrosis factor (TNFα), which is involved in the immune system (defense) and is found at high levels in the inflammatory diseases described above. By targeting TNFα, Hukyndra reduces the inflammatory process in these diseases.
Rheumatoid arthritis
Rheumatoid arthritis is an inflammatory disease of the joints.
Hukyndra is used to treat moderate to severe rheumatoid arthritis in adults. You may have been given other disease-modifying medicines, such as methotrexate, before. If you do not respond well enough to these medicines, you will be given Hukyndra.
Hukyndra may also be used to treat severe, active, and progressive rheumatoid arthritis without prior treatment with methotrexate.
Hukyndra can reduce the damage to the joints caused by the inflammatory disease and can help you move more freely.
Your doctor will decide if Hukyndra should be used with methotrexate or as monotherapy.
Polyarticular juvenile idiopathic arthritis
Polyarticular juvenile idiopathic arthritis is an inflammatory disease of the joints.
Hukyndra is used to treat polyarticular juvenile idiopathic arthritis in patients from 2 years of age. You may have been given other disease-modifying medicines, such as methotrexate, before. If you do not respond well enough to these medicines, you will be given Hukyndra.
Your doctor will decide if Hukyndra should be used with methotrexate or as monotherapy.
Enthesitis-related arthritis
Enthesitis-related arthritis is an inflammatory disease of the joints and the sites where tendons attach to the bone.
Hukyndra is used to treat enthesitis-related arthritis in patients from 6 years of age. You may have been given other disease-modifying medicines, such as methotrexate, before. If you do not respond well enough to these medicines, you will be given Hukyndra.
Ankylosing spondylitis and non-radiographic axial spondyloarthritis
Ankylosing spondylitis and non-radiographic axial spondyloarthritis are inflammatory diseases that affect the spine.
Hukyndra is used to treat severe ankylosing spondylitis and non-radiographic axial spondyloarthritis in adults. You may have been treated with other medicines before. If you do not respond well enough to these medicines, you will be given Hukyndra.
Psoriatic arthritis
Psoriatic arthritis is an inflammatory disease of the joints that is often associated with psoriasis.
Hukyndra is used to treat psoriatic arthritis in adults. Hukyndra can reduce the damage caused by the disease to the joints and can help you move more freely. You may have been treated with other medicines before. If you do not respond well enough to these medicines, you will be given Hukyndra.
Plaque psoriasis
Plaque psoriasis is a skin disease that causes red, scaly, crusty, and silvery-scaled patches. Plaque psoriasis can also affect the nails, causing them to deteriorate, thicken, and lift off the nail bed, which can be painful.
Hukyndra is used to treat
- chronic plaque psoriasis of moderate to severe intensity in adults and
- severe chronic plaque psoriasis in children and adolescents from 4 to 17 years of age who have not responded or are not suitable candidates for topical therapy and phototherapies.
Hidradenitis suppurativa
Hidradenitis suppurativa (also known as inverse acne) is a chronic and often painful inflammatory skin disease. Symptoms can include sensitive nodules (lumps) and abscesses (boils) that can secrete pus. It usually affects specific areas of the skin, such as under the breast, armpits, inner thighs, groin, and buttocks. There may also be scarring in the affected areas.
Hukyndra is used to treat
- moderate to severe hidradenitis suppurativa in adults and
- moderate to severe hidradenitis suppurativa in adolescents from 12 to 17 years.
Hukyndra can reduce the number of nodules and abscesses caused by the disease and the pain that is usually associated with this disease. You may have been treated with other medicines before. If you do not respond well enough to these medicines, you will be given Hukyndra.
Crohn's disease
Crohn's disease is an inflammatory disease of the digestive tract.
Hukyndra is used to treat
- moderate to severe Crohn's disease in adults and
- moderate to severe Crohn's disease in children and adolescents from 6 to 17 years.
You may have been given other medicines before. If you do not respond well enough to these medicines, you will be given Hukyndra.
Ulcerative colitis
Ulcerative colitis is an inflammatory disease of the large intestine.
Hukyndra is used to treat
- moderate to severe ulcerative colitis in adults and
- moderate to severe ulcerative colitis in children and adolescents from 6 to 17 years.
You may have been given other medicines before. If you do not respond well enough to these medicines, you will be given Hukyndra.
Non-infectious uveitis
Non-infectious uveitis is an inflammatory disease that affects certain parts of the eye.
Hukyndra is used to treat
- adults with non-infectious uveitis with inflammation that affects the back of the eye.
- children from 2 years of age with chronic non-infectious uveitis with inflammation that affects the front of the eye.
This inflammation can lead to a decrease in vision and/or the presence of floaters in the eye (black dots or thin lines that move across the field of vision). Hukyndra works by reducing this inflammation.
You may have been given other medicines before. If you do not respond well enough to these medicines, you will be given Hukyndra.
2. What you need to know before starting to use Hukyndra
Do not use Hukyndra:
- If you are allergic to adalimumab or to any of the other components of this medicine (included in section 6).
- If you have active tuberculosis or other severe infections (see "Warnings and precautions"). If you have symptoms of any infection, such as fever, wounds, fatigue, dental problems, it is important that you inform your doctor.
- If you have moderate or severe heart failure. It is important that you tell your doctor if you have had or have any serious heart problems (see "Warnings and precautions").
Warnings and precautions
Consult your doctor or pharmacist before starting to use Hukyndra.
Allergic reactions
- If you have an allergic reaction with symptoms such as chest tightness, difficulty breathing, dizziness, swelling, or rash, stop administering Hukyndra and contact your doctor immediately, as these reactions can be life-threatening in rare cases.
Infections
- If you have any infection, including chronic infection or a localized infection in some part of the body (e.g., an ulcer on the leg), consult your doctor before starting treatment with Hukyndra. If you are not sure, contact your doctor.
- With Hukyndra treatment, you may be more likely to get infections. This risk may be greater if you have damaged lungs. These infections can be serious and include:
- tuberculosis
- infections caused by viruses, fungi, parasites, or bacteria
- severe blood infection (sepsis)
In rare cases, these infections could be life-threatening. It is essential that if you have symptoms such as fever, wounds, fatigue, or dental problems, you tell your doctor. Your doctor may indicate that you should stop using Hukyndra for a while.
- Tell your doctor if you live or travel to regions where fungal infections (such as histoplasmosis, coccidioidomycosis, or blastomycosis) are very common.
- Tell your doctor if you have had recurrent infections or other disorders that increase the risk of infections.
- If you are over 65 years old, you may be more susceptible to infections while being treated with Hukyndra. Both you and your doctor should pay special attention to the appearance of signs of infection while being treated with Hukyndra. It is crucial that you inform your doctor if you have symptoms of infections, such as fever, wounds, feeling of fatigue, or dental problems.
Tuberculosis
- It is very important that you inform your doctor if you have had tuberculosis in the past or if you have been in close contact with someone who has had tuberculosis. If you have active tuberculosis, you should not use Hukyndra.
- Since cases of tuberculosis have been described in patients treated with adalimumab, your doctor will examine you for signs or symptoms of tuberculosis before starting your treatment with Hukyndra. This will include a thorough medical evaluation, including your medical history and appropriate diagnostic tests (e.g., chest X-ray and tuberculin test). The performance and results of these tests should be recorded in your patient information card.
- Tuberculosis can develop during treatment, even if you have received treatment to prevent tuberculosis.
- If symptoms of tuberculosis (such as persistent cough, weight loss, lack of energy, low-grade fever) or any other infection appear during or after treatment, contact your doctor immediately.
Hepatitis B
- Tell your doctor if you are a carrier of the hepatitis B virus (HBV), if you have had active HBV infections, or if you think you may be at risk of contracting HBV.
- Your doctor should perform an analysis for HBV. In people carrying HBV, adalimumab can cause the virus to become active again.
- In rare cases, especially if you are taking other medications that suppress the immune system, HBV reactivation can be life-threatening.
Surgery or dental intervention
- If you are going to undergo surgery or dental intervention, tell your doctor that you are using Hukyndra. Your doctor may recommend that you temporarily stop treatment with Hukyndra.
Demyelinating disease
- If you have or develop a demyelinating disease (a disease that affects the insulation layer around the nerves, such as multiple sclerosis), your doctor will decide whether you should be treated or continue treatment with Hukyndra. Inform your doctor immediately if you experience symptoms such as changes in vision, weakness in arms or legs, or numbness or tingling in any part of the body.
Vaccines
- Certain vaccines can cause infections and should not be administered if you are being treated with Hukyndra.
- Consult your doctor before administering any type of vaccine.
- If possible, it is recommended that children receive the scheduled vaccines for their age before starting treatment with Hukyndra.
- If you received Hukyndra while pregnant, your baby may have a higher risk of contracting an infection during the approximately five months following the last dose of Hukyndra you received during pregnancy. It is essential that you inform your baby's doctor and other healthcare professionals about the use of Hukyndra during pregnancy, so they can decide whether your baby should receive any vaccine.
Heart failure
- If you have mild heart failure and are being treated with Hukyndra, you may be closely monitored by your doctor. It is crucial that you tell your doctor if you have had or have any serious heart problems. If you develop new symptoms or your symptoms worsen (e.g., difficulty breathing or swelling of the feet), you should contact your doctor immediately. Your doctor will decide whether you should continue receiving Hukyndra.
Fever, bruising, bleeding, or pale appearance
- In some patients, the body may be unable to produce a sufficient number of the type of blood cells that help the body fight infections or contribute to stopping bleeding. Your doctor may decide to interrupt treatment. If you develop persistent fever, easy bruising, or bleeding, or are very pale, call your doctor immediately.
Cancer
- In very rare cases, certain types of cancer have been reported in children and adults treated with adalimumab or other TNF-blocking agents.
- People with more severe rheumatoid arthritis and who have had the disease for a long time may have a higher-than-average risk of developing lymphoma (a cancer that affects the lymphatic system) and leukemia (a cancer that affects the blood and bone marrow).
- If you are being treated with Hukyndra, the risk of developing lymphoma, leukemia, or other types of cancer may increase. A rare and severe type of lymphoma has been observed in patients treated with adalimumab. Some of these patients were also receiving treatment with azathioprine or 6-mercaptopurine.
- Tell your doctor if you are taking azathioprine or 6-mercaptopurine with Hukyndra.
- Cases of non-melanoma skin cancer have been observed in patients using adalimumab.
- Tell your doctor if new skin lesions appear or if existing lesions change in appearance during or after treatment.
- Cancers other than lymphoma have been reported in patients with a certain lung disease, called Chronic Obstructive Pulmonary Disease (COPD), treated with another TNF-blocking agent. If you have COPD or are a heavy smoker, you should consult your doctor to determine whether treatment with a TNF blocker is suitable for you.
Autoimmune disease
- In rare cases, treatment with Hukyndra may lead to a syndrome similar to lupus. Contact your doctor if you have symptoms such as unexplained persistent rash, fever, joint pain, or fatigue.
Children and adolescents
- Vaccines: if possible, your child should be up-to-date with all vaccines before using Hukyndra.
Other medicines and Hukyndra
Tell your doctor or pharmacist if you are taking, have recently taken, or might take any other medicine.
Do not take Hukyndra with medicines that contain the following active substances due to an increased risk of severe infections:
- anakinra
- abatacept
Hukyndra can be taken with:
- methotrexate
- certain disease-modifying antirheumatic drugs (such as sulfasalazine, hydroxychloroquine, leflunomide, and injectable gold salts)
- corticosteroids or pain medications, including non-steroidal anti-inflammatory drugs (NSAIDs).
If you have any doubts, consult your doctor.
Pregnancy and breastfeeding
- You should consider using adequate contraceptive methods to avoid becoming pregnant and continue using them for at least 5 months after the last treatment with Hukyndra.
- If you are pregnant, think you may be pregnant, or plan to have a baby, ask your doctor for advice on using this medicine.
- Hukyndra should be used during pregnancy only if necessary.
- According to a pregnancy study, there was no increased risk of congenital defects when the mother had received treatment with adalimumab during pregnancy compared to mothers with the same disease who did not receive treatment with adalimumab.
- Hukyndra can be used during breastfeeding.
- If you use Hukyndra while pregnant, your child may have a higher risk of contracting an infection.
- It is essential that you inform your baby's doctor and other healthcare professionals about the use of Hukyndra during pregnancy before your baby receives any vaccine. For more information on vaccines, see the "Warnings and precautions" section.
Driving and using machines
Hukyndra may have a minor effect on your ability to drive, ride a bicycle, or use machines. You may experience dizziness and vision disturbances after using Hukyndra.
Hukyndra contains sodium
This medicine contains less than 1 mmol of sodium (23 mg) per 0.4 ml; it is essentially "sodium-free".
3. How to use Hukyndra
Follow the administration instructions for this medication exactly as indicated by your doctor or pharmacist. If in doubt, consult your doctor or pharmacist again.
In the following table, the recommended doses of Hukyndra are indicated for each of its approved uses. Your doctor may prescribe a different dose of Hukyndra if you need a different dose.
Rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, or axial spondyloarthritis without radiographic evidence of ankylosing spondylitis | ||
Age or body weight | How much and how often to take | Notes |
Adults | 40 mg every other week | In rheumatoid arthritis, continue treatment with methotrexate during the use of Hukyndra. If your doctor decides that methotrexate is inappropriate, Hukyndra may be administered as monotherapy. If you have rheumatoid arthritis and do not receive methotrexate with your treatment with Hukyndra, your doctor may decide to administer 40 mg of Hukyndra every week or 80 mg every two weeks. |
Polyarticular juvenile idiopathic arthritis | ||
Age or body weight | How much and how often to take | Notes |
Children, adolescents, and adults from 2 years of age with a weight of 30 kg or more | 40 mg every other week | Not applicable |
Arthritis associated with enthesitis | ||
Age or body weight | How much and how often to take | Notes |
Children, adolescents, and adults from 6 years of age with a weight of 30 kg or more | 40 mg every other week | Not applicable |
Plaque psoriasis | ||
Age or body weight | How much and how often to take | Notes |
Adults | The initial dose is 80 mg (two 40 mg injections in one day), followed by 40 mg every other week starting one week after the first dose. | If you obtain an inadequate response, your doctor may increase the dose to 40 mg every week or 80 mg every two weeks. |
Children and adolescents from 4 to 17 years of age with a weight of 30 kg or more | The initial dose is 40 mg, followed by 40 mg one week later. Thereafter, the usual dose is 40 mg every other week. | Not applicable |
Hidradenitis suppurativa | ||
Age or body weight | How much and how often to take | Notes |
Adults | The initial dose is 160 mg (four 40 mg injections in one day or two 40 mg injections per day for two consecutive days), followed by a dose of 80 mg (two 40 mg injections in one day) two weeks later. After two more weeks, continue with a dose of 40 mg every week or 80 mg every two weeks, as prescribed by your doctor. | It is recommended to use a daily antiseptic liquid on the affected areas. |
Adolescents from 12 to 17 years of age, with a weight of 30 kg or more | The initial dose is 80 mg (2 injections of 40 mg in one day), followed by 40 mg every other week starting one week later. | If you obtain an inadequate response with Hukyndra 40 mg every other week, your doctor may increase the dose to 40 mg weekly or 80 mg every two weeks. It is recommended to use a daily antiseptic liquid on the affected areas. |
Crohn's disease | ||
Age or body weight | How much and how often to take | Notes |
Children, adolescents, and adults from 6 years of age with a weight of 40 kg or more | The initial dose is 80 mg (two 40 mg injections in one day), followed by 40 mg two weeks later. If a faster response is needed, the doctor may prescribe an initial dose of 160 mg (four 40 mg injections in one day or two 40 mg injections per day for two consecutive days) followed by 80 mg (two 40 mg injections in one day) two weeks later. Thereafter, the usual dose is 40 mg every other week. | Your doctor may increase the dose to 40 mg every week or 80 mg every two weeks. |
Children and adolescents from 6 to 17 years of age who weigh less than 40 kg | The initial dose is 40 mg, followed by 20 mg two weeks later. If a faster response is needed, the doctor may prescribe an initial dose of 80 mg (two 40 mg injections in one day), followed by 40 mg two weeks later. Thereafter, the usual dose is 20 mg every other week. | Your doctor may increase the frequency of the dose to 20 mg every week. |
Ulcerative colitis | ||
Age or body weight | How much and how often to take | Notes |
Adults | The initial dose is 160 mg (four 40 mg injections in one day or two 40 mg injections per day for two consecutive days), followed by a dose of 80 mg (two 40 mg injections in one day) two weeks later. Thereafter, the usual dose is 40 mg every other week. | Your doctor may increase the dose to 40 mg every week or 80 mg every two weeks. |
Children and adolescents from 6 years of age with a weight less than 40 kg | Initial dose of 80 mg (two injections of 40 mg in one day), followed by 40 mg (one injection of 40 mg) two weeks later. Thereafter, the usual dose is 40 mg every other week. | You should continue using adalimumab at the usual dose, even after turning 18 years old. |
Children and adolescents from 6 years of age with a weight of 40 kg or more | Initial dose of 160 mg (four 40 mg injections in one day or two 40 mg injections per day in two consecutive days), followed by 80 mg (two 40 mg injections in one day) two weeks later. Thereafter, the usual dose is 80 mg every other week. | You should continue using adalimumab at the usual dose, even after turning 18 years old. |
Non-infectious uveitis | ||
Age or body weight | How much and how often to take | Notes |
Adults | The initial dose is 80 mg (two 40 mg injections in one day), followed by 40 mg every other week starting one week after the initial dose. | Treatment with corticosteroids or other medications that affect the immune system may be continued. Hukyndra can also be administered alone. |
Children and adolescents from 2 years of age with a weight of at least 30 kg | 40 mg every other week | Your doctor may prescribe an initial dose of 80 mg that can be administered one week before starting the usual schedule of 40 mg every other week. The use of Hukyndra in combination with methotrexate is recommended. |
Form and route of administration
Hukyndra is injected under the skin (subcutaneously).
In section 7 "Instructions for use" you will find detailed instructions on how to inject Hukyndra.
If you use more Hukyndra than you should
If you accidentally inject Hukyndra more frequently than scheduled by your doctor or pharmacist, inform them. Always carry the medication box with you, even if it is empty.
If you forget to use Hukyndra
If you forget to administer an injection, you should inject the next dose of Hukyndra as soon as you remember. Then, the next dose will be administered as usual, as if you had not forgotten a dose.
If you interrupt treatment with Hukyndra
The decision to stop using Hukyndra should be discussed with your doctor. Your symptoms may return if you stop using Hukyndra.
If you have any other questions about the use of this medication, ask your doctor or pharmacist.
4. Possible side effects
Like all medicines, this medicine can cause side effects, although not everybody gets them. Most side effects are mild to moderate. However, some can be serious and require treatment. Side effects may appear at least up to 4 months after the last injection of Hukyndra.
Contact your doctor immediately if you notice any of the following side effects
- severe rash, hives, or other signs of allergic reaction
- swelling of the face, hands, feet
- difficulty breathing, swallowing
- shortness of breath with physical activity or when lying down or swelling of feet.
Contact your doctor as soon as possible if you notice any of the following side effects
- signs of infection such as fever, nausea, wounds, dental problems, burning sensation when urinating
- feeling of weakness or fatigue
- cough
- tingling
- numbness
- double vision
- weakness in arms or legs
- a lump or an open wound that does not heal
- signs and symptoms of blood disorders such as persistent fever, bruising, bleeding, and paleness
The symptoms described above may be signs of the following side effects, which have been observed with adalimumab.
Very common(may affect more than 1 in 10 people)
- reactions at the injection site (including pain, swelling, redness, or itching)
- lower respiratory tract infections (including colds, runny nose, sinusitis, pneumonia)
- headache
- abdominal pain
- nausea and vomiting
- rash
- muscle pain
Common(may affect up to 1 in 10 people)
- serious infections (including sepsis and flu)
- intestinal infections (including gastroenteritis)
- skin infections (including cellulitis and herpes)
- ear infection
- oral infections (including dental infection and cold sore)
- infections in the reproductive system
- urinary tract infection
- fungal infections
- joint infections
- benign tumors
- skin cancer
- allergic reactions (including seasonal allergies)
- dehydration
- mood changes (including depression)
- anxiety
- difficulty sleeping
- sensory disturbances such as tingling, itching, or numbness
- migraine
- nerve root compression (including lower back pain and leg pain)
- visual disturbances
- eye inflammation
- eyelid inflammation and eye swelling
- dizziness (feeling of dizziness or spinning)
- sensation of rapid heartbeat
- high blood pressure
- flushing
- bruising (accumulation of blood outside the blood vessels)
- cough
- asthma
- difficulty breathing
- gastrointestinal bleeding
- indigestion (indigestion, bloating, and heartburn)
- acid reflux
- dry eye syndrome (including dryness in eyes and mouth)
- itching
- itchy rash
- bruising
- skin inflammation (such as eczema)
- nail breakage on hands and feet
- increased sweating
- hair loss
- new or worsening psoriasis
- muscle spasms
- blood in urine
- kidney problems
- chest pain
- edema (swelling)
- fever
- decreased platelet count in blood, which increases the risk of bleeding or bruising
- wound healing problems
Uncommon(may affect up to 1 in 100 people)
- opportunistic infections (including tuberculosis and other infections that occur when disease resistance decreases)
- neurological infections (including viral meningitis)
- eye infections
- bacterial infections
- diverticulitis (inflammation and infection of the large intestine)
- cancer
- cancer affecting the lymphatic system
- melanoma
- immunological disorders that can affect the lungs, skin, and lymph nodes (the most common presentation is sarcoidosis)
- vasculitis (inflammation of blood vessels)
- tremor (feeling shaky)
- neuropathy (disorder of the nervous system)
- stroke
- hearing loss, tinnitus
- sensation of irregular heartbeat like skips
- heart problems that can cause difficulty breathing or swelling of ankles
- heart attack
- aneurysm of a major artery, inflammation, and clotting in a vein, blockage of a blood vessel
- lung diseases that can cause difficulty breathing (including inflammation)
- pulmonary embolism (blockage of a pulmonary artery)
- pleural effusion (abnormal fluid accumulation in the pleural space)
- pancreatitis that causes severe abdominal and back pain
- difficulty swallowing
- facial edema (swelling of the face)
- gallbladder inflammation; gallstones
- fatty liver
- night sweats
- scarring
- abnormal muscle crisis
- systemic lupus erythematosus (including skin inflammation, heart, lungs, joints, and other organs)
- sleep disturbances
- impotence
- inflammation
Rare(may affect up to 1 in 1000 people)
- leukemia (cancer that affects the blood and bone marrow)
- severe allergic reaction with shock
- multiple sclerosis
- nervous system disorders (such as optic neuritis and Guillain-Barré syndrome that can cause muscle weakness, abnormal sensations, tingling in the arms and upper body)
- cardiac arrest
- pulmonary fibrosis (scarring in the lung)
- intestinal perforation (hole in the intestine)
- hepatitis
- reactivation of hepatitis B virus
- autoimmune hepatitis (inflammation of the liver caused by the body's own immune system)
- cutaneous vasculitis (inflammation of blood vessels in the skin)
- Stevens-Johnson syndrome (early symptoms include discomfort, fever, headache, and rash)
- facial edema (swelling of the face) associated with allergic reactions
- erythema multiforme (inflammatory rash on the skin)
- lupus-like syndrome
- angioedema (localized skin inflammation)
- lichenoid skin reaction (red-purple rash with itching)
Frequency not known(cannot be estimated from the available data)
- hepatosplenic T-cell lymphoma (a rare and often fatal blood cancer)
- Merkel cell carcinoma (a type of skin cancer)
- Kaposi's sarcoma, a rare cancer related to human herpesvirus 8 infection. Kaposi's sarcoma usually occurs more frequently as purple-colored skin lesions.
- liver failure
- worsening of a disease called dermatomyositis (seen as a skin rash accompanied by muscle weakness)
- weight gain (for most patients, weight gain was reduced)
Some side effects observed with adalimumab do not have symptoms and can only be identified through a blood test. These include:
Very common(may affect more than 1 in 10 people)
- low white blood cell count
- low red blood cell count
- increased lipids in blood
- increased liver enzymes
Common(may affect up to 1 in 10 people)
- high white blood cell count
- low platelet count
- increased uric acid in blood
- abnormal sodium levels in blood
- low calcium level in blood
- low phosphate level in blood
- high blood sugar
- high lactate dehydrogenase levels in blood
- presence of autoantibodies in blood
- low potassium level in blood
Uncommon(may affect up to 1 in 100 people)
- elevated bilirubin levels (liver function test)
Rare(may affect up to 1 in 1000 people)
- low counts in blood for white blood cells, red blood cells, and platelets
Reporting of side effects
If you experience any side effects, consult your doctor or pharmacist, even if it is a possible side effect not listed in this leaflet. You can also report them directly through the national reporting system included in Appendix V. By reporting side effects, you can help provide more information on the safety of this medicine.
5. Storage of Hukyndra
Keep this medicine out of the sight and reach of children.
Do not use this medicine after the expiry date which is stated on the label and on the carton after “EXP”. The expiry date refers to the last day of the month.
Store in a refrigerator (between 2 °C and 8 °C). Do not freeze.
Store the pre-filled syringe in the outer packaging to protect it from light.
Alternative storage:
When necessary (e.g. when traveling), you may store a single Hukyndra pre-filled syringe at 20 °C to 25 °C for a maximum period of up to 30 days - make sure to protect it from light. Once you have removed the pre-filled syringe from the refrigerator to store it at 20 °C to 25 °C, you must use it within 30 days or discard it, even if you put it back in the refrigerator.
You should write down the date when you removed the pre-filled syringe from the refrigerator and the date after which you must discard the pre-filled syringe.
Do not use this medicine if the liquid is cloudy, discolored, or contains flakes or particles.
Medicines should not be disposed of via wastewater or household waste. Ask your pharmacist how to dispose of medicines no longer required. This will help protect the environment.
6. Package contents and further information
Hukyndra composition
The active substance is adalimumab.
The other ingredients are: sodium chloride, sucrose, polysorbate 80, water for injections, hydrochloric acid (for pH adjustment), sodium hydroxide (for pH adjustment).
Appearance of Hukyndra and package contents
Hukyndra 40 mg solution for injection in a pre-filled syringe with a needle protector is supplied as a sterile solution of 40 mg adalimumab dissolved in 0.4 ml of solution.
The Hukyndra pre-filled syringe is a glass syringe that contains an adalimumab solution. Each pack contains 1, 2, or 6 pre-filled syringes packaged in a blister pack and 1, 2, or 6 alcohol swabs.
Not all pack sizes may be marketed.
Hukyndra may be available in a pre-filled syringe and/or a pre-filled pen.
Marketing authorisation holder
STADA Arzneimittel AG
Stadastrasse 2-18
61118 Bad Vilbel
Germany
Manufacturers
Ivers-Lee CSM
Marie-Curie-Str.8
79539 Lörrach
Germany
Alvotech Hf
Sæmundargata 15-19
Reykjavik, 101
Iceland
STADA Arzneimittel AG
Stadastrasse 2-18
61118 Bad Vilbel
Germany
You can obtain further information about this medicine from the local representative of the marketing authorisation holder:
België/Belgique/Belgien EG (Eurogenerics) NV Tél/Tel: +32 24797878 | Lietuva UAB „STADA Baltics“ Tel: +370 52603926 |
| Luxembourg/Luxemburg EG (Eurogenerics) NV Tél/Tel: +32 4797878 |
Ceská republika STADA PHARMA CZ s.r.o. Tel: +420 257888111 | Magyarország STADA Hungary Kft Tel.: +36 18009747 |
Danmark STADA Nordic ApS Tlf: +45 44859999 | Malta Pharma.MT Ltd Tel: +356 21337008 |
Deutschland STADAPHARM GmbH Tel: +49 61016030 | Nederland Centrafarm B.V. Tel.: +31 765081000 |
Eesti UAB „STADA Baltics“ Tel: +370 52603926 | Norge STADA Nordic ApS Tlf: +45 44859999 |
Ελλ?δα STADA Arzneimittel AG Τηλ: +30 2106664667 | Österreich STADA Arzneimittel GmbH Tel: +43 136785850 |
España Laboratorio STADA, S.L. Tel: +34 934738889 | Polska STADA Poland Sp. z.o o. Tel: +48 227377920 |
France EG LABO - Laboratoires EuroGenerics Tél: +33 146948686 | Portugal Stada, Lda. Tel: +351 211209870 |
Hrvatska STADA d.o.o. Tel: +385 13764111 | România STADA M&D SRL Tel: +40 213160640 |
Ireland Clonmel Healthcare Ltd. Tel: +353 526177777 | Slovenija Stada d.o.o. Tel: +386 15896710 |
Ísland STADA Arzneimittel AG Sími: +49 61016030 | Slovenská republika STADA PHARMA Slovakia, s.r.o. Tel: +421 252621933 |
Italia EG SpA Tel: +39 028310371 | Suomi/Finland STADA Nordic ApS, Suomen sivuliike Puh/Tel: +358 207416888 |
Κ?προς STADA Arzneimittel AG Τηλ: +30 2106664667 | Sverige STADA Nordic ApS Tel: +45 44859999 |
Latvija UAB „STADA Baltics“ Tel: +370 52603926 | United Kingdom (Northern Ireland) STADA Arzneimittel AG Tel: +49 61016030 |
Date of last revision of this leaflet
Other sources of information
Detailed information on this medicine is available on the European Medicines Agency website: http://www.ema.europa.eu.
You can access detailed and up-to-date information about this medicine, including a video on how to use the pre-filled syringe, by scanning the QR code included below or on the outer packaging with your mobile phone (smartphone). You can also access this information at the following internet address: hukyndrapatients.com
Include QR code
- Instructions for use
INSTRUCTIONS FOR USE
Hukyndra (adalimumab) pre-filled syringe
Solution for injection of 40 mg/0.4 ml, for subcutaneous use
Read these instructions for use carefully before using the Hukyndra pre-filled syringe for the first time
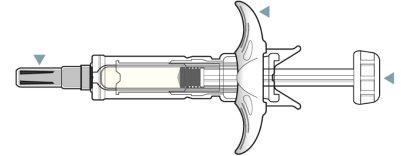
Hukyndra pre-filled syringe


Important information you need to know before injecting Hukyndra pre-filled syringe
Important information:
- For subcutaneous injection only
- Do notuse the syringe and call your healthcare professional or pharmacist if:
- The liquid is cloudy, discolored, or has flakes or particles in it
- The expiry date has passed
- The liquid has been frozen (even if it has been thawed) or exposed to direct sunlight
- The pre-filled syringe has been dropped or crushed
- Keep the needle cap on until just before injection. Keep Hukyndra out of the reach of children.
- See section 5 of the leaflet for information on how to store Hukyndra pre-filled syringe.
Before injecting:
Your healthcare professional should show you how to use the Hukyndra pre-filled syringe before you use it for the first time.
Current use of adalimumab syringe:
Even if you have used other adalimumab syringes on the market before, read the instructions completely so that you understand how to use this device correctly before attempting to inject yourself.
Do you have questions about using the Hukyndra pre-filled syringe?
Talk to your healthcare professional if you have any questions.
Preparing to inject Hukyndra pre-filled syringe
STEP 1: Remove the syringe from the refrigerator and let it reach room temperature between 20 °C and 25 °C for 15-30 minutes
1.1 Remove Hukyndra from the refrigerator (see Figure A).
1.2 Let Hukyndra reach room temperature between 20 °C and 25 °C for 15 to 30 minutes before injecting (see Figure B).
- Do notremove the gray needle cap while letting Hukyndra reach room temperature.
- Do notheat Hukyndra in any other way. For example, do notheat it in a microwave or with hot water.
- Do notuse the pre-filled syringe if the liquid has been frozen (even if it has been thawed).

Figure A


Figure B
STEP 2: Check the expiry date and the medicinal solution
2.1 Check the expiry date on the pre-filled syringe label (see Figure C).
- Do notuse the pre-filled syringe if the expiry date (EXP) has passed.
2.2 Check the medicinal solution in the pre-filled syringe to ensure it is clear and colorless (Figure C).
- Do not use the syringe and call a healthcare professional or pharmacist if the liquid is cloudy, discolored, or has flakes or particles in it.
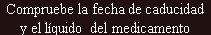

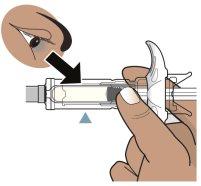
Figure C
STEP 3: Gather the devices and wash your hands
3.1 Place the following on a clean, flat surface (see Figure D):
- 1 pre-filled syringe and 1 alcohol swab.
- 1 cotton ball or gauze (not included).
- Puncture-resistant sharps container (not included). See step 9.
3.2 Wash and dry your hands (see Figure E).



Figure D

Figure E
Injecting Hukyndra pre-filled syringe
STEP 4: Choose and clean the injection site
4.1 Choose an injection site (see Figure F):
- In the front of the thighs or,
- In the stomach (abdomen) at least 5 cm away from the navel.
- Different from your last injection site (at least 3 cm away from the last injection site).
4.2 Clean the injection site with a circular motion using the alcohol swab (see Figure G).
- Do not inject through clothing.
- Do not inject into painful, bruised, red, hard, scarred, or stretch-marked skin, or areas with psoriasis.
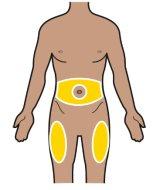
Figure F

Figure G
STEP 5: Remove the needle cap
5.1 Hold the pre-filled syringe with one hand (see Figure H).
5.2 Pull the needle cap straight off with the other hand (see Figure H).
- Discard the needle cap.
- Do not reuse it.
- Do not touch the needle with your fingers or let the needle touch anything.
- Hold the pre-filled syringe with the needle facing up. You may see air in the pre-filled syringe. Slowly push the plunger to push the air through the needle.
- You may see a drop of liquid at the end of the needle. This is normal.

Figure H
STEP 6: Hold the syringe and pinch the skin
6.1 Hold the body of the pre-filled syringe with one hand between the thumb and index finger, as if holding a pencil (see Figure I). Do not pull the plunger back at any time.
6.2 Gently pinch (pinch) the clean skin area of the injection site (abdomen or thigh) with the other hand (see Figure J). Hold the skin firmly.

Figure I

Figure J
STEP 7: Inject the medicine
7.1 Insert the needle into the pinched skin at an angle of approximately 45 degrees, with a quick motion, similar to a dart (see Figure K).
- Once the needle is in, release the skin.
7.2 Slowly push the plunger until all the liquid is injected, and the pre-filled syringe is empty (see Figure L).
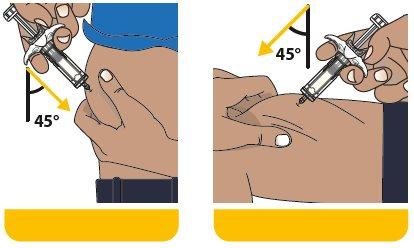
Figure K
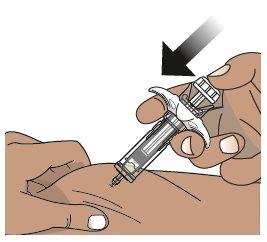
Figure L
STEP 8: Let the pre-filled syringe withdraw the needle from the skin
8.1 Slowly lift your finger off the plunger. The plunger will move up with your finger and withdraw the needle from the site, inside the needle protector (see Figure M).
- The needle will not retract until all the liquid has been injected. Consult your doctor, pharmacist, or nurse if you think you have not given a complete dose.
- It is normal to see a spring around the plunger rod after the needle retracts.
8.2 After completing the injection, place the cotton ball or gauze on the skin over the injection site.
- Do notrub.
- Mild bleeding at the injection site is normal.
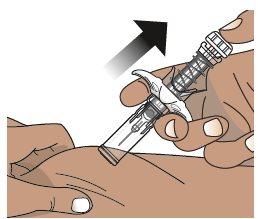
Figure M
Disposal of Hukyndra pre-filled syringe
STEP 9: Dispose of the used syringe in a sharps container
9.1 Place used needles, syringes, and sharps in a sharps container immediately after use (see Figure N).
- Do notthrow away (dispose of) loose needles and syringes in household waste
9.2 The needle cap, alcohol swab, cotton ball or gauze, and packaging can be thrown away in household waste.

Figure N
Additional information on disposal
- If you do not have a sharps container, you can use a household container that is:
- made of a heavy-duty plastic,
- can be closed with a tight-fitting, puncture-resistant lid, without sharps being able to come out,
- upright and stable during use,
- leak-resistant and
- properly labeled to warn of hazardous waste inside the container.
When your sharps container is almost full, you should follow local guidelines for the proper disposal of your sharps container.
Do notdispose of your used sharps container in household waste. Do notrecycle your used sharps container.
If you have any questions, contact your healthcare professional for assistance.
- Country of registration
- Active substance
- Prescription requiredYes
- Manufacturer
- This information is for reference only and does not constitute medical advice. Always consult a doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to HUKYNDRA 40 mg Injectable Solution in Pre-filled SyringeDosage form: INJECTABLE, 20 mgActive substance: adalimumabManufacturer: Amgen Europe B.V.Prescription requiredDosage form: INJECTABLE, 20 mgActive substance: adalimumabManufacturer: Amgen Europe B.V.Prescription requiredDosage form: INJECTABLE, 40 mgActive substance: adalimumabManufacturer: Amgen Europe B.V.Prescription required
Online doctors for HUKYNDRA 40 mg Injectable Solution in Pre-filled Syringe
Discuss questions about HUKYNDRA 40 mg Injectable Solution in Pre-filled Syringe, including use, safety considerations and prescription review, subject to medical assessment and local regulations.
Frequently Asked Questions