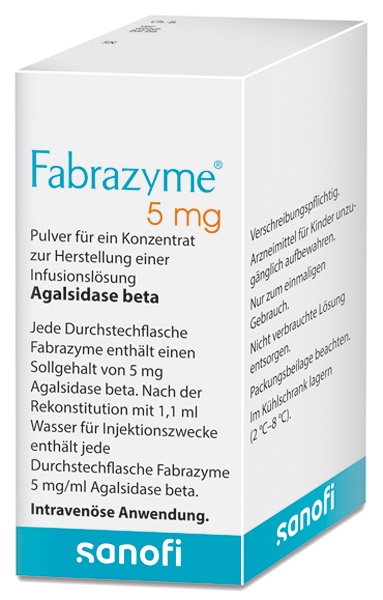
FABRAZYME 5 mg POWDER FOR CONCENTRATE FOR PERFUSION SOLUTION

How to use FABRAZYME 5 mg POWDER FOR CONCENTRATE FOR PERFUSION SOLUTION
Translated with AI
This page provides general information and does not replace a doctor’s consultation. Always consult a doctor before taking any medication. Seek urgent medical care if symptoms are severe.
Show originalContents of the leaflet
Introduction
Package Leaflet: Information for the User
Fabrazyme 5mg powder for concentrate for solution for infusion.
agalsidase beta
Read all of this leaflet carefully before you start using this medicine because it contains important information for you.
- Keep this leaflet, you may need to read it again.
- If you have any further questions, ask your doctor or pharmacist.
- This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours.
- If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet. See section 4.
Contents of the pack and other information:
- What is Fabrazyme and what is it used for
- What you need to know before you use Fabrazyme
- How to use Fabrazyme
- Possible side effects
- Storing Fabrazyme
- Contents of the pack and further information
1. What is Fabrazyme and what is it used for
Fabrazyme contains the active substance agalsidase beta and is used as enzyme replacement therapy in Fabry disease, in which the level of enzyme activity of alpha-Galactosidase is non-existent or below normal. In people with Fabry disease, a fatty substance called globotriaosylceramide (GL-3) is not removed from the body's cells and accumulates in the walls of blood vessels of organs.
Fabrazyme is indicated for long-term enzyme replacement therapy in patients with confirmed diagnosis of Fabry disease.
Fabrazyme is indicated for use in adults, children, and adolescents 8 years of age or older.
2. What you need to know before you use Fabrazyme
Do not use Fabrazyme
- if you are allergic to agalsidase beta or any of the other ingredients of this medicine (listed in section 6).
Warnings and precautions
Talk to your doctor or pharmacist before you start using Fabrazyme.
If you are being treated with Fabrazyme, you may develop infusion-related reactions. An infusion-related reaction is any adverse event that occurs during the infusion or up to the end of the infusion day (see section 4). If you experience such a reaction, you should tell your doctor immediately. You may need other medicines to prevent this type of reaction.
Children and adolescents
No clinical studies have been conducted in children from 0 to 4 years of age. The risks and benefits of Fabrazyme in children between 5 and 7 years of age have not been established yet, and therefore, no dose can be recommended for this age group.
Other medicines and Fabrazyme
Tell your doctor or pharmacist if you are taking, have recently taken, or might take any other medicines.
Tell your doctor if you are using other medicines that contain chloroquine, amiodarone, benoquin, or gentamicin. There is a theoretical risk of reduced activity of agalsidase beta.
Pregnancy, breastfeeding, and fertility
Experience with the use of Fabrazyme in pregnant women is limited. As a precaution, it is preferable to avoid the use of Fabrazyme during pregnancy. Fabrazyme passes into breast milk. Talk to your doctor about the risks and benefits of breastfeeding versus continuing treatment with Fabrazyme. No studies have been conducted to examine the effects of Fabrazyme on fertility.
If you are pregnant or breastfeeding, or think you may be pregnant or are planning to have a baby, ask your doctor or pharmacist for advice before using this medicine.
Driving and using machines
Do not drive or use tools or machines if you experience dizziness, drowsiness, vertigo, or fainting during or soon after the administration of Fabrazyme (see section 4). Talk to your doctor first.
Fabrazyme contains sodium
This medicine contains less than 1mmol of sodium (23 mg) per vial; this is essentially “sodium-free”.
3. How to use Fabrazyme
Fabrazyme is administered by infusion into a vein (intravenous infusion). It is supplied as a powder that will be mixed with sterile water before administration (see information for healthcare professionals at the end of this leaflet).
Follow the instructions for administration of this medicine exactly as told by your doctor. If you are unsure, ask your doctor again.
Fabrazyme is only used under the supervision of a doctor with experience in the treatment of Fabry disease. If you meet certain criteria, your doctor may consider that you can receive treatment at home. Contact your doctor if you wish to receive treatment at home.
The recommended dose of Fabrazyme for adults is 1 mg/kg body weight, every 2 weeks. No dose adjustment is necessary in patients with renal disease.
Use in children and adolescents
The recommended dose of Fabrazyme for children and adolescents from 8 to 16 years is 1 mg/kg body weight, every 2 weeks. No dose adjustment is necessary in patients with renal disease.
If you use more Fabrazyme than you should
Doses of up to 3 mg/kg body weight have been shown to be safe.
If you forget to use Fabrazyme
If you miss an infusion of Fabrazyme, contact your doctor.
If you have any other questions on the use of this medicine, ask your doctor.
4. Possible side effects
Like all medicines, this medicine can cause side effects, although not everybody gets them.
In clinical studies, side effects were mainly seen while patients were receiving the medicine or soon after (“infusion-related reactions”). Potentially life-threatening severe allergic reactions (“anaphylactoid reactions”) have been reported in some patients. If you experience any serious side effect, contact your doctor immediately.
Some very common side effects (may affect more than 1 in 10 people) include chills, fever, feeling of cold, nausea, vomiting, headaches, and abnormal skin sensations such as burning or tingling. Your doctor may decide to reduce the infusion rate or give you additional medicines to prevent such reactions.
List of other side effects:
Frequent (may affect up to 1 in 10 people): | ||
|
|
|
|
| |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| ||
Infrequent (may affect up to 1 in 100 people): | ||
|
|
|
|
|
|
|
|
|
|
|
|
|
| |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Frequency not known (frequency cannot be estimated from the available data) | ||
|
|
In some patients initially treated with the recommended dose and whose dose was later reduced during an additional period, certain symptoms of Fabry disease were observed more frequently.
Reporting of side effects
If you experience any side effects, talk to your doctor or nurse, even if they are not listed in this leaflet. You can also report side effects directly via the national reporting system listed in Appendix V. By reporting side effects, you can help provide more information on the safety of this medicine.
5. Storing Fabrazyme
Keep this medicine out of the sight and reach of children.
Do not use this medicine after the expiry date which is stated on the label after “EXP”. The expiry date is the last day of the month shown.
Unopened vials
Store in a refrigerator (between 2°C and 8°C).
Reconstituted and diluted solutions
The reconstituted solution should not be stored and should be diluted promptly. The diluted solution can be stored for a maximum of 24 hours at a temperature between 2°C and 8°C.
Medicines should not be disposed of via wastewater or household waste. Ask your pharmacist how to dispose of medicines no longer required. This will help protect the environment.
6. Container contents and additional information
Fabrazyme composition
- The active substance is agalsidase beta, one vial contains 5 mg. After reconstitution, each vial contains 5 mg of agalsidase beta per ml.
- The other components are:
- Mannitol (E421)
- Sodium dihydrogen phosphate monohydrate (E339)
- Disodium phosphate heptahydrate (E339)
Appearance of the product and container contents
Fabrazyme is presented as a white to off-white powder. After reconstitution, it is a clear, colorless liquid, free from foreign particles. The reconstituted solution must be diluted subsequently.
Container contents: 1, 5, and 10 vials per box. Only certain pack sizes may be marketed.
Marketing authorization holder and manufacturer
Marketing authorization holder
Sanofi B.V., Paasheuvelweg 25, 1105 BP Amsterdam, Netherlands.
Manufacturer
Genzyme Ireland Limited, IDA Industrial Park, Old Kilmeaden Road, Waterford, Ireland
For further information on this medicinal product, please contact the local representative of the marketing authorization holder:
Belgium/Belgique/Belgien/Luxembourg/Luxemburg Sanofi Belgium Tel: +32 2 710 54 00 | Lithuania Swixx Biopharma UAB Tel: +370 5 236 91 40 |
| Hungary SANOFI-AVENTIS Zrt. Tel: +36 1 505 0050 |
Czech Republic Sanofi s.r.o. Tel: +420 233 086 111 | Malta Sanofi S.r.l. Tel: +39 02 39394275 |
Denmark Sanofi A/S Tlf: +45 45 16 70 00 | Netherlands Genzyme Europe B.V. Tel: +31 20 245 4000 |
Germany Sanofi-Aventis Deutschland GmbH Tel.: 0800 04 36 996 Tel. from abroad: +49 69 305 70 13 | Norway sanofi-aventis Norge AS Tlf: +47 67 10 71 00 |
Estonia Swixx Biopharma OÜ Tel: +372 640 10 30 | Austria sanofi-aventis GmbH Tel: +43 1 80 185 - 0 |
Greece sanofi-aventis AEBE Τηλ: +30 210 900 1600 | Poland Sanofi Sp. z o.o. Tel.: +48 22 280 00 00 |
Spain sanofi-aventis, S.A. Tel: +34 93 485 94 00 | Portugal Sanofi – Produtos Farmacêuticos, Lda. Tel: +351 21 35 89 400 |
France sanofi-aventis France Tél: 0 800 222 555 Appel depuis l’étranger: +33 1 57 63 23 23 | Romania Sanofi Romania SRL Tel: +40 (0) 21 317 31 36 |
Croatia Swixx Biopharma d.o.o. Tel: +385 1 2078 500 | Slovenia Swixx Biopharma d.o.o. Tel: +386 1 235 51 00 |
Ireland sanofi-aventis Ireland Ltd. T/A SANOFI Tel: +353 (0) 1 403 56 00 | Slovak Republic Swixx Biopharma s.r.o. Tel: +421 2 208 33 600 |
Iceland Vistor hf. Sími: +354 535 7000 | Finland Sanofi Oy Puh/Tel: +358 201 200 300 |
Italy Sanofi S.r.l. Tel: 800536389 | Sweden Sanofi AB Tel: +46 (0)8 634 50 00 |
Cyprus C.A. Papaellinas Ltd. Τηλ: +357 22 741741 | United Kingdom (Northern Ireland) sanofi-aventis Ireland Ltd. T/A SANOFI Tel: +44 (0) 800 035 2525 |
Latvia Swixx Biopharma SIA Tel: +371 6 616 47 50 |
Date of last revision of this leaflet:
Other sources of information
Detailed information on this medicinal product is available on the European Medicines Agency website: http://www.ema.europa.eu. There are also links to other websites on rare diseases and orphan medicines.
--------------------------------------------------------------------------------------------------------------------
This information is intended for healthcare professionals only.
Instructions for use – reconstitution, dilution, and administration
The powder for concentrate for solution for infusion must be reconstituted with water for injections, diluted with sodium chloride 0.9% injection solution, and then administered by intravenous infusion.
From a microbiological point of view, the product should be used immediately. If not used immediately, storage and handling are the responsibility of the user. The reconstituted solution cannot be stored and must be diluted promptly; only the diluted solution can be kept for up to 24 hours at 2°C to 8°C.
Use aseptic technique
- The number of vials needed for reconstitution should be calculated based on the patient's weight, and the required vials should be removed from the refrigerator to reach room temperature (approximately 30 minutes). Each vial of Fabrazyme is for single use.
Reconstitution
- Each vial of Fabrazyme 5 mg should be reconstituted with 1.1 ml of water for injections. Avoid vigorous impact of the water for injections on the powder and foam formation. This is achieved by slowly adding the water for injections through the inner wall of the vial and not directly onto the lyophilized cake. Each vial should be tilted and gently rotated. The vial should not be inverted, turned, or shaken.
- The reconstituted solution contains 5 mg of agalsidase beta per ml and appears clear and colorless. The pH of the reconstituted solution is approximately 7.0. Before further dilution, the reconstituted solution of each vial should be visually inspected for particulate matter or color change. The solution should not be used if particles or color changes are observed.
- After reconstitution, it is recommended to dilute the vials promptly to minimize protein particle formation over time.
- Disposal of unused medicinal product and all materials that have come into contact with it should be done in accordance with local regulations.
Dilution
- Before adding the required volume of reconstituted Fabrazyme for the patient's dose, it is recommended to remove an equivalent volume of sodium chloride 0.9% injection solution from the infusion bag.
- Air in the infusion bag should be eliminated to minimize the air/liquid interface.
- Slowly withdraw 1.0 ml (equivalent to 5 mg) of the reconstituted solution from each vial to complete the required volume for the patient's dose. Do not use filter needles, and avoid foam formation.
- Slowly inject the reconstituted solution directly into the sodium chloride 0.9% injection solution (avoiding the air space) to a final concentration between 0.05 mg/ml and 0.7 mg/ml. The total volume of sodium chloride 0.9% injection solution (between 50 and 500 ml) should be determined based on the individual dose. For doses below 35 mg, a minimum of 50 ml should be used; for doses between 35 and 70 mg, a minimum of 100 ml should be used; for doses between 70 and 100 mg, a minimum of 250 ml should be used; and for doses above 100 mg, only 500 ml should be used. The infusion bag should be gently inverted or massaged to mix the diluted solution. The infusion bag should not be shaken or agitated excessively.
Administration
- For administration of the diluted solution, it is recommended to use an in-line filter with a pore size of 0.2 μm and low protein binding to remove any protein particles, which will not result in any loss of agalsidase beta activity. The initial infusion rate (IV) should not exceed 0.25 mg/min (15 mg/hour). The infusion rate can be reduced in case of infusion-associated reactions (IARs).
Once the patient's tolerance has been well established, the infusion rate can be increased in increments of 0.05 to 0.083 mg/min (increments of 3 to 5 mg/hour) with each subsequent infusion. In clinical trials with classical patients, the infusion rate was progressively increased to a minimum of 2 hours. This was achieved after 8 initial infusions at 0.25 mg/min (15 mg/hour) without any IARs, changes in infusion rate, or interruption of infusion. A further reduction in infusion time to 1.5 hours was allowed for patients without new IARs during the last 10 infusions or without serious adverse events reported in the last 5 infusions. Each increase in infusion rate of 0.083 mg/min (~5 mg/hour) was maintained for 3 consecutive infusions without new IARs, changes in infusion rate, or interruption of infusion before subsequent rate increases.
For patients weighing <30 kg, the maximum infusion rate should remain at 0.25 mg min (15 hour).< p>
- Country of registration
- Active substance
- Prescription requiredYes
- Manufacturer
- This information is for reference only and does not constitute medical advice. Always consult a doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to FABRAZYME 5 mg POWDER FOR CONCENTRATE FOR PERFUSION SOLUTIONDosage form: INJECTABLE INFUSION, UnknownActive substance: agalsidase betaManufacturer: Sanofi B.V.Prescription requiredDosage form: INJECTABLE INFUSION, 100 UActive substance: laronidaseManufacturer: Sanofi B.V.Prescription requiredDosage form: INJECTABLE PERFUSION, 30 mg/mlActive substance: cerliponase alfaManufacturer: Biomarin International LimitedPrescription required
Online doctors for FABRAZYME 5 mg POWDER FOR CONCENTRATE FOR PERFUSION SOLUTION
Discuss questions about FABRAZYME 5 mg POWDER FOR CONCENTRATE FOR PERFUSION SOLUTION, including use, safety considerations and prescription review, subject to medical assessment and local regulations.
Frequently Asked Questions