
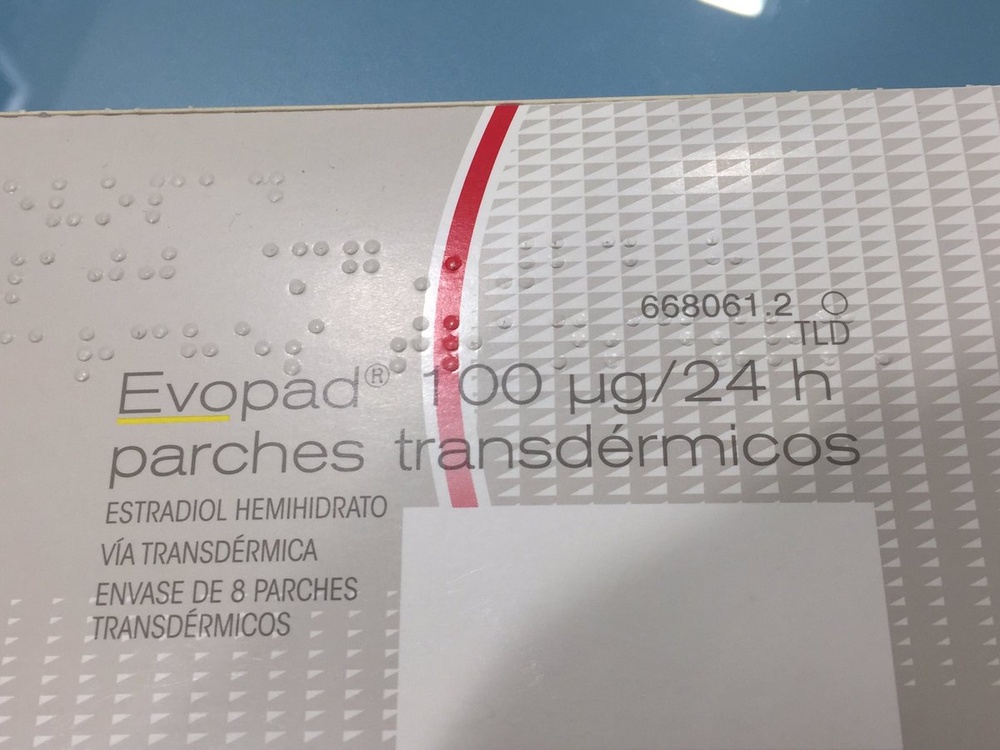
EVOPAD 100 micrograms/24H TRANSDERMAL PATCHES

How to use EVOPAD 100 micrograms/24H TRANSDERMAL PATCHES
Translated with AI
This page provides general information and does not replace a doctor’s consultation. Always consult a doctor before taking any medication. Seek urgent medical care if symptoms are severe.
Show originalContents of the leaflet
- Introduction
- What is Evopad 100(g/24 h transdermal patches and what is it used for
- What you need to know before using Evopad 100(g/24 h transdermal patches
- How to use Evopad 100(g/24 h transdermal patches
- Possible adverse effects
- Conservation of Evopad 100(g/24 h transdermal patches
- Package contents and additional information
Introduction
PACKAGE LEAFLET: INFORMATION FOR THE USER
Evopad 100?g/24 h transdermal patches
Estradiol
Read the entire leaflet carefully before starting to use the medicine because it contains important information for you.
?Keep this leaflet, as you may need to read it again.
? If you have any doubts, consult your doctor or pharmacist.
? This medicine has been prescribed to you and should not be given to others, even if they have the same symptoms, as it may harm them.
? If you experience side effects, consult your doctor or pharmacist, even if they are not listed in this leaflet (see section 4)
Contents of the package leaflet:
- What is Evopad 100?g/24 h transdermal patches and what is it used for
- What you need to know before using Evopad 100?g/24 h transdermal patches
- How to use Evopad 100?g/24 h transdermal patches
- Possible side effects
- Storage of Evopad 100?g/24 h transdermal patches
- Package contents and additional information.
1. What is Evopad 100(g/24 h transdermal patches and what is it used for
EVOPAD 100?g/24 h transdermal patches of the matrix type belong to the pharmacotherapeutic group G03CA03 (estrogens).
EVOPAD 100?g/24 h transdermal patches are indicated as hormone replacement therapy (HRT) for:
- Treatment of menopausal symptoms, natural or surgically induced, e.g. hot flashes, night sweats, urogenital disorders (atrophic vulvovaginitis)
- Prevention of osteoporosis (bone loss) if you are at high risk of suffering future fractures and cannot use other medications for this purpose. Consult your doctor about all available treatment options.
EVOPAD 100?g/24 h transdermal patches should not be used to prevent heart disease or to increase intellectual capacity.
EVOPAD 100?g/24 h transdermal patches are not a contraceptive, nor do they restore fertility.
2. What you need to know before using Evopad 100(g/24 h transdermal patches
Follow your doctor's instructions carefully.
Read the following information before using EVOPAD 25 ?g/24 h transdermal patches.
Do not use EVOPAD 25?g/24 h transdermal patches if:
- If you are allergic (hypersensitive) to estradiol or any of the other components of this medication (listed in section 6)
- you have or have had breast or uterine cancer or if you suspect you may have it
- you are pregnant or suspect you may be pregnant
- you have abnormal genital bleeding that has not been diagnosed
- you have or have had endometrial cancer or endometrial hyperplasia (abnormal growth of the endometrium)
- you have or have had venous thrombosis (blood clots in the legs) or pulmonary embolism (blood clot in the legs that affects the lungs)
- you have any condition that affects blood coagulation (thrombophilia), such as protein C, protein S, or antithrombin deficiency (see section Take special care with EVOPAD 25 ?g/24 h transdermal patches)
- you have or have recently had arterial thrombosis (e.g. angina pectoris, myocardial infarction, stroke, retinal artery occlusion)
- you have or have had severe liver disorders, until they return to normal
- you have porphyria (a blood pigment disease).
Warnings and precautions
Consult your doctor or pharmacist before starting to use EVOPAD 25 ?g/24 h transdermal patches
Visit your doctor regularly, at least once a year. Discuss with your doctor the need to adjust or continue treatment at each visit.
For the treatment of climacteric symptoms, HRT should only be initiated when symptoms affect the woman's quality of life. In all cases, a careful assessment of the risks and benefits should be made at least annually, and HRT should only be continued while the benefits outweigh the risks. The lowest effective dose and the shortest treatment duration should always be considered.
The evidence of the risks associated with HRT as a treatment for premature menopause is limited. However, the use of HRT may be more favorable in young women than in mature women due to the low risk in this patient group.
Medical examination and follow-up:
Before starting hormone replacement therapy (HRT), you should inform your doctor about your personal and family medical history. Your doctor will perform a complete physical and gynecological examination before starting treatment and periodically throughout treatment.
If you experience repeated sudden bleeding, unexpected vaginal bleeding, and changes are detected during the breast examination, a new medical examination will be necessary.
Certain situations will require monitoring by your doctor.
You should consult your doctor if any of the following situations occur or have occurred previously and/or have worsened during pregnancy or during previous hormonal treatment:
- Gynecological disorders of any kind
- History or risk factors for developing blood clots
- Risk factors for breast cancer
- High blood pressure, particularly if it worsens or does not improve with antihypertensive treatment
- Liver disorders
- Diabetes
- Disorders of the gallbladder
- Severe and recurrent migraines
- Systemic lupus erythematosus (an immune system disease)
- Epilepsy
- Asthma
- Hearing problems
- Severe swelling of the skin and other tissues of a hereditary nature
- Changes or alterations in the breasts
- Pregnancy
- Itching
- Hereditary and acquired angioedema
During treatment with EVOPAD 25 ?g/24 h transdermal patches, your doctor will monitor you continuously if you have any of the following conditions:
- Changes in heart or kidney function. Estrogens cause fluid retention.
- Mild liver function disorders
- History of jaundice (yellowing of the whites of the eyes and skin)
- High levels of fat (triglycerides) in the blood or family history of this condition
You should discontinue treatment if you meet any of the conditions indicated in the section Do not use EVOPAD 25?g/24 h transdermal patchesand if you experience any of the following situations:
- Jaundice (yellowing of the whites of the eyes and skin) or deterioration of liver function
- Significant increase in blood pressure
- New episodes of migraine-type headaches
- Pregnancy
- Swelling of the face, tongue, or throat, and difficulty swallowing or urticaria accompanied by difficulty breathing, suggesting angioedema
Be careful not to exceed the recommended doses.
Some patients may develop skin spots, especially those who have had spots during pregnancy. In these cases, it is recommended to minimize sun exposure and/or ultraviolet radiation while using EVOPAD.
EVOPAD does not help improve memory.
During hormone replacement therapy, some serious diseases may occur more frequently, such as blood clots and certain types of tumors.
BLOOD CLOTS (thrombosis)
Hormone replacement therapy increases the risk of blood clots, and this risk is higher during the first year of use.
Blood clots can block major blood vessels. If a blood clot forms in the deep veins of the legs, it can break loose and block the pulmonary arteries (pulmonary embolism). Similarly, blood clots can occur, although much less frequently, in the heart arteries (myocardial infarction, angina pectoris), in the cerebral arteries (cerebral thrombosis), or in the eyes (vision loss or double vision).
If you identify any of the possible signs of a blood clot, inform your doctor immediately. These symptoms include:
- Pain and swelling in one leg
- Sudden onset of coughing
- Severe chest pain and sometimes also arm pain
- Difficulty breathing
- Severe and unusual headache
- Vision problems (vision loss, double vision)
- Difficulty speaking clearly
- Dizziness
- Seizures
- Weakness or numbness affecting one part of the body
- Difficulty walking or holding things
The risk of blood clots may increase temporarily if you need to be immobilized for a period due to surgery or another reason. Therefore, in these cases, you should consult your doctor, as it may be advisable to interrupt treatment until you fully recover your mobility. If you are going to undergo surgery and know in advance that you will be bedridden for a period, inform your doctor.
Breast cancer
Existing data show that the use of hormone replacement therapy (HRT) with combined estrogen-progestin or estrogen-only therapy increases the risk of breast cancer. The additional risk depends on the duration of HRT use. The additional risk becomes apparent after 3 years of use. After stopping HRT, the additional risk will decrease over time, but the risk may persist for 10 years or more if HRT has been used for more than 5 years.
Comparison
In women aged 50-54 who are not using HRT, breast cancer will be diagnosed in an average of 13 to 17 out of 1000 women over a 5-year period.
In women aged 50 who start estrogen-only hormone replacement therapy for 5 years, there will be between 16 and 17 cases per 1000 women users (i.e., 0 to 3 additional cases).
In women aged 50 who start taking combined estrogen-progestin HRT for 5 years, there will be between 21 cases per 1000 women users (i.e., 4-8 additional cases).
In women aged 50-59 who are not taking HRT, an average of 27 cases of breast cancer will be diagnosed per 1000 women over a 10-year period.
In women aged 50 who start estrogen-only hormone replacement therapy for more than 10 years, there will be 34 cases per 1000 women users (i.e., 7 additional cases).
In women aged 50 who start taking combined estrogen-progestin HRT for 10 years, there will be 48 cases per 1000 users (i.e., 21 additional cases).
Ovarian cancer
Ovarian cancer occurs less frequently than breast cancer. The use of HRT with estrogen-only or combined estrogen-progestin therapy has been associated with a slightly increased risk of ovarian cancer.
The risk of ovarian cancer varies with age. For example, in women aged 50-54 who are not taking HRT, approximately 2 cases of ovarian cancer have been observed per 2000 women over a 5-year period. In women treated with HRT for 5 years, approximately 3 cases have been observed per 2000 patients (i.e., approximately 1 additional case).
Similarly, when estrogens are administered for long periods, the risk of developing tumors and abnormalities in the uterus increases. See section 4. Possible Adverse Effects. For products containing estrogens: If you have a uterus, your doctor will prescribe another hormone, progesterone, to reduce the risk of uterine cancer. At the end of the progesterone treatment period, bleeding may occur. Inform your doctor if you experience heavy or irregular bleeding throughout the cycle.
You should discuss with your doctor the possible alternative treatments available for your specific situation and how long treatment should be continued. This should be reviewed periodically throughout treatment.
Inform your doctor that you are taking EVOPAD 25 ?g/24 h transdermal patches, as it may affect the results of certain laboratory tests or analyses.
EVOPAD 25 ?g/24 h transdermal patches are not a contraceptive and should not be used as such; they also do not restore fertility.
Hormone replacement therapy does not improve memory or intellectual capacity and may even worsen it if you are over 65 years old.
Children and adolescents
EVOPAD 25?g/24 h transdermal patches should not be used in children.
Use of other medications
Inform your doctor or pharmacist if you are using or have recently used other medications, including those purchased without a prescription. Your doctor will inform you about this.
It is especially important that you inform your doctor if you are going to take or are taking any of the following medications, as they may interact with EVOPAD 25 ?g/24 h transdermal patches and modify their effect: antiepileptic medications (e.g. phenobarbital, phenytoin, and carbamazepine), a medication for hypertension (bosentan), antibiotics and other anti-infective medications (e.g. rifampicin, rifabutin, erythromycin, ketoconazole, nevirapine, efavirenz, ritonavir, nelfinavir), some anti-ulcer medications (cimetidine), and herbal preparations containing St. John's Wort - Hypericum perforatum). The effect of these preparations lasts until two weeks after stopping them.
Hormone replacement therapy may affect the way other medications work:
a medication for epilepsy (lamotrigine), as it may increase the frequency of seizures.
Medications for hepatitis C virus (HCV) (e.g. the combined regimen for HCV ombitasvir/paritaprevir/ritonavir and dasabuvir with or without ribavirin; glecaprevir/pibrentasvir or sofosbuvir/velpatasvir/voxilaprevir) may cause elevations in blood test results for liver function (increase in the liver enzyme ALT) in women using HRT with ethinylestradiol. Evopad contains estradiol instead of ethinylestradiol. It is unknown whether an increase in liver enzyme ALT can occur when using Evopad with this combined regimen for HCV.
Pregnancy and breastfeeding
If you are pregnant or breastfeeding, think you may be pregnant, or plan to become pregnant, consult your doctor or pharmacist before using this medication.
Do not use EVOPAD 25 ?g/24 h transdermal patches if you are pregnant or want to become pregnant.
Do not use EVOPAD 25 ?g/24 h transdermal patches if you are breastfeeding.
Driving and using machines
No adverse effects of EVOPAD 25 ?g/24 h transdermal patches on the ability to drive or operate machinery have been reported.
3. How to use Evopad 100(g/24 h transdermal patches
Follow exactly the administration instructions of this medication indicated by your doctor. In case of doubt, consult your doctor or pharmacist.
Remember to use your medication.
Do not suspend treatment before your doctor indicates it, as menopause symptoms may reappear.
If you think the action of EVOPAD 100?g/24 h transdermal patches is too strong or weak, inform your doctor or pharmacist.
The EVOPAD 100?g/24 h transdermal patch should be applied twice a week, removing each used patch after 3-4 days.
Your doctor will indicate the duration of your treatment with EVOPAD 100?g/24 h transdermal patches.
- Cyclic treatment of 3 weeks, followed by a 7-day therapeutic rest period during which vaginal bleeding may occur.
- Continuous treatment in cases of women without a uterus or in severe manifestations of estrogen deficiency during the therapeutic rest period.
Combined treatment with progestogen:
- In cyclic treatments of 21 days with estradiol, it is recommended to administer a progestogen jointly in the last 12 or 14 days of the cycle (e.g., starting on day 8 or 10 of the cycle).
- In continuous treatments with estradiol, it is recommended to administer a progestogen jointly for 12 or 14 consecutive days of the 28-day cycle/month.
In both treatment regimens, vaginal bleeding may occur after discontinuation of the progestogen.
Instructions for correct administration
Open the bags and through the "S"-shaped incision, remove the two parts of the protective film. The adhesive part of the transdermal system should be placed immediately on clean, dry, intact, and healthy skin, pressing with the fingers during the application time.
Each application should be made on a slightly different skin area on the trunk, below the waist.
It can remain applied during bathing and showering. If it comes off and does not reattach correctly, a new patch should be applied immediately.
It should not be applied over or near the breasts.
Creams, lotions, or powders should not be applied to the skin area where the patch will be applied.
If you use moreEVOPAD 100?g/24 h transdermal patchesthan you should
If you have used EVOPAD 100?g/24 h transdermal patches more than you should, inform your doctor or pharmacist.
It is unlikely that you will use more EVOPAD than you should with this type of application. Overdose symptoms may include breast tenderness or pain, and spotting. Some women may also experience nausea, vomiting, and discontinuation of bleeding. There is no specific treatment, and therefore, the medication to be administered should be to alleviate the symptoms. These symptoms may disappear if the patch is removed.
In case of overdose or accidental ingestion, consult the toxicology information service. Phone (91) 562 04 20.
If you forgot to use EVOPAD 100?g/24 h transdermal patches
Do not take a double dose to make up for forgotten doses.
If you forgot to change the patch on the day you were supposed to, do not worry, change it as soon as possible. Resume treatment according to the initially planned cycle. The usual change day is maintained. Forgetting a dose may increase the possibility of bleeding and spotting during the cycle. If you have doubts, consult your doctor or pharmacist.
4. Possible adverse effects
Like all medications, this medication can produce adverse effects, although not all people suffer from them.
If you consider that any of the adverse effects you suffer from is serious or if you notice any adverse effect not mentioned in this prospectus, inform your doctor or pharmacist.
Adverse reactions are listed below, classified according to their frequency, according to the following criteria:
Very frequent: May affect more than 1 in 10 people
Frequent: May affect up to 1 in 10 people
Uncommon: May affect up to 1 in 100 people
Rare: May affect up to 1 in 1,000 people
Very rare: May affect up to 1 in 10,000 people
Unknown
In clinical trials of EVOPAD 100?g/24 h transdermal patches, the following side effects have been described:
- Infections and infestations
? Frequent: genital molluscum (genital infection)
? Uncommon: genital candidiasis
- Benign, malignant, and unspecified neoplasms (including cysts and polyps)
? Rare: breast cancer
? Unknown: endometrial cancer
- Disorders of the immune system
- Uncommon: allergic reaction
- Metabolic and nutritional disorders
- Frequent: weight gain or loss
- Psychiatric disorders
? Uncommon: depression
? Rare: anxiety, increased or decreased libido (sexual desire)
- Nervous system disorders
? Frequent: headache, nervousness, mood changes, insomnia
? Uncommon: dizziness, vertigo
? Rare: paresthesia (tingling sensation), epilepsy, migraine (severe headache)
? Unknown: stroke
- Eye disorders
- Uncommon: visual disturbance
- Rare: intolerance to contact lenses
- Cardiac disorders
- Uncommon: palpitations
- Unknown: myocardial infarction
- Vascular disorders
? Uncommon: increased blood pressure
? Rare: thrombosis (blood clots)
? Unknown: deep vein thrombosis (blood clots in the veins)
- Respiratory, thoracic, and mediastinal disorders
? Unknown: pulmonary embolism (blood clots in the lungs)
- Gastrointestinal disorders
? Frequent: nausea, abdominal pain, diarrhea
? Uncommon: flatulence, difficult and laborious digestion
? Rare: abdominal bloating, vomiting, gas (flatulence)
- Hepatobiliary disorders
? Rare: gallstones
- Skin and subcutaneous tissue disorders
? Frequent: itching, rash, dry skin
? Uncommon: skin discoloration, urticaria, skin redness accompanied by pain
? Rare: excessive hair growth in women (hirsutism), acne
? Unknown: severe swelling of the skin and other tissues (mainly the lips or eyes)
- Musculoskeletal and connective tissue disorders
- Frequent: joint pain, back pain
- Uncommon: muscle pain
? Rare: muscle weakness (myasthenia), muscle cramps
- Reproductive system and breast disorders
? Very frequent: menstrual irregularities
? Frequent: irregular or continuous uterine bleeding, abnormally heavy and prolonged menstrual period, irregular vaginal bleeding, uterine cramps, vaginal inflammation, uterine wall growth, vaginal/uterine bleeding including spotting
- Uncommon: breast enlargement, painful menstrual period, breast pain, breast tenderness
? Rare: benign uterine tumor (benign uterine fibroid), breast lumps, lumps near the cervix (endocervical polyp), painful menstruation, premenstrual syndrome, breast enlargement, white discharge
- General disorders and administration site conditions
? Very frequent: itching at the application site, rash at the application site
? Frequent: pain, weakness, edema at the application site, redness at the application site, reaction at the application site, weight changes
? Uncommon: swelling due to fluid accumulation in the tissues, swelling due to accumulation in several parts of the body, swelling due to fluid accumulation in the legs and feet (edema)
? Rare: fatigue
- Investigational procedures
- Frequent: weight gain
- Laboratory anomalies
? Uncommon: increased transaminases (liver function laboratory test)
Risk of tumor development:
Hormone replacement therapy (HRT) increases the risk of breast cancer. There is a greater risk of development in women who use combined estrogen and progestogen. The increased risk of breast cancer is greater as the duration of treatment increases.
The use of estrogen-only treatment is not recommended in women with an intact uterus. If you have a uterus, your doctor will prescribe another hormone, progesterone, for 12 days in each cycle to reduce the risk of uterine cancer.
It has been observed that in long-term treatments with estrogen alone or combined, the possibilities of suffering from an ovarian tumor increase.
Risk of thrombus development:
Hormone replacement therapy increases the risk of suffering from thrombosis (blood clots), and this risk is greater during the first year of use.
Risk of heart artery diseases:
The risk of developing heart artery diseases may increase in women who use combined treatment from the age of 60.
Risk of cerebrovascular accident
The use of HRT is associated with a higher risk of cerebrovascular accident.
In oral treatment with synthetic estrogens alone or combined with progestogens, the following side effects have been reported: estrogen-dependent benign or malignant neoplasms (e.g., endometrial cancer), myocardial infarction, cerebrovascular accident, gallbladder disorders, skin and subcutaneous tissue disorders (chloasma, erythema multiforme, erythema nodosum, vascular purpura, contact dermatitis, generalized pruritus, urticaria, and angioedema), probable dementia.
If you observe any other adverse reaction not described above, consult your doctor or pharmacist.
If these effects occur, interrupt treatment and consult your doctor.
Reporting of adverse effects:
If you experience any type of adverse effect, consult your doctor or pharmacist, even if it is a possible adverse effect that does not appear in this prospectus. You can also report them directly through the Spanish Medicines Pharmacovigilance System for Human Use: https://www.notificaram.es. By reporting adverse effects, you can contribute to providing more information on the safety of this medication.
5. Conservation of Evopad 100(g/24 h transdermal patches
Keep out of sight and reach of children.
Do not store at a temperature above 25 ºC.
Do not use EVOPAD 100?g/24 h transdermal patches after the expiration date shown on the packaging.
6. Package contents and additional information
Composition of EVOPAD 25?g/24 h transdermal patches
- The active ingredient is estradiol. Each transdermal patch contains 1.60 milligrams of estradiol, which corresponds to a release of 25 micrograms of estradiol every 24 hours.
- The other components are: Acrylic-acetate vinyl copolymer adhesive, Guar gum, Polyester film.
Appearance of the product and package contents
It is presented in boxes of eight square, transparent, self-adhesive transdermal patches with a thickness of 0.2 millimeters to be applied to the skin surface.
Marketing authorization holder and manufacturer
Holder:Theramex Ireland Limited
3rd Floor, Kilmore House,
Park Lane, Spencer Dock,
Dublin 1
D01 YE64
Ireland
Manufacturer:Aesica Pharmaceuticals GmbH
Alfred-Nobel-Str. 10
40789 Monheim am Rhein
Germany
Local representative of the marketing authorization holder:
Theramex Healthcare Spain, S.L.
Calle Martínez Villergas 52, Edificio C, planta 2ª
izquierda.
28027 Madrid
Spain
Medicines should not be thrown down the drain or into the trash. Deposit the packaging and unused medicines in the SIGRE collection point at the pharmacy. If in doubt, ask your pharmacist how to dispose of the packaging and unused medicines. In this way, you will help protect the environment.
OTHER PRESENTATIONS:
EVOPAD 50?g/24 h transdermal patches:Box with 8 patches.
EVOPAD 75?g/24 h transdermal patches:Box with 8 patches.
EVOPAD 100?g/24 h transdermal patches:Box with 8 patches.
This prospectus was approved in 06/2025
Detailed and updated information on this medication is available on the website of the Spanish Agency for Medicines and Health Products (AEMPS) http://www.aemps.gob.es/
- Country of registration
- Average pharmacy price7.65 EUR
- Active substance
- Prescription requiredYes
- Manufacturer
- This information is for reference only and does not constitute medical advice. Always consult a doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to EVOPAD 100 micrograms/24H TRANSDERMAL PATCHESDosage form: GEL, 0.5 mgActive substance: estradiolManufacturer: Orion CorporationPrescription requiredDosage form: GEL, 1 mgActive substance: estradiolManufacturer: Orion CorporationPrescription requiredDosage form: TRANSDERMAL PATCH, 3 mgActive substance: estradiolManufacturer: Merus Labs Luxco Ii S.À.R.L.Prescription required
Online doctors for EVOPAD 100 micrograms/24H TRANSDERMAL PATCHES
Discuss questions about EVOPAD 100 micrograms/24H TRANSDERMAL PATCHES, including use, safety considerations and prescription review, subject to medical assessment and local regulations.
Frequently Asked Questions











