
COLUMVI 10 mg CONCENTRATE FOR INFUSION SOLUTION

How to use COLUMVI 10 mg CONCENTRATE FOR INFUSION SOLUTION
Translated with AI
This page provides general information and does not replace a doctor’s consultation. Always consult a doctor before taking any medication. Seek urgent medical care if symptoms are severe.
Show originalContents of the leaflet
Introduction
Package Leaflet: Information for the Patient
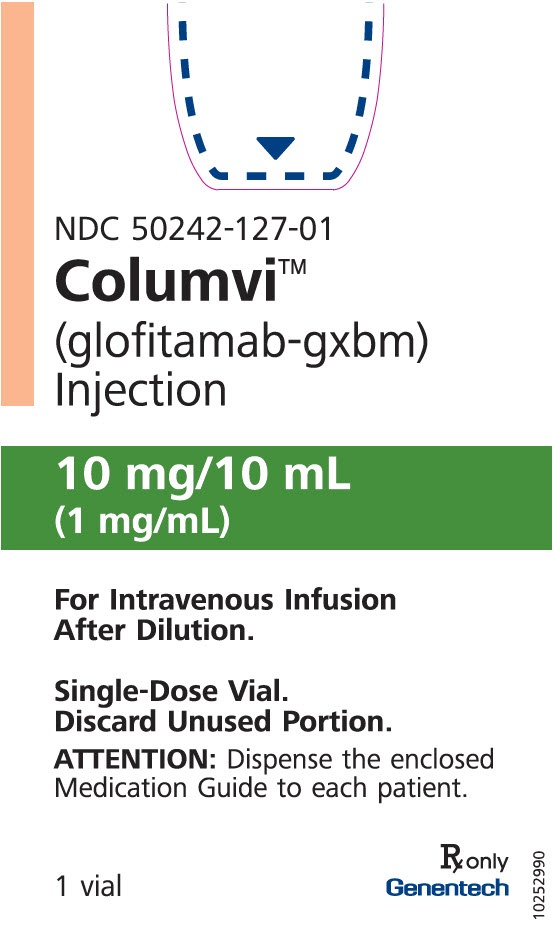
Columvi 2.5 mg concentrate for solution for infusion
Columvi 10 mg concentrate for solution for infusion
glofitamab
This medicinal product is subject to additional monitoring, which will allow for quick identification of new safety information. You can help by reporting any side effects you may get. The last section of the leaflet includes information on how to report side effects.
Read all of this leaflet carefully before you start using this medicine because it contains important information for you.
- Keep this leaflet, you may need to read it again.
- Your doctor will give you a patient information card. Read it carefully and follow the instructions it contains. Always carry this patient information card with you.
- Always show this patient information card to your doctor or nurse or if you go to hospital.
- If you have any further questions, ask your doctor or nurse.
- If you get any side effects, talk to your doctor or nurse, even if you think they might be unrelated to your medicine. See section 4.
Contents of the pack
- What is Columvi and what is it used for
- What you need to know before you are given Columvi
- How Columvi is given
- Possible side effects
- Storage of Columvi
- Contents of the pack and other information
1. What is Columvi and what is it used for
What is Columvi
Columvi is a cancer medicine that contains the active substance glofitamab.
What Columvi is used for
Columvi is used to treat adults with a type of cancer called "diffuse large B-cell lymphoma" (DLBCL). It is used when the cancer:
- has come back (relapsed), or
- has not responded to previous treatments.
Diffuse large B-cell lymphoma is a cancer that affects part of your immune system (the body's defence system).
- It affects a type of white blood cell called "B lymphocytes".
- In DLBCL, the B lymphocytes multiply out of control and build up in tissues.
How Columvi works
- The active substance in Columvi, glofitamab, is a bispecific monoclonal antibody, a type of protein that binds to two specific targets in the body. It binds to a specific protein on the surface of B lymphocytes, including cancerous B lymphocytes, and also to another protein on the surface of T lymphocytes (another type of white blood cell). This activates the T lymphocytes and makes them multiply. This, in turn, causes the destruction of the B lymphocytes, including the cancer cells.
2. What you need to know before you are given Columvi
Columvi must not be given to you
- if you are allergic to glofitamab or any of the other ingredients of this medicine (listed in section 6).
- if you are allergic to obinutuzumab, another medicine that is given before starting treatment with Columvi (see also section 3 "How Columvi is given"), or to any of the other ingredients of this medicine.
If you are not sure, talk to your doctor or nurse before you are given Columvi.
Warnings and precautions
Tell your doctor before you are given Columvi if:
- you have an infection
- you have had a long-lasting (chronic) or recurring infection
- you have or have had any kidney, liver or heart problems
- you are planning to be vaccinated in the near future
If any of the above apply to you (or you are not sure), contact your doctor before you are given Columvi.
Be aware of serious side effects.
Some side effects of Columvi are serious and potentially life-threatening. These can occur at any time during treatment with Columvi.
Tell your doctor immediatelyif you experience any of the following side effects while you are being given Columvi. The symptoms of each side effect are listed in section 4.
- Cytokine release syndrome– an exaggerated inflammatory disorder associated with medicines that stimulate T cells, characterized by fever and deterioration of multiple organs in the body. Cytokine release syndrome is more likely during cycle 1 after Columvi is given (see section 3 "How Columvi is given"). Close monitoring is required.
Before each infusion, you will be given medicines to help reduce the possible side effects of cytokine release syndrome.
?Immune effector cell-associated neurotoxicity syndrome: effects on the nervous system. Symptoms include confusion, disorientation, decreased alertness, seizures or difficulty writing and/or speaking. Close monitoring is required.
?Tumour lysis syndrome– some people may have unusual levels of certain salts in the blood (such as potassium and uric acid) caused by the rapid breakdown of cancer cells during treatment. Your doctor or nurse will do blood tests to check your condition. Before each infusion, you will be well hydrated and given medicines that can help reduce high levels of uric acid. These may help reduce the possible side effects of tumour lysis syndrome.
?Tumour flare– a reaction to certain medicines that act on the immune system and appears similar to a worsening of the cancer
?Infections– you may have signs of infection, which vary depending on where the infection is in the body.
If you have or think you may have any of the above symptoms, tell your doctor immediately.
Your doctor may:
- give you other medicines to reduce the symptoms and prevent complications,
- interrupt your treatment for a short period of time, or
- completely stop your treatment.
Children and adolescents
This medicine must not be given to children or adolescents under 18 years of age. This is because Columvi has not been studied in this age group.
Other medicines and Columvi
Tell your doctor or nurse if you are taking, have recently taken or might take any other medicines. This includes medicines obtained without a prescription and herbal medicines.
Pregnancy and contraception
- If you are pregnant, think you may be pregnant or are planning to have a baby, ask your doctor for advice before taking this medicine.
- Columvi must not be given to you if you are pregnant. This is because Columvi may harm the unborn baby.
- If you can become pregnant, you must use an effective method of contraception while you are being treated with Columvi and for 2 months after the last dose.
- If you become pregnant while you are being treated with Columvi, tell your doctor immediately.
Breast-feeding
You must not breast-feed while you are being given Columvi and for 2 months after the last dose. This is because it is not known whether Columvi passes into breast milk and could affect the baby.
Driving and using machines
Columvi may affect your ability to drive, ride a bicycle or use any tools or machines.
Do not drive, do not use tools or machines for at least 48 hours after each of your first two doses of Columvi or if you develop symptoms of immune effector cell-associated neurotoxicity syndrome (such as confusion, disorientation, decreased alertness, seizures or difficulty writing and/or speaking) and/or symptoms of cytokine release syndrome (such as fever, rapid heartbeat, dizziness or lightheadedness, chills or difficulty breathing). If you currently have these symptoms, avoid these activities and contact your doctor, nurse or pharmacist. See section 4 for more information on side effects.
3. How Columvi is given
Columvi will be given to you under the supervision of a doctor with experience in the treatment of cancer, in a hospital.
Medicines given before treatment with Columvi
- 7 days before starting treatment with Columvi,you will be given another medicine, obinutuzumab, to reduce the number of B lymphocytes in your blood.
- Between 30 and 60 minutes before you are given Columvi,you may be given other medicines (premedication) to help reduce reactions associated with cytokine release syndrome. These medicines may include:
- a corticosteroid such as dexamethasone
- a medicine to reduce fever, such as paracetamol
- an antihistamine such as diphenhydramine
How much and how often you will receive Columvi
You may receive up to 12 cycles of treatment with Columvi. Each cycle lasts 21 days. During the first two cycles, your doctor will start treatment with Columvi with a low dose and gradually increase it to the full dose.
The following is the normal administration schedule.
Cycle 1: will include pre-treatment and 2 low doses of Columvi over the next 21 days:
- Day 1 - pre-treatment with obinutuzumab
- Day 8 - initial dose of 2.5 mg of Columvi
- Day 15 - intermediate dose of 10 mg of Columvi
Cycle 2 to Cycle 12: only one dose over the next 21 days:
- Day 1 - full dose of 30 mg of Columvi
How Columvi is given and monitoring
Columvi is given by infusion into a vein (intravenous infusion). Your doctor will adjust the time needed for the infusion depending on how you respond to treatment.
- Your first infusion will be given over 4 hours. Your doctor will closely monitor you during the first infusion and for the 10 hours after it is finished. This is to monitor for any signs or symptoms of cytokine release syndrome.
- For subsequent infusions, your doctor may monitor you after the infusion is finished. This will be necessary if you had a moderate or severe cytokine release syndrome with your previous dose.
- If you do not have any cytokine release syndrome after 3 doses, your doctor may give you subsequent infusions over 2 hours.
If you miss a dose of Columvi
If you miss an appointment, make another one as soon as possible. To make the treatment completely effective, it is very important not to miss any dose.
Before stopping treatment with Columvi
Talk to your doctor before stopping treatment. Stopping treatment may make your condition worse.
If you have any other questions about the use of this medicine, ask your doctor or nurse.
4. Possible side effects
Like all medicines, this medicine can cause side effects, although not everybody gets them.
Serious side effects
Tell your doctor immediatelyif you experience any of the serious side effects listed below - you may need urgent medical treatment.
?Cytokine release syndrome (very common):symptoms may include, among others, fever, rapid heartbeat, dizziness or lightheadedness, nausea, headache, itching, confusion, chills and difficulty breathing
?Immune effector cell-associated neurotoxicity syndrome (common):symptoms may include, among others, confusion, disorientation, decreased alertness, seizures or difficulty writing and/or speaking
?Infections (very common):symptoms may include, among others, fever, chills, difficulty breathing, burning when urinating
?Tumour flare (very common):symptoms may include, among others, painful swelling of the lymph nodes, chest pain, difficulty breathing easily or pain in the tumour area
?Tumour lysis syndrome (common):symptoms may include, among others, weakness, difficulty breathing, confusion, irregular heartbeat and muscle cramps
Other side effects
Tell your doctor or nurse immediately if you notice any of the following side effects or if they get worse:
Very common (may affect more than 1 in 10 people)
?decrease in blood levels of:
- neutrophils (a type of white blood cell; neutropenia), which can cause fever or any symptom of infection
- red blood cells (anaemia), which can cause tiredness, discomfort and paleness of the skin
- platelets (a type of blood cell; thrombocytopenia), which can cause bruising or bleeding
?fever
?low levels, as measured in blood tests, of phosphate, magnesium, calcium or potassium
?rash
?constipation
?diarrhoea
?feeling sick (nausea)
?viral infections, such as lung infection, herpes zoster
?headache
Common (may affect up to 1 in 10 people)
?low levels, as measured in blood tests, of sodium, which can cause tiredness, muscle spasms or cramps
?increase in levels, as measured in blood tests, of liver enzymes and bilirubin (a yellow substance in the blood), which can cause yellowing of the skin or eyes, and dark urine
?bacterial infections, such as urinary tract infection, stomach infection or infection around the stomach
?fungal infections (mycosis)
?infections of the nose and throat (upper respiratory tract infections)
?lung infections, such as bronchitis or pneumonia (lower respiratory tract infections), which can cause fever, cough and difficulty breathing
?blood infection (septicaemia), which can cause fever, chills and confusion
?low levels, as measured in blood tests, of lymphocytes (a type of white blood cell; lymphopenia)
?fever with low levels of neutrophils (neutropenic fever)
?vomiting
?bleeding in the stomach or intestine (gastrointestinal haemorrhage), which can cause black stools or blood in the vomit
?confusion
?shaking
?sleepiness
Uncommon (may affect up to 1 in 100 people)
?swelling of the spinal cord (myelitis), which can cause muscle weakness or numbness
If you notice any of the above side effects or if they get worse, tell your doctor immediately.
Reporting of side effects
If you get any side effects, talk to your doctor or nurse. This includes any possible side effects not listed in this leaflet. You can also report side effects directly via the national reporting system listed in Appendix V. By reporting side effects, you can help provide more information on the safety of this medicine.
5. Storage of Columvi
Your doctor, pharmacist or nurse is responsible for the storage of this medicine and for the proper disposal of any unused product. The following information is intended for healthcare professionals.
- Keep this medicine out of the sight and reach of children.
- Do not use this medicine after the expiry date which is stated on the carton and on the label of the vial after EXP. The expiry date is the last day of the month shown.
- Store in a refrigerator (2 °C - 8 °C).
- Do not freeze.
- Store the vial in the outer packaging to protect it from light.
- Do not use this medicine if it is turbid, discoloured or contains particles.
Disposal of the unused medicine and all materials that have come into contact with it will be done according to local regulations.
6. Container contents and additional information
Columvi composition
- The active ingredient is glofitamab.
- Columvi 2.5 mg: each vial contains 2.5 milligrams of glofitamab (in 2.5 ml of concentrate) at a concentration of 1 mg/ml
- Columvi 10 mg: each vial contains 10 milligrams of glofitamab (in 10 ml of concentrate) at a concentration of 1 mg/ml
- The other components are: L-histidine, L-histidine monohydrate hydrochloride, L-methionine, sucrose, polysorbate 20 (E432), and water for injectable preparations.
Appearance of the product and container contents
Columvi concentrate for solution for infusion (sterile concentrate) is a clear and colorless solution presented in a glass vial.
Each Columvi container contains one vial.
Marketing authorization holder
Roche Registration GmbH
Emil-Barell-Strasse 1
79639 Grenzach-Wyhlen
Germany
Manufacturer
Roche Pharma AG
Emil-Barell-Strasse 1
79639 Grenzach-Wyhlen
Germany
You can request more information about this medication by contacting the local representative of the marketing authorization holder:
België/Belgique/Belgien N.V. Roche S.A. Tel: +32 (0) 2 525 82 11 | Lietuva UAB "Roche Lietuva" Tel: +370 5 2546799 |
| Luxembourg/ Luxemburg (See Belgium) |
Ceská republika Roche s. r. o. Tel.: +420 - 2 20382111 | Magyarország Roche (Magyarország) Kft. Tel.: +36 - 1 279 4500 |
Danmark Roche Pharma A/S Tlf: +45 - 36 39 99 99 | Malta (see Ireland) |
Deutschland Roche Pharma AG Tel.: +49 (0) 7624 140 | Nederland Roche Nederland B.V. Tel.: +31 (0) 348 438050 |
Eesti Roche Eesti OÜ Tel.: + 372 - 6 177 380 | Norge Roche Norge AS Tel.: +47 - 22 78 90 00 |
Ελλάδα Roche (Hellas) A.E. Τηλ: +30 210 61 66 100 | Österreich Roche Austria GmbH Tel: +43 (0)1 27739 |
España Roche Farma S.A. Tel.: +34 - 91 324 81 00 | Polska Roche Polska Sp.z o.o. Tel.: +48 - 22 345 18 88 |
Francia Roche Tel: +33 (0) 1 47 61 40 00 | Portugal Roche Farmacêutica Química, Ltd Tel.: +351 - 21 425 70 00 |
Hrvatska Roche d.o.o. Tel: +385 1 4722 333 | România Roche România S. R. L. Tel: +40 21 206 47 01 |
Irlanda Roche Products (Ireland)Ltd. Tel: +353 (0)1 469 0700 | Slovenija Roche farmacevtska družba d.o.o. Tel.: +386 - 1 360 26 00 |
Ísland Roche Pharma A/S c/o Icepharma hf Sími: +354 540 8000 | Slovenská republika Roche Slovensko, s.r.o. Tel.: +421 - 2 52638201 |
Italia Roche S.p.A. Tel.: +39 - 039 2471 | Suomi/Finland Roche Oy Puh/Tel: +358 (0) 10 554 500 |
Κύπρος Roche (Hellas) A.E. Τηλ: +30 210 61 66 100 | Sverige Roche AB Tel.: +46 (0) 8 726 1200 |
Latvija Roche Latvija SIA Tel: +371 - 6 7039831 | United Kingdom (Northern Ireland) Roche Products (Ireland)Ltd. Tel: +44 (0) 1707 366000 |
Date of last revision of this prospectus:
This medicinal product has been authorized with a "conditional approval". This type of approval means that more information is expected to be obtained for this medicinal product.
The European Medicines Agency will review the new information for this medicinal product at least once a year, and this prospectus will be updated as necessary.
Other sources of information
Detailed information on this medicinal product is available on the European Medicines Agency website: https://www.ema.europa.eu
--------------------------------------------------------------------------------------------------------------
This information is intended solely for healthcare professionals:
Columvi should be administered by intravenous infusion through a specific infusion line. It should not be administered as an intravenous bolus.
The following are the instructions for dilution of Columvi before administration.
Dilution instructions
?Columvi does not contain preservatives and is intended for single use
?Before intravenous administration, Columvi must be diluted by a healthcare professional using an aseptic technique.
?Do not shake the vial. Visually inspect the Columvi vial for particles or discoloration before administration. Columvi is a clear and colorless solution. Discard the vial if the solution is cloudy, has changed color, or contains visible particles.
?Withdraw the appropriate volume of sodium chloride 9 mg/ml (0.9%) or sodium chloride 4.5 mg/ml (0.45%) injectable solution, as described in Table 1, from the infusion bag using a sterile needle and syringe, and discard the solution.
?Withdraw the required volume of Columvi concentrate for the planned dose from the vial with a sterile needle and syringe, and dilute in the infusion bag (see Table 1 below). Discard any remaining product in the vial.
?The final concentration of glofitamab after dilution should be 0.1 to 0.6 mg/ml.
?Gently invert the infusion bag to mix the solution and avoid excessive foam formation. Do not shake.
?Inspect the infusion bag for particles and discard if present.
?Before starting the intravenous infusion, the contents of the infusion bag should be at room temperature (25°C).
Table 1. Dilution of Columvi for infusion
Dose of Columvi to be administered | Infusion bag size | Volume of sodium chloride 9 mg/ml (0.9%) or 4.5 mg/ml (0.45%) injectable solution to be withdrawn and discarded | Volume of Columvi concentrate to be added |
2.5 mg | 50 ml | 27.5 ml | 2.5 ml |
100 ml | 77.5 ml | 2.5 ml | |
10 mg | 50 ml | 10 ml | 10 ml |
100 ml | 10 ml | 10 ml | |
30 mg | 50 ml | 30 ml | 30 ml |
100 ml | 30 ml | 30 ml |
Only sodium chloride 9 mg/ml (0.9%) or 4.5 mg/ml (0.45%) injectable solution should be used to dilute Columvi, as other solvents have not been tested.
When diluted with sodium chloride 9 mg/ml (0.9%) injectable solution, Columvi is compatible with intravenous infusion bags made of polyvinyl chloride (PVC), polyethylene (PE), polypropylene (PP), or polyolefin without PVC. When diluted with sodium chloride 4.5 mg/ml (0.45%) injectable solution, Columvi is compatible with intravenous infusion bags made of PVC.
No incompatibilities have been observed with infusion equipment with surfaces in contact with the product made of polyurethane (PUR), PVC, or PE, and in-line filter membranes made of polyethersulfone (PES) or polysulfone. The use of an in-line filter is optional.
Intravenous infusion solution
Chemical and physical stability has been demonstrated during use for a maximum of 72 hours at 2-8°C and 24 hours at 30°C, followed by a maximum infusion time of 8 hours.
From a microbiological point of view, the diluted solution should be used immediately. If not used immediately, the storage times and conditions before use are the responsibility of the user and would normally not exceed 24 hours between 2°C and 8°C, unless the dilution has been performed in controlled and validated aseptic conditions.
Disposal
The Columvi vial is for single use.
Disposal of unused medicinal products and all materials that have come into contact with them should be carried out in accordance with local regulations.
- Country of registration
- Active substance
- Prescription requiredYes
- Manufacturer
- This information is for reference only and does not constitute medical advice. Always consult a doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to COLUMVI 10 mg CONCENTRATE FOR INFUSION SOLUTIONDosage form: INJECTABLE PERFUSION, 2.5 mgActive substance: glofitamabManufacturer: Roche Registration GmbhPrescription requiredDosage form: INJECTABLE INFUSION, 50 mgActive substance: brentuximab vedotinManufacturer: Takeda Pharma A/SPrescription requiredDosage form: INJECTABLE PERFUSION, 100 mgActive substance: belantamab mafodotinManufacturer: Glaxosmithkline Trading Services LimitedPrescription required
Online doctors for COLUMVI 10 mg CONCENTRATE FOR INFUSION SOLUTION
Discuss questions about COLUMVI 10 mg CONCENTRATE FOR INFUSION SOLUTION, including use, safety considerations and prescription review, subject to medical assessment and local regulations.
Frequently Asked Questions







