BUPRENORPHINE TEVA 35 micrograms/hour transdermal patch

How to use BUPRENORPHINE TEVA 35 micrograms/hour transdermal patch
Translated with AI
This page provides general information and does not replace a doctor’s consultation. Always consult a doctor before taking any medication. Seek urgent medical care if symptoms are severe.
Show originalContents of the leaflet
Introduction
Package Leaflet: Information for the User
Buprenorphine Teva 35 micrograms/hour transdermal patch EFG
Buprenorphine
Read all of this leaflet carefully before you start using this medicine because it contains important information for you.
- Keep this leaflet, you may need to read it again.
- If you have any further questions, ask your doctor or pharmacist.
- This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours.
- If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet. See section 4.
Contents of the pack
- What is Buprenorphine Teva and what is it used for
- What you need to know before you use Buprenorphine Teva
- How to use Buprenorphine Teva
- Possible side effects
- Storage of Buprenorphine Teva
- Contents of the pack and other information
1. What is Buprenorphine Teva and what is it used for
The active substance of Buprenorphine Teva is buprenorphine.
Buprenorphine Teva is a pain reliever (a medicine for pain relief) indicated for the relief of moderate to severe cancer pain and severe pain that does not respond to other types of pain relievers. Buprenorphine Teva acts through the skin. When the transdermal patch is applied to the skin, the active ingredient buprenorphine passes through the skin into the blood. Buprenorphine is an opioid (a strong pain reliever) that reduces pain by acting on the central nervous system (in specific nerve cells in the spinal cord and brain). The effect of the transdermal patch lasts up to a maximum of four days. Buprenorphine Teva is not suitable for the treatment of acute (short-term) pain.
2. What you need to know before you use Buprenorphine Teva
Do not use Buprenorphine Teva
- if you are allergic to buprenorphine or to any of the other ingredients of this medicine (listed in section 6),
- if you are addicted to strong pain relievers (opioids),
- if you have a disease in which you have great difficulty breathing or in which this may occur,
- if you are taking MAO inhibitors (certain medicines for the treatment of depression) or have taken them in the last two weeks before treatment with Buprenorphine Teva (see “Other medicines and Buprenorphine Teva”),
- in case of myasthenia gravis (a type of severe muscle weakness),
- in case of delirium tremens (confusion and tremors caused by alcohol withdrawal after habitual excessive alcohol consumption or during an episode of high alcohol consumption),
- in case of pregnancy.
Buprenorphine Teva should not be used to treat withdrawal syndrome in drug addicts.
Warnings and precautions
Consult your doctor or pharmacist before you start using Buprenorphine Teva
- if you have recently drunk a lot of alcohol,
- if you have epileptic seizures or convulsions (attacks),
- if you have altered consciousness (feeling of dizziness or fainting), for unknown reasons,
- if you are in a state of shock (a sign could be cold sweat),
- if you have increased intracranial pressure (e.g. after head injury or brain disease), without the possibility of artificial respiration,
- if you have difficulty breathing or are taking other medication that may make you breathe more slowly or weakly (see “Other medicines and Buprenorphine Teva”),
- if you have depression or other diseases that are treated with antidepressants.
The use of these medicines together with Buprenorphine Teva may cause serotonin syndrome, a potentially life-threatening disease (see “Other medicines and Buprenorphine Teva”),
- if you have liver problems,
- if you have a tendency to abuse medicines or drugs.
Also, note the following precautions:
- Some people may become dependent on strong pain relievers such as Buprenorphine Teva when they use them for a long time. These patients may have effects after they stop using them (see “If you stop treatment with Buprenorphine Teva”).
- Fever and ambient heat can lead to higher than normal amounts of buprenorphine in the blood. Also, ambient heat can prevent the transdermal patch from sticking properly. Therefore, consult your doctor if you have a fever and do not expose yourself to heat sources (e.g. sauna, infrared lamps, electric blankets or hot water bottles).
- Sleep-related breathing disorders: Buprenorphine Teva may cause sleep-related breathing disorders such as sleep apnea (pauses in breathing during sleep) and sleep-related hypoxemia (low oxygen levels in the blood). Symptoms may include pauses in breathing during sleep, nighttime awakenings due to difficulty breathing, difficulty maintaining sleep or excessive daytime sleepiness. Contact your doctor if you or someone else observes these symptoms. Your doctor may consider a dose reduction.
- Athletes should be warned that this medicine may give a positive result in doping tests.
Tolerance, dependence, and addiction
This medicine contains buprenorphine, an opioid substance. Repeated use of opioids can reduce the effectiveness of the medicine (your body gets used to the medicine, this is what is known as tolerance). Repeated use of Buprenorphine Teva can also cause dependence, abuse, and addiction, which can lead to a potentially life-threatening overdose. The risk of side effects may increase with a higher dose and longer duration of use. Dependence or addiction can make you feel like you no longer have control over the amount of medicine you need to take or how often you need to take it.
The risk of becoming dependent or addicted varies from person to person. You may have a higher risk of becoming dependent or addicted to Buprenorphine Teva if:
- You or a family member have a history of abuse or dependence on alcohol, prescription medicines, or illicit substances (“addiction”).
- You are a smoker.
- You have ever had problems with your mood (depression, anxiety, or personality disorder) or have received psychiatric treatment for other mental illnesses.
If you notice any of the following signs while taking Buprenorphine Teva, it could be a sign that you have become dependent or addicted:
- You need to take the medicine for longer than recommended by your doctor.
- You need to take more doses than recommended.
- You may feel like you need to keep using your medicine, even when it no longer helps to relieve pain.
- You are using the medicine for reasons other than those prescribed, for example, “to calm down” or “to help you sleep”.
- You have made repeated attempts to stop or control the use of the medicine without success.
- You do not feel well when you stop taking the medicine and feel better when you take it again (“withdrawal symptoms”).
If you notice any of these signs, talk to your doctor to address the most appropriate treatment strategy in your case, including when it is appropriate to stop taking it and how to do so safely (see section 3 “If you stop treatment with Buprenorphine Teva”).
Children and adolescents
Buprenorphine Teva should not be used in persons under 18 years of age, as there is no experience with this age group to date.
Other medicines and Buprenorphine Teva
Tell your doctor or pharmacist if you are using, have recently used, or might use any other medicines.
- Buprenorphine Teva should not be used with MAO inhibitors (certain medicines for the treatment of depression), or if you have taken them in the last two weeks.
- Buprenorphine Teva may cause drowsiness, vomiting, dizziness, or blurred vision, or may make you breathe more slowly or weakly. These side effects may be intensified if you take other medicines that may have the same effects. These other medicines include other strong pain relievers (opioids), certain medicines for sleeping, anesthetics, and medicines for the treatment of certain psychological diseases such as tranquilizers, antidepressants, and neuroleptics.
The concomitant use of Buprenorphine Teva and sedative medicines such as benzodiazepines or related medicines increases the risk of drowsiness, breathing difficulties (respiratory depression), coma, and can be potentially life-threatening. Due to this, concomitant use should only be considered when other treatment options are not possible.
However, if your doctor prescribes Buprenorphine Teva together with sedative medicines, your doctor must limit the dose and duration of concomitant treatment.
Tell your doctor about all sedative medicines you are taking and closely follow the recommended dose. It may be useful to inform friends or family members so they are aware of the signs and symptoms indicated above. Contact your doctor when you experience such symptoms.
The concomitant use of Buprenorphine Teva and gabapentinoids such as gabapentin or pregabalin used to treat epilepsy or pain due to nerve problems (neuropathic pain) may cause breathing difficulties (respiratory depression), low blood pressure, deep drowsiness, coma, and can be potentially life-threatening.
- If Buprenorphine Teva is used with anticholinergic medicines or medicines with anticholinergic activity, such as medicines for treating depression, medicines used to treat allergies, dizziness, or nausea (antihistamines or antiemetics), medicines for treating psychiatric disorders (antipsychotics or neuroleptics), muscle relaxants, or medicines for treating Parkinson's disease, the anticholinergic side effects may increase.
- If Buprenorphine Teva is used with some medicines, the action of the transdermal patch may be intensified. These medicines include, for example, certain anti-infectives and antifungals (e.g. those containing erythromycin or ketoconazole) or medicines for HIV (e.g. those containing ritonavir).
- If Buprenorphine Teva is used with other medicines, the action of the transdermal patch may be reduced. These medicines include, for example, dexamethasone, certain products for the treatment of epilepsy (e.g. those containing carbamazepine or phenytoin) or medicines used for the treatment of tuberculosis (e.g. rifampicin).
- Some medicines may increase the side effects of Buprenorphine Teva and may occasionally cause very serious reactions. Do not take any other medicine while you are taking Buprenorphine Teva without consulting your doctor first, especially antidepressants such as moclobemide, tranilcipromine, citalopram, escitalopram, fluoxetine, fluvoxamine, paroxetine, sertraline, duloxetine, venlafaxine, amitriptyline, doxepin, or trimipramine. These medicines may interact with Buprenorphine Teva, and you may experience symptoms such as involuntary muscle contractions, including the muscles that control eye movement, agitation, hallucinations, coma, excessive sweating, tremors, exaggerated reflexes, increased muscle tension, body temperature above 38 °C. Contact your doctor if you suffer from these symptoms.
Using Buprenorphine Teva with food, drinks, and alcohol
Do not drink alcohol while using Buprenorphine Teva. Alcohol may intensify certain side effects of the transdermal patch and may make you feel unwell. If you drink grapefruit juice, it may intensify the effects of Buprenorphine Teva.
Pregnancy, breast-feeding, and fertility
If you are pregnant or breast-feeding, think you may be pregnant, or are planning to have a baby, ask your doctor or pharmacist for advice before using this medicine.
There is no sufficient experience with the use of Buprenorphine Teva in pregnant women to date. Therefore, do not use Buprenorphine Teva during pregnancy.
Buprenorphine, the active ingredient contained in the transdermal patch, inhibits milk production and passes into breast milk. Therefore, do not use Buprenorphine Teva during breast-feeding.
Driving and using machines
Buprenorphine Teva may make you feel dizzy, drowsy, or have double or blurred vision, and may affect your reflexes so that you do not react adequately or quickly enough in the event of sudden or unexpected situations. This applies especially:
- at the beginning of treatment
- when changing the dose
- when changing from another medicine to Buprenorphine Teva
- if you are also taking other medicines that act on the brain
- if you drink alcohol
If you are affected, you should not drive or operate machinery while using Buprenorphine Teva. This also applies at the end of treatment with Buprenorphine Teva. Do not drive or operate machinery for at least 24 hours after removal of the patch.
In case of doubt, consult your doctor or pharmacist.
3. How to use Buprenorphine Teva
Follow your doctor's instructions for administering this medication exactly. If in doubt, consult your doctor or pharmacist again.
Before starting treatment and periodically during it, your doctor will discuss with you what you can expect from using this medication, when and for how long you should take it, when to contact your doctor, and when to stop taking it (see also "If you stop treatment with Buprenorphine Teva").
This medication is available in three doses: Buprenorphine Teva 35 micrograms/hour transdermal patch EFG, Buprenorphine Teva 52.5 micrograms/hour transdermal patch EFG, and Buprenorphine Teva 70 micrograms/hour transdermal patch EFG.
Your doctor has chosen this buprenorphine patch as the most suitable for you. During treatment, your doctor may change the transdermal patch you use to one with a lower or higher dose if necessary.
The recommended dose is:
Adults
Follow these instructions unless your doctor has given you different instructions. Apply the buprenorphine patch (as detailed below) and change it after four days, at most. To facilitate use, you can change the patch 2 times a week on fixed days, e.g., "always on Mondays in the morning and Thursdays in the afternoon". To help you remember when to change the transdermal patch, note it in the carton calendar. If your doctor has instructed you to take other painkillers in addition to the transdermal patch, strictly follow your doctor's instructions, or you will not fully benefit from the treatment with buprenorphine.
Children and adolescents
This medication should not be used in people under 18 years of age because there is no experience in this age group yet.
Elderly patients
No dose adjustment is required in elderly patients.
Patients with renal impairment / patients on dialysis
In patients with renal impairment and patients on dialysis, no dose adjustment is needed.
Patients with hepatic impairment
In patients with hepatic impairment, the intensity and duration of the action of buprenorphine may be affected. If you belong to this group of patients, your doctor will monitor you with greater care.
Method of administration
Before applying a transdermal patch
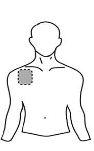
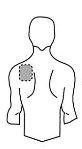
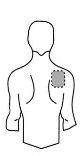
| Chest |
|
|
Back |
|
|
- If the chosen area has hair, cut it with scissors. Do not shave!
- Avoid areas of the skin that are red, irritated, or have any other type of spots, such as large scars.
- The area of skin you choose must be dry and clean. If necessary, wash it with cold or lukewarm water. Do not use soap or other detergents. After a hot bath or shower, wait until your skin is completely dry and cool. Do not apply lotions, creams, or ointments to the chosen area. This could prevent the transdermal patch from sticking properly.
Applying the transdermal patch:
Step 1: Each transdermal patch is sealed in an envelope. Just before use, cut the envelope along the sealed edge with scissors. Be careful not to damage the transdermal patches. Take the transdermal patch. |
|
Step 2: The adhesive side of the transdermal patch is covered by a transparent protective film. Carefully peel off halfof the film. Try not to touch the adhesive part of the transdermal patch. |
|
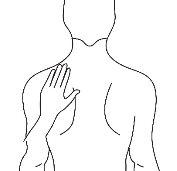
Step 3: Stick the transdermal patch to the area of skin you have chosen and remove the rest of the film. |
|
Step 4: Press the transdermal patch against your skin with the palm of your hand and count slowly to 30. Make sure the entire transdermal patch is in contact with your skin, especially the edges. |
|
Step 5: Wash your hands after using the transdermal patch. Do not use any cleaning products. | |
While wearing the transdermal patch
You can wear the transdermal patch for up to 4 days. If you have applied the transdermal patch correctly, the risk of it coming off is low. You can shower, bathe, or swim while wearing it. However, do not expose the transdermal patch to extreme heat (e.g., sauna, infrared lamps, electric blankets, or hot water bottles).
In the unlikely event that your transdermal patch falls off before you need to change it, do not use the same transdermal patch again. Apply a new one immediately (see "Changing the transdermal patch" below).
Changing the transdermal patch
- Remove the old patch carefully.
- Fold it in half with the adhesive side facing inward.
- Dispose of it with caution, out of sight and reach of children.
- Apply a new transdermal patch to a different area of skin (as described before). At least 1 week should pass before you can apply a new patch to the same area of skin.
Duration of treatment
Your doctor will indicate the duration of your treatment with this medication. Do not stop treatment with buprenorphine on your own, as the pain may return and you may feel unwell (see also "If you stop treatment with Buprenorphine Teva").
If you think the effect of this medication is too strong or too weak, tell your doctor or pharmacist.
If you use more Buprenorphine Teva than you should
If this happens, there may be signs of a buprenorphine overdose. An overdose can intensify the adverse effects of buprenorphine, such as drowsiness, nausea, and vomiting. You may have pinpoint pupils, and your breathing may become slow and weak. You could also suffer a cardiovascular collapse.
As soon as you realize you have used more transdermal patches than you should, remove the excess transdermal patches and consult your doctor or pharmacist immediately.
In case of overdose or accidental ingestion, consult the Toxicology Information Service, phone 91 562 04 20, indicating the medication and the amount used.
If you forget to use Buprenorphine Teva
If you forget an application, apply a new transdermal patch as soon as you remember. This will make you change your routine, e.g., if you normally apply your transdermal patch on Mondays and Thursdays, but you forget and do not apply the new transdermal patch until Wednesday, from then on you will need to change your transdermal patches on Wednesdays and Saturdays. Note the new pair of days in the carton calendar. If you change the transdermal patch too late, the pain may return. In this case, consult your doctor.
Never apply more than one transdermal patch to make up for the one you forgot!
If you stop treatment with Buprenorphine Teva
If you stop or finish treatment with this medication too soon, the pain will return. If you want to stop treatment due to unpleasant side effects, consult your doctor. Your doctor will tell you what you can do and if you can be treated with other medications.
Some people may experience withdrawal effects after using powerful painkillers for a long time and stopping them. The risk of having these effects after stopping the application of buprenorphine patches is very low. However, if you feel agitated, anxious, nervous, or restless, if you are hyperactive, have difficulty sleeping, or have digestive problems, consult your doctor.
If you have any other questions about using this medication, ask your doctor or pharmacist.
4. Possible side effects
Like all medications, this medication can cause side effects, although not everyone will experience them.
If you experience swelling of the hands, feet, knees, face, lips, mouth, or throat, which can cause difficulty swallowing or breathing, hives, fainting, yellowing of the skin and eyes (also called jaundice), remove the transdermal patch and consult your doctor or go to the nearest hospital immediately. These may be symptoms of a rare, severe allergic reaction.
The following side effects have been reported:
Very common(may affect more than 1 in 10 people):
- nausea (feeling sick)
- erythema, pruritus
Common(may affect up to 1 in 10 people)
- dizziness, headache
- shortness of breath
- vomiting, constipation
- skin changes (exanthema, usually due to repeated use), increased sweating
- edema (swelling of the legs), fatigue
Uncommon(may affect up to 1 in 100 people):
- confusion, sleep disorders, restlessness
- different degrees of sedation (serenity), ranging from fatigue to confusion
- circulatory disorders (such as hypotension or rarely, loss of consciousness due to a drop in blood pressure)
- dry mouth
- rash
- urinary retention (less urine than normal), urination disorders
- weakness (depression)
Rare(may affect up to 1 in 1,000 people):
- loss of appetite
- hallucinations, such as hallucinations, anxiety, nightmares, decreased sexual desire
- difficulty concentrating, speech disorders, confusion, balance disorders, abnormal sensations in the skin (feeling of heat, tingling, or numbness)
- vision changes, blurred vision, eyelid swelling
- hot flashes
- breathing difficulties (respiratory depression)
- heartburn
- hives
- erection difficulties
- withdrawal symptoms, reactions at the administration site
Very rare(may affect up to 1 in 10,000 people):
- severe allergic reactions
- dependence, mood changes
- muscle contraction, taste changes
- pinpoint pupils
- ear pain
- hyperventilation, hiccups
- gagging
- pustules, blisters
- chest pain
Frequency not known(frequency cannot be estimated from available data):
- contact dermatitis (skin rash with inflammation that may include a burning sensation), skin discoloration
If you notice any of the above side effects, consult your doctor as soon as possible.
In some cases, late local allergic reactions with marked signs of inflammation occur. In these cases, treatment with Buprenorphine Teva should be discontinued after consulting your doctor.
Some people may experience withdrawal symptoms after using powerful painkillers for a long time and stopping them. After treatment with Buprenorphine Teva, the risk of experiencing withdrawal symptoms is low. However, if you feel agitated, anxious, nervous, or restless, if you are hyperactive, have difficulty sleeping, or have digestive problems, consult your doctor.
Reporting side effects
If you experience any side effects, consult your doctor or pharmacist, even if they are possible side effects not listed in this leaflet. You can also report them directly through the Spanish Pharmacovigilance System for Human Use Medicines: https://www.notificaram.es. By reporting side effects, you can help provide more information on the safety of this medication.
5. Storage of Buprenorphine Teva
Keep this medication out of sight and reach of children.
Do not use this medication after the expiration date stated on the packaging and on the envelope after CAD. The expiration date is the last day of the month indicated.
This medication does not require special storage conditions.
Keep this medication in a safe and protected place, where others cannot access it. It can cause serious harm and be fatal if used accidentally or intentionally by people who have not been prescribed it.
Medications should not be thrown away in drains or trash. Deposit the packaging and medications you no longer need at the SIGRE Point in the pharmacy. If in doubt, ask your pharmacist how to dispose of the packaging and medications you no longer need. This will help protect the environment.
6. Package contents and additional information
Composition of Buprenorphine Teva
The active ingredient is buprenorphine.
Each 25 cm2 transdermal patch contains 20 mg of buprenorphine and releases 35 micrograms of buprenorphine per hour.
The other components are:
- Adhesive matrix (with buprenorphine) povidone K90, levulinic acid, oleyl oleate, poly[acrylic acid-co-butylacrylate-co-(2-ethylhexyl)acrylate-co-vinyl acetate] (5:15:75:5)
- Adhesive matrix (without buprenorphine): poly[(2-ethylhexyl)acrylate-co-glycidyl methacrylate-co-(2-hydroxyethyl)acrylate-co-vinyl acetate] (68:0.15:5:27)
- Separator film between the adhesive matrices with and without buprenorphine: poly(ethylene terephthalate) film.
- Coating layer: polyester.
- Protective release film (on the front covering the adhesive matrix containing buprenorphine): siliconized poly(ethylene terephthalate) film.
- Blue printing ink
Appearance of Buprenorphine Teva and package contents
Beige rectangular patch with rounded edges, printed with "Buprenorphine" and "35 μg / h"
Each transdermal patch is sealed in a child-resistant envelope. The patches are available in packs containing 3, 4, 5, 6, 8, 10, 12, 16, 18, or 20 transdermal patches.
Only some pack sizes may be marketed.
Marketing authorization holder
Teva Pharma S.L.U.
C/ Anabel Segura, 11 Edificio Albatros B, 1ª planta
28108 Alcobendas (Madrid)
Spain
Manufacturer
Labtec GmbH
Heykenaukamp 10, Hamburg
21147 Germany
or
Merckle GmbH
Ludwig-Merckle-Straße 3, Blaubeuren
89143 Germany
or
Teva Operations Poland Sp.z.o.o
ul. Mogilska 80, Krakow
31-546 Poland
This medication is authorized in the Member States under the following names:
Germany: | Buprenoratiopharm 35 Mikrogramm/Stunde Transdermales Pflaster |
Austria: | Buprenorphin ratiopharm 35 Mikrogramm/h transdermales Pflaster |
Belgium: | Buprenorphine Teva 35 microgram/u pleister voor transdermaal gebruik Buprenorphine Teva 35 microgrammes/h dispositif transdermique Buprenorphine Teva 35 Mikrogramm/S transdermales Pflaster |
Spain: | Buprenorfina Teva 35 microgramos/hora parche transdérmico EFG |
Finland: | Buprenorphine ratiopharm 35 mikrog/tunti depotlaastari |
Croatia: | Laribon 35 mikrograma/h transdermalni flaster |
Netherlands: | Buprenorfine Teva 35 microgram/uur pleister voor transdermaal gebruik |
Portugal: | Buprenorfina ratiopharm |
United Kingdom: | Timpron 35 micrograms/h Transdermal patch |
Date of the last revision of this leaflet:October 2024
Detailed and updated information on this medication is available on the website of the Spanish Agency for Medicines and Health Products (AEMPS) http://www.aemps.gob.es/
You can access detailed and updated information about this medication by scanning the QR code included in the packaging with your smartphone. You can also access this information at the following internet address: https://cima.aemps.es/cima/dochtml/p/80609/P_80609.html
QR+URL
- Country of registration
- Average pharmacy price21.53 EUR
- Active substance
- Prescription requiredYes
- Manufacturer
- This information is for reference only and does not constitute medical advice. Always consult a doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to BUPRENORPHINE TEVA 35 micrograms/hour transdermal patchDosage form: TRANSDERMAL PATCH, 35 micrograms/hourActive substance: buprenorphineManufacturer: Andromaco Pharma S.L.Prescription requiredDosage form: TRANSDERMAL PATCH, 52.5 micrograms/hourActive substance: buprenorphineManufacturer: Andromaco Pharma S.L.Prescription requiredDosage form: TRANSDERMAL PATCH, 70 micrograms/hourActive substance: buprenorphineManufacturer: Andromaco Pharma S.L.Prescription required
Online doctors for BUPRENORPHINE TEVA 35 micrograms/hour transdermal patch
Discuss questions about BUPRENORPHINE TEVA 35 micrograms/hour transdermal patch, including use, safety considerations and prescription review, subject to medical assessment and local regulations.
Frequently Asked Questions