
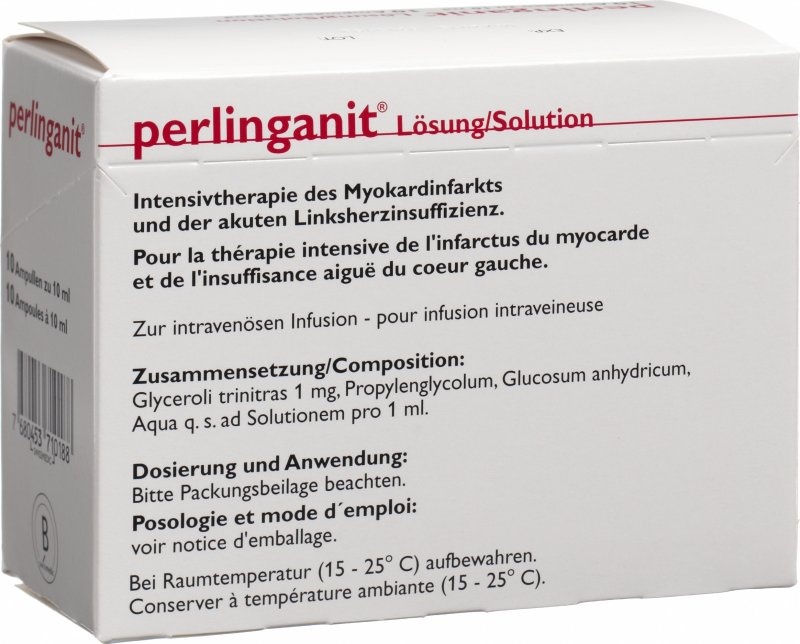
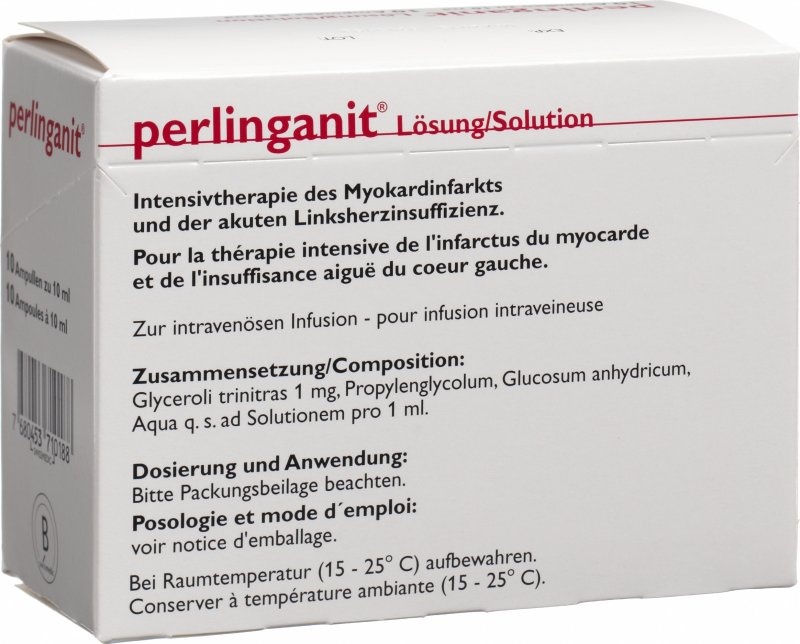
Perlinganit
Ask a doctor about a prescription for Perlinganit

How to use Perlinganit
Leaflet attached to the packaging: patient information
Perlinganit, 1 mg/ml, solution for infusion
Glyceryl trinitrate
You should carefully read the contents of the leaflet before using the medicine, as it contains important information for the patient.
- You should keep this leaflet, so that you can read it again if you need to.
- If you have any doubts, you should consult a doctor, pharmacist, or nurse.
- This medicine has been prescribed specifically for you. Do not pass it on to others. The medicine may harm another person, even if their symptoms are the same as yours.
- If you experience any side effects, including those not listed in this leaflet, you should tell your doctor, pharmacist, or nurse. See section 4.
Table of contents of the leaflet
- 1. What is Perlinganit and what is it used for
- 2. Important information before using Perlinganit
- 3. How to use Perlinganit
- 4. Possible side effects
- 5. How to store Perlinganit
- 6. Contents of the packaging and other information
1. What is Perlinganit and what is it used for
Perlinganit contains glyceryl trinitrate (1 ml of solution for intravenous infusion contains 1 mg of glyceryl trinitrate). The medicine belongs to the group of organic nitrates. It has a direct vasodilating effect on the muscles of blood vessel walls. Under the influence of the medicine, blood vessels expand. Perlinganit mainly expands venous vessels and, in higher doses, also arterial vessels. This reduces the burden on the heart and the demand for oxygen in the heart muscle. The medicine also improves blood flow through the heart muscle, which reduces cardiac ischemia. As a result, pain symptoms and the size of the heart muscle damage decrease. Additionally, the medicine counteracts coronary vessel spasms. Perlinganit also has a beneficial effect on patients with chronic heart failure, reducing symptoms and improving exercise tolerance in these patients. Other possible effects of the medicine include: relaxation of smooth muscles in the bronchi, digestive tract, bile ducts, urinary system, and uterus, but these effects have no significant therapeutic importance. Indications for use of the medicine:
- Unstable angina pectoris, including variant angina (Prinzmetal's angina)
- Acute myocardial infarction
- Acute left ventricular failure
- Hypertensive crisis with congestive heart failure
- Controlled lowering of blood pressure
2. Important information before using Perlinganit
When not to use Perlinganit:
During treatment with Perlinganit, you must not take the following medicines (see also the section "Perlinganit and other medicines"):
- phosphodiesterase inhibitors (medicines used for erectile dysfunction), such as sildenafil, vardenafil, tadalafil,
- riociguat (a medicine used for chronic thromboembolic pulmonary hypertension and pulmonary arterial hypertension).
Warnings and precautions
Before starting treatment with Perlinganit, you should consult a doctor or pharmacist. You should exercise particular caution when using Perlinganit:
- in myocardial infarction with low filling pressure,
Administration of even small doses of Perlinganit may cause a significant drop in blood pressure (especially in patients with hypovolemia or low blood pressure before infusion) with excessive slowing of heart rate, cerebral hypoxia, or worsening of ischemic heart disease symptoms. The medicine may also exacerbate symptoms of ischemic heart disease in patients with hypertrophic cardiomyopathy and left ventricular outflow tract obstruction. In some patients receiving Perlinganit infusion for 12 hours a day, during breaks in treatment, coronary pain may occur. During administration of the medicine, tolerance and cross-tolerance to other nitrates may develop. To avoid this phenomenon, the smallest effective doses of the medicine are used, and glyceryl trinitrate is periodically administered alternately with other vasodilating medicines. There have been reports of methemoglobinemia (a blood disorder characterized by: cyanosis, dyspnea, headache, dizziness, drowsiness, and coma; can be fatal) after treatment with glyceryl trinitrate. Treatment of methemoglobinemia with methylene blue is contraindicated in patients with glucose-6-phosphate dehydrogenase deficiency or methemoglobin reductase deficiency. Perlinganit should not be used in patients who have taken medicines containing phosphodiesterase inhibitors (e.g., sildenafil, vardenafil, tadalafil) in the last 24 hours (48 hours for tadalafil). Patients treated with Perlinganit should not take phosphodiesterase inhibitors. During treatment with this medicine, you should avoid consuming alcohol, as it may enhance the hypotensive and vasodilating effects of glyceryl trinitrate.
Children and adolescents
The safety and efficacy of the medicine in children have not been established.
Using Perlinganit in patients with renal and/or hepatic impairment
The doctor will decide on the appropriate dose adjustment in patients with severe liver and/or kidney failure. See also section 3 "How to use Perlinganit".
Using Perlinganit in elderly patients
The doctor will decide on the appropriate dose adjustment in elderly patients. See also section 3 "How to use Perlinganit".
Pregnancy, breastfeeding, and fertility
If you are pregnant or breastfeeding, think you may be pregnant, or plan to have a child, you should consult a doctor before using this medicine. Perlinganit may be used in pregnant women only under the supervision of a doctor, and only when the doctor believes that the benefits to the mother outweigh the potential risks to the fetus. Data indicate that glyceryl trinitrate may be excreted into human milk. Therefore, Perlinganit should be avoided in breastfeeding women. There are no data on the effects of glyceryl trinitrate on human fertility.
Driving and using machines
Perlinganit may impair the ability to drive vehicles and operate machinery. This effect is enhanced by concurrent alcohol consumption.
Perlinganit and other medicines
You should tell your doctor about all medicines you are currently taking or have recently taken, as well as any medicines you plan to take. Concurrent use of other medicines with hypotensive effects, such as beta-adrenergic blockers, calcium antagonists, vasodilating medicines, angiotensin-converting enzyme inhibitors, monoamine oxidase inhibitors, diuretics, and alcohol, may enhance the hypotensive effect of glyceryl trinitrate. Such an effect may also occur with the use of neuroleptics and tricyclic antidepressants. Phosphodiesterase inhibitors (e.g., sildenafil, vardenafil, tadalafil) may also enhance the hypotensive effect of glyceryl trinitrate. This may lead to life-threatening cardiovascular complications. Therefore, glyceryl trinitrate should not be used in patients who have taken phosphodiesterase inhibitors in the last 24 hours (48 hours for tadalafil). Concurrent administration of tissue plasminogen activator (t-PA) and Perlinganit may increase the clearance of t-PA by increasing blood flow through the liver. Concurrent use of Perlinganit and dihydroergotamine may increase the concentration of the latter in the blood, leading to increased blood pressure. Caution is advised in patients with ischemic heart disease, as dihydroergotamine may counteract the effects of glyceryl trinitrate, leading to coronary vasoconstriction. In patients previously treated with organic nitrates (e.g., isosorbide dinitrate or mononitrate), higher doses of Perlinganit may be necessary to achieve the desired effects. Caution is advised when using products containing sapropterin. Nonsteroidal anti-inflammatory drugs (e.g., ibuprofen), except for acetylsalicylic acid, may reduce the therapeutic effect of glyceryl trinitrate. Concurrent use of heparin and Perlinganit may reduce the effect of heparin. Concurrent use of Perlinganit and acetylsalicylic acid may reduce blood pressure. Concurrent use of Perlinganit and riociguat is contraindicated, as it may cause hypotension (low blood pressure).
Perlinganit contains glucose
A 10 ml ampoule contains 480 mg of glucose. This should be taken into account in patients with diabetes.
3. How to use Perlinganit
This medicine should always be used in accordance with the doctor's recommendations. If you have any doubts, you should consult a doctor. The doctor will adjust the dosage to the patient's needs. Perlinganit is administered in a hospital setting, either as a diluted solution (in continuous intravenous infusion using an automatic device regulating the drip rate) or as an undiluted solution (using a syringe pump), with constant monitoring of cardiovascular parameters. Depending on the type and severity of the disease, it may be necessary to perform invasive hemodynamic measurements during treatment as a supplement to routine diagnostic tests (blood pressure measurements, heart rate, diuresis). The dosage should be adjusted individually to the patient's needs. Administration of Perlinganit starts with a dose of 0.75 to 1.0 mg/h, then the dose is adjusted according to the patient's needs, usually not exceeding 8 mg/h, and in rare cases up to 10 mg/h. It is recommended to start the infusion at a low rate (even 5 μg/min), increasing the rate every 3 to 5 minutes by 5 to 10 μg/min until a response is achieved. In patients with severe angina pectoris, doses of 2 to 8 mg/h (33 to 133 μg/min) should be used. In acute left ventricular failure (pulmonary edema), the medicine should be administered at a dose of 2 to 8 mg/h in continuous infusion for 1 to 2 days. In acute myocardial infarction, to combat coronary pain (when opioid administration is insufficient), 2 to 8 mg/h should be used until the pain subsides. In patients with hypertensive crisis and heart failure, Perlinganit should be used in intravenous infusion at a dose of 2 to 8 mg/h (average 5 mg/h) under constant control of blood pressure and heart rate. In controlled blood pressure lowering, depending on the method of general anesthesia used and the degree of expected blood pressure reduction, 2 to 10 μg of Perlinganit per kg of body weight per minute should be used, under constant control of blood pressure (invasive measurement) and ECG. Preparation of the Perlinganit solution should be performed under aseptic conditions, immediately after opening the ampoule. Perlinganit can be administered with commonly used intravenous infusion solutions, such as physiological saline, 5% or 10% glucose solution, or Ringer's solution. When diluting the Perlinganit solution with an infusion solution, the manufacturer's recommendations should be followed, especially regarding compatibility with other substances, contraindications, side effects, and interactions.
Dilution table
| Amount of active substance (glyceryl trinitrate) | 10 mg | 20 mg | 30 mg | 40 mg | 50 mg | |
| Perlinganit solution | 10 ml | 20 ml | 30 ml | 40 ml | 50 ml | |
| Amount of infusion solution to achieve the following dilutions (in milliliters): | 1+10 1+20 1+40 | 100 200 400 | 200 400 800 | 300 600 1200 | 400 800 1600 | 500 1000 2000 |
| Amount of ready-to-use solution for infusion (in milliliters): | 1+10 1+20 1+40 | 110 210 410 | 220 420 820 | 330 630 1230 | 440 840 1640 | 550 1050 2050 |
Dosing of Perlinganit after dilution
The medicine does not contain ethanol or potassium ions. The doctor will decide on the appropriate dosing of Perlinganit in patients with severe liver or kidney failure, or in elderly patients. The table below shows the recommended doses of glyceryl trinitrate and the corresponding infusion rates for different dilutions.
| Dilution | 1 + 10 | 1 + 20 | 1 + 40 |
| Recommended dose of glyceryl trinitrate per hour | Infusion rate ml/hour | Infusion rate ml/hour | Infusion rate ml/hour |
| 0.50 mg 5.50 10.50 20.50 0.75 mg 8.25 15.75 30.75 1.00 mg 11.00 21.00 41.00 1.25 mg 13.75 26.25 51.25 1.50 mg 16.50 31.50 61.50 2.00 mg 22.00 42.00 82.00 2.50 mg 27.50 52.50 102.50 3.00 mg 33.00 63.00 123.00 3.50 mg 38.50 73.50 143.50 4.00 mg 44.00 84.00 164.00 4.50 mg 49.50 94.50 184.50 5.00 mg 55.00 105.00 205.00 5.50 mg 60.50 115.50 225.50 6.00 mg 66.00 126.00 246.00 7.00 mg 77.00 147.00 287.00 8.00 mg 88.00 168.00 328.00 9.00 mg 99.00 189.00 369.00 10.00 mg 110.00 210.00 410.00 | |||
Usually, treatment starts with the lowest possible dose, and then the dose is increased or decreased according to the response to treatment. Administration of glyceryl trinitrate is recommended to start with an infusion rate of 5 to 10 μg/min, increasing every 5 minutes by 5 μg/min until a response is achieved. The dose can be increased up to a maximum of 167 μg/min. The doctor will decide on the appropriate monitoring of blood pressure and maintaining its level ≥90 mmHg, modifying the infusion rate of glyceryl trinitrate accordingly. There are no data indicating the need for dose adjustment in elderly patients. WarningInfusion sets for Perlinganit solution should be made of polyethylene (PE), polypropylene (PP), or polytetrafluoroethylene (PTFE). Other materials, such as polyvinyl chloride (PVC) or polyurethane (PU), cause adsorption of glyceryl trinitrate to the infusion set wall and reduce the concentration of the medicine in the solution. When using materials made of PVC or PU, the dosage should be adjusted individually, depending on the patient's needs. Tolerance and cross-tolerance to other nitrate compounds have been reported during treatment with Perlinganit. If you feel that the effect of Perlinganit is too strong or too weak, you should consult a doctor.
Using a higher than recommended dose of Perlinganit
If you have taken a higher dose of Perlinganit than recommended, you should immediately consult a doctor or pharmacist.Overdose may lead to: excessive lowering of blood pressure (systolic blood pressure below 90 mmHg), pallor, increased sweating, decreased pulse, tachycardia, dizziness due to changes in body position, headache, weakness, dizziness, nausea, vomiting, and diarrhea. After administration of organic nitrates, including Perlinganit, there have been reports of methemoglobinemia with cyanosis, dyspnea, headache, dizziness, drowsiness, and coma. Very high doses may cause increased intracranial pressure and cerebral symptoms. Treatment should focus on increasing blood pressure. In mild overdose, it is sufficient to place the patient with their legs elevated. In more severe poisonings, treatment should be in accordance with the recommendations for the treatment of poisonings and shock, and immediate medical attention is necessary.
4. Possible side effects
Like all medicines, Perlinganit can cause side effects, although not everybody gets them. During treatment with Perlinganit, the following side effects have been observed: Very common (occurring in more than 1 in 10 patients): headache, Common (occurring in more than 1 in 100 patients): tachycardia, weakness, dizziness (including those related to changes in body position), drowsiness, orthostatic hypotension, Uncommon (occurring in less than 1 in 100 patients): worsening of angina pectoris symptoms, circulatory collapse (sometimes with bradycardia and arrhythmias, and loss of consciousness), nausea, vomiting, skin allergic reactions (e.g., rash), contact allergy, itching, feeling of heat (burning), flushing, and skin irritation. Rare (occurring in less than 1 in 10,000 patients): heartburn. Frequency not known (frequency cannot be estimated from the available data): hypotension (reduced blood pressure), sudden flushing of the face with a feeling of heat, palpitations, generalized rash, tachycardia. Isolated cases: exfoliative dermatitis. During treatment with organic nitrates, including Perlinganit, there have been reports of significant lowering of blood pressure with nausea, vomiting, anxiety, pallor, and excessive sweating. Note: During treatment with Perlinganit, temporary reduction of oxygen partial pressure in the blood may occur due to relative redistribution of blood flow to poorly ventilated areas of the lungs. This may lead to hypoxia of the heart muscle, especially in patients with coronary artery disease. Perlinganit may cause dose-dependent headaches related to cerebral vasodilation. These symptoms usually disappear despite continued treatment. If headaches persist during treatment, mild painkillers should be used. If headaches do not respond to treatment, the doctor will decide on reducing the dose of Perlinganit or discontinuing its administration. If necessary, the doctor will decide on treatment with a beta-adrenergic blocker to avoid slight tachycardia. Reporting side effects If you experience any side effects, including those not listed in this leaflet, you should tell your doctor, pharmacist, or nurse. Side effects can be reported directly to the Department of Monitoring of Adverse Reactions to Medicinal Products of the Office for Registration of Medicinal Products, Medical Devices, and Biocidal Products: Al. Jerozolimskie 181C, 02-222 Warsaw, tel.: 22 49-21-301, fax: 22 49-21-309, Website: https://smz.ezdrowie.gov.pl Side effects can also be reported to the marketing authorization holder. By reporting side effects, you can help provide more information on the safety of this medicine.
5. How to store Perlinganit
Do not store above 25°C. The medicine should be stored out of sight and reach of children. Do not use this medicine after the expiry date stated on the carton. The expiry date refers to the last day of the month. Medicines should not be disposed of via wastewater or household waste. You should ask your pharmacist how to dispose of medicines that are no longer needed. This will help protect the environment.
6. Contents of the packaging and other information
What Perlinganit contains
- The active substance of the medicine is glyceryl trinitrate. 1 ampoule (10 ml) contains 10 mg of glyceryl trinitrate in 10 ml of isotonic solution.
- The other ingredients of the medicine are: propylene glycol, glucose, hydrochloric acid, water for injections.
What Perlinganit looks like and what the pack contains
Perlinganit 1 mg/ml, solution for infusion, is a clear, colorless, and odorless solution. Perlinganit is available in packs of: 10 ampoules of 10 ml, in a cardboard box. The Perlinganit solution is sterile and does not contain preservatives. The ampoule is not intended for multiple use.
Marketing authorization holder and manufacturer
Marketing authorization holder: Merus Labs Luxco II S.à.R.L. 208, Val des Bons Malades L-2121 Luxembourg Luxembourg Manufacturer: Aesica Pharmaceuticals GmbH Alfred-Nobel-Str. 10 40789 Monheim Germany For more detailed information, you should consult the representative of the marketing authorization holder. Merus Labs Luxco II S.à.R.L. 208, Val des Bons Malades L-2121 Luxembourg Luxembourg
Date of last revision of the leaflet: 01/12/2022
- Country of registration
- Active substance
- Prescription requiredNo
- Manufacturer
- ImporterAesica Pharmaceuticals GmbH
- This information is for reference only and does not constitute medical advice. Always consult a licensed doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to PerlinganitDosage form: Ointment, 20 mg/gActive substance: glyceryl trinitrateManufacturer: Chema-Elektromet Spółdzielnia PracyPrescription not requiredDosage form: Aerosol, 0.4 mg/doseActive substance: glyceryl trinitrateManufacturer: EGIS Pharmaceuticals PLCPrescription requiredDosage form: Tablets, 6.5 mgActive substance: glyceryl trinitratePrescription required
Alternatives to Perlinganit in other countries
The best alternatives with the same active ingredient and therapeutic effect.
Alternative to Perlinganit in Spain
Alternative to Perlinganit in Ukraine
Online doctors for Perlinganit
Discuss dosage, side effects, interactions, contraindications, and prescription renewal for Perlinganit – subject to medical assessment and local rules.










