
How to use Nuvaring
Leaflet accompanying the packaging: information for the user
Warning! The leaflet should be kept. Information on the immediate packaging in a foreign language.
NuvaRing, (0.120 mg + 0.015 mg)/24 h, vaginal therapeutic system
Etonogestrel + Ethinylestradiol
Important information about combined hormonal contraceptives
- If used correctly, they are one of the most reliable, reversible methods of contraception.
- To a small extent, they increase the risk of blood clots in veins and arteries, especially in the first year of use or after resuming use after a break of 4 weeks or more.
- One should be vigilant and consult a doctor if the patient suspects that symptoms of blood clots have occurred (see section 2 "Blood clots").
One should carefully read the contents of the leaflet before using the medicine, as it contains important information for the patient.
- One should keep this leaflet, so that it can be re-read if necessary.
- In case of any doubts, one should consult a doctor or pharmacist.
- This medicine has been prescribed to a specific person. It should not be given to others. The medicine may harm another person.
- If the patient experiences any side effects, including any side effects not listed in this leaflet, they should tell their doctor, pharmacist, or nurse. See section 4.
Table of contents of the leaflet
- 1. What NuvaRing is and what it is used for
- 2. Important information before using NuvaRing
- 3. How to use NuvaRing
- 4. Possible side effects
- 5. How to store NuvaRing
- 6. Contents of the packaging and other information
1. What NuvaRing is and what it is used for
NuvaRing is a contraceptive in the form of a vaginal therapeutic system, preventing pregnancy. Each vaginal therapeutic system contains a small amount of two female sex hormones - etonogestrel and ethinylestradiol. These hormones are slowly released from the system into the bloodstream. Due to the small dose of hormones released, NuvaRing is classified as a low-dose hormonal contraceptive. Since NuvaRing releases two different hormones, it is also a combined contraceptive.
2. Important information before using NuvaRing
General notes
Before starting to use NuvaRing, one should read the information about blood clots (thrombosis) in section 2. It is especially important to read about the symptoms of blood clots (see section 2 "Blood clots").
NuvaRing, like other hormonal contraceptives, does not protect against HIV infection (AIDS) or other sexually transmitted diseases.
2.1 When not to use NuvaRing
NuvaRing should not be used if the patient has any of the following conditions. If the patient has any of the following conditions, they must inform their doctor. The doctor will discuss with the patient which other contraceptive method will be more suitable.
- if the patient currently has (or has ever had) a blood clot in the veins of the legs (deep vein thrombosis), in the lungs (pulmonary embolism), or in other organs,
- if the patient knows they have a blood clotting disorder - for example, protein C deficiency, protein S deficiency, antithrombin III deficiency, factor V Leiden, or antiphospholipid antibodies,
- if the patient needs to have surgery or will be immobilized for a long time (see section "Blood clots"),
- if the patient has had a heart attack or stroke,
- if the patient has (or has had in the past) angina pectoris (a disease that causes severe chest pain, which can be the first symptom of a heart attack) or a transient ischemic attack (temporary stroke symptoms),
- if the patient has any of the following diseases, which may increase the risk of a blood clot in an artery:
- severe diabetes with blood vessel damage
- very high blood pressure
- very high levels of fats in the blood (cholesterol or triglycerides)
- hyperhomocysteinemia
- if the patient has (or has had in the past) a type of migraine called "migraine with aura",
- if the patient has (or has had in the past) pancreatitis associated with high levels of fats in the blood,
- if the patient has (or has had in the past) severe liver disease, and liver function has not returned to normal,
- if the patient has (or has had in the past) a benign or malignant liver tumor,
- if the patient has (or has had in the past) breast cancer or cancer of the genital organs, or if there is a suspicion of these cancers,
- if the patient has unexplained vaginal bleeding,
- if the patient is allergic to ethinylestradiol or etonogestrel or any of the other ingredients of this medicine (listed in section 6).
If any of the above symptoms occur for the first time during the use of NuvaRing, the system should be removed from the vagina immediately and a doctor should be consulted. In the meantime, a non-hormonal contraceptive method should be used.
2.2 Warnings and precautions
When should one contact a doctor?
- if the patient notices possible symptoms of a blood clot, which may indicate that the patient has a blood clot in the leg (deep vein thrombosis), a blood clot in the lungs (pulmonary embolism), a heart attack, or a stroke (see section below "Blood clots").
One should tell the doctor if the patient has any of the following conditions.
If these symptoms occur or worsen during the use of NuvaRing, one should also tell the doctor.
- if breast cancer occurs in the patient's close relatives;
- if the patient has epilepsy (see section 2.4 "NuvaRing and other medicines");
- if the patient has liver disease (e.g., jaundice) or gallbladder disease (e.g., gallstones);
- if the patient has Crohn's disease or ulcerative colitis (chronic inflammatory bowel diseases);
- if the patient has systemic lupus erythematosus (a disease that affects the body's natural defense system);
- if the patient has hemolytic uremic syndrome (a blood clotting disorder that causes kidney failure);
- if the patient has sickle cell anemia (a hereditary disease of red blood cells);
- if the patient has been diagnosed with high levels of fats in the blood (hypertriglyceridemia) or a positive family history for this disease. Hypertriglyceridemia is associated with an increased risk of developing pancreatitis;
- if the patient needs to have surgery or will be immobilized for a long time (see section 2 "Blood clots");
- if the patient has recently given birth, as they are at increased risk of blood clots. One should consult a doctor to find out how soon they can start using NuvaRing after giving birth;
- if the patient has superficial thrombophlebitis (blood clots in the veins under the skin);
- if the patient has varicose veins;
- if the patient has diseases that occurred for the first time or worsened during pregnancy or previous use of sex hormones (e.g., hearing loss, porphyria [a blood disease], pregnancy herpes [a blistering skin rash during pregnancy], or Sydenham's chorea [a neurological disorder characterized by involuntary, sudden movements of the body]);
- one should consult a doctor immediately if symptoms of angioedema occur, such as swelling of the face, tongue, and/or throat, and/or difficulty swallowing or a rash that may be associated with difficulty breathing. Estrogen-containing medicines may cause or worsen the symptoms of hereditary and acquired angioedema;
- if the patient has chloasma (yellow-brown patches, so-called "pregnancy patches", especially on the face) now or in the past. If they occur, one should avoid excessive sun exposure and ultraviolet radiation;
Page 3 of 18
- if the patient has conditions that make it difficult to use NuvaRing, such as frequent constipation, uterine prolapse, or pain during intercourse;
- if the patient experiences sudden, frequent need to urinate with a burning sensation and/or pain, and if the patient cannot locate the vaginal therapeutic system inside the vagina. These symptoms may indicate that the vaginal therapeutic system has been accidentally inserted into the bladder.
BLOOD CLOTS
The use of combined hormonal contraceptives, such as the NuvaRing vaginal therapeutic system, is associated with an increased risk of blood clots, compared to not using them. In rare cases, a blood clot can block a blood vessel and cause serious complications.
- in the veins (also known as "venous thromboembolism" or "deep vein thrombosis");
- in the arteries (also known as "arterial thromboembolism").
Not all patients who have a blood clot will recover fully. In rare cases, the effects of a blood clot can be permanent or, very rarely, fatal.
One should remember that the overall risk of serious blood clots caused by NuvaRing is small.
HOW TO RECOGNIZE THE OCCURRENCE OF BLOOD CLOTS
One should consult a doctor immediately if they notice any of the following symptoms.
- swelling of the leg or swelling along a vein in the leg or foot, especially if it is accompanied by:
- pain or tenderness in the leg, which may only be felt when standing or walking,
- increased temperature in the affected leg,
- change in skin color of the leg, such as pallor, redness, or discoloration. Deep vein thrombosis
- sudden unexplained shortness of breath or rapid breathing;
- sudden cough without an obvious cause, which may be accompanied by coughing up blood;
- sharp chest pain, which may worsen with deep breathing;
- severe dizziness or fainting;
- rapid or irregular heartbeat;
- severe abdominal pain. If the patient is unsure, they should consult a doctor, as some of these symptoms, such as coughing or shortness of breath, may be mistaken for milder conditions, such as a respiratory infection (e.g., a cold). Symptoms usually occur in one eye:
- sudden loss of vision or
- painless vision disturbances, which may progress to vision loss. Retinal vein thrombosis (blood clot in the eye)
Page 4 of 18
| Heart attack |
| Stroke |
| Blood clots blocking other blood vessels |
BLOOD CLOTS IN VEINS
What can happen if blood clots form in veins?
- The use of combined hormonal contraceptives is associated with an increased risk of blood clots in veins (venous thromboembolism). Although these side effects are rare, they can occur. Most often, they occur in the first year of using combined hormonal contraceptives.
- If blood clots form in the veins in the leg or foot, it can lead to the development of deep vein thrombosis.
- If a blood clot moves from the leg and settles in the lungs, it can cause pulmonary embolism.
- In very rare cases, a blood clot can form in another organ, such as the eye (retinal vein thrombosis).
When is the risk of blood clots in veins highest?
The risk of forming blood clots in veins is highest during the first year of using combined hormonal contraceptives for the first time. The risk may also be higher when resuming the use of combined hormonal contraceptives (the same or a different medicine) after a break of 4 weeks or more.
What affects the risk of blood clots in veins?
Page 5 of 18
The risk of blood clots in veins associated with the use of the NuvaRing vaginal therapeutic system is small, but some factors can increase this risk.
- if the patient is severely overweight (body mass index (BMI) over 30 kg/m^2);
- if someone in the patient's close family has had blood clots in the legs, lungs, or other organs at a young age (e.g., under 50 years old). In this case, the patient may have a hereditary blood clotting disorder;
- if the patient needs to have surgery or will be immobilized for a long time due to injury or illness or has a leg in a cast. It may be necessary to stop using NuvaRing for a few weeks before surgery or immobilization. If the patient needs to stop using NuvaRing, they should ask their doctor when they can resume using it;
- with age (especially over 35 years);
- if the patient has recently given birth.
The risk of blood clots increases with the number of risk factors present in the patient.
Traveling by air (>4 hours) may temporarily increase the risk of blood clots, especially if the patient has another risk factor.
It is essential to tell the doctor if any of the above factors occur in the patient, even if they are unsure. The doctor may decide to stop the use of NuvaRing.
One should inform the doctor if any of the above conditions change during the use of NuvaRing, e.g., if someone in the patient's close family is diagnosed with a blood clot without a known cause or if the patient gains significant weight.
BLOOD CLOTS IN ARTERIES
Page 6 of 18
What can happen if blood clots form in arteries?
Similarly to blood clots in veins, blood clots in arteries can cause serious consequences, such as a heart attack or stroke.
Factors that increase the risk of blood clots in arteries
It is essential to note that the risk of heart attack or stroke associated with the use of the NuvaRing vaginal therapeutic system is very small, but it may increase:
- with age (over approximately 35 years);
- if the patient smokes. While using a hormonal contraceptive like the NuvaRing vaginal therapeutic system, it is recommended to quit smoking. If the patient is unable to quit smoking and is over 35 years old, the doctor may recommend using a different type of contraception;
- if the patient is overweight;
- if the patient has high blood pressure;
- if someone in the patient's close family has had a heart attack or stroke at a young age (under 50 years old). In this case, the patient may also be at increased risk of having a heart attack or stroke;
- if the patient or someone in their close family has been diagnosed with high levels of fats in the blood (cholesterol or triglycerides);
- if the patient has migraines, especially migraines with aura;
- if the patient has heart disease (valve damage, heart rhythm disturbance called atrial fibrillation);
- if the patient has diabetes.
If the patient has more than one of the above conditions or if any of them are severe, the risk of blood clots may be even higher.
One should inform the doctor if any of the above conditions change during the use of the NuvaRing vaginal therapeutic system, e.g., if the patient starts smoking, if someone in their close family is diagnosed with a blood clot without a known cause, or if the patient gains significant weight.
Cancer
The following information is based on studies using combined oral contraceptives and may also apply to NuvaRing. Information on the vaginal use of hormonal contraceptives (as in the case of NuvaRing) is not available.
Among women using combined contraceptives, a slightly higher incidence of breast cancer has been found, although it is not known whether this is caused by the medicines used. It is possible that women using combined contraceptives are more likely to have their breasts examined, which may lead to more tumors being detected.
The increased incidence of breast cancer stops gradually after stopping the use of combined contraceptives.
Regular breast examination is very important. If a lump is found, one should consult a doctor. One should also inform the doctor if someone in their close family has had or has breast cancer (see section 2.2 "Warnings and precautions").
In rare cases, women using combined contraceptives have been found to have benign liver tumors, and very rarely, malignant liver tumors as well. If the patient experiences unusual, severe abdominal pain, they should consult their doctor.
There have been reports that women using combined contraceptives are less likely to develop endometrial cancer (cancer of the lining of the uterus) and ovarian cancer. It is possible that this also applies to NuvaRing, but this has not been confirmed yet.
Page 7 of 18
Mental disorders
Some women using hormonal contraceptives, including NuvaRing, have reported depression or low mood. Depression can be severe and sometimes lead to suicidal thoughts. If mood changes and symptoms of depression occur, one should consult a doctor as soon as possible for further medical advice.
2.3 Children and adolescents
The safety and efficacy of NuvaRing have not been studied in adolescents under the age of 18.
2.4 NuvaRing and other medicines
One should always tell their doctor about the medicines or herbal products they are currently using. One should also inform their doctor of another specialty or dentist prescribing other medicines (or pharmacist) about the use of NuvaRing. They may inform about the need to use an additional contraceptive method (e.g., a male condom), and if so, for how long, as well as whether it is necessary to modify the use of another medicine.
Some medicines
- may affect the level of NuvaRing in the blood;
- may reduce its contraceptive effectiveness;
- may cause unexpected bleeding.
This applies to medicines used to treat:
- epilepsy (e.g., primidone, phenytoin, barbiturates, carbamazepine, oxcarbazepine, topiramate, felbamate);
- tuberculosis (e.g., rifampicin);
- HIV infection (e.g., ritonavir, nelfinavir, nevirapine, efavirenz);
- hepatitis C virus infection (e.g., boceprevir, telaprevir);
- other infectious diseases (e.g., griseofulvin);
- high blood pressure in the blood vessels of the lungs (bosentan);
- depressive moods (St. John's Wort).
If the patient is taking medicines or herbal products that may reduce the effectiveness of NuvaRing, they should use a mechanical contraceptive method (e.g., a male condom) as well. Due to the fact that the effect of another medicine on NuvaRing may persist for up to 28 days after stopping the medicine, it is necessary to use additional mechanical contraception during this time.
Note: NuvaRing should not be used with a diaphragm, cervical cap, or female condom.
NuvaRing may affect the action of other medicines, such as:
- medicines containing cyclosporin;
- the antiepileptic medicine lamotrigine (this may lead to an increased frequency of seizures).
If the patient has a hepatitis C virus infection and is taking medicines containing ombitasvir, paritaprevir, ritonavir, and dasabuvir or glecaprevir, pibrentasvir, NuvaRing should not be used, as it may cause an increase in liver function test results in the blood (an increase in the activity of the liver enzyme ALT).
Before starting these medicines, the doctor will prescribe a different type of contraceptive.
The use of the NuvaRing vaginal therapeutic system can be resumed about 2 weeks after the end of this treatment. See section 2.1 "When not to use NuvaRing".
Page 8 of 18
Before taking any medicine, one should consult a doctor or pharmacist.
During the use of NuvaRing, tampons can be used at the same time. One should insert NuvaRing before inserting a tampon. One should be careful when removing a tampon to avoid accidentally removing NuvaRing as well. If NuvaRing is expelled, it is enough to rinse the vaginal therapeutic system with cold or lukewarm water and reinsert it as soon as possible.
Damage to the vaginal therapeutic system has occurred during the use of vaginal products, such as moisturizers or treatments for infections (see section 3.4 "What to do if the NuvaRing vaginal therapeutic system is damaged"). The use of spermicides or vaginal antifungal medicines does not reduce the contraceptive effectiveness of NuvaRing.
Diagnostic tests
If laboratory tests of blood or urine are performed, one should inform the persons performing the tests about the use of NuvaRing, as the use of the vaginal therapeutic system may affect the results of some laboratory tests.
2.5 Pregnancy and breastfeeding
NuvaRing should not be used during pregnancy or if there is a suspicion that the woman is pregnant. If the patient becomes pregnant during the use of NuvaRing, the vaginal therapeutic system should be removed and a doctor should be consulted.
If the patient wants to stop using NuvaRing because they want to become pregnant, they should read the information in section 3.5 "What to do if the patient wants to stop using NuvaRing".
The use of NuvaRing is not recommended during breastfeeding. If the patient wants to use NuvaRing during breastfeeding, they should consult their doctor first.
2.6 Driving and using machines
NuvaRing does not affect the ability to drive or use machines.
3. How to use NuvaRing
NuvaRing can be inserted and removed by the patient themselves. The doctor will instruct when to start using NuvaRing. The vaginal therapeutic system should be inserted on the appropriate day of the cycle (see section 3.3 "When to insert the first NuvaRing vaginal therapeutic system") and left in place for 3 weeks in a row. One should regularly check if the NuvaRing vaginal therapeutic system is in the vagina (e.g., before and after intercourse) to ensure contraceptive protection. After 3 weeks, NuvaRing should be removed and a 1-week break should be taken. Usually, during this break, withdrawal bleeding occurs.
3.1 Inserting and removing NuvaRing
- 1. Before inserting the system, one should check the expiration date (see section 5 "How to store NuvaRing").
- 2. Before inserting or removing the system, one should wash their hands.
- 3. One should choose the most comfortable position for insertion, e.g., standing with one leg raised, squatting, or lying down.
- 4. One should remove NuvaRing from the pouch.
- 5. Holding the system between the thumb and index finger, one should squeeze it and insert it into the vagina (see Figures 1-4). Alternatively, the system can be inserted using the NuvaRing Applicator (not included in the NuvaRing packaging). The NuvaRing Applicator may not be available in all countries. The correct position of NuvaRing is one in which it is not felt. If the system is uncomfortable, one should gently adjust the position of the NuvaRing system (e.g., push it slightly further into the vagina) until they feel comfortable. The position of the system in the vagina does not affect its contraceptive effectiveness.
- 6. After 3 weeks, one should remove the system from the vagina. This can be done by hooking the index finger under the edge of the system or by grasping it with the index and middle fingers and pulling it out (Figure 5). If the patient is unable to locate the system in the vagina but cannot remove it, they should consult their doctor.
- 7. One should dispose of the used system with other household waste, preferably in a sealed pouch in which it was originally packaged. One should not flush NuvaRing down the toilet.

Figure 1
Remove the system from the pouch

Figure 2
Squeeze the system
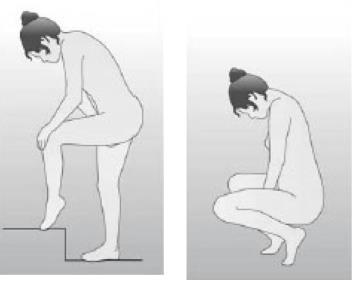
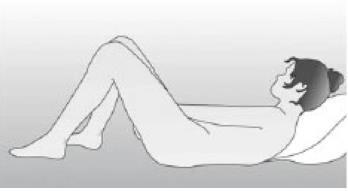
Figure 3
Choose the most comfortable position
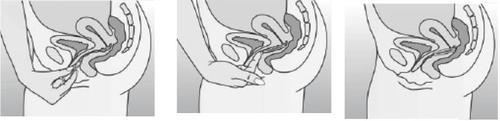
Figure 4A
Figure 4B
Figure 4C
Insert the system into the vagina with one hand (Figure 4A), if necessary, using the other hand to spread the labia. Place it inside the vagina so that it does not cause discomfort (Figure 4B). Leave the system in the vagina for 3 weeks (Figure 4C).

Figure 5
Remove the system from the vagina, hooking the index finger under the edge or grasping it with the index and middle fingers and pulling it out.
3.2 Three weeks of use, one week of break
Page 11 of 18
- 1. The system must be in the vagina for three weeks without interruption, counting from the day of insertion.
- 2. After three weeks, it should be removed on the same day of the week it was inserted, at approximately the same time. For example, if NuvaRing was inserted on a Wednesday at around 10:00 PM, it should be removed on the Wednesday three weeks later, at around 10:00 PM.
- 3. After removing the system, one should take a 1-week break. During this time, bleeding may occur. It usually starts 2-3 days after removal.
- 4. A new system should be inserted exactly one week after the break (on the same day of the week as usual and at approximately the same time), even if bleeding is still present. If the insertion of the new system is delayed by more than 3 hours, its contraceptive effectiveness may be reduced. In such a case, one should follow the instructions in section 3.4 "What to do if the patient forgets to insert a new NuvaRing vaginal therapeutic system after the break".
If NuvaRing is used according to the above instructions, subsequent bleedings will occur approximately every month on the same days of the week.
3.3 When to insert the first NuvaRing vaginal therapeutic system
- - If no hormonal contraceptive was used in the previous cycleInsert NuvaRing on the first day of the natural cycle (i.e., the first day of menstruation). NuvaRing is effective from the moment of insertion. There is no need to use any additional contraceptive methods. One can also start using NuvaRing between the 2nd and 5th day of menstruation, but in this case, during the first 7 days of using NuvaRing, an additional contraceptive method (such as a male condom) should be used. This recommendation applies only to the first use of NuvaRing.
- - If the patient used a combined hormonal contraceptive in the previous monthInsert NuvaRing no later than the day after stopping the current contraceptive. If the current contraceptive has tablets that do not contain active substances, one should start using NuvaRing no later than the day after taking the last tablet that does not contain active substances. If in doubt about which tablet this is, one should ask their doctor or pharmacist. One should not extend the break in using the current tablets beyond the recommended period. If the patient has been using their tablets regularly and is sure they are not pregnant, they can stop taking the tablets on any day and start using NuvaRing immediately.
- - If the patient used a transdermal system (patch) in the previous monthInsert NuvaRing no later than the day after stopping the transdermal system. One should not extend the break in using the transdermal system beyond the recommended period. If the patient has been using the transdermal system regularly and is sure they are not pregnant, they can stop using the transdermal system on any day and start using NuvaRing immediately.
- - If the patient used a minipill (progestin-only contraceptive) in the previous monthOne can stop taking the minipill on any day and start using NuvaRing the next day at the same time. During the first 7 days of using NuvaRing, an additional contraceptive method (such as a male condom) should be used.
Page 12 of 18
- - If the patient used injections or an implant, or an intrauterine system releasing progestin [IUD] in the previous monthInsert NuvaRing on the day of the next planned injection or on the day the implant or intrauterine system is removed. During the first 7 days of using NuvaRing, an additional contraceptive method (such as a male condom) should be used.
- - After giving birthAfter giving birth, the doctor may recommend using NuvaRing only after the first menstruation. Sometimes, one can start using NuvaRing earlier; the doctor will advise when. If the patient is breastfeeding and wants to use NuvaRing, they should discuss this with their doctor first.
- - After a miscarriageAccording to the doctor's instructions.
3.4 What to do if…
What to do if the NuvaRing vaginal therapeutic system is accidentally expelled from the vagina
NuvaRing may be accidentally expelled from the vagina, e.g., if it is not inserted correctly, during tampon removal, during intercourse, due to constipation, or uterine prolapse. Therefore, one should regularly check if the system is in the vagina (e.g., before and after intercourse).
Note: The translation provided is a complete translation of the original text, maintaining all HTML structure, tags, and formatting exactly as provided, translating only the text content within HTML tags, preserving all HTML attributes, classes, IDs, and structural elements, and preserving all medical terminology accuracy in English.3.5 Procedure when a patient wants to stop using NuvaRing
NuvaRing can be stopped at any time.
If the patient does not want to become pregnant, she should ask her doctor about other contraceptive methods.
If the patient stops using NuvaRing because she wants to become pregnant, she should wait until the first menstruation and then start trying to conceive. This will help determine the date of birth.
4. Possible side effects
Like all medicines, NuvaRing can cause side effects, although not everybody gets them. If any side effects occur, especially serious and persistent ones or changes in health that the patient considers related to the use of NuvaRing, the patient should consult a doctor.
All women using combined hormonal contraceptives have an increased risk of developing blood clots in the veins (venous thromboembolism) or blood clots in the arteries (arterial thrombosis). To obtain detailed information about the various risk factors associated with the use of combined hormonal contraceptives, the patient should refer to section 2 "Important information before using NuvaRing".
Page 15 of 18
If an allergic reaction (hypersensitivity) to any of the components of NuvaRing occurs, it may manifest as (frequency not known): angioedema and/or anaphylactic reaction [swelling of the face, lips, tongue, and/or throat and/or difficulty swallowing] or the occurrence of hives potentially with difficulty breathing. In these cases, NuvaRing should be removed and a doctor consulted immediately (see also section 2.2 "Warnings and precautions").
Women using NuvaRing have reported the following side effects:
Common:may occur in up to 1 in 10 women
- abdominal pain, nausea
- vaginal infections caused by fungi (such as "thrush"); discomfort caused by the presence of the system in the vagina; genital itching; discharge
- headache or migraine; depressive mood; decreased libido
- breast pain; pelvic pain; painful menstruation
- acne
- weight gain
- expulsion of the system.
Uncommon:may occur in up to 1 in 100 women
- vision disturbances; dizziness
- bloating; vomiting, diarrhea, or constipation
- fatigue, malaise, or restlessness; mood changes; sudden mood swings
- edema
- urinary tract infections
- problems or pain during urination; urgency or need to urinate; frequent urination
- discomfort during intercourse, including pain, bleeding, inconvenience related to the presence of the system, felt by the partner
- increased blood pressure
- increased appetite
- back pain; muscle cramps; pain in the lower or upper limbs
- decreased skin sensitivity
- breast tenderness or enlargement; fibrocystic breast disease (cysts that can cause swelling or pain in the breasts)
- cervicitis; cervical polyps; cervical ectropion
- changes in menstrual bleeding (e.g., heavy, prolonged, irregular, or complete absence of menstruation); pelvic discomfort; premenstrual syndrome; uterine cramps
- vaginal infections (fungal or bacterial); feeling of burning, unpleasant odor, pain, discomfort, or dryness of the vagina or vulva
- hair loss, rash, itching, or hives.
Rare:may occur in up to 1 in 1000 women
- harmful blood clots in a vein or artery, for example: in the leg or foot (e.g., deep vein thrombosis) in the lungs (e.g., pulmonary embolism) heart attack stroke transient ischaemic attack or temporary stroke-like symptoms, known as a transient ischaemic attack blood clots in the liver, stomach, and intestine, kidneys, or eye. The likelihood of developing blood clots may be higher if the patient has other risk factors (see section 2 for further information on risk factors for blood clots and symptoms of blood clots).
Page 16 of 18
information on risk factors for blood clots and symptoms of blood clots).
- galactorrhea.
Unknown(frequency cannot be estimated from the available data)
- chloasma (brownish-yellow spots on the skin, especially on the face)
- partner's genital discomfort (such as irritation, rash, itching)
- inability to remove the therapeutic vaginal system without medical assistance (e.g., due to the therapeutic vaginal system adhering to the vaginal wall)
- vaginal wall damage associated with damage to the therapeutic vaginal system.
Women using combined hormonal contraceptives have reported breast cancer and liver tumors. For detailed information, see section 2.2 "Warnings and precautions", "Tumors".
Very rarely, NuvaRing may be damaged. For additional information, see section 3.4 "Procedure in case of damage to the therapeutic vaginal system".
Reporting side effects
If any side effects occur, including any side effects not listed in the leaflet, the patient should tell her doctor, pharmacist, or nurse.
Side effects can be reported directly to the Department of Drug Safety Monitoring of the Office for Registration of Medicinal Products, Medical Devices, and Biocidal Products, Al. Jerozolimskie 181C, PL-02 222 Warsaw, tel.: +48 22 49-21-301, fax: +48 22 49-21-309, website: https://smz.ezdrowie.gov.pl
Reporting side effects will help gather more information on the safety of the use of NuvaRing.
5. How to store NuvaRing
The medicine should be stored out of sight and reach of children.
A doctor should be consulted if a child is exposed to the hormones contained in NuvaRing.
Store at a temperature below 30°C. Store in the original packaging to protect from light and moisture.
NuvaRing should not be used after 4 months from the date of issue of the medicine in the pharmacy. The date of issue is stated on the box and on the sachet.
NuvaRing should not be used after the expiry date stated on the packaging. The expiry date refers to the last day of the given month.
NuvaRing should not be used if it has changed color or if any signs of deterioration are visible.
The used therapeutic vaginal system should be disposed of in a regular household waste bin, preferably in a sealed sachet. NuvaRing should not be flushed down the toilet. Like other medicines, unused or expired systems should not be disposed of in the sewage system or household waste bins. The patient should ask her pharmacist how to dispose of medicines that are no longer needed. This will help protect the environment.
Page 17 of 18
6. Contents of the packaging and other information
What NuvaRing contains
- The active substances of NuvaRing are: etonogestrel (11.7 mg) and ethinyl estradiol (2.7 mg).
- The other ingredients are: poly(ethylene-vinyl acetate), 28% vinyl acetate, poly(ethylene-vinyl acetate), 9% vinyl acetate (a type of plastic that does not dissolve in the body), and magnesium stearate.
Etonogestrel and ethinyl estradiol are released from the therapeutic vaginal system in amounts of 0.120 mg/day and 0.015 mg/day, respectively, over a period of 3 weeks.
What NuvaRing looks like and what the packaging contains
NuvaRing is a flexible, transparent, colorless or almost colorless ring with an outer diameter of 54 mm.
Each therapeutic vaginal system is packaged in a separate foil sachet. The sachet can be reopened after opening. The sachets are placed in a cardboard box with a leaflet and stickers to help remember when to insert and remove NuvaRing.
The packaging contains 1 or 3 systems.
Other information
For more detailed information, the patient should contact the marketing authorization holder or the parallel importer.
Marketing authorization holder in Greece, the country of export:
N.V. Organon, Kloosterstraat 6, 5349 AB Oss, Netherlands
Manufacturer:
N.V. Organon, Kloosterstraat 6, 5349 AB Oss, Netherlands
Parallel importer:
Delfarma Sp. z o.o., ul. Św. Teresy od Dzieciątka Jezus 111, 91-222 Łódź
Repackaged by:
Delfarma Sp. z o.o., ul. Św. Teresy od Dzieciątka Jezus 111, 91-222 Łódź
Marketing authorization number in Greece, the country of export: 57201/1-9-2015
Parallel import authorization number: 69/23
This medicinal product is authorized in the Member States of the European Economic Area and in the United Kingdom (Northern Ireland) under the following names:
NuvaRing
0.120 mg/ 0.015 mg/ 24 h, therapeutic vaginal system
Austria, Belgium, Czech Republic, Denmark, Estonia, Finland, France, Germany, Greece, Hungary, Iceland, Ireland, Italy, Latvia, Lithuania, Luxembourg, Malta, Netherlands, Norway, Romania, Poland, Portugal, Slovakia, Slovenia, Spain, Sweden, United Kingdom (Northern Ireland).
Date of approval of the leaflet: 05.04.2023
[Information about the trademark]
Page 18 of 18
- Country of registration
- Active substance
- Prescription requiredYes
- Marketing authorisation holder (MAH)N.V. Organon
- This information is for reference only and does not constitute medical advice. Always consult a licensed doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to NuvaringDosage form: System, (0.12 mg + 0.015 mg)/24 hActive substance: vaginal ring with progestogen and estrogenPrescription requiredDosage form: System, (0.120 mg + 0.015 mg)/24 hActive substance: vaginal ring with progestogen and estrogenManufacturer: N.V. OrganonPrescription requiredDosage form: System, (0.12 mg + 0.015 mg)/24 hActive substance: vaginal ring with progestogen and estrogenPrescription required
Alternatives to Nuvaring in other countries
The best alternatives with the same active ingredient and therapeutic effect.
Alternative to Nuvaring in Ukraine
Alternative to Nuvaring in Spain
Online doctors for Nuvaring
Discuss dosage, side effects, interactions, contraindications, and prescription renewal for Nuvaring – subject to medical assessment and local rules.







