How to use Circlet
Leaflet accompanying the packaging: information for the user
Circlet, (0.120 mg + 0.015 mg)/24 h, Therapeutic intrauterine system
Etonogestrel + Ethinylestradiol
Important information about combined hormonal contraceptives
- If used correctly, they are one of the most reliable, reversible methods of contraception.
- To a small extent, they increase the risk of blood clots in veins and arteries, especially in the first year of use or after resuming use after a break of 4 weeks or more.
- Caution should be exercised and a doctor should be consulted if the patient suspects that symptoms of blood clots have occurred (see section 2 "Blood clots").
You should carefully read the contents of the leaflet before using the medicine, as it contains important information for the patient.
You should keep this leaflet so that you can read it again if you need to.
In case of any doubts, you should consult a doctor or pharmacist.
This medicine has been prescribed to a specific person. It should not be given to others. The medicine may harm another person.
If the patient experiences any side effects, including any side effects not listed in this leaflet, they should tell their doctor or pharmacist. See section 4.
Table of contents of the leaflet
- 1. What is Circlet and what is it used for
- 2. Important information before using Circlet
- 3. How to use Circlet
- 4. Possible side effects
- 5. How to store Circlet
- 6. Contents of the packaging and other information
1. What is Circlet and what is it used for
Circlet is a contraceptive in the form of an intrauterine therapeutic system, preventing pregnancy. Each intrauterine therapeutic system contains a small amount of two female sex hormones - etonogestrel and ethinylestradiol. These hormones are slowly released from the system into the bloodstream. Due to the small dose of hormones released, Circlet is classified as a low-hormone contraceptive. Since Circlet releases two different hormones, it is also a combined contraceptive.
2. Important information before using Circlet
General notes
Before starting to use Circlet, you should read the information about blood clots (thrombosis) in section 2. It is especially important to read about the symptoms of blood clots (see section 2 "Blood clots").
This leaflet describes situations in which you should stop using Circlet or in which its effectiveness may be reduced. In these situations, you should refrain from sexual intercourse or use an additional non-hormonal contraceptive method, such as a male condom or another mechanical method. You should notuse methods based on a calendar or body temperature measurement. They may be ineffective because Circlet affects changes in body temperature and cervical mucus consistency throughout the month.
Circlet, like other hormonal contraceptives, does not protect against HIV infection (AIDS) or other sexually transmitted diseases.
2.1 When not to use Circlet
You should not use Circlet if you have any of the following conditions.
If you have any of the following conditions, you must inform your doctor. The doctor will discuss with you which other contraceptive method will be more suitable.
if you currently have (or have ever had) a blood clot in the veins of the legs (deep vein thrombosis), in the lungs (pulmonary embolism), or in other organs,
if you know you have blood coagulation disorders - such as protein C deficiency, protein S deficiency, antithrombin III deficiency, factor V Leiden, or antiphospholipid antibodies,
if you need to have surgery or will be immobilized for a long time (see section "Blood clots"),
if you have had a heart attack or stroke,
if you have (or have had) angina pectoris (a disease that causes severe chest pain, which can be the first symptom of a heart attack) or a transient ischemic attack (transient stroke symptoms);
- severe diabetes with vascular damage
- very high blood pressure
- very high levels of fats in the blood (cholesterol or triglycerides)
- a disease called hyperhomocysteinemia
- if you have (or have had) a type of migraine called "migraine with aura",
- if you have (or have had) pancreatitis associated with high levels of fats in the blood,
- if you have (or have had) severe liver disease, and liver function has not returned to normal,
- if you have (or have had) a benign or malignant liver tumor,
- if you have (or have had) breast cancer or genital cancer, or if such cancers are suspected,
- if you have unexplained vaginal bleeding,
- if you are allergic to ethinylestradiol or etonogestrel, or any of the other ingredients of this medicine (listed in section 6).
If any of the above symptoms occur for the first time during the use of Circlet, you should immediately remove the system from the vagina and consult a doctor, and in the meantime, use a non-hormonal contraceptive method.
If you have a hepatitis C virus infection and are taking medicines containing ombitasvir, paritaprevir, ritonavir, and dasabuvir or glecaprevir, pibrentasvir, you should not use the Circlet intrauterine system (see also section 2.4 "Circlet and other medicines").
2.2 Warnings and precautions
When should you contact a doctor?
You should immediately consult a doctor
- -if you notice probable symptoms of blood clots, which may indicate that you have blood clots in the leg (deep vein thrombosis), blood clots in the lungs (pulmonary embolism), a heart attack, or a stroke (see below "Blood clots (thrombosis)"). To get a description of these serious side effects, see "How to recognize the occurrence of blood clots".
You should tell your doctor if you have any of the following conditions.
If these symptoms appear or worsen during the use of Circlet, you should also tell your doctor.
- if breast cancer is present or has occurred in close relatives;
- if you have epilepsy (see section 2.4 "Circlet and other medicines");
- if you have liver disease (e.g., jaundice) or gallbladder disease (e.g., gallstones);
- if you have Crohn's disease or ulcerative colitis (chronic inflammatory bowel diseases);
- if you have systemic lupus erythematosus (a disease that affects the body's natural defense system);
- if you have hemolytic uremic syndrome (a blood clotting disorder that causes kidney failure);
- if you have sickle cell anemia (a hereditary disease of red blood cells);
- if you have been diagnosed with high levels of fats in the blood (hypertriglyceridemia) or a positive family history for this disease. Hypertriglyceridemia is associated with an increased risk of developing pancreatitis;
- if you need to have surgery or will be immobilized for a long time (see section 2 "Blood clots");
- if you have recently given birth, as you are then in a group with an increased risk of blood clots. You should consult a doctor to find out how soon you can start using Circlet after giving birth;
- if you have superficial thrombophlebitis (blood clots in the veins under the skin);
- if you have varicose veins;
- if you have diseases that occurred for the first time or worsened during pregnancy or previous use of sex hormones (e.g., hearing loss, porphyria [a blood disease], pregnancy herpes [a blistering skin rash during pregnancy], or Sydenham's chorea [a nervous system disease in which there are involuntary, sudden movements of the body]);
- in case of symptoms of angioedema, such as swelling of the face, tongue, and (or) throat, and (or) difficulty swallowing or the occurrence of hives, potentially with impaired breathing, you should immediately consult a doctor. Estrogen-containing medicines may cause or worsen symptoms of hereditary and acquired angioedema;
- if you have chloasma (brownish-yellow spots, so-called "pregnancy spots", especially on the face) now or in the past. If they occur, you should avoid excessive sun exposure and ultraviolet radiation;
- if you have conditions that make it difficult to use Circlet, such as frequent constipation, cervical prolapse, or pain during intercourse;
- if you experience sudden, frequent need to urinate with a burning sensation and (or) pain, and if you cannot locate the intrauterine system in the vagina. These symptoms may indicate that the intrauterine system has been accidentally inserted into the bladder.
BLOOD CLOTS
The use of combined hormonal contraceptives, such as the Circlet intrauterine system, is associated with an increased risk of blood clots, compared to when no therapy is used. In rare cases, a blood clot can block a blood vessel and cause serious complications.
Blood clots can occur
- in veins (hereinafter referred to as "venous thromboembolism" or "venous thromboembolic disease")
- in arteries (hereinafter referred to as "arterial thromboembolism" or "arterial thromboembolic disease").
Not all patients recover fully after a blood clot. In rare cases, the effects of a blood clot can be permanent or, very rarely, fatal.
Remember that the total risk of harmful blood clots caused by Circlet is small.
HOW TO RECOGNIZE THE OCCURRENCE OF BLOOD CLOTS
You should immediately consult a doctor if you notice any of the following symptoms.
Are you experiencing any of these symptoms?
Why is the patient likely to suffer
- swelling of the leg or swelling along a vein in the leg or foot, especially if it is accompanied by:
- pain or tenderness in the leg, which may only be felt while standing or walking,
- increased temperature in the affected leg,
- change in skin color of the leg, such as pallor, redness, or cyanosis. Deep vein thrombosis
- sudden unexplained shortness of breath or rapid breathing;
- sudden unexplained cough, which may be accompanied by coughing up blood;
- sharp chest pain, which may worsen with deep breathing;
- severe dizziness or fainting;
- rapid or irregular heartbeat;
- severe abdominal pain;
If you are unsure, you should consult a doctor,
Pulmonary embolism
| because some of these symptoms, such as cough or shortness of breath, may be mistaken for milder conditions, such as a respiratory infection (e.g., a cold). | |
Symptoms usually occur in one eye:
| Retinal vein thrombosis (blood clot in the eye) |
| Heart attack |
| Stroke |
| Blood clots blocking other blood vessels |
BLOOD CLOTS IN VEINS
What can happen if blood clots form in a vein?
- The use of combined hormonal contraceptives is associated with an increased risk of blood clots in the veins (venous thromboembolism). Although these side effects are rare, they can occur. Most often, they occur in the first year of using combined hormonal contraceptives.
- If blood clots form in the veins in the leg or foot, it can lead to the development of deep vein thrombosis.
- If a blood clot moves from the leg and settles in the lungs, it can cause pulmonary embolism.
- In very rare cases, a blood clot can form in another organ, such as the eye (retinal vein thrombosis).
When is the risk of blood clots in a vein the highest?
The risk of forming blood clots in a vein is highest during the first year of using combined hormonal contraceptives for the first time. The risk may also be higher when resuming the use of combined hormonal contraceptives (the same or a different medicine) after a break of 4 weeks or more.
After the first year, the risk decreases, but it is always higher compared to when combined hormonal contraceptives are not used.
If you stop using Circlet, the risk of blood clots returns to normal within a few weeks.
What affects the risk of blood clots?
The risk of blood clots associated with the use of the Circlet intrauterine system is small, but some factors can increase this risk. The risk is higher:
- if you are significantly overweight (body mass index (BMI) over 30 kg/m);
- if someone in your immediate family has had blood clots in the legs, lungs, or other organs at a young age (e.g., under 50 years old). In this case, you may have hereditary blood coagulation disorders;
- if you need to have surgery or will be immobilized for a long time due to injury or illness, or have a leg in a cast. It may be necessary to stop using Circlet for a few weeks before surgery or immobilization. If you need to stop using Circlet, you should ask your doctor when you can resume using it;
- with age (especially over 35 years old);
- if you have recently given birth.
The risk of blood clots increases with the number of risk factors present in the patient.
Long-distance air travel (>4 hours) may temporarily increase the risk of blood clots, especially if you have another risk factor.
It is essential to tell your doctor if any of these factors apply to you, even if you are not sure. Your doctor may decide to stop using Circlet.
You should inform your doctor if any of the above conditions change during the use of Circlet, e.g., if someone in your immediate family is diagnosed with thrombosis without a known cause or if you gain significant weight.
BLOOD CLOTS IN ARTERIES
What can happen if blood clots form in an artery?
Similarly to blood clots in veins, blood clots in arteries can have serious consequences, such as a heart attack or stroke.
Factors that increase the risk of blood clots in arteries
It is essential to note that the risk of a heart attack or stroke associated with the use of the Circlet intrauterine system is very small, but it may increase:
- with age (over approximately 35 years old);
- if you smoke.While using a hormonal contraceptive like the Circlet intrauterine system, it is recommended to quit smoking. If you are unable to quit smoking and are over 35 years old, your doctor may recommend using a different type of contraception;
- if you are overweight;
- if you have high blood pressure;
- if someone in your immediate family has had a heart attack or stroke at a young age (under 50 years old). In this case, you may also be at increased risk of having a heart attack or stroke;
- if you or someone in your immediate family has been diagnosed with high levels of fats in the blood (cholesterol or triglycerides);
- if you have migraines, especially migraines with aura;
- if you have heart disease (valve damage, arrhythmia called atrial fibrillation);
- if you have diabetes.
If you have more than one of the above conditions or if any of them are particularly severe, the risk of blood clots may be even higher.
You should inform your doctor if any of the above conditions change during the use of the Circlet intrauterine system, e.g., if you start smoking, if someone in your immediate family is diagnosed with thrombosis without a known cause, or if you gain significant weight.
Cancer
The following information was obtained from studies using combined oral contraceptives and may also apply to Circlet. Information on the vaginal use of hormonal contraceptives (as in the case of Circlet) is not available.
Among women using combined contraceptives, a slightly more frequent occurrence of breast cancer has been found, although it is not known whether this is caused by the medicines used. It is possible that women using combined contraceptives are more likely to have breast cancer detected, as they undergo medical examinations more frequently. The increased frequency of breast cancer decreases gradually after stopping the use of combined contraceptives.
Regular breast examination is very important. If a lump is detected, you should consult a doctor. You should also inform your doctor if breast cancer has occurred or occurs in close relatives (see section 2.2 "Warnings and precautions").
In rare cases, women using combined contraceptives have been found to have benign liver tumors, and very rarely, malignant liver tumors. If you experience unusual, severe abdominal pain, you should consult your doctor.
There are reports that women using combined contraceptives less frequently develop endometrial cancer (cancer of the uterine lining) and ovarian cancer. It is possible that this also applies to Circlet, but it has not been confirmed yet.
Mental disorders
Some women using hormonal contraceptives, including Circlet, have reported depression or low mood. Depression can be severe and sometimes lead to suicidal thoughts.
If mood changes and symptoms of depression occur, you should consult your doctor as soon as possible for further medical advice.
2.3 Children and adolescents
The safety and efficacy of Circlet have not been studied in adolescents under the age of 18.
2.4 Circlet and other medicines
You should always inform your doctor about the medicines or herbal products you are currently using. You should also inform your doctor of another specialty or a prescribing dentist (or pharmacist) about the use of Circlet. They may inform you about the need to use an additional contraceptive method (e.g., male condoms), and if so, for how long, and whether it is necessary to modify the use of another medicine.
Some medicines
- may affect the level of Circlet in the blood;
- may reduce its contraceptive effectiveness;
- may cause unexpected bleeding.
This applies to medicines used to treat:
- epilepsy (e.g., primidone, phenytoin, barbiturates, carbamazepine, oxcarbazepine, topiramate, felbamate);
- tuberculosis (e.g., rifampicin);
- HIV infection (e.g., ritonavir, nelfinavir, nevirapine, efavirenz);
- hepatitis C virus infection (e.g., boceprevir, telaprevir);
- other infectious diseases (e.g., griseofulvin);
- high blood pressure in the blood vessels of the lungs (bosentan);
- depressive moods (St. John's wort).
If you are taking medicines or herbal products that may reduce the effectiveness of Circlet, you should also use a mechanical contraceptive method (such as a male condom). Due to the fact that the effect of another medicine on Circlet may persist for up to 28 days after stopping the medicine, it is necessary to use additional mechanical contraception during this time. Note: Circlet should not be used with a diaphragm, cervical cap, or female condom. The use of spermicides or vaginal antifungal medicines does not reduce the contraceptive effectiveness of Circlet.
Circlet may affect the action of other medicines, such as
- cyclosporine-containing medicines
- the antiepileptic medicine lamotrigine (which may lead to an increased frequency of seizures).
If you have a hepatitis C virus infection and are taking medicines containing ombitasvir, paritaprevir, ritonavir, and dasabuvir or glecaprevir, pibrentasvir, you should not use the Circlet intrauterine system, as this may cause an increase in liver function test results in blood tests (an increase in the activity of the liver enzyme ALT).
Before starting these medicines, your doctor will prescribe a different type of contraceptive.
You can resume using the Circlet intrauterine system about 2 weeks after finishing this treatment. See section 2.1 "When not to use Circlet".
Before taking any medicine, you should consult your doctor or pharmacist.
During the use of Circlet, you can also use tampons. You should insert Circlet before inserting a tampon. You should be careful when removing a tampon to avoid accidentally removing Circlet as well. If Circlet is expelled, it is enough to wash the intrauterine system with cold or warm water and reinsert it as soon as possible.
Damage to the intrauterine system has occurred during the use of vaginal products, such as moisturizers or treatments for infections (see section 3.4 "Procedure in case of damage to the intrauterine system").
Diagnostic tests
If you are undergoing blood or urine tests, you should inform the persons performing the tests about the use of Circlet, as the use of the intrauterine system may affect the results of some laboratory tests.
2.5 Pregnancy and breastfeeding
Circlet should not be used during pregnancy or if there is a suspicion that the woman is pregnant. If you become pregnant while using Circlet, you should remove the intrauterine system and consult a doctor.
If you want to stop using Circlet because you want to become pregnant, you should read the contents of section 3.5 "Procedure when the patient wants to stop using Circlet".
The use of Circlet is not recommended during breastfeeding. If you want to use Circlet during breastfeeding, you should first consult your doctor.
2.6 Driving and operating machinery
Circlet does not affect the ability to drive or operate machinery.
3. How to use Circlet
Circlet can be inserted and removed by yourself. Your doctor will instruct you on when to start using Circlet. The intrauterine system should be inserted on the appropriate day of the cycle (see section 3.3 "When to insert the first Circlet intrauterine system") and left in place for 3 weeks in a row. You should regularly check that the Circlet intrauterine system is in the vagina (e.g., before and after sexual intercourse) to ensure contraceptive protection.
After 3 weeks, you should remove Circlet and take a 1-week break. Usually, during this break, withdrawal bleeding occurs.
You should not use certain mechanical contraceptive methods for women, such as a diaphragm, cervical cap, or female condom, while using Circlet. You should not use these mechanical contraceptive methods as an additional method of contraception, as Circlet may interfere with the proper insertion and placement of the diaphragm, cervical cap, or female condom. However, you can use a male condom as an additional mechanical contraceptive method.
3.1 Inserting and removing Circlet
- 1. Before inserting the system, check its expiration date (see section 5 "How to store Circlet").
- 2. Before inserting or removing the system, wash your hands.
- 3. Choose the most comfortable position for insertion, such as standing with one leg raised, squatting, or lying down.
- 4. Remove Circlet from the sachet.
- 5. Holding the system with your thumb and index finger, squeeze it and insert it into the vagina (see Figures 1-4). Alternatively, the system can be inserted using the NuvaRing Applicator (not included with the Circlet packaging). The NuvaRing Applicator may not be available in all countries. The correct position of the Circlet system is one in which you do not feel it. If the system is uncomfortable, you should gently change its position (e.g., push the system slightly further into the vagina) until you feel comfortable. The position of the system in the vagina does not affect its contraceptive effectiveness.
- 6. After 3 weeks, remove the system from the vagina. You can do this by hooking your index finger under the edge of the system or by grasping it with your index and middle fingers and pulling it out (Figure 5). If you are unable to locate the system in the vagina but cannot remove it, you should consult your doctor.
- 7. Dispose of the used system with other household waste, preferably in a sealed sachet, in which it was originally packaged. Do not flush Circlet down the toilet.
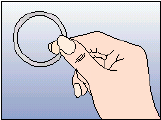
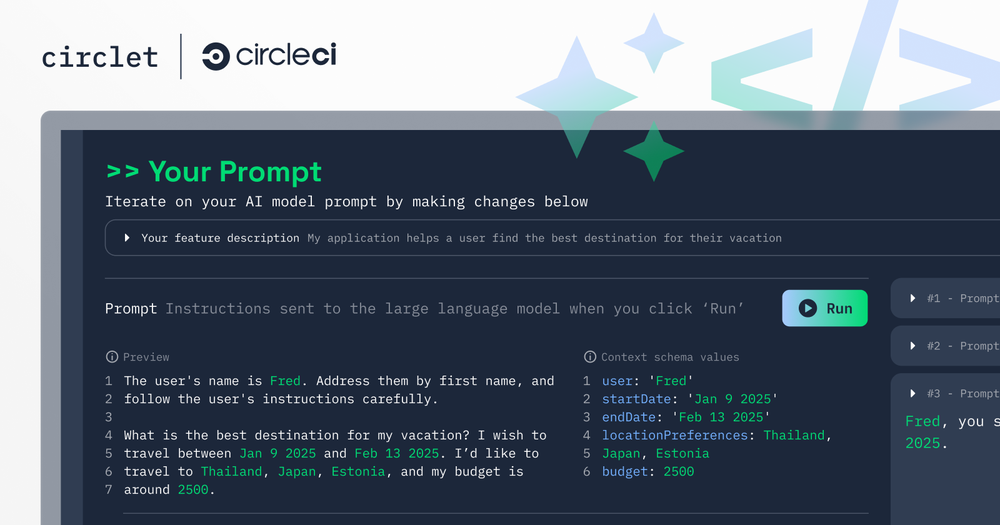
Figure 1
Remove the system from the sachet
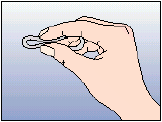
Figure 2
Squeeze the system
Figure 3
Choose the most comfortable position
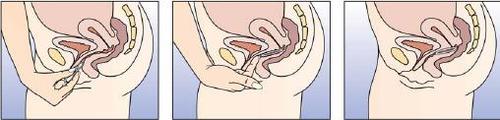
Figure 4A Figure 4B Figure 4C
Insert the system into the vagina with one hand (Figure 4A), if necessary, using the other hand to spread the labia. Place it inside the vagina so that it does not cause discomfort (Figure 4B). Leave the system in the vagina for 3 weeks (Figure 4C).

Figure 5
Remove the system from the vagina, hooking your index finger under the edge of the system or grasping it with your index and middle fingers and pulling it out.
3.2 Three weeks of use, one week of break
- 1. The system must be in the vagina for three weeks without interruption, counting from the day of insertion.
- 2. After three weeks, you should remove it on the same day of the week that it was inserted, and at approximately the same time. For example, if Circlet was inserted on a Wednesday at around 10:00 PM, it should be removed on the same Wednesday, three weeks later, at around 10:00 PM.
- 3. After removing the system, you should take a 1-week break. During this time, you may experience bleeding.
- 4. A new system should be inserted exactly one week after the break (on the same day of the week as usual, and at approximately the same time), even if bleeding is still present. If the insertion of the new system is delayed by more than 3 hours, its contraceptive effectiveness may be reduced. In such a case, you should follow the instructions in section 3.4 "Procedure if the patient forgets to insert a new intrauterine system after a 1-week break".
If you use Circlet according to the above instructions, subsequent bleeding will occur approximately every month on the same days of the week.
3.3 When to insert the first Circlet intrauterine system
- If you did not usea hormonal contraceptivein the previous cycle
Insert Circlet on the first day of your natural cycle (i.e., the first day of your period). Circlet is effective from the moment of insertion. There is no need to use any additional contraceptive methods.
You can also start using Circlet between the 2nd and 5th day of your period, but in this case, you should use an additional contraceptive method (such as a male condom) during the first 7 days of using Circlet. This recommendation applies only to the first use of Circlet.
- If you usedcombined hormonal oral contraceptivesin the previous month
You should start using Circlet no later than the day after stopping the current medicine. If the current medicine also contains inactive tablets, you should start using Circlet no later than the day after taking the last inactive tablet. If you are unsure which tablet is which, you should ask your doctor or pharmacist. Do not extend the break in using the current tablets beyond the recommended period.
If you have been taking your tablets regularly and are sure you are not pregnant, you can stop taking the tablets on any day and start using Circlet immediately.
- If you useda contraceptive transdermal system(patch)in the previous month
You should start using Circlet no later than the day after stopping the transdermal system. Do not extend the break in using the transdermal system beyond the recommended period. If you have been using the transdermal system regularly and are sure you are not pregnant, you can stop using the transdermal system on any day and start using Circlet immediately.
- If you useda minipill(progestogen-only contraception)in the previous month
You can stop using the minipill on any day and start using Circlet the next day at the same time you would have taken the minipill. During the first 7 days of using Circlet, you should also use an additional contraceptive method (such as a male condom).
- If you usedinjections or an implant, or a progestogen-releasing intrauterine system (IUD)in the previous month
You should start using Circlet on the day of the next planned injection or on the day the implant or progestogen-releasing intrauterine system is removed. During the first 7 days of using Circlet, you should use an additional contraceptive method (such as a male condom).
- After childbirth
After giving birth, your doctor may recommend using Circlet only after your first menstrual period. Sometimes, you can start using Circlet earlier; your doctor will advise you when. If you are breastfeeding and want to use Circlet, you should discuss this with your doctor first.
- After a miscarriage
Follow your doctor's instructions.
3.4 What to do if…
Procedure in case of accidental expulsion of the system from the vagina
Circlet may be accidentally expelled from the vagina, e.g., if it was not inserted correctly, during tampon removal, during intercourse, due to constipation, or due to cervical prolapse. Therefore, you should regularly check that the system is in the vagina (e.g., before and after sexual intercourse).
3.5 Procedure when the patient wants to stop using Circlet
Circlet can be stopped at any time.
If the patient does not want to become pregnant, she should ask her doctor about other contraceptive methods.
If the patient stops using Circlet because she wants to become pregnant, she should wait until the first menstruation and only then start trying to become pregnant. This will help determine the date of birth.
4. Possible side effects
Like all medicines, Circlet can cause side effects, although not everybody gets them. If side effects occur, especially severe and persistent ones or changes in health status that the patient considers related to the use of Circlet, the patient should consult a doctor.
All women using combined hormonal contraceptives have an increased risk of developing blood clots in veins (venous thromboembolism) or blood clots in arteries (arterial thrombosis). To obtain detailed information on the various risk factors associated with the use of combined hormonal contraceptives, the patient should refer to section 2 "Important information before using Circlet".
If there is an allergy (hypersensitivity) to any of the components of Circlet, it may manifest as (frequency not known): angioedema and/or anaphylactic reaction [swelling of the face, lips, tongue, and/or throat and/or difficulty swallowing] or the occurrence of urticaria potentially with difficulty breathing. In these cases, Circlet should be removed and the patient should contact a doctor immediately (see also section 2.2 "Warnings and precautions").
Women using Circlet have reported the following side effects:
- Frequent: may occur in no more than 1 in 10 women
- abdominal pain, nausea
- vaginal infections by fungi (such as "thrush"); discomfort caused by the presence of the system in the vagina; genital itching; discharge
- headache or migraine; depressive mood; decreased libido
- breast pain; pelvic pain; painful menstruation
- acne
- weight gain
- expulsion of the system
Infrequent: may occur in no more than 1 in 100 women
- vision disorders; dizziness
- bloating; vomiting; diarrhea or constipation
- feeling of fatigue, malaise or irritability; mood changes; sudden mood changes
- edema
- urinary tract infections
- problems or pain during urination; urgency to urinate or need to urinate frequently
- discomfort during intercourse, including pain, bleeding, inconvenience related to the presence of the system felt by the partner
- increased blood pressure
- increased appetite
- back pain; muscle cramps; pain in the lower or upper limbs
- decreased skin sensitivity
- breast tenderness or enlargement; fibrocystic breast disease (cysts that can cause swelling or pain in the breast)
- cervicitis; cervical polyps; eversion of the external cervical os
- changes in menstrual bleeding (e.g., heavy, prolonged, irregular, or complete lack of menstruation); pelvic discomfort; premenstrual syndrome; uterine cramps
- vaginal infections (fungal or bacterial); feeling of burning, unpleasant odor, pain, discomfort, or dryness of the vagina or vulva
- hair loss, rash, itching, or hives
- urticaria
Rare: may occur in no more than 1 in 1000 women
- harmful blood clots in a vein or artery, for example: in the leg or foot (e.g., deep vein thrombosis) in the lungs (e.g., pulmonary embolism) heart attack stroke mini-stroke or transient stroke-like symptoms, known as a transient ischemic attack blood clots in the liver, stomach, and intestine, kidneys, or eye. The probability of developing blood clots may be higher if the patient has other risk factors (see section 2 for further information on risk factors for blood clots and symptoms of blood clots).
- galactorrhea
Unknown (frequency cannot be determined from available data)
- chloasma (brownish-yellow spots on the skin, especially on the face)
- partner's genital discomfort (such as irritation, rash, itching)
- inability to remove the therapeutic vaginal system without medical assistance (e.g., due to the therapeutic vaginal system adhering to the vaginal wall)
- vaginal wall damage related to damage to the therapeutic vaginal system
Women using combined hormonal contraceptives have reported breast cancer and liver tumors. For detailed information, see section 2.2 "Warnings and precautions", "Tumors".
Very rarely, Circlet may be damaged. For additional information, see section 3.4 "Procedure in case of damage to the therapeutic vaginal system".
Reporting side effects
If any side effects occur, including any side effects not listed in the leaflet, the patient should tell her doctor or pharmacist.
Side effects can be reported directly to the Department of Adverse Reaction Monitoring of Medicinal Products, Medical Devices, and Biocidal Products:
Jerozolimskie Avenue 181C, 02-222 Warsaw, Tel.: +48 22 49 21 301, Fax: +48 22 49 21 309, Website: https://smz.ezdrowie.gov.pl .
Side effects can also be reported to the marketing authorization holder.
Reporting side effects will help gather more information on the safety of the medication.
5. How to store Circlet
The medication should be stored out of sight and reach of children.
A doctor should be consulted in case of exposure of a child to the hormones contained in Circlet.
Store at a temperature below 30°C. Store in the original packaging to protect from light and moisture.
Do not use Circlet after 4 months from the date of dispensing. The date of dispensing is indicated on the box and on the sachet.
Do not use Circlet after the expiration date indicated on the box and on the sachet.
Do not use Circlet if it has changed color or if there are any signs of deterioration.
The used therapeutic vaginal system should be disposed of in a regular household waste bin, preferably in a sealed sachet. Circlet should not be flushed down the toilet. Like other medications, unused or expired systems should not be disposed of in the sewage system or household waste bins. The patient should ask her pharmacist how to dispose of medications that are no longer needed. This will help protect the environment.
6. Package contents and other information
What Circlet contains
- The active substances of Circlet are: etonogestrel (11.7 mg) and ethinyl estradiol (2.7 mg)
- The other ingredients are: ethylene and vinyl acetate copolymers (28% and 9% vinyl acetate) (a type of plastic that does not dissolve in the body) and magnesium stearate.
Etonogestrel and ethinyl estradiol are released from the therapeutic vaginal system in amounts of 0.120 mg/day and 0.015 mg/day over a period of 3 weeks.
What Circlet looks like and what the package contains
Circlet is a flexible, transparent, colorless or almost colorless ring with an outer diameter of 54 mm.
Each therapeutic vaginal system is packaged in a separate foil sachet. The sachet can be reopened after opening. The sachets are placed in a cardboard box with a leaflet.
The package contains 1 or 3 systems.
Not all pack sizes may be marketed.
Marketing authorization holder and manufacturer
Marketing authorization holder:
Organon Polska Sp. z o.o.
Marszałkowska Street 126/134
00-008 Warsaw
Tel.: +48 22 105 50 01
[email protected]
Manufacturer:
N.V. Organon, Kloosterstraat 6, 5349 AB Oss, Netherlands.
This medicinal product is authorized in the Member States of the European Economic Area under the following names:
Circlet
0.120 mg/0.015 mg/24 h, Therapeutic Vaginal System
Belgium, Germany, Hungary, Luxembourg, Netherlands, Poland, Portugal, Slovakia, Spain.
Date of last revision of the leaflet: 09/2022
These stickers, stuck on the corresponding day in the calendar, can help remember when to insert and remove the Circlet therapeutic vaginal system.
Insert system
Remove system
therapeutic vaginal system Circlet
therapeutic vaginal system Circlet
- Country of registration
- Active substance
- Prescription requiredYes
- Manufacturer
- ImporterN.V. Organon
- This information is for reference only and does not constitute medical advice. Always consult a licensed doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to CircletDosage form: System, (0.12 mg + 0.015 mg)/24 hActive substance: vaginal ring with progestogen and estrogenPrescription requiredDosage form: System, (0.12 mg + 0.015 mg)/24 hActive substance: vaginal ring with progestogen and estrogenPrescription requiredDosage form: System, (0.120 mg + 0.015 mg)/24 hActive substance: vaginal ring with progestogen and estrogenPrescription not required
Alternatives to Circlet in other countries
The best alternatives with the same active ingredient and therapeutic effect.
Alternative to Circlet in Ukraine
Alternative to Circlet in Spain
Online doctors for Circlet
Discuss dosage, side effects, interactions, contraindications, and prescription renewal for Circlet – subject to medical assessment and local rules.