How to use Novinette
Leaflet attached to the packaging: patient information
Novynette, 0.02 mg + 0.15 mg, film-coated tablets
Ethinylestradiol + Desogestrel
Important information about combined hormonal contraceptives:
- If used correctly, they are one of the most reliable, reversible methods of contraception.
- They slightly increase the risk of blood clots in veins and arteries, especially in the first year of use or after resuming use after a break of 4 weeks or more.
- Caution should be exercised and a doctor should be consulted if the patient suspects that symptoms of blood clots have occurred (see section 2 "Blood clots").
You should carefully read the contents of the leaflet before using the medicine, as it contains important information for the patient
- The leaflet should be kept in case it needs to be read again.
- In case of any doubts, a doctor or pharmacist should be consulted.
- This medicine has been prescribed specifically for this person. It should not be passed on to others. The medicine may harm another person.
- If the patient experiences any side effects, including any side effects not listed in this leaflet, they should tell their doctor or pharmacist. See section 4.
Table of contents of the leaflet
- 1. What is Novynette and what is it used for
- 2. Important information before using Novynette
- 3. How to use Novynette
- 4. Possible side effects
- 5. How to store Novynette
- 6. Contents of the pack and other information
1. What is Novynette and what is it used for
Novynette is a combined oral contraceptive containing ethinylestradiol (estrogen) and desogestrel (progestogen) in low doses.
The mechanism of action of Novynette involves inhibiting ovulation and causing changes in the consistency of cervical mucus.
When used correctly, Novynette provides effective and reversible contraception.
However, in certain situations, its contraceptive effectiveness may be reduced or it may be necessary to discontinue the medicine (see section 2). It is then recommended to either abstain from sexual intercourse or use other contraceptive methods, such as condoms or spermicides.
Remember that combined oral contraceptives, such as Novynette, do not protect against
infection with sexually transmitted diseases (such as AIDS). Only the use of condoms has a protective effect.
2. Important information before using Novynette
General notes
Before starting to take Novynette, you should read the information about blood clots (thrombosis) in section 2. It is especially important to read about the symptoms of blood clots (see section 2 "Blood clots").
Novynette should not be used to delay the start of bleeding.
In exceptional cases, when there is a need to delay the start of bleeding, a doctor should be consulted.
Before starting to use Novynette, the doctor will ask the patient a few questions about her health and the health of her close relatives. The doctor will also measure blood pressure and, depending on the individual case, may also perform some other tests.
When not to use Novynette
Novynette should not be used if the patient has any of the conditions listed below. If the patient has any of the conditions listed below, she should inform her doctor. The doctor will discuss with the patient which other contraceptive method will be more suitable.
- If the patient is allergic to ethinylestradiol or desogestrel or any of the other ingredients of this medicine (listed in section 6); may cause itching, rash or swelling;
- If the patient currently has (or has ever had) a blood clot in the blood vessels of the legs (deep vein thrombosis), lungs (pulmonary embolism), or other organs;
- If the patient knows she has disorders that affect blood clotting - such as protein C deficiency, protein S deficiency, antithrombin III deficiency, factor V Leiden, or antiphospholipid antibodies;
- If the patient requires surgery or will be immobilized for a long time (see "Blood clots");
- If the patient has had a heart attack or stroke;
- If the patient has (or has had in the past) angina pectoris (a disease that causes severe chest pain and may be the first symptom of a heart attack) or transient ischemic attack (transient stroke symptoms);
- If the patient has any of the following diseases that may increase the risk of a blood clot in an artery:
- severe diabetes with blood vessel damage,
- very high blood pressure,
- very high levels of fats in the blood (cholesterol or triglycerides),
- a disease called hyperhomocysteinemia;
- If the patient has (or has had in the past) a type of migraine called "migraine with aura";
- If the patient has (or has had in the past) pancreatitis;
- If the patient has (or has had in the past) liver disease, and liver function has not returned to normal;
- If the patient has (or has had in the past) liver tumors;
- If the patient has (or has had in the past) or suspects breast cancer or genital organ cancer;
- If the patient has unexplained vaginal bleeding;
- If the patient has an enlarged endometrium (abnormal growth of the uterine lining);
- If the patient is pregnant or breastfeeding.
Novynette should not be used in patients with hepatitis C and taking medicinal products containing ombitasvir/paritaprevir/ritonavir, dasabuvir, glecaprevir/pibrentasvir, or sofosbuvir/velpatasvir/voxilaprevir (see also "Novynette and other medicines").
Warnings and precautions
Before starting to use Novynette, the patient should discuss this with her doctor or pharmacist.
In some cases, special caution should be exercised when using Novynette or other combined hormonal contraceptives, and regular visits to the doctor may be necessary.
The patient should tell her doctor if she has any of the following conditions.
If these symptoms occur or worsen while using Novynette, the patient should also tell her doctor.
- if the patient experiences symptoms of angioedema, such as swelling of the face, tongue, and/or throat, and/or difficulty swallowing or hives, potentially with breathing difficulties, she should contact her doctor immediately. Products containing estrogens may cause or worsen symptoms of hereditary or acquired angioedema.
- if the patient smokes;
- if the patient is overweight;
- if the patient has high blood pressure;
- if the patient has heart valve problems or heart rhythm disorders;
- if the patient has superficial thrombophlebitis (blood clots in the veins under the skin);
- if the patient has Crohn's disease or ulcerative colitis (chronic inflammatory bowel diseases);
- if the patient has systemic lupus erythematosus (a disease that affects the body's natural defense system);
- if the patient has hemolytic uremic syndrome (a blood clotting disorder that causes kidney failure);
- if the patient has sickle cell anemia (a hereditary disease of red blood cells);
- if the patient has been diagnosed with high levels of fats in the blood (hypertriglyceridemia) or has a family history of this disease. Hypertriglyceridemia is associated with an increased risk of developing pancreatitis;
- if the patient requires surgery or will be immobilized for a long time (see "Blood clots").
- if the patient has recently given birth, she is at increased risk of blood clots. The patient should consult her doctor to find out how soon she can start taking Novynette after giving birth;
- if the patient has varicose veins;
- if the patient has a family history of breast cancer;
- if the patient has liver or gallbladder disease;
- if the patient has diabetes;
- if the patient has depression or mood changes;
- if the patient has epilepsy (see "Novynette and other medicines");
- if the patient has a disease that first appeared during pregnancy or while using sex hormones [e.g. hearing loss, a blood disease called porphyria, herpes gestationis (a skin rash that occurs during pregnancy), Sydenham's chorea (a nervous system disease that causes involuntary body movements)];
When to contact a doctor?
The patient should contact her doctor immediately
- -if she notices any of the following symptoms, which may indicate that she has a blood clot in her leg (deep vein thrombosis), lung (pulmonary embolism), heart attack, or stroke (see below "Blood clots (thrombosis)"). To find a description of these serious side effects, see "How to recognize a blood clot".
- if she has chloasma (brown spots on the skin, also known as melasma, especially on the face). In this case, she should avoid direct exposure to sunlight or ultraviolet radiation.
BLOOD CLOTS
The use of combined hormonal contraceptives, such as Novynette, is associated with an increased risk of blood clots compared to not using them. In rare cases, a blood clot can block a blood vessel and cause serious complications.
Blood clots can occur
- in veins (also known as "venous thromboembolism" or "venous thrombosis"),
- in arteries (also known as "arterial thrombosis" or "arterial thromboembolism"). Not all blood clots are completely resolved after treatment, and in rare cases, the effects of a blood clot can be permanent or, very rarely, fatal.
Remember that the overall risk of harmful blood clots caused by Novynette is small.
HOW TO RECOGNIZE A BLOOD CLOT
The patient should contact her doctor immediately if she notices any of the following symptoms.
Is the patient experiencing any of these symptoms?
Why is the patient likely to be suffering from
these symptoms?
- swelling of the leg or swelling along a vein in the leg or foot, especially if it is accompanied by:
- pain or tenderness in the leg, which may only be felt when standing or walking, Deep vein thrombosis
only when standing or walking,
- increased temperature in the affected leg,
- change in skin color of the leg, such as pallor, redness, or cyanosis.
- sudden unexplained shortness of breath or rapid breathing;
- sudden unexplained cough, which may be accompanied by coughing up blood;
- sharp chest pain, which may worsen with deep breathing;
- severe dizziness or fainting;
- rapid or irregular heartbeat;
- severe abdominal pain.
If the patient is unsure, she should contact her doctor,
as some of these symptoms, such as coughing or shortness of breath, may be mistaken for milder conditions, such as a respiratory infection (e.g. a cold).
Pulmonary embolism
Symptoms usually occur in one eye:
- sudden loss of vision or, Retinal vein thrombosis (blood clot in the eye)
| |
| Myocardial infarction |
| Stroke |
| Blood clots blocking other blood vessels |
BLOOD CLOTS IN VEINS
What can happen if a blood clot forms in a vein?
- The use of combined hormonal contraceptives is associated with an increased risk of blood clots in the veins (venous thromboembolism). Although these side effects are rare, they can occur, especially in the first year of using combined hormonal contraceptives.
- If blood clots form in the veins of the leg or foot, it can lead to the development of deep vein thrombosis.
- If a blood clot breaks loose from the leg and lodges in the lungs, it can cause a pulmonary embolism.
- In very rare cases, a blood clot can form in another organ, such as the eye (retinal vein thrombosis).
When is the risk of blood clots in a vein highest?
The risk of forming a blood clot in a vein is highest during the first year of using combined hormonal contraceptives for the first time. The risk may also be higher when resuming the use of combined hormonal contraceptives (the same or a different medicine) after a break of 4 weeks or more.
After the first year, the risk decreases, although it is always higher compared to not using combined hormonal contraceptives.
If the patient stops using Novynette, the risk of blood clots returns to normal within a few weeks.
What factors increase the risk of blood clots in veins?
The risk depends on the natural risk of venous thromboembolism and the type of combined hormonal contraceptive used.
The overall risk of blood clots in the legs or lungs associated with Novynette is small.
- In a year, about 2 out of 10,000 women who do not use combined hormonal contraceptives and are not pregnant will develop blood clots.
- In a year, about 5-7 out of 10,000 women who use combined hormonal contraceptives containing levonorgestrel, norethisterone, or norgestimate will develop blood clots.
- In a year, about 9-12 out of 10,000 women who use combined hormonal contraceptives containing desogestrel, such as Novynette, will develop blood clots.
- The risk of blood clots depends on the patient's individual medical history (see "Factors that increase the risk of blood clots", below).
| Risk of blood clots in a year | |
| Women who do not use combined hormonal pills, patches, vaginal rings, and are not pregnant. | About 2 out of 10,000 women |
| Women using combined hormonal contraceptive pills containing levonorgestrel, norethisterone, or norgestimate. | About 5-7 out of 10,000 women |
| Women using Novynette. | About 9-12 out of 10,000 women |
Factors that increase the risk of blood clots in veins
The risk of blood clots associated with Novynette is small, but some factors can increase this risk. The risk is higher:
- if the patient is significantly overweight (body mass index (BMI) over 30 kg/m2);
- if someone in the patient's close family has had blood clots in the legs, lungs, or other organs at a young age (e.g. under 50 years old). In this case, the patient may have a hereditary blood clotting disorder;
- if the patient needs to have surgery, is immobilized for a long time due to injury or illness, or has a leg in a cast. It may be necessary to temporarily stop using Novynette for a few weeks before surgery or immobilization. If the patient needs to stop using Novynette, she should ask her doctor when she can resume using the medicine;
- with age (especially over 35 years old);
- if the patient has recently given birth.
The risk of blood clots increases with the number of risk factors present in the patient.
Long-haul air travel (>4 hours) may temporarily increase the risk of blood clots, especially if the patient has another risk factor.
It is essential to tell the doctor if any of these risk factors are present, even if the patient is not sure. The doctor may decide to stop the use of Novynette.
If any of the above conditions change while using Novynette, the patient should inform her doctor, e.g. if someone in her close family is diagnosed with a blood clot without a known cause or if the patient gains significant weight.
BLOOD CLOTS IN ARTERIES
What can happen if a blood clot forms in an artery?
Similar to blood clots in veins, blood clots in arteries can cause serious consequences, such as a heart attack or stroke.
Factors that increase the risk of blood clots in arteries
It is essential to note that the risk of a heart attack or stroke associated with Novynette is very small, but it may increase:
- with age (over about 35 years old);
- if the patient smokes.While using a hormonal contraceptive like Novynette, it is recommended to quit smoking. If the patient cannot quit smoking and is over 35 years old, the doctor may recommend using a different type of contraception;
- if the patient is overweight;
- if the patient has high blood pressure;
- if someone in the patient's close family has had a heart attack or stroke at a young age (under 50 years old). In this case, the patient may also be at increased risk of having a heart attack or stroke;
- if the patient or someone in her close family has high levels of fats in the blood (cholesterol or triglycerides);
- if the patient has migraines, especially migraines with aura;
- if the patient has heart disease (valve damage, heart rhythm disorder called atrial fibrillation);
- if the patient has diabetes.
If the patient has more than one of the above conditions or if any of them are severe, the risk of blood clots may be even higher.
The patient should inform her doctor if any of the above conditions change while using Novynette, e.g. if she starts smoking, someone in her close family is diagnosed with a blood clot without a known cause, or if she gains significant weight.
Pill and cancer
Women using the pill have a slightly increased risk of breast cancer compared to women of the same age who do not use the pill. This small increase in the risk of breast cancer disappears gradually within 10 years of stopping the pill.
It is not known whether this difference is caused by the pill. It may be related to the fact that women using the pill are more likely to have regular medical check-ups and breast cancer is detected earlier.
Rarely, women using the pill have been reported to have benign liver tumors, and even more rarely, malignant liver tumors. If the patient experiences severe abdominal pain, she should contact her doctor.
Psychological disorders
Some women using hormonal contraceptives, including Novynette, have reported depression or low mood. Depression can be severe and sometimes lead to suicidal thoughts. If mood changes or symptoms of depression occur, the patient should contact her doctor as soon as possible for further medical advice.
Irregular bleeding
During the first few months of using Novynette, unexpected bleeding (breakthrough bleeding) may occur. If such bleeding persists for longer than a few months or starts after a few months, the doctor should be consulted to determine the cause.
What to do if bleeding does not occur during the pill-free week
If all the pills have been taken correctly, it is very unlikely that the patient is pregnant. However, if the expected withdrawal bleeding does not occur twice in a row, it may indicate pregnancy. The patient should contact her doctor immediately. The patient should only start the next pack of Novynette when she is sure she is not pregnant.
Children and adolescents
The safety and efficacy of Novynette in adolescents under 18 years of age have not been established. There are no available data.
Novynette and other medicines
The patient should tell her doctor or pharmacist about all medicines she is currently taking or has recently taken, as well as any medicines she plans to take. The patient should also inform any other doctor or dentist prescribing any other medicine (or pharmacist) that she is using Novynette. Doctors may advise whether additional contraceptive methods should be used (e.g. condoms) and for how long.
Novynette should not be used in patients with hepatitis C and taking medicinal products containing ombitasvir/paritaprevir/ritonavir, dasabuvir, glecaprevir/pibrentasvir, or sofosbuvir/velpatasvir/voxilaprevir, as these medicines may cause abnormal liver function test results (increased liver enzyme activity).
Before starting these medicines, the doctor will prescribe a different contraceptive method.
Novynette can be started again about 2 weeks after the end of the above-mentioned treatment. See "When not to use Novynette".
Certain medicines may affect the levels of Novynette in the blood, leading to reducedcontraceptive effectivenessand unexpected bleeding. These include
- medicines used to treat:
- epilepsy (e.g. phenytoin, phenobarbital, primidone, carbamazepine, felbamate, oxcarbazepine, topiramate),
- tuberculosis (e.g. rifampicin, rifabutin),
- HIV infection (protease inhibitors and non-nucleoside reverse transcriptase inhibitors, such as ritonavir, nevirapine, efavirenz, nelfinavir),
- hepatitis C (boceprevir, telaprevir),
- fungal infections (griseofulvin),
- high blood pressure in the blood vessels of the lungs (bosentan),
- herbal products containing St. John's Wort ( Hypericum perforatum). If the patient wants to use herbal products containing St. John's Wort while using Novynette, she should consult her doctor first.
The following medicines may reduce the tolerance of Novynette:
- ketokonazole, itraconazole, fluconazole (used to treat fungal infections);
- macrolide antibiotics, such as clarithromycin, erythromycin (used to treat bacterial infections);
- calcium channel blockers, such as diltiazem (used to treat certain heart diseases and high blood pressure);
- etoricoxib (used to treat arthritis, osteoarthritis).
Novynette may affect the action of other medicines, such as:
- cyclosporin (a medicine used to prevent organ rejection after transplants),
- the antiepileptic medicine lamotrigine (may increase the frequency of seizures),
- tizanidine (a medicine used to treat muscle spasticity),
- levothyroxine (a medicine used to treat hypothyroidism),
- theophylline (a medicine used to treat asthma).
Before using any medicine, the patient should consult her doctor or pharmacist.
Lab tests
The patient should inform her doctor or laboratory staff that she is taking the pill, as oral contraceptives may affect the results of some laboratory tests.
Pregnancy and breastfeeding
If the patient is pregnant or breastfeeding, thinks she may be pregnant, or plans to have a child, she should consult her doctor or pharmacist before using this medicine.
Novynette should not be used during pregnancy. If the patient is pregnant or thinks she may be pregnant, she should stop using Novynette immediately and inform her doctor without delay.
Novynette is not recommended during breastfeeding. If the patient is breastfeeding and wants to use the pill during this time, she should contact her doctor.
Driving and using machines
While using Novynette, the patient can drive and use machines.
Novynette contains lactose
If the patient has been diagnosed with intolerance to some sugars, she should contact her doctor before taking the medicine.
3. How to use Novynette
This medicine should always be used as directed by the doctor. In case of doubt, the patient should consult her doctor or pharmacist.
Each pack of Novynette contains 1 blister pack of 21 film-coated tablets or 3 blister packs of 21 film-coated tablets. The special labeling of the blister packs with the symbols of the days of the week makes it easier to control the regular use of the contraceptive pills.
Each tablet in the pack is marked with the symbol of the day of the week on which it should be taken. The patient should take 1 tablet daily for 21 consecutive days, following the direction of the arrows on the blister pack, until the pack is empty.
After taking all 21 tablets from the blister pack, there is a 7-day break in taking the tablets. During the 2nd or 3rd day of the break, withdrawal bleeding should occur, similar to a menstrual period.
The patient should start taking the tablets from the next pack on the 8th day (after the 7-day break), even if the bleeding has not stopped yet. With regular use of Novynette, the start of taking the tablets from the next pack will always fall on the same day of the week, and the bleeding will occur on the same day of the month.
The tablets should always be taken at the same time.
Taking the tablets in the morning (the first thing in the morning) or late in the evening (the last thing before bedtime) can make it easier to remember to take them regularly.
The tablets should be swallowed whole, with water if necessary.
How to start using Novynette
If the patient has not used hormonal contraceptives in the previous month
The patient should start taking the tablets on the first day of her natural menstrual cycle (i.e. on the first day of her period). It is allowed to start taking the tablets between the 2nd and 5th day, but in this case, during the first cycle, additional mechanical contraceptive methods (e.g. condoms) should be used for the first 7 days of taking the tablets.
Switching from another combined contraceptive (pill, vaginal ring, transdermal patch)
The patient should start using Novynette the day after taking the last active tablet of the previous oral contraceptive, or at the latest, on the day after the usual break in using the previous contraceptive method. Additional contraceptive methods are not required.
If the patient has been using a vaginal ring or transdermal patch, she should start taking Novynette on the day the ring or patch is removed, or at the latest, on the day the next ring or patch would have been applied. Additional contraceptive methods are not required.
Switching from progestogen-only contraceptives (mini-pill, injections, implants)
The patient can switch from a progestogen-only pill at any time (from an implant on the day of its removal or from injections on the day the next injection is scheduled) to Novynette, but in all cases, additional contraceptive methods should be used for the first 7 days of taking the tablets.
Use after miscarriage in the first trimester of pregnancy
The patient should start taking the tablets immediately. Additional contraceptive methods are not required.
Use after childbirth or miscarriage in the second trimester of pregnancy
For breastfeeding women, see "Pregnancy and breastfeeding".
The doctor will advise the patient to start taking the tablets between the 21st and 28th day after childbirth or miscarriage in the second trimester. If the patient starts taking the tablets later, she should use additional mechanical contraceptive methods (e.g. condoms) for the first 7 days of taking the tablets. However, if the patient has had sexual intercourse, she should make sure she is not pregnant before starting to use the tablets or wait for her first menstrual period.
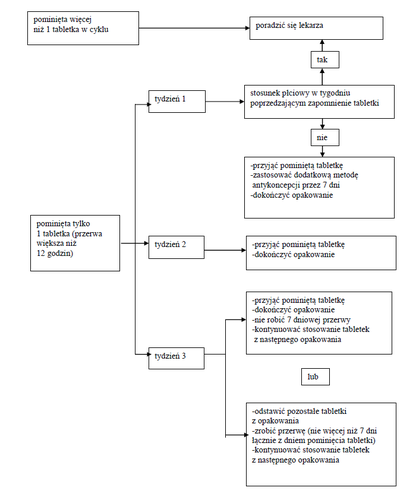
What to do if more than one tablet is missed from the pack
The patient should consult her doctor.
In the case of missed tablets, the patient should follow the two basic rules below:
- 1. The break in continuous tablet-taking should never be longer than 7 days.
- 2. It is necessary to take tablets continuously for 7 days to achieve the proper suppression of the hypothalamic-pituitary-ovarian axis.
In daily practice, the doctor may give the following advice:
Week 1
The patient should take the last missed tablet as soon as she remembers, even if it means taking 2 tablets at the same time. Then she should continue taking the tablets at the usual time of day. For the next 7 days, she should use additional mechanical contraceptive methods, such as condoms. If the patient had sexual intercourse during the 7 days before missing the tablet, she should consider the possibility of pregnancy. The more tablets are missed and the closer they are to the break in taking the tablets, the higher the risk of pregnancy.
Week 2
The patient should take the last missed tablet as soon as she remembers, even if it means taking 2 tablets at the same time. Then she should continue taking the tablets at the usual time of day. If the tablets have been taken correctly for the 7 days before missing the tablet, there is no need to use additional contraceptive methods. However, if this is not the case or if the patient has missed more than 1 tablet, she should use additional contraceptive methods for 7 days.
Week 3
The risk of reduced contraceptive protection is inevitable due to the upcoming break in taking the tablets. However, this can be prevented by adjusting the way the tablets are taken. Therefore, there is no need to use additional contraceptive methods if one of the two alternative rules below is followed, provided that all the tablets have been taken correctly during the 7 days before missing the tablet. If this is not the case, the patient should follow the first of the two alternative rules and use additional contraceptive methods for the next 7 days.
- 1. The patient should take the last missed tablet as soon as she remembers, even if it means taking 2 tablets at the same time. Then she should continue taking the tablets at the usual time of day. The next pack of Novynette should be started immediately after finishing the current pack, i.e. without a break between packs. Withdrawal bleeding may not occur until the end of the next pack, but the patient may experience breakthrough bleeding or spotting during tablet-taking.
- 2. The doctor may advise the patient to stop taking the tablets from the current pack. In this case, the patient should have a break of up to 7 days, including the days she missed the tablets, and then continue taking the tablets from the next pack.
If the patient misses tablets and does not have withdrawal bleeding during the first break in taking the tablets, she should consider the possibility of pregnancy.
4. Possible Side Effects
Like all medicines, this medicine can cause side effects, although not everybody gets them.
If any side effects occur, especially severe and persistent ones, or changes in health that the patient considers to be related to the use of Novynette, a doctor should be consulted.
A doctor should be contacted immediately if the patient experiences any of the following symptoms of angioedema: swelling of the face, tongue, and/or throat, and/or difficulty swallowing or urticaria, potentially with difficulty breathing (see also "Warnings and Precautions").
In all women using combined hormonal contraceptives, there is an increased risk of blood clots in the veins (venous thromboembolism) or blood clots in the arteries (arterial thrombosis). For detailed information on the various risk factors associated with the use of combined hormonal contraceptives, see section 2 "Important Information Before Using Novynette".
Frequent (may occur in up to 1 in 10 people):depression, mood changes, headache, nausea, abdominal pain, breast pain, breast tenderness, weight gain.
Uncommon (may occur in up to 1 in 100 people):fluid retention, decreased libido, migraine, vomiting, diarrhea, rash, urticaria, breast enlargement.
Rare (may occur in up to 1 in 1000 people):hypersensitivity, increased libido, eye irritation due to contact lenses, skin disorders (erythema multiforme, erythema nodosum), abnormal cervical smear, breast discharge, weight loss.
Harmful blood clots in a vein or artery, for example:
- in the leg or foot (e.g., deep vein thrombosis),
- in the lungs (e.g., pulmonary embolism),
- heart attack,
- stroke,
- mini-stroke or transient stroke-like symptoms, known as a transient ischemic attack,
- blood clots in the liver, stomach, and/or intestine, kidneys, or eye. The risk of blood clots may be higher if the patient has any other risk factors (see section 2 for further information on risk factors and symptoms of blood clots).
Reporting Side Effects
If any side effects occur, including any side effects not listed in the leaflet, a doctor or pharmacist should be informed. Side effects can be reported directly to the Department of Post-Marketing Surveillance of Adverse Reactions to Medicinal Products, Office for Registration of Medicinal Products, Medical Devices, and Biocidal Products, Al. Jerozolimskie 181C, 02-222 Warsaw, Tel.: +48 22 49 21 301, Fax: +48 22 49 21 309, Website: https://smz.ezdrowie.gov.pl. Side effects can also be reported to the marketing authorization holder. By reporting side effects, more information can be gathered on the safety of the medication.
5. How to Store Novynette
The medication should be stored out of sight and reach of children.
Store at a temperature below 30°C. Store in the original packaging.
Do not use this medication after the expiration date stated on the packaging. The expiration date refers to the last day of the specified month.
Medications should not be disposed of in wastewater or household waste containers. A pharmacist should be asked how to dispose of unused medications. This will help protect the environment.
6. Package Contents and Other Information
What Novynette Contains
The active substances are ethinylestradiol and desogestrel. One coated tablet contains 20 micrograms of ethinylestradiol and 150 micrograms of desogestrel.
Other ingredients are:
Tablet core: α-tocopherol, magnesium stearate, colloidal silicon dioxide, stearic acid, povidone, potato starch, lactose monohydrate, quinoline yellow (E104).
Coating: propylene glycol, polyethylene glycol 6000, hydroxypropylmethylcellulose.
What Novynette Looks Like and What the Package Contains
Pale yellow, round, biconvex tablets with engraved "RG" on one side and "P9" on the other side.
A carton box contains 1 blister or 3 blisters of 21 coated tablets.
Marketing Authorization Holder and Manufacturer
Gedeon Richter Plc.
Gyömrői út 19-21
1103 Budapest, Hungary
For more detailed information, please contact the local representative of the marketing authorization holder:
GEDEON RICHTER POLSKA Sp. z o.o.
Medical Department
ul. ks. J. Poniatowskiego 5
05-825 Grodzisk Mazowiecki
Tel. +48 (22)755 96 48
[email protected]
Date of Last Update of the Leaflet:
- Country of registration
- Active substance
- Prescription requiredYes
- Manufacturer
- ImporterGedeon Richter Plc.
- This information is for reference only and does not constitute medical advice. Always consult a licensed doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to NovinetteDosage form: Tablets, 30 mcg + 150 mcgActive substance: desogestrel and ethinylestradiolManufacturer: mibe GmbH Arzneimittel Sun-Farm Sp. z o.o.Prescription requiredDosage form: Tablets, 20 mcg + 150 mcgActive substance: desogestrel and ethinylestradiolManufacturer: mibe GmbH Arzneimittel Sun-Farm Sp. z o.o.Prescription requiredDosage form: Tablets, 0.15 mg + 0.03 mgActive substance: desogestrel and ethinylestradiolManufacturer: N.V. OrganonPrescription required
Alternatives to Novinette in other countries
The best alternatives with the same active ingredient and therapeutic effect.
Alternative to Novinette in Ukraine
Alternative to Novinette in Spain
Online doctors for Novinette
Discuss dosage, side effects, interactions, contraindications, and prescription renewal for Novinette – subject to medical assessment and local rules.