

Fluticomb

Ask a doctor about a prescription for Fluticomb

How to use Fluticomb
Leaflet accompanying the packaging: patient information
Fluticomb, (25 micrograms + 50 micrograms)/dose, inhalation aerosol,
suspension
Fluticomb, (25 micrograms + 125 micrograms)/dose, inhalation aerosol, suspension
Fluticomb, (25 micrograms + 250 micrograms)/dose, inhalation aerosol, suspension
Salmeterol + Fluticasone propionate
It is essential to carefully read the contents of the leaflet before using the medicine, as it contains important information for the patient.
- The leaflet should be kept to be able to read it again if necessary.
- In case of any doubts, the doctor or pharmacist should be consulted.
- This medicine has been prescribed to a specific person. It should not be given to others. The medicine may harm another person, even if the symptoms of their illness are the same.
- If the patient experiences any side effects, including any side effects not listed in this leaflet, they should tell their doctor or pharmacist. See section 4.
Table of contents of the leaflet
- 1. What is Fluticomb and what is it used for
- 2. Important information before using Fluticomb
- 3. How to use Fluticomb
- 4. Possible side effects
- 5. How to store Fluticomb
- 6. Contents of the packaging and other information
1. What is Fluticomb and what is it used for
Fluticomb contains two active substances: salmeterol (as salmeterol xinafoate) and fluticasone propionate.
- Salmeterol is a long-acting bronchodilator. Bronchodilators help maintain the patency of the airways. This facilitates the flow of air to and from the lungs. The effect lasts for at least 12 hours.
- Fluticasone propionate is a corticosteroid that reduces swelling and irritation of the lungs.
The doctor has prescribed this medicine to the patient to prevent breathing disorders that occur in asthma. To ensure proper control of asthma, Fluticomb must be used every day, as recommended by the doctor.
Fluticomb prevents the occurrence of shortness of breath and wheezing in the airways. However, it should not be used to control sudden attacks of shortness of breath or wheezing in the airways. If such an attack occurs, it is necessary to use a fast-acting bronchodilator, such as salbutamol, immediately. The patient should always have such a medicine with them.
It is very important to use the fast-acting bronchodilator, such as salbutamol, and the patient should always have such a medicine with them.
2. Important information before using Fluticomb
When not to use Fluticomb:
- if the patient is allergic to salmeterol, fluticasone propionate, or any other component of this medicine - norflurane (HFA - 134a).
Warnings and precautions
Before starting to use Fluticomb, the patient should discuss it with their doctor or pharmacist, especially if they have:
- heart disease, including irregular or rapid heartbeat,
- hyperthyroidism,
- high blood pressure,
- diabetes (Fluticomb may increase blood glucose levels),
- low potassium levels in the blood,
- tuberculosis currently being treated or having been treated or other lung infections.
If the patient experiences blurred vision or other vision disturbances, they should contact their doctor.
Fluticomb and other medicines
The patient should tell their doctor or pharmacist about all medicines they are currently taking or have recently taken, as well as any medicines they plan to take, including those used for asthma and those available without a prescription. Fluticomb should not be used with certain medicines. Before starting to use Fluticomb, the patient should inform their doctor about taking the following medicines:
- β-adrenergic blockers (e.g., atenolol, propranolol, and sotalol). β-adrenergic blockers are most often used to treat high blood pressure or other heart diseases.
- Medicines used to treat infections (e.g., ketoconazole, itraconazole, and erythromycin), including some medicines used to treat HIV (e.g., ritonavir, cobicistat-containing products). Some of these medicines may increase the levels of fluticasone propionate or salmeterol in the body. This may increase the risk of side effects, including irregular heartbeat or worsening of existing side effects. The doctor may want to closely monitor the patient's condition while taking such medicines.
- Corticosteroids (orally or by injection). If the patient has recently taken such medicines, it may increase the risk of adrenal gland dysfunction.
- Diuretics used to treat high blood pressure.
- Other bronchodilators (such as salbutamol).
- Medicines containing xanthine derivatives, often used to treat asthma.
Pregnancy and breastfeeding
If the patient is pregnant or breastfeeding, thinks they may be pregnant, or plans to have a child, they should consult their doctor before using this medicine.
Driving and using machines
It is unlikely that Fluticomb will affect the ability to drive or use machines.
Athletes
Using the medicine without therapeutic need is doping and may still result in a positive doping test.
3. How to use Fluticomb
This medicine should always be used as directed by the doctor or pharmacist. In case of doubts, the doctor or pharmacist should be consulted.
- Fluticomb should be used daily until the doctor recommends otherwise. The recommended dose should not be exceeded. In case of doubts, the doctor or pharmacist should be consulted.
- The use of Fluticomb should not be stopped or the dose reduced without consulting the doctor.
- Fluticomb should be inhaled into the lungs through the mouth.
- The number of doses should always be controlled. The inhaler is designed to deliver 120 doses. However, it is not possible to determine when the inhaler is empty and when 120 doses have been released. A small amount of suspension may remain in the container. Therefore, the inhaler should be replaced after 120 doses have been released to ensure that the correct amount of medicine is received in each release.
Adults and adolescents over 12 years old:
- Fluticomb, (25 micrograms + 50 micrograms): two inhalations twice a day.
- Fluticomb, (25 micrograms + 125 micrograms): two inhalations twice a day.
- Fluticomb, (25 micrograms + 250 micrograms): two inhalations twice a day.
Children from 4 to 12 years old:
- Fluticomb (25 micrograms + 50 micrograms): two inhalations twice a day.
- Fluticomb is not recommended for use in children under 4 years old.
If the symptoms are well-controlled while using Fluticomb twice a day, the doctor may recommend reducing the frequency of use to once a day. The dose can be given:
- once a day, in the evening, if the patient's symptoms occur at night,
- once a day, in the morning, if the patient's symptoms occur during the day.
It is very important to follow the doctor's recommendations regarding the number of inhalations to be used and how often to use them. If the patient is using Fluticomb to treat asthma, the doctor will regularly check the symptoms.
In case of worsening asthma symptoms or loss of asthma control, the patient should
immediately contact their doctor.There may be an increase in wheezing, more frequent chest tightness, or a need for a higher dose of a fast-acting inhalation medicine to facilitate breathing. In such a situation, the patient should continue to use Fluticomb but not increase the number of inhalations. The symptoms of the disease may worsen, and the patient's condition may deteriorate. The patient should contact their doctor, as they may need additional treatment.
Instructions for using the inhaler
- The doctor, nurse, or pharmacist should instruct the patient on how to properly use the inhaler. They should periodically check if the patient is using the inhaler correctly. Using Fluticomb contrary to the doctor's recommendation or incorrect use of the inhaler may cause the medicine to not produce the expected improvement in asthma.
- The medicine is placed in a pressure container, in a plastic housing with a mouthpiece.
- A new full inhaler has enough medicine for at least 120 doses. After 120 releases, the inhaler may no longer have enough medicine to deliver a full dose.
Checking the inhaler
- 1. Before first use, check if the inhaler is working. Remove the cap from the inhaler mouthpiece by gently pressing the sides of the cap with your thumb and index finger.
- 2. To make sure the inhaler is working, shake it vigorously, point the mouthpiece away from you, and press the container firmly to release a dose of medicine into the air. Repeat this process, shaking the inhaler and releasing a second dose of medicine into the air. Before using the inhaler, release two doses of medicine into the air.
- 3. After these two attempts, you can start using the inhaler.
- 4. If the inhaler has not been used for a week or longer, it should be tested. To do this, shake it vigorously and then point the mouthpiece away from you and press the container firmly to release two doses of medicine into the air.
WARNING
Never remove the metal containers from the inhaler at any time. If the inhaler is very cold (below 0°C), remove the metal container from the plastic housing and warm it in your hands for a few minutes before use. Never use anything else to heat the inhaler. After warming and before using the inhaler, press the container firmly to release two doses of medicine into the air.
Reordering
Before the inhaler is empty and all doses have been released, a new inhaler should be ordered. It is essential to remember this to avoid being without the medicine.
Using the inhaler
It is crucial to start breathing slowly, as slowly as possible, before using the inhaler.


- 1. Inhale while standing or sitting upright.
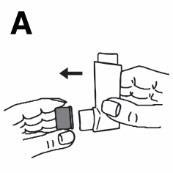
- 2. Remove the cap from the inhaler mouthpiece (as shown in Figure A).
- 3. Check the mouthpiece outside and inside to ensure it is clean and free of foreign objects.
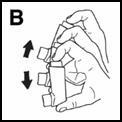
- 4. Shake the inhaler 4 or 5 times to ensure the contents are evenly mixed (Figure B).
- 5. Hold the inhaler with your fingers, with your thumb on the base of the inhaler, below the mouthpiece. Take a deep breath out, as deep as possible (Figure C).
- 6. Put the mouthpiece in your mouth, between your upper and lower teeth, and close your lips around it. Do not bite the mouthpiece.
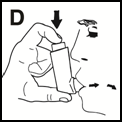
- 7. Start a slow and deep inhalation through your mouth. Immediately after starting inhalation, press the inhaler to release a dose of medicine, and then continue with a calm, deep inhalation (Figure D).
- 8. Hold your breath, remove the inhaler from your mouth, and take your finger off the inhaler. Hold your breath for a few seconds or as long as it is comfortable, then exhale slowly.
- 9. Wait about half a minute before repeating the steps described in points 4 to 8.
- 10. Rinsing the mouth with water and spitting it out and (or) brushing your teeth after inhalation helps prevent hoarseness and thrush.
- 11. After inhalation, always put the cap back on the mouthpiece to prevent dust from entering it (Figure E). Put the cap on by clicking it into place. Do not use too much force.
Do not rush through the steps in points 5, 6, 7, and 8. It is essential to breathe as slowly as possible before inhalation. To ensure that the inhalation is performed correctly, initially, the patient should control the way they take the medicine in front of a mirror. The "mist" coming out of the inhaler, mouth, or nose during inhalation indicates incorrect inhalation technique. The patient should repeat the steps starting from point 4. As with all inhalers, caregivers should ensure that children prescribed Fluticomb use the inhaler correctly, as described above. If the patient has difficulty coordinating their breath and inhalation from the inhaler, the doctor may recommend using the inhaler with an AeroChamber Plus inhalation chamber. The doctor, nurse, or pharmacist should instruct the patient on how to properly use the inhaler with the inhalation chamber and how to care for the inhalation chamber, as well as answer any questions the patient may have. If the patient uses an inhalation chamber, it is essential not to stop using it without consulting the doctor or nurse. Other inhalation chambers should not be used to inhale Fluticomb, and the type of inhalation chamber used should not be changed. It is also essential for the patient not to change the type of inhalation chamber or stop using the inhalation chamber without consulting the doctor. The doctor may decide to change the treatment. Always consult the doctor before making any changes to the asthma treatment. Older children or people with weak hands may find it easier to hold the inhaler with both hands. They should hold the inhaler with two index fingers on top of the inhaler and both thumbs on the bottom below the mouthpiece.
Cleaning the inhaler
To prevent the inhaler from clogging, it should be cleaned at least once a week. To clean the inhaler:
- Remove the cap from the mouthpiece.
- Do not remove the metal container from the plastic housing during cleaning or at any other time.
- Clean the mouthpiece inside and outside and the plastic housing outside with a dry cloth or tissue.
- Put the cap back on the mouthpiece. When the cap is properly placed, it will click. Do not use too much force.
- Do not wash or immerse any parts of the inhaler in water.
Using a higher dose of Fluticomb than recommended
It is essential to use the inhaler as directed. If a higher dose than recommended is used accidentally, the doctor or pharmacist should be informed. The following may occur: faster than normal heartbeat, tremors, dizziness, headache, muscle weakness, and joint pain. If higher doses are used for an extended period, the doctor or pharmacist should be consulted for advice, as high doses of Fluticomb may cause a decrease in the production of steroid hormones by the adrenal glands.
Missing a dose of Fluticomb
A double dose should not be used to make up for a missed dose. The next dose should be taken at the scheduled time.
Stopping the use of Fluticomb
It is very important to take Fluticomb every day as directed by the doctor. The patient should take the medicine until the doctor recommends stopping it. The patient should not suddenly stop taking Fluticomb or reduce the dose, as the symptoms of the disease may worsen. Additionally, sudden stopping or reduction of Fluticomb may (very rarely) cause adrenal gland dysfunction (adrenal insufficiency), which can sometimes cause side effects. These side effects may include:
- abdominal pain,
- fatigue and loss of appetite, nausea,
- vomiting and diarrhea,
- weight loss,
- headache and drowsiness,
- low blood sugar,
- low blood pressure and seizures.
When the body is under stress, such as from fever, injury (e.g., a car accident), infection, or surgery, adrenal insufficiency may worsen, and any of the above side effects may occur. If the patient experiences any of these side effects, they should inform their doctor or pharmacist. To prevent these symptoms, the doctor may prescribe additional corticosteroids in tablet form (e.g., prednisolone). If the patient has any further doubts about using this medicine, they should consult their doctor or pharmacist.
4. Possible side effects
Like all medicines, Fluticomb can cause side effects, although not everybody gets them. To minimize the risk of side effects, the doctor will recommend the smallest dose of Fluticomb that controls asthma.
Allergic reactions: The patient may experience sudden breathing difficulties immediately after
using Fluticomb.There may be an increase in wheezing, coughing, or shortness of breath, as well as itching, rash (hives), and swelling (usually of the face, lips, tongue, or throat). There may also be a feeling of a very fast heartbeat, weakness, and dizziness (which can lead to falling or loss of consciousness). If any of these symptoms occur suddenly after using Fluticomb, the patient should stop using Fluticomb and contact their doctor immediately.Allergic reactions to Fluticomb are uncommon (they may occur less often than in 1 in 100 people). Other side effects:
Very common (may occur more often than in 1 in 10 people):
- Headache - this side effect usually decreases over time while continuing treatment.
- Increased frequency of colds in patients with chronic obstructive pulmonary disease (COPD).
Common (may occur less often than in 1 in 10 people):
- Thrush (painful, creamy-yellow patches) in the mouth and throat, as well as tongue pain, hoarseness, and throat irritation. Rinsing the mouth with water and spitting it out and (or) brushing your teeth after each inhalation may be helpful. The doctor may recommend an antifungal medicine to treat thrush.
- Pain, swelling of the joints, and muscle pain.
- Muscle cramps.
The following side effects have been reported in patients with chronic obstructive pulmonary disease (COPD):
- Pneumonia and bronchitis (lung infection). The patient should tell their doctor if they experience any of the following symptoms: increased mucus production, change in mucus color, fever, chills, worsening cough, or increased breathing difficulties.
- Easier bruising and fractures.
- Sinusitis (feeling of tension and fullness in the nose, cheeks, and behind the eyes, sometimes with a pulsating headache).
- Decreased potassium levels in the blood (the patient may experience irregular heartbeat, muscle weakness, or cramps).
Uncommon (may occur less often than in 1 in 100 people):
- Increased blood sugar (glucose) levels (hyperglycemia). In patients with diabetes, it may be necessary to monitor blood sugar levels more frequently and adjust the dose of antidiabetic medicines being taken.
- Cataract (clouding of the lens of the eye).
- Very fast heartbeat (tachycardia).
- Feeling of trembling and fast or irregular heartbeat (palpitations) - these symptoms usually are not serious and decrease over time while continuing treatment.
- Chest pain.
- Anxiety (occurs mainly in children).
- Sleep disturbances.
- Allergic skin rash.
Rare (may occur less often than in 1 in 1000 people):
- Wheezing or breathing difficulties worsening immediately after taking Fluticomb.If such symptoms occur, the patient should stop using Fluticomb, use a fast-acting inhalation medicine to facilitate breathing, and contact their doctor immediately.
- Fluticomb may disrupt the normal production of steroid hormones by the body, especially when taking high doses of the medicine for a long time. The symptoms include:
- growth retardation in children and adolescents,
- decreased bone density,
- glaucoma,
- weight gain,
- rounding of the face (Cushing's syndrome). The doctor will regularly check if the patient is experiencing such side effects and ensure that the patient is using the smallest dose of Fluticomb that controls asthma.
- Changes in behavior, such as excessive excitement and irritability (these symptoms occur mainly in children).
- Irregular heartbeat or extra beats (arrhythmia). The patient should inform their doctor about this, but not stop using Fluticomb unless the doctor recommends it.
- Fungal infection of the esophagus, which can cause difficulty swallowing.
Side effects with unknown frequency (frequency cannot be estimated from available data):
- Depression or aggression. The occurrence of these side effects is more likely in children.
- Blurred vision.
Reporting side effects
If the patient experiences any side effects, including any side effects not listed in this leaflet, they should tell their doctor or pharmacist. Side effects can be reported directly to the Department of Adverse Reaction Monitoring of Medicinal Products, Medical Devices, and Biocidal Products of the Office for Registration of Medicinal Products, Medical Devices, and Biocidal Products, Al. Jerozolimskie 181C, 02-222 Warsaw, Tel.: +48 22 49 21 301, Fax: +48 22 49 21 309, website: https://smz.ezdrowie.gov.pl. Side effects can also be reported to the marketing authorization holder. By reporting side effects, more information can be collected on the safety of the medicine.
5. How to store Fluticomb
The medicine should be stored out of sight and reach of children. Do not store above 25°C. After using the inhaler, put the cap back on the mouthpiece by clicking it into place. Do not use too much force. The metal container contains a suspension under pressure. Do not expose to temperatures above 50°C, protect from direct sunlight. Do not puncture, break, or burn the container, even if it seems empty. As with most inhalation medicines in pressure containers, the therapeutic effect of this medicine may decrease when the container is cold. Do not use this medicine after the expiry date stated on the packaging after EXP. The expiry date refers to the last day of the month stated. The inscription on the packaging after the abbreviation EXP indicates the expiry date, and after the abbreviation Lot, it indicates the batch number. Medicines should not be disposed of via wastewater or household waste. The patient should ask their pharmacist how to dispose of medicines that are no longer needed. This will help protect the environment.
6. Contents of the packaging and other information
What Fluticomb contains
- The active substances of Fluticomb are salmeterol and fluticasone propionate. Each dose of the medicine contains 25 micrograms of salmeterol (as salmeterol xinafoate) and 50, 125, or 250 micrograms of fluticasone propionate.
- The other ingredient is the propellant: norflurane (HFA - 134a). This medicine contains fluorinated greenhouse gases. Each 120-dose inhaler contains 11.2 g of HFA - 134a, which corresponds to 0.016 tons of CO2 equivalent (GWP = 1430).
What Fluticomb looks like and what the packaging contains
Fluticomb is supplied in a metered-dose inhaler containing the medicine as a pressurized suspension for inhalation through the mouth to the lungs. The container under pressure contains a homogeneous suspension for inhalation. Packaging: aluminum container with a metering valve, fitted with a plastic mouthpiece with a purple cap, all in a cardboard box. Each package contains 1 inhaler. Each inhaler contains 120 doses.
Marketing authorization holder and manufacturer
Marketing authorization holder
Zakłady Farmaceutyczne POLPHARMA S.A., ul. Pelplińska 19, 83-200 Starogard Gdański, tel. +48 22 364 61 01
Manufacturer
Genetic S.p.A., Contrada Canfora, 84084 Fisciano (SA), Italy, Zakłady Farmaceutyczne POLPHARMA S.A., ul. Pelplińska 19, 83-200 Starogard Gdański, Poland, Date of last revision of the leaflet:March 2025
- Country of registration
- Active substance
- Prescription requiredYes
- Manufacturer
- ImporterGenetic S.p.A Zakłady Farmaceutyczne POLPHARMA SA
- This information is for reference only and does not constitute medical advice. Always consult a licensed doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to FluticombDosage form: Powder, 50 mcg + 250 mcgActive substance: salmeterol and fluticasoneManufacturer: Aeropharm GmbHPrescription requiredDosage form: Powder, 50 mcg + 500 mcgActive substance: salmeterol and fluticasoneManufacturer: Aeropharm GmbHPrescription requiredDosage form: Powder, (50 micrograms + 500 micrograms)/doseActive substance: salmeterol and fluticasonePrescription required
Alternatives to Fluticomb in other countries
The best alternatives with the same active ingredient and therapeutic effect.
Alternative to Fluticomb in Spain
Alternative to Fluticomb in Ukraine
Online doctors for Fluticomb
Discuss dosage, side effects, interactions, contraindications, and prescription renewal for Fluticomb – subject to medical assessment and local rules.














