HYRIMOZ 80 mg SOLUTION FOR INJECTION IN A PRE-FILLED PEN


How to use HYRIMOZ 80 mg SOLUTION FOR INJECTION IN A PRE-FILLED PEN
Translated with AI
This page provides general information and does not replace a doctor’s consultation. Always consult a doctor before taking any medication. Seek urgent medical care if symptoms are severe.
Show originalContents of the leaflet
Introduction
Package Leaflet: Information for the Patient
Hyrimoz 80 mg solution for injection in pre-filled pen
adalimumab
Read all of this leaflet carefully before you start using this medicine because it contains important information for you.
- Keep this leaflet, you may need to read it again.
- Your doctor will give you a patient information card, which contains important safety information that you need to know before and during treatment with Hyrimoz.
Keep this patient information cardduring your treatment and for the next 4 months after your last injection (or your child's last injection) of Hyrimoz.
- If you have any further questions, ask your doctor or pharmacist.
- This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours.
- If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet. See section 4.
Contents of the pack
- What is Hyrimoz and what is it used for
- What you need to know before you use Hyrimoz
- How to use Hyrimoz
- Possible side effects
- Storage of Hyrimoz
- Contents of the pack and other information
- Instructions for use
1. What is Hyrimoz and what is it used for
Hyrimoz contains the active substance adalimumab, a medicine that works on your body's immune system.
Hyrimoz is used to treat the following inflammatory diseases:
- rheumatoid arthritis,
- psoriatic plaque,
- hidradenitis suppurativa,
- Crohn's disease,
- ulcerative colitis,
- non-infectious uveitis.
The active substance in Hyrimoz, adalimumab, is a monoclonal antibody. Monoclonal antibodies are proteins that target a specific part of the body.
The target of adalimumab is another protein called tumor necrosis factor (TNFα), which is found in high concentrations in the inflammatory diseases described above. By binding to TNFα, Hyrimoz blocks its action and reduces inflammation in these diseases.
Rheumatoid Arthritis
Rheumatoid arthritis is an inflammatory disease of the joints.
Hyrimoz is used to treat rheumatoid arthritis in adults. If you have moderate to severe active rheumatoid arthritis, you may have been given other medicines, such as methotrexate, before. If these medicines have not worked well enough, you will be given Hyrimoz to treat your rheumatoid arthritis.
Hyrimoz can also be used to treat severe, active, and progressive rheumatoid arthritis without previous treatment with methotrexate.
Hyrimoz can reduce the damage to the cartilage and bones of the joints caused by the disease and improve physical function.
Hyrimoz is usually used in combination with methotrexate. If your doctor considers that methotrexate is not suitable for you, Hyrimoz can be given alone.
Psoriatic Plaque
Psoriatic plaque is an inflammatory disease of the skin that causes red, scaly, crusty, and silvery-scaled areas. Psoriatic plaque can also affect the nails, causing them to deteriorate, thicken, and lift off the nail bed, which can be painful. It is believed that psoriasis is caused by a defect in the body's immune system that leads to an increase in skin cell production.
Hyrimoz is used to treat moderate to severe psoriatic plaque in adults.
Hidradenitis Suppurativa in Adults and Adolescents
Hidradenitis suppurativa (also known as inverse acne) is a long-term and often painful inflammatory disease of the skin. Symptoms can include sensitive nodules (lumps) and abscesses (boils) that can secrete pus.
It usually affects specific areas of the skin, such as under the breast, in the armpits, inner thighs, groin, and buttocks. There may also be scarring in the affected areas.
Hyrimoz is used to treat
- moderate to severe hidradenitis suppurativa in adults and
- moderate to severe hidradenitis suppurativa in adolescents from 12 to 17 years old.
Hyrimoz can reduce the number of nodules and abscesses and the pain that is usually associated with this disease. You may have received other medicines before. If these medicines have not worked well enough, you will be given Hyrimoz.
Crohn's Disease in Adults and Children
Crohn's disease is an inflammatory disease of the digestive tract.
Hyrimoz is used to treat
- moderate to severe Crohn's disease in adults and
- moderate to severe Crohn's disease in children and adolescents from 6 to 17 years old.
If you have Crohn's disease, you will be treated first with other medicines. If you do not respond well enough to these medicines, you will be given Hyrimoz to reduce the signs and symptoms of Crohn's disease.
Ulcerative Colitis in Adults and Children
Ulcerative colitis is an inflammatory disease of the large intestine.
Hyrimoz is used to treat
- moderate to severe ulcerative colitis in adults and
- moderate to severe ulcerative colitis in children and adolescents from 6 to 17 years old.
If you have ulcerative colitis, you may be given other medicines first. If these medicines have not worked well enough, you will be given Hyrimoz to reduce the signs and symptoms of the disease.
Non-Infectious Uveitis in Adults and Children
Non-infectious uveitis is an inflammatory disease that affects certain parts of the eye. The inflammation causes a decrease in vision and/or the presence of floaters in the eye (black dots or thin lines that move across the field of vision). Hyrimoz works by reducing this inflammation.
Hyrimoz is used to treat
- adults with non-infectious uveitis with inflammation that affects the back of the eye,
- children from 2 years old with chronic non-infectious uveitis with inflammation that affects the front of the eye.
You may have received other medicines before. If you do not respond well enough to these medicines, you will be given Hyrimoz.
2. What you need to know before your child starts using Hyrimoz
Do not use Hyrimoz
- If you are allergic to adalimumab or any of the other ingredients of this medicine (listed in section 6).
- If you have a severe infection, including tuberculosis, sepsis (blood poisoning), or other opportunistic infections (uncommon infections associated with a weakened immune system). If you have symptoms of any infection, such as fever, wounds, fatigue, or dental problems, it is important that you inform your doctor (see "Warnings and Precautions").
- If you have moderate to severe heart failure. It is important that you tell your doctor if you have had or have any serious heart problems (see "Warnings and Precautions").
Warnings and Precautions
Consult your doctor or pharmacist before starting treatment with Hyrimoz.
Allergic Reaction
- If you have an allergic reaction with symptoms such as chest tightness, difficulty breathing, dizziness, swelling, or rash, stop using Hyrimoz and contact your doctor immediately, as these reactions can be life-threatening.
Infections
- If you have any infection, including chronic or localized infections (such as a leg ulcer), consult your doctor before starting treatment with Hyrimoz. If you are not sure, contact your doctor.
- With treatment with Hyrimoz, you may be more likely to get infections. This risk may be higher if you have reduced lung function. These infections can be serious and include tuberculosis, viral, fungal, parasitic, or bacterial infections, or other uncommon infectious organisms, and sepsis (blood poisoning).
- In rare cases, these infections can be life-threatening. It is important that if you have symptoms such as fever, wounds, fatigue, or dental problems, you inform your doctor. Your doctor may decide to temporarily stop treatment with Hyrimoz.
Tuberculosis (TB)
- Since cases of tuberculosis have been reported in patients treated with adalimumab, your doctor will examine you for signs or symptoms of tuberculosis before starting treatment with Hyrimoz. This will include a thorough medical examination, including your medical history and diagnostic tests (such as chest X-ray and tuberculin test). The results of these tests should be recorded on your patient information card. It is very important that you inform your doctor if you have had tuberculosis or have been in contact with a patient with tuberculosis. Tuberculosis can develop during treatment, even if you have received preventive treatment for tuberculosis. If symptoms of tuberculosis (persistent cough, weight loss, lack of energy, low-grade fever) or any other infection appear during or after treatment, contact your doctor immediately.
Travel/Recurrent Infection
- Tell your doctor if you have lived or traveled in areas where fungal infections such as histoplasmosis, coccidioidomycosis, or blastomycosis are common.
- Tell your doctor if you have a history of recurrent infections or other conditions or factors that increase the risk of infections.
Hepatitis B Virus
- Tell your doctor if you are a carrier of the hepatitis B virus (HBV), if you have an active HBV infection, or if you think you may be at risk of getting HBV. Your doctor should perform an HBV test. Adalimumab may reactivate HBV in people who carry this virus. In rare cases, especially if you are taking other medicines that suppress the immune system, reactivation of HBV infection can be life-threatening.
Age over 65 years
- If you are over 65 years old, you may be more likely to get infections while being treated with Hyrimoz. You and your doctor should pay special attention to the appearance of signs of infection while you are being treated with Hyrimoz. It is important that you inform your doctor if you have symptoms of infections, such as fever, wounds, feeling tired, or dental problems.
Dental Procedures or Surgery
- If you are going to have a surgical or dental procedure, tell your doctor that you are using Hyrimoz. Your doctor may recommend that you temporarily stop treatment with Hyrimoz.
Demyelinating Disease
- If you have or develop a demyelinating disease (a disease that affects the protective covering of the nerves, such as multiple sclerosis), your doctor will decide whether you should be treated or continue treatment with Hyrimoz. Tell your doctor immediately if you have symptoms such as changes in vision, weakness in arms or legs, or numbness or tingling in any part of the body.
Vaccines
- Certain vaccines contain live, weakened forms of bacteria or viruses, which can cause diseases and should not be given during treatment with Hyrimoz, as they may cause infections. Consult your doctor before receiving any type of vaccine. It is recommended that children receive all scheduled vaccinations for their age before starting treatment with Hyrimoz. If you receive Hyrimoz while pregnant, your child may have a higher risk of getting infections during the 5 months following the last dose of Hyrimoz you received during pregnancy. It is important that you inform your child's pediatrician and other healthcare professionals about your use of Hyrimoz during pregnancy, so they can decide whether your child should receive any vaccine (for more information on vaccines, see the "Warnings and Precautions" section).
Heart Failure
- It is important that you tell your doctor if you have had or have any serious heart problems. If you have mild heart failure and are being treated with Hyrimoz, your doctor should closely monitor your heart failure. If new symptoms of heart failure or worsening of existing symptoms appear (such as difficulty breathing or swelling of the feet), you should contact your doctor immediately.
Fever, Bruises, Bleeding, or Pale Appearance
- In some patients, the body may be unable to produce enough of the type of blood cells that fight infections (white blood cells) or those that help stop bleeding (platelets). If you have persistent fever, bruising, or bleeding easily, or are very pale, consult your doctor immediately. Your doctor may decide to interrupt treatment.
Cancer
- In very rare cases, certain types of cancer have been reported in children and adults treated with adalimumab or other TNFα blockers. People with rheumatoid arthritis who have had the disease for a long time and have more severe disease may have a higher than average risk of developing lymphoma or leukemia (cancer that affects blood cells and bone marrow). If you are being treated with Hyrimoz, the risk of getting lymphoma, leukemia, or other types of cancer may increase. A specific and severe type of lymphoma has been observed in rare cases in patients treated with adalimumab.
Some of these patients were also taking the medicines azathioprine or mercaptopurine. Tell your doctor if you are taking azathioprine or mercaptopurine with Hyrimoz.
- Additionally, cases of non-melanoma skin cancer have been observed in patients using adalimumab. Tell your doctor if new areas of damaged skin appear or if existing marks or damaged areas change in appearance during or after treatment.
- Cases of cancer, other than lymphoma, have been reported in patients with a certain lung disease, called chronic obstructive pulmonary disease (COPD), treated with another TNFα blocker. If you have COPD, or are a heavy smoker, you should discuss with your doctor whether treatment with a TNFα blocker is suitable for you.
Autoimmune Diseases
- In rare cases, treatment with Hyrimoz may lead to a lupus-like syndrome. Contact your doctor if you have symptoms such as unexplained persistent rash, fever, joint pain, or fatigue.
Children and Adolescents
- Vaccines: if possible, your child should be up-to-date with all vaccinations before using Hyrimoz.
Other Medicines and Hyrimoz
Tell your doctor or pharmacist if you are taking, have recently taken, or might take any other medicines.
Hyrimoz can be taken with methotrexate or with certain disease-modifying antirheumatic drugs (sulfasalazine, hydroxychloroquine, leflunomide, and injectable gold preparations), corticosteroids, or painkillers, including non-steroidal anti-inflammatory drugs (NSAIDs).
Do not use Hyrimoz with medicines whose active substances are anakinra or abatacept due to an increased risk of serious infections. It is not recommended to combine adalimumab and other TNFα blockers with anakinra or abatacept, due to the possible increased risk of infections, including serious infections, and other potential drug interactions. If you have any doubts, consult your doctor.
Pregnancy and Breastfeeding
- You should consider using adequate contraceptive methods to avoid becoming pregnant and continue their use for at least 5 months after the last treatment with Hyrimoz.
- If you are pregnant or think you may be pregnant, or plan to become pregnant, ask your doctor for advice before taking this medicine.
- Hyrimoz should be used during pregnancy only if necessary.
- According to a pregnancy study, there was no higher risk of congenital defects when the mother had received treatment with adalimumab during pregnancy compared to mothers with the same disease who did not receive treatment with adalimumab.
- Hyrimoz can be used during breastfeeding.
- If you use Hyrimoz while pregnant, your child may have a higher risk of getting infections.
- It is important that you inform your child's pediatrician and other healthcare professionals about your use of Hyrimoz during pregnancy, so they can decide whether your child should receive any vaccine (for more information on vaccines, see the "Warnings and Precautions" section).
Driving and Using Machines
The influence of Hyrimoz on the ability to drive, ride a bicycle, or use machines is small. You may experience dizziness and vision disturbances after using Hyrimoz.
Hyrimoz contains sodium
This medicine contains less than 1 mmol (23 mg) of sodium per 0.8 ml dose; this is essentially "sodium-free".
3. How to use Hyrimoz
Follow your doctor's administration instructions for this medication exactly. If in doubt, consult your doctor again.
The following table indicates the recommended doses of Hyrimoz for each of its approved uses. Your doctor may prescribe a different dose of Hyrimoz if you need a different dose.
Rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, or axial spondyloarthritis without radiographic evidence of ankylosing spondylitis | ||
Age or body weight | What quantity and how often should it be taken? Frequency of administration | Notes |
Adults | 40 mg every other week as a single dose | In the case of rheumatoid arthritis, treatment with methotrexate is maintained during the use of Hyrimoz. If your doctor determines that methotrexate is inappropriate, Hyrimoz can be administered alone. If you have rheumatoid arthritis and do not receive methotrexate during your treatment with Hyrimoz, your doctor may decide to give you 40 mg of Hyrimoz every week or 80 mg every other week. |
Plaque psoriasis | ||
Age or body weight | What quantity and how often should it be taken? | Notes |
Adults | An initial dose of 80 mg (as an 80 mg injection), followed by 40 mg every other week starting one week after the initial dose. | You should continue injecting Hyrimoz for as long as your doctor has indicated. If that dose does not work well enough, your doctor may increase the dose to 40 mg weekly or 80 mg every other week. |
Hidradenitis suppurativa | ||
Age or body weight | What quantity and how often should it be taken? | Notes |
Adults | An initial dose of 160 mg (as two 80 mg injections on the same day or one 80 mg injection per day for two consecutive days), followed by a dose of 80 mg (as an 80 mg injection) two weeks later. After two more weeks, continue with a dose of 40 mg weekly or 80 mg every other week, as prescribed by your doctor. | It is recommended to use an antiseptic liquid daily on the affected areas. |
Adolescents from 12 to 17 years of age with a weight of 30 kg or more | An initial dose of 80 mg (as an 80 mg injection), followed by 40 mg every other week starting one week later. | If that dose does not work well enough, your doctor may increase the dose to 40 mg weekly or 80 mg every other week. It is recommended to use an antiseptic liquid daily on the affected areas. |
Crohn's disease | ||
Age or body weight | What quantity and how often should it be taken? | Notes |
Children, adolescents, and adults with a weight of 40 kg or more | An initial dose of 80 mg (as 80 mg injections), followed by 40 mg every other week starting two weeks later. If a faster response is required, your doctor may prescribe an initial dose of 160 mg (as two 80 mg injections on the same day or 80 mg injections per day for two consecutive days), followed by 80 mg (as an 80 mg injection) two weeks later. From then on, the usual dose is 40 mg every other week. | If that dose does not work well enough, your doctor may increase the dose to 40 mg weekly or 80 mg every other week. |
Pediatric Crohn's disease | ||
Age or body weight | What quantity and how often should it be taken? | Notes |
Children and adolescents from 6 to 17 years of age with a weight less than 40 kg | An initial dose of 40 mg followed by 20 mg every other week starting two weeks later. If a faster response is required, your doctor may prescribe an initial dose of 80 mg (as 80 mg injections) followed by 40 mg two weeks later. From then on, the usual dose is 20 mg every other week. | If that dose does not work well enough, the doctor of your child may increase the frequency of the dose to 20 mg weekly. |
Ulcerative colitis | ||
Age or body weight | What quantity and how often should it be taken? | Notes |
Adults | An initial dose of 160 mg (as two 80 mg injections on the same day or one 80 mg injection per day for two consecutive days) followed by 80 mg (as an 80 mg injection) two weeks later. From then on, the usual dose is 40 mg every other week. | If that dose does not work well enough, your doctor may increase the dose to 40 mg weekly or 80 mg every other week. |
Pediatric ulcerative colitis | ||
Age and body weight | What quantity and how often should it be taken? | Notes |
Children and adolescents from 6 years of age with a weight of 40 kg or more | An initial dose of 160 mg (as two 80 mg injections on the same day or one 80 mg injection per day for two consecutive days) initially, followed by 80 mg (as an 80 mg injection) two weeks later. From then on, the usual dose is 80 mg every other week. | Patient who reach 18 years of age while on treatment with 80 mg every other week should continue with the prescribed dose. |
Children and adolescents from 6 years of age with a weight less than 40 kg | An initial dose of 80 mg (as an 80 mg injection) initially, followed by 40 mg (as a 40 mg injection) two weeks later. From then on, the usual dose is 40 mg every other week. | Patient who reach 18 years of age while on treatment with 40 mg every other week should continue with the prescribed dose. |
Non-infectious uveitis | ||
Age or body weight | What quantity and how often should it be taken? | Notes |
Adults | An initial dose of 80 mg (as an 80 mg injection), followed by 40 mg every other week starting one week after the initial dose. | In non-infectious uveitis, treatment with corticosteroids or other medicines that affect the immune system can be continued during the use of Hyrimoz. Hyrimoz can also be administered alone. You should continue injecting Hyrimoz for as long as your doctor has indicated. |
Children and adolescents from 2 years of age with a weight of 30 kg or more | 40 mg every other week | Your doctor may also prescribe an initial dose of 80 mg, which can be administered one week before starting the usual dose of 40 mg every other week. The use of Hyrimoz in combination with methotrexate is recommended. |
Children and adolescents from 2 years of age with a weight less than 30 kg | 20 mg every other week | Your doctor may also prescribe an initial dose of 40 mg, which can be administered one week before starting the usual dose of 20 mg every other week. The use of Hyrimoz in combination with methotrexate is recommended. |
Form and route of administration
Hyrimoz is injected under the skin (subcutaneously).
Detailed instructions on how to inject Hyrimoz are found in section 7, “Instructions for use”.
If you use more Hyrimoz than you should
If you accidentally inject Hyrimoz more frequently than you should, call your doctor or pharmacist and explain that you have taken more than necessary. Always carry the medicine box with you, even if it is empty.
If you forget to use Hyrimoz
If you forget to administer an injection, you should inject the next dose of Hyrimoz as soon as you remember. Then, the next dose will be administered as usual, as if you had not forgotten a dose.
If you interrupt treatment with Hyrimoz
The decision to stop using Hyrimoz should be discussed with your doctor. Your symptoms may return after stopping treatment.
If you have any other questions about the use of this medication, ask your doctor or pharmacist.
4. Possible Adverse Effects
Like all medicines, this medicine can cause adverse effects, although not all people suffer from them. Most adverse effects are mild to moderate. However, some can be serious and require treatment. Adverse effects may appear up to 4 months or more after the last injection of Hyrimoz.
Seek medical attention urgentlyif you notice any of the following signs of allergic reaction or heart failure:
- severe rash, hives;
- swelling of the face, hands, feet;
- difficulty breathing, swallowing;
- difficult breathing with physical activity or when lying down or swelling of feet.
Contact your doctor as soon as possibleif you notice any of the following effects:
- signs and symptoms of infection such as fever, nausea, wounds, dental problems, burning sensation when urinating, feeling of weakness, fatigue, or cough;
- symptoms of nervous system problems, such as tingling, numbness, double vision, weakness in arms or legs;
- signs of skin cancer, such as a lump or an open sore that does not heal;
- signs and symptoms of blood disorders such as persistent fever, bruising, bleeding, and paleness.
The following adverse effects have been observed with adalimumab:
Very Common(may affect more than 1 in 10 people)
- injection site reactions (including pain, swelling, redness, or itching);
- lower respiratory tract infections (including colds, runny nose, sinusitis, pneumonia);
- headache;
- abdominal pain (stomach);
- nausea and vomiting;
- rash;
- muscle pain.
Common(may affect up to 1 in 10 people)
- severe infections (including sepsis and flu);
- intestinal infections (including gastroenteritis);
- skin infections (including cellulitis and herpes);
- ear infection;
- mouth infections (including dental infection and cold sore);
- infections of the reproductive system;
- urinary tract infections;
- fungal infections;
- joint infections;
- benign tumors;
- skin cancer;
- allergic reactions (including seasonal allergy);
- dehydration;
- mood changes (including depression);
- anxiety;
- drowsiness and difficulty sleeping;
- sensory disturbances such as tingling, prickling, or numbness;
- migraine;
- symptoms of nerve root compression (including lower back pain and leg pain);
- visual disturbances;
- eye inflammation;
- eyelid inflammation and eye swelling;
- vertigo (feeling of spinning);
- feeling of rapid heartbeat;
- high blood pressure;
- flushing;
- bruises (solid swelling with clotted blood);
- cough;
- asthma;
- difficulty breathing;
- gastrointestinal bleeding;
- indigestion (heartburn, bloating, and discomfort);
- acid reflux;
- dry eye syndrome (including dryness in eyes and mouth);
- itching;
- itchy rash;
- bruises;
- skin inflammation (such as eczema);
- breaking of fingernails and toenails;
- increased sweating;
- hair loss;
- new or worsening psoriasis;
- muscle spasms;
- blood in urine;
- kidney problems;
- chest pain;
- edema (fluid accumulation in the body that can cause swelling of the affected tissue);
- fever;
- low platelet count in blood, which increases the risk of bleeding or bruising;
- wound healing problems.
Uncommon(may affect up to 1 in 100 people)
- unusual infections (including tuberculosis) and other infections that occur when disease resistance decreases;
- neurological infections (including viral meningitis);
- eye infections;
- bacterial infections;
- diverticulitis (inflammation and infection of the large intestine);
- cancer, including cancer that affects the lymphatic system (lymphoma) and melanoma (a type of skin cancer);
- immune system disorders that can affect the lungs, skin, and lymph nodes (the most common presentation is in the form of a disease called sarcoidosis);
- vasculitis (inflammation of blood vessels);
- tremors (feeling shaky);
- neuropathy (nerve damage);
- stroke;
- hearing loss, tinnitus;
- feeling of irregular heartbeat like skips;
- heart problems that can cause difficulty breathing or swelling of ankles;
- heart attack;
- aneurysm (balloon-like bulge in a major artery), inflammation, and clotting in a vein, blockage of a blood vessel;
- lung diseases that can cause difficulty breathing (including inflammation);
- pulmonary embolism (blockage of a lung artery);
- pleural effusion (abnormal fluid accumulation in the pleural space);
- pancreatitis (inflammation of the pancreas that causes severe abdominal and back pain);
- difficulty swallowing;
- facial edema (swelling);
- gallbladder inflammation; gallstones;
- fatty liver (fat accumulation in liver cells);
- night sweats;
- scars;
- abnormal muscle crisis;
- systemic lupus erythematosus (an immune system disorder that includes inflammation of the skin, heart, lungs, joints, and other organs);
- sleep disturbances;
- impotence;
- inflammations.
Rare(may affect up to 1 in 1,000 people)
- leukemia (cancer that affects the blood and bone marrow);
- severe allergic reaction with shock;
- multiple sclerosis;
- nerve disorders (such as optic neuritis of the eye and Guillain-Barré syndrome, a disease that can cause muscle weakness, abnormal sensations, tingling in the arms and upper body);
- cardiac arrest;
- pulmonary fibrosis (scarring in the lungs);
- intestinal perforation (hole in the intestinal wall);
- hepatitis (inflammation of the liver);
- reactivation of hepatitis B virus infection;
- autoimmune hepatitis (inflammation of the liver caused by the body's own immune system);
- cutaneous vasculitis (inflammation of blood vessels in the skin);
- Stevens-Johnson syndrome (a potentially life-threatening disease with flu-like symptoms and blistering rash);
- facial edema (swelling) associated with allergic reactions;
- erythema multiforme (inflammatory rash on the skin);
- lupus-like syndrome;
- angioedema (localized skin swelling);
- lichenoid reaction on the skin (purple-red rash with itching).
Frequency Not Known(cannot be estimated from the available data)
- hepatosplenic T-cell lymphoma (a rare and often fatal blood cancer);
- Merkel cell carcinoma (a type of skin cancer);
- Kaposi's sarcoma, a rare cancer related to human herpesvirus 8 infection. Kaposi's sarcoma usually manifests more frequently as purple-colored skin lesions;
- liver failure;
- worsening of a disease called dermatomyositis (seen as skin rash accompanied by muscle weakness);
- weight gain (for most patients, weight gain was reduced).
Some adverse effects observed in clinical studies with adalimumab do not have symptoms and can only be identified through a blood test. These include:
Very Common(may affect more than 1 in 10 people)
- low white blood cell count;
- low red blood cell count;
- high lipid levels in blood;
- high liver enzymes.
Common(may affect up to 1 in 10 people)
- high white blood cell count;
- low platelet count;
- high uric acid levels in blood;
- abnormal sodium levels in blood;
- low calcium levels in blood;
- low phosphate levels in blood;
- high blood sugar;
- high lactate dehydrogenase levels in blood;
- presence of autoantibodies in blood;
- low potassium levels in blood.
Uncommon(may affect up to 1 in 100 people)
- high bilirubin levels (liver function test).
Rare(may affect up to 1 in 1,000 people)
- low counts in blood for white blood cells, red blood cells, and platelets.
Reporting of Adverse Effects
If you experience any type of adverse effect, consult your doctor or pharmacist, even if it is a possible adverse effect that does not appear in this prospectus.
You can also report them directly through the national reporting system included in Appendix V. By reporting adverse effects, you can contribute to providing more information on the safety of this medicine.
5. Storage of Hyrimoz
Keep this medicine out of the sight and reach of children.
Do not use this medicine after the expiration date that appears on the label/blister/box after "CAD" or "EXP". The expiration date is the last day of the month indicated.
Store in a refrigerator (between 2 °C and 8 °C). Do not freeze.
Keep the pre-filled pen in the outer packaging to protect it from light.
Alternative storage:
When necessary (e.g., when traveling), you can store Hyrimoz at room temperature (up to 25 °C) for a maximum period of 42 days (make sure to protect it from light). Once the pre-filled pen is removed from the refrigerator to store at room temperature, it must be used within the next 42 days or discarded, even if it is later returned to the refrigerator. You must record the date you removed the pre-filled pen from the refrigerator and the date after which it must be discarded.
Medicines should not be disposed of via wastewater or household waste. Ask your pharmacist how to dispose of the packaging and medicines you no longer need. This will help protect the environment.
6. Package Contents and Additional Information
Hyrimoz Composition
- The active substance is adalimumab. Each pre-filled pen contains 80 mg of adalimumab in 0.8 ml of solution.
- The other components are: adipic acid, mannitol (E 421), polysorbate 80 (E 433), hydrochloric acid (E 507), sodium hydroxide (E 524), and water for injections (see section 2 "Hyrimoz contains sodium").
Product Appearance and Package Contents
Hyrimoz 80 mg solution for injection (injection) in a pre-filled pen is supplied as 0.8 ml of a clear to slightly opalescent, colorless or slightly yellowish solution.
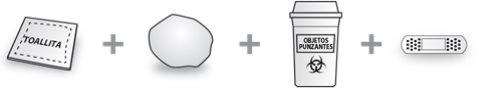
Hyrimoz is supplied in a single-use pre-filled syringe attached to a triangular-shaped pen with a transparent viewing window and label. The inner syringe of the pen is made of Type I glass with a stainless steel needle of 29 gauge and an inner needle cap made of rubber (thermoplastic elastomer), with 0.8 ml of solution.
Packs containing 1, 2, and 3 pre-filled pens of Hyrimoz.
Only some pack sizes may be marketed.
Hyrimoz is available in a pre-filled syringe and a pre-filled pen.
Marketing Authorization Holder
Sandoz GmbH
Biochemiestr. 10
6250 Kundl
Austria
Manufacturer
Sandoz GmbH Schaftenau
Biochemiestr. 10
6336 Langkampfen
Austria
Novartis Pharmaceutical Manufacturing GmbH
Biochemiestrasse 10
6336 Langkampfen
Austria
You can request more information about this medicinal product from the local representative of the marketing authorization holder:
België/Belgique/Belgien Sandoz nv/sa Tél/Tel: +32 2 722 97 97 | Lietuva Sandoz Pharmaceuticals d.d filialas Tel: +370 5 2636 037 |
| Luxembourg/Luxemburg Sandoz nv/sa (Belgique/Belgien) Tél/Tel.: +32 2 722 97 97 |
Ceská republika Sandoz s.r.o. Tel: +420 225 775 111 | Magyarország Sandoz Hungária Kft. Tel.: +36 1 430 2890 |
Danmark/Norge/Ísland/Sverige Sandoz A/S Tlf/Sími/Tel: +45 63 95 10 00 | Malta Sandoz Pharmaceuticals d.d. Tel: +356 21222872 |
Deutschland Hexal AG Tel: +49 8024 908 0 | Nederland Sandoz B.V. Tel: +31 36 52 41 600 |
Eesti Sandoz d.d. Eesti filiaal Tel: +372 665 2400 | Österreich Sandoz GmbH Tel: +43 5338 2000 |
Ελλάδα Novartis (Hellas) A.E.B.E. Τηλ: +30 210 281 17 12 | Polska Sandoz Polska Sp. z o.o. Tel.: +48 22 209 70 00 |
España Sandoz Farmacéutica, S.A. Tel: +34 900 456 856 | Portugal Sandoz Farmacêutica Lda. Tel: +351 21 196 40 00 |
France Sandoz SAS Tél: +33 1 49 64 48 00 | România Sandoz SRL Tel: +40 21 407 51 60 |
Hrvatska Sandoz d.o.o. Tel: +385 1 23 53 111 | Slovenija Lek farmacevtska družba d.d. Tel: +386 1 580 21 11 |
Ireland Rowex Ltd. Tel: + 353 27 50077 | Slovenská republika Sandoz d.d. - organizačná zložka Tel: +421 2 48 200 600 |
Italia Sandoz S.p.A. Tel: +39 02 96541 | Suomi/Finland Sandoz A/S Puh/Tel: +358 10 6133 400 |
Κύπρος SANDOZ HELLAS ΜΟΝΟΠΡΟΣΩΠΗ Α.Ε. (Ελλάδα) Τηλ: +30 216 600 5000 | United Kingdom (Northern Ireland) Sandoz GmbH Tel: +43 5338 2000 |
Latvija Sandoz d.d. Latvia filiale Tel: +371 67 892 006 |
Date of Last Revision of this Leaflet
Other Sources of Information
Detailed information on this medicinal product is available on the European Medicines Agency website: http://www.ema.europa.eu.
- Instructions for Use
To help avoid possible infections and ensure correct use of Hyrimoz, it is important that you follow these instructions.
Make sure you read, understand, and follow these instructions for use before injecting Hyrimoz. Your healthcare professional should have taught you how to prepare and inject Hyrimoz correctly with the Hyrimoz single-dose pre-filled pen before you use it for the first time. If you have any questions, consult your healthcare professional.
Your Hyrimoz Single-Use Pre-Filled Pen
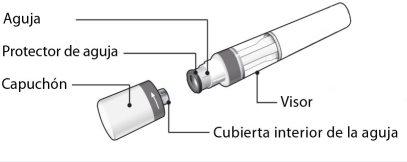
Figure A:parts of the Hyrimoz pen
In Figure A, the pen is shown with the cap removed. Do not remove the cap until you are ready to administer the injection.
It is Important That: |
|
Storage of the Pen |
Keep Hyrimoz and all medicines out of the reach of children. |
What You Need for Injection: |
Place the following items on a clean and flat surface. The carton includes:
The pen carton does not include (see Figure B):
Figure B:items not included in the carton |
Before Injection Preparing the Pen | |
If the syringe does not pass any of the above checks, contact your pharmacist. |
Figure C:safety checks before injection |
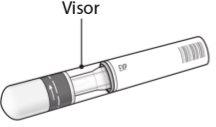
1. Choosing the Injection Site: | |
|
Figure D:choose the injection site |
| |
|
Figure E:clean the injection site |
| |
|
Figure F:remove the cap |
| |
|
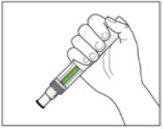
Figure G:hold the pen |
Injection |
Before Injection, Read the Following: During the injection, you will hear 2 loud clicks:
You must continue to hold the pen firmly against the skin until you see that a green indicatorfills the entire viewing window and stops moving. |
| |
|
Figure H:start the injection |
| |
|
Figure I:complete the injection |
After Injection | |
| |
You may see a small amount of blood at the injection site. You can press a cotton ball or gauze against the site for 10 seconds. Do not rub the injection site. If necessary, you can cover it with a small adhesive bandage. |
Figure J:check the green indicator |
| |
|
Figure K:disposal of used pen |
If you have any questions, consult a doctor, pharmacist, or nurse who is familiar with Hyrimoz.
- Country of registration
- Active substance
- Prescription requiredYes
- Manufacturer
- This information is for reference only and does not constitute medical advice. Always consult a doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to HYRIMOZ 80 mg SOLUTION FOR INJECTION IN A PRE-FILLED PENDosage form: INJECTABLE, 20 mgActive substance: adalimumabManufacturer: Amgen Europe B.V.Prescription requiredDosage form: INJECTABLE, 20 mgActive substance: adalimumabManufacturer: Amgen Europe B.V.Prescription requiredDosage form: INJECTABLE, 40 mgActive substance: adalimumabManufacturer: Amgen Europe B.V.Prescription required
Online doctors for HYRIMOZ 80 mg SOLUTION FOR INJECTION IN A PRE-FILLED PEN
Discuss questions about HYRIMOZ 80 mg SOLUTION FOR INJECTION IN A PRE-FILLED PEN, including use, safety considerations and prescription review, subject to medical assessment and local regulations.
Frequently Asked Questions