REMSIMA 120 mg SOLUTION FOR INJECTION IN PRE-FILLED PEN


How to use REMSIMA 120 mg SOLUTION FOR INJECTION IN PRE-FILLED PEN
Translated with AI
This page provides general information and does not replace a doctor’s consultation. Always consult a doctor before taking any medication. Seek urgent medical care if symptoms are severe.
Show originalContents of the leaflet
Introduction
Package Leaflet: Information for the User
Remsima 120 mg solution for injection in pre-filled pen
infliximab
Read all of this leaflet carefully before you start using this medicine because it contains important information for you.
- Keep this leaflet, you may need to read it again.
- Your doctor will also give you a patient information card, which contains important safety information that you need to know before and during treatment with Remsima.
- When you start a new card, keep this card as a reference for 4 months after your last dose of Remsima.
- If you have any further questions, ask your doctor, pharmacist, or nurse.
- This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours.
- If you get any side effects, talk to your doctor, pharmacist, or nurse. This includes any possible side effects not listed in this leaflet. See section 4.
Contents of the pack
- What is Remsima and what is it used for
- What you need to know before you use Remsima
- How to use Remsima
- Possible side effects
- Storing Remsima
- Contents of the pack and other information
- Instructions for use
1. What is Remsima and what is it used for
Remsima contains the active substance infliximab. Infliximab is a monoclonal antibody – a type of protein that binds to a specific target in the body called TNF (tumor necrosis factor) alpha.
Remsima belongs to a group of medicines called “TNF blockers”. It is used in adults for the following inflammatory diseases:
- Rheumatoid arthritis.
- Psoriatic arthritis
- Ankylosing spondylitis (Bechterew's disease)
- Psoriasis
- Crohn's disease
- Ulcerative colitis.
Remsima works by selectively binding to TNF alpha and blocking its action. TNF alpha is involved in the body's inflammatory processes, so blocking it can reduce inflammation in your body.
Rheumatoid Arthritis
Rheumatoid arthritis is an inflammatory disease of the joints. If you have active rheumatoid arthritis, you will first be given other medicines. If these medicines do not work well enough, you will be given Remsima with another medicine called methotrexate to:
- reduce the signs and symptoms of your disease,
- slow down the damage to your joints,
- improve your physical function.
Psoriatic Arthritis
Psoriatic arthritis is an inflammatory disease of the joints, usually accompanied by psoriasis. If you have active psoriatic arthritis, you will first be given other medicines. If these medicines do not work well enough, you will be given Remsima to:
- reduce the signs and symptoms of your disease,
- reduce the damage to your joints,
- improve your physical function.
Ankylosing Spondylitis (Bechterew's Disease)
Ankylosing spondylitis is an inflammatory disease of the spine. If you have ankylosing spondylitis, you will first be given other medicines. If these medicines do not work well enough, you will be given Remsima to:
- reduce the signs and symptoms of your disease,
- improve your physical function.
Psoriasis
Psoriasis is an inflammatory disease of the skin. If you have moderate to severe plaque psoriasis, you will first be given other medicines or treatments such as phototherapy. If these medicines or treatments do not work well enough, you will be given Remsima to reduce the signs and symptoms of your disease.
Ulcerative Colitis
Ulcerative colitis is an inflammatory disease of the intestine. If you have ulcerative colitis, you will first be given other medicines. If these medicines do not work well enough, you will be given Remsima to treat your disease.
Crohn's Disease
Crohn's disease is an inflammatory disease of the intestine. If you have Crohn's disease, you will first be given other medicines. If these medicines do not work well enough, you will be given Remsima to:
- treat active Crohn's disease,
- reduce the number of abnormal connections (fistulas) between your intestine and your skin, that have not been controlled by other medicines or surgery.
2. What you need to know before you use Remsima
You must not use Remsima if:
- you are allergic to infliximab or any of the other ingredients of Remsima (listed in section 6),
- you are allergic to proteins that come from mice,
- you have tuberculosis (TB) or another serious infection such as pneumonia or sepsis (serious bacterial infection of the blood),
- you have a moderate or severe heart failure.
If any of the above applies to you, do not use Remsima. If you are not sure, consult your doctor before you are given Remsima.
Warnings and precautions
Consult your doctor before or during treatment with Remsima if:
You have previously received treatment with any medicine that contains infliximab
- Tell your doctor if you have received treatment with medicines that contain infliximab in the past and now start a new treatment with Remsima.
- If you have interrupted treatment with infliximab for more than 16 weeks, there is a higher risk of allergic reactions when you start treatment again.
Local reactions at the injection site
- Some patients who receive infliximab by injection under the skin have experienced local reactions at the injection site. The signs of a local reaction at the injection site may include redness, pain, itching, swelling, hardening, bruising, bleeding, feeling of cold, feeling of tingling, irritation, rash, ulcer, nodules, blisters, and scabs on the skin at the injection site.
- Most of these reactions are mild to moderate and most resolve on their own within a day.
Infections
- Before you are given Remsima, tell your doctor if you have an infection, even if it is minor.
- Before you are given Remsima, tell your doctor if you have ever lived or traveled to a place where infections such as histoplasmosis, coccidioidomycosis, or blastomycosis are common. These infections are caused by specific types of fungi that can affect the lungs or other parts of your body.
- You may be more likely to get infections when you are being treated with Remsima. If you are 65 years of age or older, you have a higher risk.
- These infections can be serious and include tuberculosis, infections caused by viruses, fungi, bacteria, or other organisms in the environment, and sepsis, which can be life-threatening.
Tell your doctor immediately if you notice signs of infection during treatment with Remsima, such as fever, cough, flu-like symptoms, general feeling of being unwell, redness or feeling of warmth on the skin, wounds, or dental problems. Your doctor may recommend temporarily stopping treatment with Remsima.
Tuberculosis (TB)
- It is very important that you tell your doctor if you have ever had TB or if you have been in close contact with someone who has had or has TB.
- Your doctor will perform a test to see if you have TB. Cases of TB have been reported in patients treated with infliximab, even in patients who have been treated with medicines for TB. Your doctor will record these tests on your patient information card.
- If your doctor thinks you are at risk of getting TB, you may be treated with medicines for TB before you are given Remsima.
Tell your doctor immediately if you notice signs of TB during treatment with Remsima. The signs include persistent cough, weight loss, feeling of tiredness, fever, night sweats.
Hepatitis B virus
- Before you use Remsima, tell your doctor if you are a carrier of hepatitis B or if you have had it in the past.
- Tell your doctor if you think you may be at risk of getting hepatitis B.
- Your doctor should perform tests for the hepatitis B virus.
- Treatment with TNF blockers, such as Remsima, may cause reactivation of the hepatitis B virus in patients who are carriers of this virus, which in some cases can be life-threatening.
- If you experience reactivation of hepatitis B, your doctor may need to stop your treatment and may give you medicines such as antiviral therapy with supportive treatment.
Heart problems
- Tell your doctor if you have any heart problems, such as mild heart failure.
- Your doctor will want to keep a close eye on your heart.
Tell your doctor immediately if you notice signs of new or worsening heart failure during treatment with Remsima. The signs include difficulty breathing or swelling of the feet.
Cancer and lymphoma
- Before you are given Remsima, tell your doctor if you have or have ever had lymphoma (a type of blood cancer) or any other cancer.
- Patients with severe rheumatoid arthritis who have had the disease for a long time may have a higher risk of developing lymphoma.
- Patients treated with Remsima may have a higher risk of developing lymphoma or other types of cancer.
- Some patients who have received TNF blockers, including infliximab, have developed a rare type of cancer called hepatosplenic T-cell lymphoma. Most of these patients were adolescent or young adult males and most had Crohn's disease or ulcerative colitis. This type of cancer is usually fatal. Almost all of these patients had also received medicines containing azathioprine or 6-mercaptopurine, in addition to TNF blockers.
- Some patients treated with infliximab have developed certain types of skin cancer. Tell your doctor if you notice any changes in your skin or growths on your skin during or after treatment.
- Some women treated with infliximab for rheumatoid arthritis have developed cervical cancer. Women treated with Remsima, even those over 60 years of age, may be recommended regular cervical cancer screening by their doctor.
Lung disease or heavy smoking
- Before you are given Remsima, tell your doctor if you have a lung disease called chronic obstructive pulmonary disease (COPD) or if you are a heavy smoker.
- Patients with COPD and patients who are heavy smokers may have a higher risk of developing cancer with treatment with Remsima.
Nervous system disease
- Tell your doctor if you have or have ever had a problem that affects your nervous system before you are given Remsima. This includes multiple sclerosis, Guillain-Barré syndrome, if you have had seizures or have been diagnosed with “optic neuritis”.
Tell your doctor immediately if you notice symptoms of nervous system disease during treatment with Remsima. The symptoms can be changes in vision, weakness in the arms or legs, numbness or tingling in any part of the body.
Abnormal skin openings
- Consult your doctor if you have any abnormal skin openings (fistulas) before you are given Remsima.
Vaccines
- Consult your doctor if you have recently had or are scheduled to have a vaccine.
- Before you start treatment with Remsima, you should receive all recommended vaccines. You can receive some vaccines during treatment with Remsima but you must not receive live vaccines (vaccines that contain a live but weakened infectious agent) while you are using Remsima because they may cause infections. If you received Remsima while you were pregnant, your baby may also have a higher risk of getting an infection as a result of receiving a live vaccine during the first year of life. It is important that you inform your baby's doctors and other healthcare professionals about your treatment with Remsima so that they can decide when your baby can be vaccinated, including live vaccines such as the BCG vaccine (used to prevent tuberculosis).
- If you are breastfeeding, it is important that you inform your baby's doctors and other healthcare professionals about your treatment with Remsima before your baby is vaccinated.
For more information, see the section on Pregnancy and breastfeeding
Therapeutic infectious agents
- Tell your doctor if you have recently received or are scheduled to receive treatment with an infectious agent (such as a BCG instillation used for cancer treatment).
Surgery or dental procedures
- Tell your doctor if you are going to have any surgery or dental procedure.
- Tell your surgeon or dentist that you are being treated with Remsima and show them your patient information card.
Liver problems
- Some patients who received Remsima have developed serious liver problems.
- Tell your doctor immediately if you notice symptoms of liver problems during treatment with Remsima. The symptoms can be yellowing of the skin and eyes, dark brown urine, pain or swelling in the upper right side of the stomach, joint pain, skin rash, or fever.
Low blood cell counts
- In some patients who receive Remsima, the body cannot produce enough blood cells that help fight infections or help stop bleeding.
- Tell your doctor immediately if you notice symptoms of low blood cell counts during treatment with Remsima. The symptoms can be persistent fever, bleeding or bruising easily, small red or purple spots caused by bleeding under the skin, or paleness.
Immune system disorder
- Some patients who received Remsima have developed symptoms of an immune system disorder called lupus.
- Tell your doctor immediately if you develop symptoms of lupus during treatment with Remsima. The symptoms can be joint pain or a rash on the cheeks or arms due to sun sensitivity.
Children and adolescents
Do not give this medicine to children and adolescents under 18 years of age as there are no data to demonstrate that this medicine is safe and effective in this age group.
Other medicines and Remsima
Patients with inflammatory diseases are already taking medicines to treat their condition. These medicines may cause side effects. Your doctor will advise you which other medicines you should continue to use while you are being treated with Remsima.
Tell your doctor if you are using, have recently used, or might use any other medicines, including any other medicines for the treatment of Crohn's disease, ulcerative colitis, rheumatoid arthritis, ankylosing spondylitis, psoriatic arthritis, or psoriasis, or medicines that you can buy without a prescription, such as vitamins or herbal remedies.
In particular, tell your doctor if you are using any of the following medicines:
- Medicines that affect your immune system.
- Kineret (which contains anakinra). Remsima and Kineret must not be used at the same time.
- Orencia (which contains abatacept). Remsima and Orencia must not be used at the same time.
You must not receive live vaccines while you are using Remsima. If you were using Remsima during pregnancy or if you are receiving Remsima during breastfeeding, inform your baby's doctor and other healthcare professionals about your treatment with Remsima before your baby receives any vaccine.
If you are not sure if any of the above applies to you, consult your doctor, pharmacist, or nurse before you start using Remsima.
Pregnancy, breastfeeding, and fertility
- If you are pregnant or breastfeeding, think you may be pregnant, or are planning to have a baby, ask your doctor for advice before using this medicine. Remsima should only be used during pregnancy or breastfeeding if your doctor thinks it is necessary for you.
- You should avoid becoming pregnant while you are being treated with Remsima and for 6 months after treatment has finished. Discuss the use of contraceptive measures during this time with your doctor.
- If you received Remsima during pregnancy, your baby may have a higher risk of getting an infection.
- It is important that you inform your baby's doctors and other healthcare professionals about your treatment with Remsima before your baby is vaccinated. If you received Remsima while you were pregnant, giving the BCG vaccine (used to prevent tuberculosis) to your baby within 12 months after birth may cause serious infections, including death. Live vaccines, such as the BCG vaccine, must not be given to your baby within 12 months after birth unless your baby's doctor recommends otherwise. For more information, see the section on vaccines.
- If you are breastfeeding, it is important that you inform your baby's doctors and other healthcare professionals about your treatment with Remsima before your baby is vaccinated. Live vaccines must not be given to your baby while you are breastfeeding unless your baby's doctor recommends otherwise.
- In children born to women treated with infliximab during pregnancy, a serious decrease in the number of white blood cells in the blood has been reported. If your baby has fevers or infections, contact your baby's doctor immediately.
Driving and using machines
Remsima is unlikely to affect your ability to drive or use tools or machines. If you feel tired, dizzy, or unwell after you are given Remsima, do not drive or use tools or machines.
Remsima contains sodium and sorbitol
This medicine contains less than 1 mmol of sodium (23 mg) per dose, which is essentially “sodium-free” and 45 mg of sorbitol in each 120 mg dose.
3. How Remsima will be administered to you
Follow exactly the administration instructions of this medicine indicated by your doctor.
In case of doubt, consult your doctor again.
Rheumatoid Arthritis
Your doctor will start your treatment with or without two intravenous infusions of Remsima at 3 mg per kilogram of body weight (administered in a vein, usually in the arm, over a period of 2 hours). If Remsima subcutaneous injection doses are administered to initiate treatment, Remsima 120 mg should be administered as a subcutaneous injection followed by additional subcutaneous injections at 1, 2, 3, and 4 weeks after the first injection, and from then on, every 2 weeks. The usual recommended dose of Remsima subcutaneous injection is 120 mg every 2 weeks, regardless of body weight.
Psoriatic Arthritis, Ankylosing Spondylitis (Bechterew's disease), and Psoriasis
Your doctor will start your treatment with two intravenous infusions of Remsima at 5 mg per kilogram of body weight (administered in a vein, usually in the arm, over a period of 2 hours). They are administered with a 2-week difference through intravenous infusion. After 4 weeks from the last intravenous infusion, you will be administered Remsima through a subcutaneous injection (under the skin).
The usual recommended dose of Remsima subcutaneous injection is 120 mg every 2 weeks, regardless of body weight.
Crohn's Disease and Ulcerative Colitis
Your doctor will start your treatment with two or three intravenous infusions of Remsima at 5 mg per kilogram of body weight (administered in a vein, usually in the arm, over a period of 2 hours). They are administered with a 2-week difference through intravenous infusion and may be administered with an additional intravenous infusion 4 weeks after the second infusion for patients with Crohn's disease and ulcerative colitis at the discretion of your doctor to initiate treatment with Remsima. After 4 weeks from the last intravenous infusion, you will be administered Remsima through a subcutaneous injection (under the skin).
The usual recommended dose of Remsima subcutaneous injection is 120 mg every 2 weeks, regardless of body weight.
How Remsima will be administered to you
- Remsima 120 mg injectable solution is administered through subcutaneous injection (under the skin) only. It is essential to consult the product labels to ensure that the correct formulation is being administered according to the prescription.
- For patients with rheumatoid arthritis, your doctor may initiate treatment with Remsima with or without two intravenous infusions of Remsima. For patients with Crohn's disease, ulcerative colitis, ankylosing spondylitis, psoriatic arthritis, or psoriasis, two infusions of Remsima will be administered to initiate treatment with Remsima. For patients with Crohn's disease or ulcerative colitis, two or three intravenous infusions of infliximab will be administered to initiate treatment with Remsima.
- For patients with rheumatoid arthritis, if treatment is initiated with Remsima without two intravenous infusions of Remsima, the following table indicates the frequency at which Remsima 120 mg will normally be administered subcutaneously after the first dose.
2nd dose | 1 week after the 1st dose |
3rd dose | 2 weeks after the 1st dose |
4th dose | 3 weeks after the 1st dose |
5th dose | 4 weeks after the 1st dose |
Other doses | 6 weeks after the 1st dose and then every 2 weeks |
- Your doctor or nurse will administer the intravenous infusions of infliximab with a 2-week difference, and an additional intravenous infusion may be administered 4 weeks after the second infusion for patients with Crohn's disease and ulcerative colitis at the discretion of your doctor to initiate treatment with Remsima. The first subcutaneous injection of Remsima will be administered 4 weeks after the last intravenous infusion, followed by subcutaneous injections of Remsima administered every 2 weeks.
- The first subcutaneous injection of Remsima will be administered under the supervision of your doctor.
- After adequate training, if you feel well-trained and confident to inject Remsima yourself, your doctor may allow you to inject the following doses of Remsima at home.
- Talk to your doctor if you have any questions about how to administer an injection yourself. You will find detailed "Instructions for use" at the end of the leaflet.
If you use more Remsima than you should
If you have used more Remsima than you should (either by injecting too much at one time or using it too frequently), talk to a doctor, pharmacist, or nurse immediately. Always carry the medicine packaging with you, even if it is empty.
If you forget to use Remsima
Missed dose up to 7 days
If you miss a dose of Remsima up to 7 days after the originally scheduled dose, you should take the missed dose immediately. Take the next dose on the originally planned date and then follow the original dosing schedule.
Missed dose for 8 or more days
If you miss a dose of Remsima 8 or more days after the originally scheduled dose, you should not take the missed dose. Take the next dose on the originally planned date and then follow the original dosing schedule.
If you are unsure when to inject Remsima, call your doctor.
If you have any other questions about the use of this medicine, consult your doctor, pharmacist, or nurse.
4. Possible side effects
Like all medicines, this medicine can cause side effects, although not everybody gets them. Most side effects are mild to moderate. However, some patients may experience serious side effects and may require treatment. Side effects can also occur after your treatment with Remsima has finished.
Inform your doctor immediately if you notice any of the following:
- Signs of an allergic reactionsuch as swelling of the face, lips, mouth, or throat, which can cause difficulty swallowing or breathing, skin rash, hives, swelling of the hands, feet, or ankles. Some of these reactions can be serious or potentially life-threatening. An allergic reaction can occur within 2 hours of your injection or later. Other allergic side effects can occur up to 12 days after your injection, such as muscle pain, fever, joint pain, or jaw pain, sore throat, or headache.
- Signs of a local reaction at the injection sitesuch as redness, pain, itching, swelling, hardening, bruising, bleeding, feeling of cold, tingling sensation, irritation, rash, ulcer, nodules, blisters, and crusts.
- Signs of a heart problemsuch as chest pain or discomfort, arm pain, stomach pain, difficulty breathing, anxiety, dizziness, fainting, sweating, nausea (feeling sick), vomiting, palpitations or pounding in the chest, fast or slow heartbeat, and swelling of the feet.
- Signs of infection (including TB)such as fever, fatigue, persistent cough, difficulty breathing, flu-like symptoms, weight loss, night sweats, diarrhea, wounds, accumulation of pus in the abdomen or around the anus (abscess), dental problems, or a burning sensation when urinating.
- Possible signs of cancerincluding, but not limited to, swelling of the lymph nodes, weight loss, fever, rare skin nodules, changes in moles or skin color, or unusual vaginal bleeding.
- Signs of a lung problemsuch as cough, difficulty breathing, or chest tightness.
- Signs of a nervous system problem (including eye problems)such as signs of a stroke (sudden numbness or weakness of your face, arm, or leg, especially on one side of your body; sudden confusion, difficulty speaking or understanding; difficulty seeing with one or both eyes, difficulty walking, dizziness, loss of balance or coordination, or a severe headache), seizures, numbness/tingling in any part of the body, or weakness in arms or legs, vision changes such as double vision or other eye problems.
- Signs of a liver problem(including hepatitis B infection when you have had hepatitis B before) such as yellowing of the skin and eyes, dark brown urine, pain or swelling in the upper right part of the stomach, joint pain, skin rash, or fever.
- Signs of an immune system disordersuch as joint pain or a sun-sensitive rash on the cheeks or arms (lupus) or cough, difficulty breathing, fever, or skin rash (sarcoidosis).
- Signs of low blood cell countssuch as persistent fever, bleeding or bruising easily, small red or purple spots caused by bleeding under the skin, or paleness.
- Signs of serious skin problemssuch as red or circular patches on the skin, often with central blisters on the trunk, large areas of peeling skin, ulcers in the mouth, throat, nose, genitals, and eyes, or small pus-filled bumps that can spread across the body. These skin reactions can be accompanied by fever.
Inform your doctor immediately if you notice any of the above.
The following side effects have been observed with Remsima:
Very common:may affect more than 1 in 10 people
- Stomach pain, nausea
- Viral infections such as herpes or flu
- Upper respiratory tract infections such as sinusitis
- Headache
- Injection site reaction
- Pain.
Common:may affect up to 1 in 10 people
- Changes in liver function, increased liver enzymes (shown in blood tests)
- Lung or chest infections, such as bronchitis or pneumonia
- Difficult or painful breathing, chest pain
- Bleeding in the stomach or intestines, diarrhea, indigestion, heartburn, constipation
- Hives (nettle rash), itchy skin rash, dry skin
- Balance or dizziness problems
- Fever, increased sweating
- Circulation problems such as low or high blood pressure
- Bruising, flushing, or nosebleeds
- Feeling tired or weak
- Bacterial infections such as septicemia, abscess, or skin infection (cellulitis)
- Fungal skin infection
- Blood problems such as anemia or low white blood cell count
- Swollen lymph nodes
- Depression, sleep problems
- Eye problems, including red eyes and infections
- Fast heartbeat (tachycardia) or palpitations
- Joint, muscle, or back pain
- Urinary tract infection
- Psoriasis, skin problems such as eczema, and hair loss
- Injection site reactions such as pain, swelling, redness, or itching
- Chills, fluid accumulation under the skin causing swelling
- Feeling of numbness or tingling.
Uncommon:may affect up to 1 in 100 people
- Lack of blood flow, vein swelling
- Blood accumulation outside blood vessels (hematoma) or bruising
- Skin problems such as blisters, warts, abnormal skin color or pigmentation, or swollen lips, or thickened skin, or redness, scaly and peeling skin
- Severe allergic reactions (e.g., anaphylaxis), immune system disorder called lupus, allergic reactions to foreign proteins
- Slow-healing wounds
- Liver inflammation (hepatitis) or gallbladder inflammation, liver damage
- Feeling forgetful, irritable, confused, nervous
- Eye problems, including blurred or reduced vision, or swollen or inflamed eyes
- Heart problems or worsening of existing heart problems, decreased heart rate
- Fainting
- Seizures, nerve problems
- Intestinal ulcers or obstruction, stomach pain or cramps
- Pancreas inflammation (pancreatitis)
- Fungal infections such as Candida or fungal nail infection
- Lung problems (such as edema)
- Fluid around the lungs (pleural effusion)
- Narrowing of the airways in the lungs, causing difficulty breathing
- Inflammation of the membrane that protects the lung, causing severe chest pain that worsens with breathing (pleurisy)
- Tuberculosis
- Kidney infections
- Low platelet count, too many white blood cells in the blood, bruising, or black and blue marks
- Vaginal infections
- Blood test results showing "antibodies" against your own body
- Changes in cholesterol and fat levels in the blood
- Weight gain (for most patients, the weight gain was small)
Rare:may affect up to 1 in 1,000 people
- A type of blood cancer (lymphoma)
- Your blood not providing enough oxygen to your body, circulation problems such as narrowing of a blood vessel
- Inflammation of the membranes that protect the brain (meningitis)
- Infections due to a weakened immune system
- Hepatitis B infection when you have had hepatitis B before
- Liver inflammation caused by an immune system problem (autoimmune hepatitis)
- Liver problem that causes yellowing of the skin and eyes (jaundice)
- Swelling or abnormal growth of tissues
- Severe allergic reaction that can cause loss of consciousness and can be life-threatening (anaphylactic shock)
- Inflammation of small blood vessels (vasculitis)
- Immune system disorders that can affect the lungs, skin, and lymph nodes (such as sarcoidosis)
- Accumulation of immune cells as a result of an inflammatory response (granulomatous lesions)
- Lack of interest or emotion
- Serious skin problems such as toxic epidermal necrolysis, Stevens-Johnson syndrome, and acute generalized exanthematous pustulosis
- Other skin problems such as erythema multiforme, blisters, and skin peeling, or boils (furunculosis)
- Severe nervous system problems such as transverse myelitis, multiple sclerosis-like disease, optic neuritis, and Guillain-Barré syndrome
- Inflammation in the eye that can cause changes in vision, including blindness
- Fluid in the membrane that protects the heart (pericardial effusion)
- Serious lung problems (such as interstitial lung disease)
- Melanoma (a type of skin cancer)
- Cervical cancer
- Low blood cell counts, including a severe decrease in the number of white blood cells in the blood
- Small red or purple spots caused by bleeding under the skin
- Abnormal blood test results showing "complement factor" that is part of the immune system
- Lichenoid reactions (itchy red-purple rash and/or thick grayish-white lines on the mucous membranes)
Frequency not known:cannot be estimated from the available data
- Cancer
- A rare blood cancer that mainly affects young men (hepatosplenic T-cell lymphoma)
- Liver failure
- Merkel cell carcinoma (a type of skin cancer)
- Kaposi's sarcoma, a rare cancer related to human herpesvirus 8 infection. Kaposi's sarcoma usually occurs more frequently as purple skin lesions
- Worsening of a disease called dermatomyositis (manifested as a skin rash accompanied by muscle weakness)
- Heart attack
- Stroke
- Temporary loss of vision during or within 2 hours of infusion
- Infection due to a live vaccine because of a weakened immune system
Reporting of side effects
If you experience any side effects, talk to your doctor, pharmacist, or nurse, even if it is possible side effects not listed in this leaflet. You can also report them directly through the national reporting system included in Appendix V.
By reporting side effects, you can help provide more information on the safety of this medicine.
5. Storage of Remsima
- Keep this medicine out of the sight and reach of children.
- Do not use this medicine after the expiry date that appears on the label and carton after EXP. The expiry date is the last day of the month indicated.
- Store in a refrigerator (between 2°C and 8°C). Do not freeze. Keep the medicine in the original packaging to protect it from light.
- This medicine can also be stored in the original carton outside the refrigerator at up to 25°C for a single period of up to 28 days, but not beyond the initial expiry date. In this situation, it must not be refrigerated again. Write the new expiry date on the carton, including day/month/year. Discard this medicine if it has not been used by the new expiry date or the expiry date printed on the carton, whichever is earlier.
- Medicines should not be disposed of via wastewater or household waste. Ask your pharmacist how to dispose of the packaging and any unused medicine. This will help protect the environment.
6. Container Contents and Additional Information
Remsima Composition
- The active ingredient is infliximab. Each 1 ml pre-filled syringe contains 120 mg of infliximab.
- The other components are acetic acid, sodium acetate trihydrate, sorbitol, polysorbate 80, and water for injectable preparations.
Product Appearance and Container Contents
Remsima is a transparent to opalescent, colorless to pale brown solution presented in a single-use pre-filled pen.
Each container contains 1 pre-filled pen with 2 alcohol-impregnated wipes, 2 pre-filled pens with 2 alcohol-impregnated wipes, 4 pre-filled pens with 4 alcohol-impregnated wipes, or 6 pre-filled pens with 6 alcohol-impregnated wipes.
Not all pack sizes may be marketed.
Marketing Authorization Holder
Celltrion Healthcare Hungary Kft.
1062 Budapest
Váci út 1-3. WestEnd Office Building B torony
Hungary
Manufacturer
Millmount Healthcare Ltd.
Block 7
City North Business Campus
Stamullen, Co. Meath K32 YD60
Ireland
Nuvisan GmbH
Wegenerstraße 13,
89231 Neu Ulm,
Germany
Nuvisan France SARL
2400, Route des Colles,
06410, Biot,
France
Kymos, SL
Ronda De Can Fatjó 7B, Parc Tecnològic del Vallès,
Cerdanyola del Vallès,
Barcelona, 08290, Spain
Midas PharmaGmbH
Rheinstraße 49
55218 Ingelheim am Rhein
Germany
You can request more information about this medicinal product by contacting the local representative of the marketing authorization holder:
België/Belgique/Belgien Celltrion Healthcare Belgium BVBA Tél/Tel: + 32 1528 7418 | Lietuva Celltrion Healthcare Hungary Kft. 1062 Budapest Váci út 1-3. WestEnd Office Building B torony Hungary |
| Luxembourg/Luxemburg Celltrion Healthcare Belgium BVBA Tél/Tel: + 32 1528 7418 |
Ceská republika Celltrion Healthcare Hungary Kft. 1062 Budapest Váci út 1-3. WestEnd Office Building B torony Hungary | Magyarország Celltrion Healthcare Hungary Kft. 1062 Budapest Váci út 1-3. WestEnd Office Building B torony Hungary |
Danmark Celltrion Healthcare Denmark ApS Fuglevangsvej 11, 1962 Frederiksberg C, Denmark Tlf: +45 3535 2989 | Malta Mint Health Ltd. Tel: +356 2093 9800 |
Deutschland Celltrion Healthcare Deutschland GmbH Tel: + 49 (0)30 346494150 | Nederland Celltrion Healthcare Netherlands B.V. Tel: + 31 20 888 7300 |
Eesti Celltrion Healthcare Hungary Kft. 1062 Budapest Váci út 1-3. WestEnd Office Building B torony Hungary | Norge Celltrion Healthcare Norway AS Fjordalléen 16, 0250 Oslo, Norway [email protected] |
Ελλ?δα ΒΙΑΝΕΞ Α.Ε. Τηλ: +30 210 8009111 – 120 | Österreich Astro-Pharma GmbH Tel: +43 1 97 99 860 |
España KERN PHARMA, S.L. Tel: +34 93 700 25 25 | Polska Celltrion Healthcare Hungary Kft. 1062 Budapest Váci út 1-3. WestEnd Office Building B torony Hungary |
France Celltrion Healthcare France SAS Tél: + 33 (0)1 71 25 27 00 | Portugal Celltrion Portugal, Unipessoal Lda. Tel: + 351 21 936 8542 |
Hrvatska OKTAL PHARMA d.o.o. Tel: +385 1 6595 777 | România Celltrion Healthcare Hungary Kft. 1062 Budapest Váci út 1-3. WestEnd Office Building B torony Hungary |
Ireland Celltrion Healthcare Ireland Limited Tel: +353 1 223 4026 | Slovenija OKTAL PHARMA d.o.o. Tel: +386 1 519 29 22 |
Ísland Vistor hf. Sími: +354 535 7000 | Slovenská republika Celltrion Healthcare Hungary Kft. 1062 Budapest Váci út 1-3. WestEnd Office Building B torony Hungary |
Italia Celltrion Healthcare Italy S.r.l. Via Luigi Galvani, 24 - 20124 Milano (MI) Tel: +39 0247 927040 | Suomi/Finland Celltrion Healthcare Finland Oy. Puh/Tel: +358 29 170 7755 |
Κ?προς C.A. Papaellinas Ltd Τηλ: + 357 22741741 | Sverige Celltrion Sweden AB Tel: +46 8 80 11 77 [email protected] |
Latvija Celltrion Healthcare Hungary Kft. 1062 Budapest Váci út 1-3. WestEnd Office Building B torony Hungary |
Date of Last Revision of this Leaflet: {MM/AAAA}
Other Sources of Information
Detailed information on this medicinal product is available on the European Medicines Agency website: http://www.ema.europa.eu.
The leaflet for this medicinal product can be found on the European Medicines Agency website in all languages of the European Union/European Economic Area.
- Instructions for Use
Read these instructions carefully before using the Remsima pen. Consult your healthcare professional if you have questions about using the Remsima pen.
Important Information
- Use the pen ONLYif your healthcare professional has trained you in the correct way to prepare and administer an injection.
- Ask your healthcare professional how often you will need to administer an injection.
- Rotate the injection site each time you administer an injection. Each new injection site should be at least 3 cm from the previous injection site.
- Do notuse the pen if it has been dropped or if it is visibly damaged. A damaged pen may not function properly.
- Do notreuse the pen.
- Do notshake the pen at any time.
About the Remsima Pen
Parts of the Pen (see Figure A):
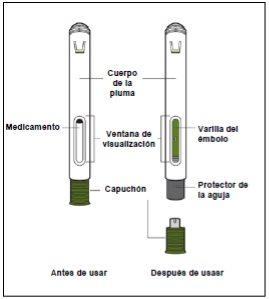
Figure A
- Do notremove the cap until you are ready to administer the injection. Once you remove the cap, do notrecap the pen.
Preparation for Injection
- Gather the supplies for the injection.
- Prepare a clean and flat surface, such as a table or countertop, in a well-lit area.
- Remove the pen from the refrigerator.
- Make sure you have the following supplies:
- Pen
- Alcohol swab
- Cotton ball or gauze*
- Adhesive bandage*
- Sharps disposal container*
*Items not included in the box.
- Inspect the pen.
Do notuse the pen if:
- It is cracked or damaged.
- The expiration date has passed.
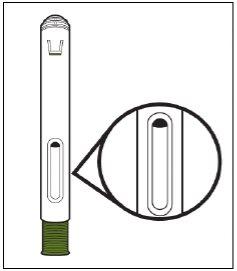
- Inspect the medicine (see Figure B).
The liquid should be transparent, colorless to pale brown. Do notuse the pen if the liquid is cloudy or discolored, or if it contains particles. Note: You may see bubbles in the liquid. This is normal |
Figure B |
- Wait 30 minutes.
- Let the pen come to room temperature for 30 minutes to allow it to warm up naturally.
Do notheat the pen using heat sources, such as warm water or a microwave.
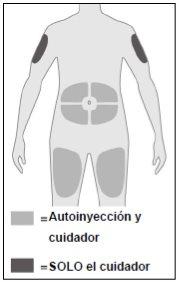
- Choose an injection site (see Figure C).
You can administer the injection in the following areas:
DO NOTadminister the injection in skin that is less than 5 cm from the navel, or that is sensitive, damaged, bruised, or scarred. Note: Rotate the injection site each time you administer an injection. Each new injection site should be at least 3 cm from the previous injection site. |
Figure C |
- Wash your hands.
- Wash your hands with soap and water, and dry them well.
- Clean the injection site.
- Clean the injection site with an alcohol swab.
- Let the skin dry before administering the injection.
Do notblow or touch the injection site before administering the injection.
Administer the Injection
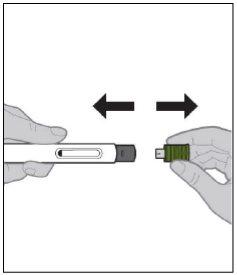
- Remove the cap (see Figure D).
Do nottouch the needle protector. If you do, you may cause a needlestick injury. |
Figure D |
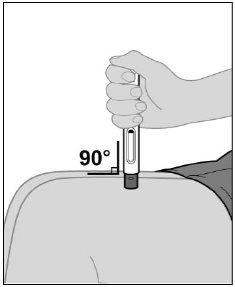
- Place the pen on the injection site (see Figure E).
|
Figure E |
- Start the injection (see Figure F).
Note: When you start the injection, you will hear the first click and the green olive plunger rod will start to fill the window.
|
Figure F |
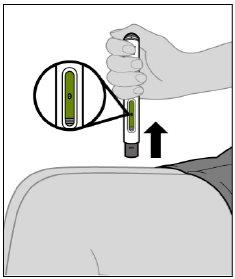
- Finish the injection (see Figure G).
|
Figure G |
- Remove the pen from the injection site.
Do notrub the injection site. Note: After removing the pen from the injection site, the needle will automatically cover (see Figure I). Note: If the green olive plunger rod does not fill the window completely, you will not receive the full dose. Do not reuse the pen in this case. Call your healthcare provider immediately. |
Figure H |
Figure I |
After the Injection
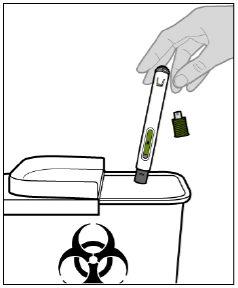
- Dispose of the pen (see Figure J).
Do notrecap the pen. Note: Keep the pen and the sharps disposal container out of the sight and reach of children. |
Figure J |
- Country of registration
- Active substance
- Prescription requiredYes
- Manufacturer
- This information is for reference only and does not constitute medical advice. Always consult a doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to REMSIMA 120 mg SOLUTION FOR INJECTION IN PRE-FILLED PENDosage form: INJECTABLE PERFUSION, 100 mgActive substance: infliximabManufacturer: Samsung Bioepis Nl B.V.Prescription requiredDosage form: INJECTABLE PERFUSION, 100 mgActive substance: infliximabManufacturer: Pfizer Europe Ma EeigPrescription requiredDosage form: INJECTABLE PERFUSION, UnknownActive substance: infliximabManufacturer: Janssen Biologics B.V.Prescription required
Online doctors for REMSIMA 120 mg SOLUTION FOR INJECTION IN PRE-FILLED PEN
Discuss questions about REMSIMA 120 mg SOLUTION FOR INJECTION IN PRE-FILLED PEN, including use, safety considerations and prescription review, subject to medical assessment and local regulations.
Frequently Asked Questions