
FENTANEST 0,05 mg/ml SOLUÇÃO INJETÁVEL
Pergunte a um médico sobre a prescrição de FENTANEST 0,05 mg/ml SOLUÇÃO INJETÁVEL

Como usar FENTANEST 0,05 mg/ml SOLUÇÃO INJETÁVEL
Introdução
Prospecto: Informação para o paciente
Fentanest 0,05 mg/ml solução injetável
Citrato de fentanilo
Leia todo o prospecto atentamente antes de começar a usar este medicamento, porque contém informações importantes para si.
|
Conteúdo do prospecto:
- O que é Fentanest e para que é utilizado
- O que precisa saber antes de começar a usar Fentanest
- Como usar Fentanest solução injetável
- Efeitos adversos possíveis
- Conservação de Fentanest
- Conteúdo do envase e informações adicionais
1. O que é Fentanest e para que é utilizado
Fentanest contém fentanilo como princípio ativo. É um medicamento potente para o alívio da dor, que pertence ao grupo dos analgésicos narcóticos ou opioides.
Fentanest é utilizado:
- Em anestesia geral ou local, como analgésico narcótico complementar.
- Como medicação analgésica prévia para ajudar a induzir e a manter a anestesia geral e local, ao ser administrado junto com algum medicamento neuroléptico (medicamento que produz sedação do sistema nervoso), como por exemplo droperidol.
- Como anestésico com o oxigênio, em pacientes de alto risco submetidos a intervenções cirúrgicas.
2. O que precisa saber antes de começar a usar Fentanest
Não use Fentanest
- Se é alérgico a fentanilo ou a qualquer um dos outros componentes deste medicamento (incluídos na seção 6).
- Se apresenta intolerância conhecida a este medicamento ou a outros morfinomiméticos (medicamentos que têm um efeito parecido ao da morfina).
- Se apresenta traumatismo craneoencefálico, aumento da pressão intracraniana ou coma.
- Se o paciente é menor de 2 anos.
Advertências e precauções
Consulte o seu médico, farmacêutico ou enfermeiro antes de começar a usar Fentanest se:
Você ou alguém da sua família já abusou ou foi dependente do álcool, medicamentos sujeitos a prescrição ou drogas ilegais (“adicção”).
- É você fumante.
- Alguma vez teve problemas com o seu estado de ânimo (depressão, ansiedade ou um transtorno de personalidade) ou se foi tratado por um psiquiatra por outra doença mental.
Como ocorre com outros opioides potentes, a depressão respiratória(respiração lenta ou débil que não pode proporcionar uma ventilação e perfusão adequadas aos pulmões) depende da dosagem e pode ser revertida com o uso de um antagonista dos narcóticos (como por exemplo, naloxona). No entanto, pode ser necessário administrar doses adicionais deste antagonista, já que a depressão respiratória pode durar mais que a ação do antagonista dos opioides. A analgesia profunda vem acompanhada de uma marcada depressão respiratória que pode persistir ou reaparecer durante o período pós-operatório. Por esta razão, os pacientes devem permanecer sob uma vigilância adequada. Devem estar disponíveis um equipamento de reanimação e medicamentos antagonistas dos narcóticos. A hiperventilação (respiração mais rápida e profunda do que o normal) durante a anestesia pode alterar a resposta do paciente ao dióxido de carbono, afetando a respiração no período pós-operatório.
Pode produzir-se rigidez muscular, incluindo rigidez dos músculos torácicos, que se pode evitar tomando as seguintes medidas: injeção intravenosa muito lenta (que normalmente é suficiente para doses baixas), premedicação com benzodiazepinas e administração de relaxantes musculares.
Podem ocorrer movimentos mioclônicos não epilépticos(movimentos bruscos e involuntários).
Se o paciente não recebe quantidades suficientes de um medicamento anticolinérgico (medicamentos que calmam os espasmos musculares do intestino), ou quando fentanilo está associado a um relaxante muscular não vagolítico, pode ocorrer bradicardia(descenso na frequência cardíaca), e até paro cardíaco. A bradicardia pode ser tratada com a administração de atropina.
Os opioides podem induzir pressão arterial baixa, especialmente nos pacientes com uma diminuição significativa na quantidade normal de sangue (hipovolemia). Devem ser empregadas as medidas adequadas para manter uma pressão arterial estável.
Deve ser evitada a utilização de injeção em bolo rápida de opioides em pacientes com a função cerebrovascular comprometida; a diminuição transitória da pressão arterial média foi às vezes acompanhada por uma redução transitória da perfusão cerebral nesses pacientes.
Se se interromper o tratamento, podem aparecer sintomas de abstinência. Informe o seu médico ou enfermeira se você acredita que lhe está acontecendo isso (ver também seção 4. Efeitos adversos possíveis).
Dependência e adicção
Este medicamento contém fentanilo, que é um opioide. Pode causar dependência e/ou adicção. |
O uso repetido dos analgésicos opioides pode fazer com que o medicamento perca eficácia (quem o toma se acostuma com ele). Também pode produzir dependência e adicção, o que pode dar lugar a sobredoses potencialmente mortais. É importante que consulte o seu médico se lhe preocupa chegar a uma situação de dependência de Fentanest.
Em especial, informe o seu médico ou farmacêutico se está tomando:
- Alguns analgésicos para a dor neuropática (gabapentina e pregabalina).
Os pacientes sob tratamento prolongado com opioides ou com histórico de dependência a opioides podem requerer doses mais altas.
Recomenda-se reduzir a dose nos pacientes de idade avançada e debilitados. É necessário um ajuste cuidadoso da dose deste medicamento em pacientes com os seguintes transtornos: hipotireoidismo (diminuição dos níveis de hormonas tireoides), doença pulmonar, depressão respiratória, alcoolismo, função renal ou hepática deteriorada. Estes pacientes requerem, além disso, uma monitorização pós-operatória prolongada.
No uso simultâneo de fentanilo e droperidol, o médico deve conhecer as características de cada medicamento, especialmente as diferenças na duração da ação. A administração desses medicamentos ao mesmo tempo aumenta a possibilidade de pressão arterial baixa. Droperidol pode causar movimentos incontrolados do corpo ou da face, que podem ser controlados com medicamentos para a doença de Parkinson.
Uso de Fentanest com outros medicamentos
Comunique ao seu médico ou farmacêutico que está utilizando ou utilizou recentemente ou poderia ter que utilizar qualquer outro medicamento.
Deve ser evitado o uso simultâneo dos derivados do ácido barbitúricocom fentanilo, pois podem aumentar o efeito depressor de fentanilo sobre a respiração.
Não se recomenda o uso simultâneo de fentanilo com buprenorfina, nalbufina ou pentazocina(medicamentos indicados para o alívio da dor), pois podem provocar sintomas de abstinência em pacientes dependentes de opioides.
O uso simultâneo de Fentanest com medicamentos para retardar a atividade do sistema nervoso central (outros depressores do sistema nervoso central) pode produzir efeitos depressores adicionais, hipoventilação e hipotensão, e sedação profunda ou coma. Os depressores do sistema nervoso central incluem:
- opioides,
- antipsicóticos,
- hipnóticos,
- anestésicos gerais,
- relaxantes musculoesqueléticos,
- antihistamínicos sedantes,
- bebidas alcoólicas.
A epinefrina não deve ser nunca utilizada como agente vasoativo com o fentanilo, porque pode dar lugar a hipotensão.
Portanto, o uso simultâneo de qualquer um dos fármacos e substâncias ativas mencionadas requer vigilância do paciente.
Foi notificado que os inibidores da MAO(certo grupo de medicamentos antidepressivos), produzem um aumento do efeito dos analgésicos narcóticos, especialmente nos pacientes com insuficiência cardíaca. Portanto, fentanilo não deve ser usado durante os 14 dias posteriores à interrupção do tratamento com este tipo de medicamentos. Por regra geral, se recomenda suspender a administração dos inibidores da MAO nas duas semanas anteriores a qualquer intervenção cirúrgica. No entanto, vários relatórios descrevem o uso de fentanilo durante as intervenções cirúrgicas em pacientes que recebem os inibidores da monoaminooxidase sem que tenham ocorrido interações.
O emprego simultâneo de inibidores potentes do CYP3A4, p. ex.: ritonavir, cetoconazol, itraconazol, antibióticos macrólidos, com fentanilo, poderia dar lugar a um aumento das concentrações no plasma do fentanilo, as quais poderiam aumentar ou prolongar tanto os efeitos terapêuticos como os adversos e poderiam causar depressão respiratória grave. Nesta situação, são apropriados um cuidado especial e observação do paciente. Não se recomenda o emprego simultâneo de ritonavir ou outros inibidores do CYP3A4 potentes com fentanilo, a menos que o paciente esteja monitorizado de forma constante.
O uso concomitante de fentanilo e de medicamentos sedantes como as benzodiazepinas ou medicamentos relacionados aumenta o risco de sonolência, dificuldades para respirar (depressão respiratória), coma e pode ser mortal. Por isso, o uso concomitante apenas deve ser considerado quando não forem possíveis outras opções de tratamento.
No entanto, se o seu médico lhe prescrever fentanilo junto com medicamentos sedantes, a dose e duração do tratamento concomitante devem ser limitadas pelo seu médico.
Informe ao seu médico sobre todos os medicamentos sedantes que está tomando e siga atentamente as recomendações do seu médico quanto à dose. Poderia ser útil informar amigos ou familiares para que estejam a par dos sinais e sintomas antes mencionados. Entre em contato com o seu médico quando experimentar tais sintomas.
Gravidez, lactação e fertilidade
Se está grávida ou em período de lactação, ou acredita que possa estar grávida ou tem intenção de engravidar, consulte o seu médico ou farmacêutico antes de utilizar este medicamento.
Não foi estabelecida a segurança do uso de fentanilo durante a gravidez. Fentanilo não deve ser utilizado durante a gravidez, a menos que seja claramente necessário. O uso prolongado durante a gravidez pode causar síndrome de abstinência no recém-nascido.
Não se recomenda o uso de fentanilo durante o parto (incluindo a cesárea) já que fentanilo atravessa a placenta e pode produzir depressão respiratória no recém-nascido.
Fentanilo passa para o leite materno e pode produzir sedação e depressão respiratória no recém-nascido. Portanto, não se recomenda amamentação durante 24 horas após a administração do medicamento.
Condução e uso de máquinas
Não conduza nem maneje ferramentas ou máquinas após ter recebido Fentanest, pois este medicamento pode afetar a sua capacidade de reação. O seu médico lhe indicará quanto tempo deve esperar antes de voltar a conduzir ou utilizar máquinas.
Advertências sobre o doping
Informa-se os desportistas que este medicamento contém um componente que pode estabelecer um resultado analítico de controlo do doping como positivo.
Fentanest contém sódio
Este medicamento contém menos de 23 mg de sódio (1 mmol) por ampola de 2, 3 e 5 ml; isto é, essencialmente “isento de sódio”.
Este medicamento contém 35,4 mg de sódio (componente principal do sal de cozinha) em cada ampola de 10 ml. Isto equivale a 1,81% da ingestão diária máxima de sódio recomendada para um adulto.
3. Como usar Fentanest
Posologia
Este medicamento deve ser administrado por um médico ou enfermeiro. O seu médico determinará qual é a dose mais adequada para si, de acordo com a sua idade, peso, estado geral de saúde, tipo de intervenção e uso de outros medicamentos.
Pacientes de idade avançada e debilitados
A dose administrada a pacientes de idade avançada (65 anos ou mais) ou a pacientes debilitados logo antes da intervenção cirúrgica é menor do que a indicada para outros adultos. Se o médico considerar necessário, pode ser administrada outra dose adicional posteriormente.
Crianças de 2 anos de idade e maiores
A dose administrada às crianças logo antes da intervenção cirúrgica depende do peso da criança. Se o médico considerar necessário, pode ser administrada outra dose adicional posteriormente.
Os adolescentes de 12 a 17 anos recebem a mesma dose que os adultos.
Crianças menores de 2 anos de idade
Não há experiência de uso deste medicamento em crianças menores de 2 anos. Portanto, não se recomenda administrar este medicamento nesta faixa etária.
Pacientes com problemas renais
O médico pode decidir reduzir a dose administrada a pacientes com problemas renais.
Pacientes obesos
A dose administrada a pacientes obesos logo antes da intervenção cirúrgica pode ser inferior à indicada para outros adultos. Se o médico considerar necessário, pode ser administrada outra dose adicional posteriormente.
Via de administração
Este medicamento pode ser administrado em uma veia ou em um músculo.
Se lhe administrarem mais Fentanilo do que deve
Como a administração deste medicamento será realizada no hospital e será feita por um médico, é pouco provável que lhe sejam administradas doses excessivas. No entanto, consulte o seu médico ou enfermeiro se acredita que lhe tenham administrado demasiado medicamento ou se começar a experimentar dificuldades respiratórias, tonturas ou sintomas de baixa pressão arterial ou rigidez muscular. Uma sobredose também pode provocar um transtorno cerebral (conhecido como leucoencefalopatia tóxica).
Se tiver alguma outra dúvida sobre o uso deste medicamento, pergunte ao seu médico ou enfermeiro.
4. Efeitos adversos possíveis
Como todos os medicamentos, este medicamento pode produzir efeitos adversos, embora nem todas as pessoas os sofram.
Muito frequentes(podem afetar mais de 1 em cada 10 pessoas):
- Sonolência.
- Dor de cabeça, tontura.
- Náuseas, vómitos, constipação.
- Sudorese, prurido.
Frequentes(podem afetar até 1 em cada 10 pessoas):
- Sedação, nervosismo, perda de apetite, depressão.
- Secura da boca (xerostomia), mal-estar na parte superior do abdômen (dispepsia).
- Reações da pele na zona de aplicação.
Pouco frequentes(podem afetar até 1 em cada 100 pessoas):
- Euforia, amnésia, insônia, alucinações, agitação.
- Tremor, sensação de formigamento (parestesia), transtornos da fala, rigidez muscular, mioclonia (movimentos musculares involuntários, rápidos e irregulares).
- Taquicardia, bradicardia.
- Hipertensão, hipotensão.
- Dispnéia (falta de ar), hipoventilação.
- Diarréia.
- Erupções cutâneas agudas (exantema), rubor da pele (eritema).
- Retenção urinária.
- Dificuldade para engolir.
Raros(podem afetar até 1 em cada 1.000 pessoas):
- Arritmia.
- Dilatação dos vasos sanguíneos.
- Hipó.
- Edema (inchaço), sensação de frio.
Muito raros(podem afetar até 1 em cada 10.000 pessoas):
- Reação alérgica grave em todo o corpo (reação anafiláctica).
- Idéias delirantes, estados de excitação, astenia, ansiedade, confusão, disfunção sexual, sintomas de síndrome de abstinência.
- Torpeza ou perda de coordenação (ataxia), convulsões (incluindo convulsões clônicas e convulsões do grande mal).
- Diminuição da visão em um ou dois olhos (ambliopia)
- Depressão respiratória, apneia.
- Flatulência com dor, oclusão intestinal.
- Dor na bexiga urinária (cistalgia), diminuição na produção de urina (oligúria).
Frequência não conhecida(não podem ser estimadas a partir dos dados disponíveis):
- Desenvolvimento de tolerância e dependência física e psicológica, com o uso prolongado de fentanilo.
- Delirio (os sintomas podem consistir em uma combinação de agitação, inquietude, desorientação, confusão, medo, ver ou ouvir coisas que realmente não existem, transtornos do sono, pesadelos).
- Sintomas de síndrome de abstinência (pode manifestar-se pela aparição dos seguintes efeitos adversos: náuseas, vómitos, diarreia, ansiedade, calafrios, tremor e sudorese).
A depressão respiratória é o efeito mais grave de fentanilo.
Outros efeitos adversos:
Laringoespasmo.
Após a administração de fentanilo com outro neuroléptico, como droperidol, podem aparecer as seguintes reações adversas: tremor, nervosismo, experiências alucinatórias pós-operatórias e sintomas extrapiramidais.
Comunicação de efeitos adversos
Se experimentar qualquer tipo de efeito adverso, consulte o seu médico ou farmacêutico, mesmo que se trate de efeitos adversos que não aparecem neste prospecto. Também pode comunicá-los diretamente através do Sistema Espanhol de Farmacovigilância de medicamentos de Uso Humano: https://www.notificaram.es/. Mediante a comunicação de efeitos adversos, você pode contribuir para fornecer mais informações sobre a segurança deste medicamento.
5. Conservação de Fentanest
Mantenha fora da vista e do alcance das crianças.
Não requer condições especiais de conservação. Conservar no envase original para protegê-lo da luz. Use imediatamente após a abertura.
Não utilize este medicamento após a data de validade que aparece no envase após “CAD”. A data de validade é o último dia do mês que se indica.
Os medicamentos não devem ser jogados nos desagües, nem na lixeira. A eliminação do medicamento não utilizado e de todos os materiais que tenham estado em contato com ele será realizada de acordo com a normativa local. Dessa forma, você ajudará a proteger o meio ambiente.
6. Conteúdo do envase e informação adicional
Composição de Fentanest
- O princípio ativo é o fentanilo. Cada ml de solução contém 0,0785 mg de citrato de fentanilo, equivalentes a 0,05 mg de fentanilo.
Cada ampola de 2 ml contém 0,157 mg de citrato de fentanilo, equivalentes a 0,1 mg de fentanilo.
Cada ampola de 3 ml contém 0,2355 mg de citrato de fentanilo, equivalentes a 0,15 mg de fentanilo.
Cada ampola de 5 ml contém 0,3925 mg de citrato de fentanilo, equivalentes a 0,25 mg de fentanilo.
Cada ampola de 10 ml contém 0,785 mg de citrato de fentanilo, equivalentes a 0,5 mg de fentanilo.
- Os demais componentes são cloreto de sódio e água para injetável.
Aspecto do produto e conteúdo do envase
Caixas de 10 ampolas de 2 ml, 5 ampolas de 3 ml, 10 ampolas de 3 ml, 10 ampolas de 5 ml ou 10 ampolas de 10 ml.
Pode ser que apenas alguns tamanhos de envase sejam comercializados.
As ampolas são transparentes e contêm um líquido transparente e incolor.
Título da autorização de comercialização e responsável pela fabricação
Kern Pharma, S.L.
Vênus, 72 - Pol. Ind. Colón II
08228 Terrassa - Barcelona
Espanha
Data da última revisão deste prospecto: Março 2025
A informação detalhada e atualizada deste medicamento está disponível na página Web da Agência Espanhola de Medicamentos e Produtos Sanitários (AEMPS) http://www.aemps.gob.es/
Esta informação está destinada apenas a profissionais do setor sanitário:
Consulte a Ficha Técnica ou resumo das características do produto para obter uma descrição completa e outra informação.
Posologia e forma de administração
Este medicamento apenas deve ser administrado em um ambiente onde seja possível controlar as vias respiratórias e por parte de profissionais que possam vigiar as vias respiratórias (ver a Ficha Técnica seção 4.4).
A dose deste medicamento deve ser determinada de forma individual segundo a idade, peso corporal, estado físico, estado patológico subjacente, uso de outros fármacos e tipo de intervenção cirúrgica e de anestesia.
Adultos
Premedicação
Como premedicação (de 30 a 60 minutos antes da cirurgia) a dose habitual é de 0,7 a 1,4 ?g/kg (de 0,014 a 0,028 mL/kg) de fentanest por via intramuscular ou intravenosa lenta.
Uso como suplemento analgésico da anestesia local
Fentanest injetável pode ser administrado como analgésico complementar à anestesia local em doses de entre 0,35 a 1,4 ?g/kg (0,007 a 0,028 mL/kg) por via intramuscular ou intravenosa.
Uso como suplemento analgésico da anestesia geral.
Doses baixas: 2 µg /kg (0,04 mL/kg)
Fentanilo em doses mais baixas é muito útil nas intervenções cirúrgicas “menores” mas dolorosas.
Doses moderadas: 2 – 20 µg/kg (0,04-0,4 mL/kg)
Quando o procedimento cirúrgico é mais complicado, é necessário administrar uma dose moderada.
A duração da ação é dose-dependente.
Doses altas: 20 – 50 µg /kg (0,4-1 mL/kg)
Durante as intervenções cirúrgicas “maiores” nas quais o procedimento é mais prolongado, a administração das doses 20 – 50 µg/kg (0,4-1 mL/kg) de fentanilo com protóxido de nitrogênio/oxigênio mostrou um efeito amortecedor.
Seu médico realizará ventilação e observação pós-operatória.
Os incrementos de 25- 250 microgramas/kg (0,5 – 5 ml) podem ser administrados em função do que você necessita e da duração da intervenção cirúrgica.
Uso como agente anestésico.
Quando é particularmente importante reduzir a reação ao estímulo cirúrgico, podem ser administradas doses de 50 – 100 ?g/kg (1-2 mL/kg) por via intramuscular ou intravenosa com oxigênio e um relaxante muscular. Esta técnica proporciona a anestesia sem o uso adicional de agentes anestésicos.
Em alguns casos pode ser necessário administrar doses até 150 ?g/kg (3 mL/kg) para alcançar um efeito anestésico.
Fentanilo foi usado nos procedimentos cirúrgicos a coração aberto e certas intervenções cirúrgicas maiores nos pacientes para os quais se indica particularmente uma proteção do coração contra o excesso de oxigênio.
Uso em pacientes de idade avançada e debilitados
Tal como ocorre com outros opioides, a dose administrada nos pacientes de idade avançada ou debilitados deve ser reduzida.
Uso em crianças.
Para a indução e o mantenimento da anestesia em crianças de dois até doze anos de idade, recomenda-se reduzir a dose a 2 – 3 ?g/kg (0,04-0,06 mL/kg).
Uso em pacientes com insuficiência renal
Os dados obtidos de um estudo em que se administrou fentanilo por via intravenosa em pacientes submetidos a transplante renal sugerem que a eliminação de fentanilo pode estar reduzida na população de pacientes. Se os pacientes com afecção renal receberem fentanilo, deve-se observá-los com cuidado em busca de sinais de toxicidade por fentanilo e reduzir a dose em caso necessário (ver Dose e Administração).
Pacientes obesos
Nos pacientes obesos, existe risco de sobredose se a dose for calculada com base no peso corporal. A dose para os pacientes obesos deve ser calculada com base na massa corporal magra mais do que apenas no peso corporal.
Advertências e precauções especiais de emprego
Assim como sucede com outros opióides fortes:
A depressão respiratória guarda relação com a dose e pode ser invertida com a administração de um antagonista narcótico (naloxona), mas pode ser necessário administrar doses adicionais deste antagonista, pois a depressão respiratória poderia ter uma maior duração de ação do que os antagonistas opióides. A analgesia profunda vai acompanhada de uma marcada depressão respiratória que pode persistir ou reaparecer no período pós-operatório. Portanto, deve-se submeter os pacientes a uma supervisão apropriada. É necessário dispor de equipamento de reanimação e antagonistas narcóticos.
A hiperventilação durante a anestesia poderia modificar a resposta do paciente ao CO2, o que afetaria a respiração durante o período pós-operatório.
Pode produzir-se rigidez muscular, incluindo rigidez dos músculos torácicos, que pode ser evitada se se adotarem as medidas seguintes: injeção intravenosa lenta (que geralmente é suficiente para doses baixas), premedicação com uma benzodiazepina e administração de relaxantes musculares.
Podem aparecer movimentos (mi)clônicos não epilépticos.
Pode produzir-se bradicardia e possivelmente asistolia se o paciente receber uma quantidade insuficiente de anticolinérgico, ou ao combinar Fentanest com um relaxante muscular não vagolítico. A bradicardia pode ser tratada administrando atropina.
Os opióides podem provocar hipotensão, especialmente em pacientes com hipovolemia. Devem ser adotadas as medidas adequadas para manter uma pressão arterial estável.
Deve-se evitar a injeção rápida em bolo de opióides em pacientes com alteração da distensibilidade cerebrovascular, pois a redução transitória da pressão arterial média se acompanhou ocasionalmente de uma redução transitória da irrigação sanguínea cerebral nestes pacientes.
Os pacientes que recebem tratamento prolongado com opióides ou com antecedentes de abuso de opióides poderiam requerer doses maiores.
Se Fentanest for administrado com droperidol, o médico deve conhecer as propriedades de cada fármaco, especialmente a diferença na duração da ação. A incidência de hipotensão aumenta ao administrar esta combinação. Droperidol pode provocar sintomas extrapiramidais que podem ser controlados com fármacos antiparkinsonianos.
Dependência farmacológica e abuso potencial
Pode-se desenvolver tolerância, dependência física e psicológica após a administração repetida de opioides. Os riscos aumentam nos pacientes com antecedentes pessoais de abuso de substâncias (incluído o abuso ou a adicção de drogas ou álcool).
Síndrome de abstinência
A administração repetida a intervalos curtos durante períodos prolongados pode dar origem ao desenvolvimento de um síndrome de abstinência após a interrupção do tratamento, que pode se manifestar pela aparência dos seguintes efeitos adversos: náuseas, vômitos, diarreia, ansiedade, escalofríos, tremores e sudorese.
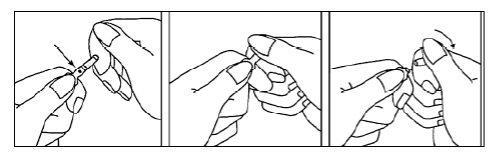
Instruções para a abertura das ampolas
- Mantenha a ampola entre os dedos índice e polegar com a ponta da ampola orientada para cima.
- Segure a ponta da ampola colocando o dedo índice da outra mão contra o pescoço da ampola. Coloque o dedo polegar para cobrir a ponta da ampola, conforme mostra o desenho.
- Com os dedos índices juntos, pressione na ponta para abrir a ampola.
Incompatibilidades
Na ausência de estudos de compatibilidade, este medicamento não deve ser misturado com outros.
Contraindicações
- Hipersensibilidade ao princípio ativo ou a algum dos excipientes incluídos na seção 6 da ficha técnica, ou a outros opioides.
- Insuficiência respiratória sem ventilação mecânica, devido ao efeito depressor respiratório específico dos fármacos morfinomiméticos.
- País de registo
- Disponibilidade em farmáciasProblema de disponibilidade reportado
- Substância ativa
- Requer receita médicaSim
- Fabricante
- Esta informação é apenas para referência e não constitui aconselhamento médico. Consulte sempre um médico antes de tomar qualquer medicamento. A Oladoctor não se responsabiliza por decisões médicas baseadas neste conteúdo.
- Alternativas a FENTANEST 0,05 mg/ml SOLUÇÃO INJETÁVELForma farmacêutica: INJETÁVEL, 50 microgramasSubstância ativa: fentanylFabricante: Laboratorios Basi Industria Farmaceutica S.A.Requer receita médicaForma farmacêutica: INJETÁVEL, 0,05 mg/mlSubstância ativa: fentanylFabricante: Kalceks AsRequer receita médicaForma farmacêutica: COMPRIMIDO SUBLINGUAL, 30 MICROGRAMASSubstância ativa: sufentanilFabricante: Laboratoire AguettantRequer receita médica
Alternativas a FENTANEST 0,05 mg/ml SOLUÇÃO INJETÁVEL noutros países
As melhores alternativas com o mesmo princípio ativo e efeito terapêutico.
Alternativa a FENTANEST 0,05 mg/ml SOLUÇÃO INJETÁVEL em Polónia
Alternativa a FENTANEST 0,05 mg/ml SOLUÇÃO INJETÁVEL em Ukraine
Médicos online para FENTANEST 0,05 mg/ml SOLUÇÃO INJETÁVEL
Avaliação de posologia, efeitos secundários, interações, contraindicações e renovação da receita de FENTANEST 0,05 mg/ml SOLUÇÃO INJETÁVEL – sujeita a avaliação médica e regras locais.














