
CLEXANE 6.000 UI (60 mg)/0,6 ml SOLUÇÃO INJETÁVEL EM SERINGA PREENCHIDA
Pergunte a um médico sobre a prescrição de CLEXANE 6.000 UI (60 mg)/0,6 ml SOLUÇÃO INJETÁVEL EM SERINGA PREENCHIDA

Como usar CLEXANE 6.000 UI (60 mg)/0,6 ml SOLUÇÃO INJETÁVEL EM SERINGA PREENCHIDA
Introdução
Prospecto: informação para o utilizador
CLEXANE 6.000 UI (60 mg)/0,6 ml solução injetável em seringa pré-carregada
enoxaparina sódica
Leia todo o prospecto atentamente antes de começar a usar este medicamento, porque contém informações importantes para si.
- Conserva este prospecto, porque pode ter que voltar a lê-lo.
- Se tiver alguma dúvida, consulte o seu médico, farmacêutico ou enfermeira.
- Este medicamento foi prescrito apenas para si, e não deve dá-lo a outras pessoas, mesmo que tenham os mesmos sintomas que si, porque pode prejudicá-las.
- Se experimentar efeitos adversos, consulte o seu médico ou farmacêutico, mesmo que se trate de efeitos adversos que não aparecem neste prospecto. Ver seção 4.
Conteúdo do prospecto
- O que é Clexane e para que se utiliza
- O que precisa saber antes de começar a usar Clexane
- Como usar Clexane
- Efeitos adversos possíveis
- Conservação de Clexane
- Conteúdo do envase e informação adicional
1. O que é Clexane e para que se utiliza
Clexane contém um princípio ativo denominado enoxaparina sódica. Pertence a um grupo de medicamentos denominado “heparina de baixo peso molecular” ou HBPM.
Como actua Clexane
Clexane actua de duas formas:
- Impedindo que os coágulos de sangue já existentes se tornem maiores. Isso ajuda ao seu organismo a rompê-los e a que não continuem a fazer-lhe mal.
- Interrompendo a formação de novos coágulos na sangue.
Para que se usa Clexane
Pode-se usar Clexane para:
- Tratar os coágulos que há na sangue
- Evitar a formação de coágulos na sangue nas seguintes situações:
- antes e depois de uma operação quirúrgica
- quando tiver uma doença a curto prazo e não puder mover-se durante algum tempo
- se teve um coágulo de sangue devido ao cancro, para prevenir que se formem mais coágulos.
- Para evitar a formação de coágulos de sangue quando tiver angina instável (uma doença em que não chega suficiente quantidade de sangue ao coração) ou depois de um ataque ao coração
- Evitar a formação de coágulos de sangue nos tubos do aparelho de diálise (que se emprega em pessoas que padecem problemas graves de rim).
2. O que precisa saber antes de começar a usar Clexane
Não use Clexanese:
- é alérgico a:
- enoxaparina sódica ou a algum dos outros componentes deste medicamento (incluídos na seção 6)
- a heparina ou a outras heparinas de baixo peso molecular como nadroparina, tinzaparina ou dalteparina.
Os sinais de uma reação alérgica incluem: erupção, problemas para respirar ou engolir, inchação de cara, lábios, língua, cavidade bucal, garganta ou olhos.
- teve uma reação à heparina que causou uma diminuição grave no número de células que intervêm na coagulação (plaquetas) nos últimos 100 dias
- tem anticorpos frente à enoxaparina no sangue
- está sangrando abundantemente ou padece doenças de alto risco de sangramento como:
- úlcera de estômago, intervenção recente de cérebro ou olhos, ou hemorragia cerebral.
- está usando Clexane para tratar coágulos na sangue, e vai ter em 24 horas:
- uma punção lombar ou espinal
- uma operação com anestesia espinal ou epidural.
Não use Clexane se lhe afecta alguma das condições mencionadas. Se não tem a certeza, consulte o seu médico ou farmacêutico antes de usar Clexane.
Advertências e precauções
Não se deve trocar Clexane por outras “heparinas de baixo peso molecular” como nadroparina, tinzaparina ou dalteparina. Isso é porque não são exactamente iguais e não têm a mesma actividade nem as mesmas instruções de uso.
Consulte o seu médico ou farmacêutico antes de começar a usar Clexane se:
- alguma vez teve uma reação à heparina que causou uma diminuição grave no número de células que intervêm na coagulação (plaquetas)
- lhe foi implantada uma válvula cardíaca
- tem endocardite (uma infecção do revestimento interior do coração)
- tem antecedentes de úlcera gástrica
- teve recentemente uma hemorragia cerebral
- tem alta a pressão sanguínea
- tem diabetes ou problemas nos vasos sanguíneos dos olhos causados pela diabetes (denominado retinopatia diabética)
- foi operado recentemente de olhos ou cérebro
- é uma pessoa de idade avançada (por cima dos 65 anos) e especialmente se é maior de 75 anos
- tem problemas de rim
- tem problemas de fígado
- apresenta um peso muito baixo ou tem sobrepeso
- tem alto os níveis de potássio no sangue (que poderia comprovar-se com uma análise de sangue)
- actualmente está usando medicamentos que afectam o sangramento (ver seção 2, “Uso de Clexane com outros medicamentos”)
- tem algum problema com a sua coluna ou lhe foi feita cirurgia espinal.
Se lhe afecta alguma das condições mencionadas (ou não tem a certeza), consulte o seu médico ou farmacêutico antes de usar Clexane.
Para os pacientes que recebem doses superiores a 210 mg/dia, este medicamento contém mais de 24 mg de sódio (componente principal da sal de mesa/para cozinhar) em cada dose. Isso equivale a 1,2% da ingesta diária máxima de sódio recomendada para um adulto.
Análises e controles
Poderia ter que realizar-se uma análise de sangue antes de começar a utilizar este medicamento, e enquanto o estiver usando; isso é para comprovar o nível das células que intervêm na coagulação (plaquetas) e os níveis de potássio no sangue.
Crianças e adolescentes
Não se avaliou a eficácia e segurança de Clexane em crianças ou adolescentes.
Uso deClexanecom outros medicamentos
Informa o seu médico ou farmacêutico se está utilizando, utilizou recentemente ou poderia ter que utilizar qualquer outro medicamento.
- warfarina – empregada para reduzir a coagulação da sangue
- aspirina (também conhecida como ácido acetilsalicílico ou AAS), clopidogrel ou outros medicamentos usados para interromper a formação de coágulos na sangue (ver seção 3, “Mudança de medicamento anticoagulante”)
- injeção de dextrano – usado como substituto da sangue
- ibuprofeno, diclofenaco, ketorolaco e outros medicamentos conhecidos como anti-inflamatórios não esteroideos utilizados para tratar a dor e a inflamação em artrite e outras doenças
- prednisolona, dexametasona e outros medicamentos utilizados para tratar o asma, a artrite reumatoide e outras doenças
- medicamentos que aumentam os níveis de potássio no sangue como sales de potássio, medicamentos para eliminar líquidos (diuréticos), e alguns medicamentos para tratar problemas de coração.
Operações quirúrgicas e anestesia
Em caso de que lhe vão a realizar uma punção lombar ou espinal, ou vai a submeter-se a uma operação quirúrgica onde se vai a utilizar uma anestesia espinal ou epidural, informe o seu médico que está usando Clexane.
Gravidez e lactação
Se está grávida, acredita que possa estar grávida ou tem intenção de ficar grávida, consulte o seu médico ou farmacêutico antes de utilizar este medicamento.
Se está grávida e tem implantada uma válvula cardíaca mecânica, poderia ter um risco maior de que se formem coágulos na sangue. O seu médico falará com si sobre este tema.
Se está em período de lactação ou planeia dar a lactação, deve consultar o seu médico antes de utilizar este medicamento.
Condução e uso de máquinas
Clexane não afecta a capacidade para conduzir e usar máquinas.
Recomenda-se que o profissional de saúde anote o nome comercial e o número de lote do produto que está a usar.
3. Como usar Clexane
Siga exatamente as instruções de administração deste medicamento indicadas pelo seu médico ou farmacêutico. Em caso de dúvida, consulte novamente o seu médico ou farmacêutico.
Uso do medicamento
- Normalmente o seu médico ou enfermeira lhe administrará Clexane. Isso ocorre porque ele deve ser administrado por injeção.
- Clexane é geralmente administrado por injeção sob a pele (via subcutânea).
- Clexane pode ser administrado por injeção nas veias (via intravenosa) após certos tipos de ataques cardíacos ou operações cirúrgicas.
- Clexane pode ser adicionado ao tubo que sai do corpo (linha arterial) no início de uma sessão de diálise.
- Não administre Clexane no músculo (via intramuscular).
Quantidade a ser administrada
- Seu médico decidirá a quantidade de Clexane a ser administrada. A quantidade dependerá do motivo pelo qual será usado.
- Se tiver algum problema renal, pode ser que seja administrada uma quantidade menor de Clexane.
- Tratamento da formação de coágulos no sangue
- A dose habitual é de 150 UI (1,5 mg) por quilograma de peso corporal uma vez ao dia ou 100 UI (1 mg) por quilograma de peso corporal duas vezes ao dia.
- Seu médico decidirá por quanto tempo receberá Clexane.
- Interrupção da formação de coágulos no sangue durante operações cirúrgicas ou períodos de mobilidade limitada devido a uma doença
- A dose dependerá da probabilidade de desenvolver um coágulo. Será administrada 2.000 UI (20 mg) ou 4.000 UI (40 mg) de Clexane ao dia.
- Se for operado, geralmente a primeira injeção será administrada 2 ou 12 horas antes da operação.
- Se tiver mobilidade reduzida devido a uma doença, geralmente será administrada 4.000 UI (40 mg) de Clexane ao dia.
- Seu médico decidirá por quanto tempo receberá Clexane.
- Interrupção da formação de coágulos quando tiver angina instável ou após ter tido um ataque cardíaco
- Clexane pode ser usado em 2 tipos diferentes de ataques cardíacos.
- A quantidade de Clexane a ser administrada dependerá da idade e do tipo de ataque cardíaco que teve.
Ataque cardíaco do tipo IAMSEST (infarto do miocárdio sem elevação do segmento ST):
- A dose habitual é de 100 UI (1 mg) por quilograma de peso corporal a cada 12 horas.
- Geralmente, seu médico dirá que também deve tomar aspirina (ácido acetilsalicílico).
- Seu médico decidirá por quanto tempo receberá Clexane.
Ataque cardíaco do tipo IAMCEST (infarto do miocárdio com elevação do segmento ST) se for menor de 75 anos:
- Será administrada uma injeção inicial intravenosa de 3.000 UI (30 mg) de Clexane.
- Ao mesmo tempo, será administrada uma injeção de Clexane sob a pele (injeção subcutânea). A dose habitual é de 100 UI (1 mg) por quilograma de peso corporal, a cada 12 horas.
- Geralmente, seu médico dirá que também deve tomar aspirina (ácido acetilsalicílico).
- Seu médico decidirá por quanto tempo receberá Clexane.
Ataque cardíaco do tipo IAMCEST se tiver 75 anos ou mais:
- A dose habitual é de 75 UI (0,75 mg) por quilograma de peso corporal, a cada 12 horas.
- A quantidade máxima de Clexane administrada nas duas primeiras injeções é de 7.500 UI (75 mg).
- Seu médico decidirá por quanto tempo receberá Clexane.
Para pacientes submetidos a uma intervenção coronária percutânea (ICP):
- Dependendo de quando foi administrada a última injeção de Clexane, seu médico pode decidir administrar uma dose adicional de Clexane antes de uma intervenção ICP. Seria por injeção na veia.
- Interrupção da formação de coágulos sanguíneos nos tubos do aparelho de diálise
- A dose habitual é de 100 UI (1 mg) por quilograma de peso corporal.
- Clexane é adicionado ao tubo que sai do corpo (linha arterial) no início de uma sessão de diálise. Essa quantidade geralmente é suficiente para uma sessão de 4 horas. No entanto, é possível que seu médico pratique uma nova injeção de 50 UI a 100 UI (de 0,5 a 1 mg) por quilograma de peso corporal, se necessário.
Se vai injetar Clexane sozinho
Se puder administrar Clexane sozinho, seu médico ou enfermeira mostrarão como fazer. Não tente injetar sozinho se não lhe ensinaram a forma de fazer. Se não tiver certeza do que fazer, consulte imediatamente seu médico ou enfermeira. Se a injeção for realizada sob a pele de forma correta (o que se denomina “injeção subcutânea”), isso ajudará a reduzir a dor e o hematoma no ponto de injeção.
Antes de injetar Clexane sozinho
- Prepare o que vai precisar: seringa, pedaço de algodão com álcool ou sabão e água, e contêiner para objetos pontiagudos
- Verifique a data de validade do medicamento. Se expirou, não o use
- Verifique se a seringa não está danificada e se a solução do medicamento é transparente. Se não for, use outra seringa
- Certe-se de que conhece a quantidade a ser injetada
- Revise na zona do seu estômago se a última injeção causou vermelhidão, mudança da cor da pele, inchaço, supuração ou dor que ainda persiste. Se isso ocorrer, consulte com seu médico ou enfermeira
Instruções para injetar Clexane sozinho:
(Instruções para seringas sem dispositivo de segurança)
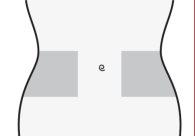
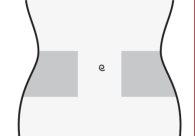
Preparação do local de injeção
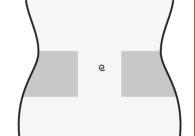
- Escolha uma zona no lado direito ou esquerdo do seu estômago. Pelo menos a 5 cm do umbigo e em direção a qualquer um dos dois lados.
- Não se injete dentro dos 5 cm que rodeiam o umbigo ou ao redor do mesmo se existem cicatrizes ou hematomas.
- Para se injetar, alterne o lado esquerdo e direito do seu estômago, dependendo de onde foi injetada a última vez.
- Lave as mãos. Limpe (não esfregue) a zona em que vai realizar a injeção com um pedaço de algodão com álcool ou com sabão e água.
- Sente-se ou deite-se em uma posição confortável para que esteja relaxado. Verifique se pode ver a zona em que se vai injetar. O mais adequado é em um divã, cadeira reclinável, ou em uma cama com travesseiros.
Seleção da dose
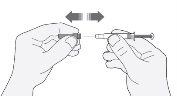
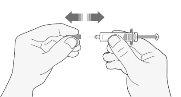
- Retire cuidadosamente o capuchão da agulha da seringa puxando-o. Descarte o capuchão.
- Antes de se injetar, não pressione o êmbolo para eliminar as bolhas de ar. Isso pode dar lugar a uma perda de medicamento.
- Uma vez que tenha retirado o capuchão, não toque nada com a agulha. Dessa forma, garantirá que a agulha continue estando limpa (estéril).
- Quando a quantidade de medicamento na seringa coincide com a dose que lhe foi prescrita, não há necessidade de ajustar a dose. Agora já está preparado para a administração da injeção.
- Quando a dose depende do seu peso corporal, pode ser necessário ajustar a dose na seringa para que coincida com a dose prescrita. Nesse caso, poderá se livrar do excesso de medicamento mantendo a seringa apontando para baixo (para manter a bolha de ar na seringa) e expulsando o excesso em um contêiner.
- Pode aparecer uma gota no extremo da agulha. Se isso acontecer, é necessário eliminar a gota antes de administrar a injeção dando golpes suaves na seringa com a agulha apontando para baixo. Agora já está preparado para a administração da injeção.
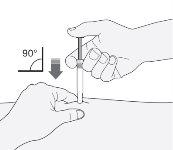
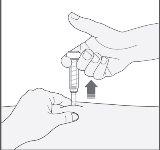
Administração da injeção
- Segure a seringa com a mão que escreve (como se fosse um lápis). Com a outra mão, puxe suavemente a zona que limpou do seu estômago, entre o dedo indicador e o polegar para formar um dobra na pele.
- Certe-se de segurar esse dobra da pele enquanto durar a injeção.
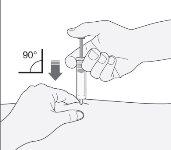
- Mantenha a seringa de maneira que a agulha aponte reta para baixo (verticalmente com um ângulo de 90º). Introduza toda a agulha no dobra da pele.
- Pressione o êmbolo com o seu polegar. Dessa forma, administrará a medicação no tecido gordo do estômago. Complete a injeção usando todo o medicamento da seringa.
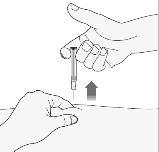
- Retire a agulha do local de injeção puxando reto dela. Oriente a agulha afastada de si mesmo e de outras pessoas. Agora pode soltar o dobra da pele.
Quando tiver terminado
- Para evitar que lhe saia um hematoma, não esfregue a zona de injeção após a injeção.
- Deposite a seringa usada no contêiner para objetos pontiagudos. Feche bem a tampa do contêiner e coloque o contêiner fora do alcance das crianças. Quando o contêiner estiver cheio, elimine-o como seu médico ou farmacêutico lhe indicou.
A eliminação do medicamento não utilizado e de todos os materiais que tenham estado em contato com ele será realizada de acordo com a normativa local.
Instruções para seringas com dispositivo de segurança automático tipo ERISTM:
Preparação do local de injeção
- Escolha uma zona no lado direito ou esquerdo do seu estômago. Pelo menos a 5 cm do umbigo e em direção a qualquer um dos dois lados.
- Não se injete dentro dos 5 cm que rodeiam o umbigo ou ao redor do mesmo se existem cicatrizes ou hematomas.
- Para se injetar, alterne o lado esquerdo e direito do seu estômago, dependendo de onde foi injetada a última vez.
- Lave as mãos. Limpe (não esfregue) a zona em que vai realizar a injeção com um pedaço de algodão com álcool ou com sabão e água.
- Sente-se ou deite-se em uma posição confortável para que esteja relaxado. Verifique se pode ver a zona em que se vai injetar. O mais adequado é em um divã, cadeira reclinável, ou em uma cama com travesseiros.
Seleção da dose
- Retire cuidadosamente o capuchão da agulha da seringa puxando-o. Descarte o capuchão.
- Antes de se injetar, não pressione o êmbolo para eliminar as bolhas de ar. Isso pode dar lugar a uma perda de medicamento.
- Uma vez que tenha retirado o capuchão, não toque nada com a agulha. Dessa forma, garantirá que a agulha continue estando limpa (estéril).

- Quando a quantidade de medicamento na seringa coincide com a dose que lhe foi prescrita, não há necessidade de ajustar a dose. Agora já está preparado para a administração da injeção.
- Quando a dose depende do seu peso corporal, pode ser necessário ajustar a dose na seringa para que coincida com a dose prescrita. Nesse caso, poderá se livrar do excesso de medicamento mantendo a seringa apontando para baixo (para manter a bolha de ar na seringa) e expulsando o excesso em um contêiner.
- Pode aparecer uma gota no extremo da agulha. Se isso acontecer, é necessário eliminar a gota antes de administrar a injeção dando golpes suaves na seringa com a agulha apontando para baixo. Agora já está preparado para a administração da injeção.
Administração da injeção
- Segure a seringa com a mão que escreve (como se fosse um lápis). Com a outra mão, puxe suavemente a zona que limpou do seu estômago, entre o dedo indicador e o polegar para formar um dobra na pele.
- Certe-se de segurar esse dobra da pele enquanto durar a injeção.
- Mantenha a seringa de maneira que a agulha aponte reta para baixo (verticalmente com um ângulo de 90º). Introduza toda a agulha no dobra da pele.
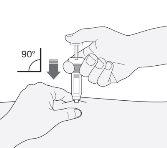
- Pressione o êmbolo com o seu polegar. Dessa forma, administrará a medicação no tecido gordo do estômago. Complete a injeção usando todo o medicamento da seringa.
- Retire a agulha do local de injeção puxando reto dela. Uma capa protetora cobrirá automaticamente a agulha. Agora pode soltar o dobra da pele. O dispositivo de segurança só liberará a capa protetora quando a seringa estiver vazia pressionando profundamente o êmbolo.
Quando tiver terminado
- Para evitar que lhe saia um hematoma, não esfregue a zona de injeção após a injeção.
- Deposite a seringa usada no contêiner para objetos pontiagudos. Feche bem a tampa do contêiner e coloque o contêiner fora do alcance das crianças. Quando o contêiner estiver cheio, elimine-o como seu médico ou farmacêutico lhe indicou.
A eliminação do medicamento não utilizado e de todos os materiais que tenham estado em contato com ele será realizada de acordo com a normativa local.
Instruções para seringas com dispositivo de segurança automático tipo PREVENTISTM:
Preparação do local de injeção
- Escolha uma zona no lado direito ou esquerdo do seu estômago. Pelo menos a 5 cm do umbigo e em direção a qualquer um dos dois lados.
- Não se injete dentro dos 5 cm que rodeiam o umbigo ou ao redor do mesmo se existem cicatrizes ou hematomas.
- Para se injetar, alterne o lado esquerdo e direito do seu estômago, dependendo de onde foi injetada a última vez.
- Lave as mãos. Limpe (não esfregue) a zona em que vai realizar a injeção com um pedaço de algodão com álcool ou com sabão e água.
- Sente-se ou deite-se em uma posição confortável para que esteja relaxado. Verifique se pode ver a zona em que se vai injetar. O mais adequado é em um divã, cadeira reclinável, ou em uma cama com travesseiros.
Seleção da dose
- Retire cuidadosamente o capuchão da agulha da seringa puxando-o. Descarte o capuchão.
- Antes de se injetar, não pressione o êmbolo para eliminar as bolhas de ar. Isso pode dar lugar a uma perda de medicamento.
- Uma vez que tenha retirado o capuchão, não toque nada com a agulha. Dessa forma, garantirá que a agulha continue estando limpa (estéril).
- Quando a quantidade de medicamento na seringa coincide com a dose que lhe foi prescrita, não há necessidade de ajustar a dose. Agora já está preparado para a administração da injeção.
- Quando a dose depende do seu peso corporal, pode ser necessário ajustar a dose na seringa para que coincida com a dose prescrita. Nesse caso, poderá se livrar do excesso de medicamento mantendo a seringa apontando para baixo (para manter a bolha de ar na seringa) e expulsando o excesso em um contêiner.
- Pode aparecer uma gota no extremo da agulha. Se isso acontecer, é necessário eliminar a gota antes de administrar a injeção dando golpes suaves na seringa com a agulha apontando para baixo. Agora já está preparado para a administração da injeção.
Administração da injeção
- Segure a seringa com a mão que escreve (como se fosse um lápis). Com a outra mão, puxe suavemente a zona que limpou do seu estômago, entre o dedo indicador e o polegar para formar um dobra na pele.
- Certe-se de segurar esse dobra da pele enquanto durar a injeção.
- Mantenha a seringa de maneira que a agulha aponte reta para baixo (verticalmente com um ângulo de 90º). Introduza toda a agulha no dobra da pele.
- Pressione o êmbolo com o seu polegar. Dessa forma, administrará a medicação no tecido gordo do estômago. Complete a injeção usando todo o medicamento da seringa.
- Retire a agulha do local de injeção puxando reto dela, mantendo o dedo no êmbolo. Oriente a agulha afastada de si mesmo e de outras pessoas, e pressione firmemente o êmbolo para ativar o sistema de segurança. A capa protetora cobrirá automaticamente a agulha. Escutará um “clic” que confirma a ativação do sistema de segurança. Agora pode soltar o dobra da pele.

Quando tiver terminado
- Para evitar que lhe saia um hematoma, não esfregue a zona de injeção após a injeção.
- Deposite a seringa usada no contêiner para objetos pontiagudos. Feche bem a tampa do contêiner e coloque o contêiner fora do alcance das crianças. Quando o contêiner estiver cheio, elimine-o como seu médico ou farmacêutico lhe indicou.
A eliminação do medicamento não utilizado e de todos os materiais que tenham estado em contato com ele será realizada de acordo com a normativa local.
Troca de medicamento anticoagulante
- Troca de Clexane para medicamentos para reduzir a coagulação do sangue denominados antagonistas da vitamina K (como warfarina)
Seu médico solicitará que lhe realizem a determinação no sangue de um parâmetro denominado INR e lhe dirá quando deve interromper o tratamento com Clexane.
- Troca de medicamentos para reduzir a coagulação do sangue denominados antagonistas da vitamina K (como warfarina) para Clexane
Interrompa o uso do antagonista da vitamina K. Seu médico solicitará que lhe realizem a determinação no sangue de um parâmetro denominado INR e lhe dirá quando começar a utilizar Clexane.
- Troca de Clexane para tratamento com anticoagulantes orais diretos
Interrompa o uso de Clexane.
4. Possíveis efeitos adversos
Assim como todos os medicamentos, este medicamento pode produzir efeitos adversos, embora nem todas as pessoas os sofram.
Efeitos adversos graves
Interrompa o tratamento com Clexanee informe imediatamente ao seu médico ou enfermeirase experimentar qualquer sinal de reação alérgica grave (como erupção, problemas para respirar ou engolir, inchaço da face, lábios, língua, cavidade bucal, garganta ou olhos).
Interrompa o tratamento com enoxaparina e informe imediatamente ao seu médico ou enfermeira se experimentar algum dos seguintes sintomas:
- uma erupção generalizada, vermelha e escamosa, com protuberâncias sob a pele e bolhas, acompanhada de febre. Os sintomas costumam aparecer no início do tratamento (pustulose exantemática generalizada aguda).
Assim como outros medicamentos semelhantes para reduzir os coágulos no sangue, Clexane pode causar sangramento. Isso pode colocar em perigo a sua vida. Em alguns casos, o sangramento pode não ser evidente.
Informar imediatamente ao seu médico se:
- tiver qualquer sangramento que não pare por si mesmo
- tiver sinais de sangramento excessivo (como se sentir muito fraco, cansaço, palidez, ou tontura com dor de cabeça ou inchaço inexplicável).
Seu médico pode decidir mantê-lo sob estrita observação ou mudar sua medicação.
Deve informar imediatamente ao seu médico:
- se apresentar qualquer sinal de bloqueio de um vaso sanguíneo por um coágulo de sangue como:
- dor tipo cãibra, vermelhidão, calor, ou inchaço em uma das suas pernas – que são sintomas de trombose venosa profunda
- dificuldade para respirar, dor no peito, desmaio ou tosse com sangue – que são sintomas de embolia pulmonar
- se tiver erupção cutânea dolorosa com pontos de cor vermelha escura sob a pele que não desaparecem ao pressioná-los.
Seu médico pode solicitar uma análise de sangue para verificar o número de plaquetas.
Outros efeitos adversos:
Muito frequentes(podem afetar mais de 1 de cada 10 pessoas):
- sangramento
- aumento das enzimas hepáticas.
Frequentes(podem afetar até 1 de cada 10 pessoas):
- se aparecem hematomas com maior frequência do que o habitual - isso pode ser devido a um problema do sangue devido a um número baixo de plaquetas
- placas rosadas na pele - aparecem com maior frequência na zona em que lhe foram injetados Clexane
- erupção na pele (habões, urticária)
- vermelhidão e coceira na pele
- hematoma ou dor no local de injeção
- diminuição do número de células vermelhas no sangue
- aumento do número de plaquetas no sangue
- dor de cabeça.
Pouco frequentes(podem afetar até 1 de cada 100 pessoas):
- dor de cabeça grave repentina - isso pode ser um sinal de hemorragia no cérebro
- sensação de sensibilidade à palpação e inchaço do estômago - pode ser indicativo de uma hemorragia gástrica
- lesões vermelhas e grandes na pele, de forma irregular com ou sem bolhas
- irritação na pele (irritação local)
- amarelamento da pele ou olhos, e escurecimento do colorido da urina - isso pode ser devido a um problema do fígado.
Raros(podem afetar até 1 de cada 1.000 pessoas):
- reação alérgica grave - os sinais dessa reação podem incluir: erupção na pele, problemas para engolir ou respirar, inchaço nos lábios, face, garganta ou língua
- aumento do potássio no sangue - isso é mais provável que ocorra em pessoas com problemas de rim ou diabetes. Seu médico pode verificar isso realizando uma análise de sangue
- aumento do número de eosinófilos no sangue - seu médico pode verificar isso realizando uma análise de sangue
- perda de cabelo
- osteoporose (uma doença em que os ossos podem fraturar com maior probabilidade)
- formigamento, entorpecimento e fraqueza nos músculos (especialmente na parte inferior do corpo) quando lhe foi feita uma punção lombar ou uma anestesia espinhal
- perda de controle da bexiga ou do intestino (de modo que não pode controlar suas necessidades)
- endurecimento ou nódulo no local de injeção.
Comunicação de efeitos adversos
Se experimentar qualquer tipo de efeito adverso, consulte o seu médico, farmacêutico ou enfermeira, mesmo que se trate de possíveis efeitos adversos que não aparecem neste prospecto. Também pode comunicá-los diretamente através do Sistema Español de Farmacovigilância de medicamentos de Uso Humano: https://www.notificaram.es. Mediante a comunicação de efeitos adversos, você pode contribuir para fornecer mais informações sobre a segurança deste medicamento.
5. Conservação de Clexane
Não conservar a temperatura superior a 25°C. Não congelar.
Mantenha este medicamento fora da vista e do alcance das crianças.
Não utilize este medicamento após a data de validade que aparece no envase após CAD. A data de validade é o último dia do mês que se indica.
Não utilize este medicamento se observar uma fissura na seringa, partículas em suspensão na solução, ou um colorido anormal da solução (ver “Aspecto do produto e conteúdo do envase”).
Os medicamentos não devem ser jogados nos deságues nem na lixeira. Deposite os envases e os medicamentos que não precisa no Ponto SIGRE da farmácia. Em caso de dúvida, pergunte ao seu farmacêutico como se livrar dos envases e dos medicamentos que já não precisa. Dessa forma, ajudará a proteger o meio ambiente.
6. Conteúdo do envase e informação adicional
Composição de Clexane
- O princípio ativo é enoxaparina sódica
Cada ml contém 100 mg de enoxaparina sódica, equivalente a 10.000 UI de atividade de anti-Xa
- Cada seringa pré-carregada com 0,6 ml contém 6.000 UI (60 mg) de enoxaparina sódica
- O outro componente é água para preparações injetáveis
Aspecto do produto e conteúdo do envase
Clexane é uma solução injetável em seringa pré-carregada de vidro (com ou sem dispositivo de segurança automático), transparente, de incolora a amarelada.
Aparece em envases de 2, 5, 6, 10, 12, 20, 24, 30, 50, 100 seringas pré-carregadas, e em envases múltiplos de 3 x 10, 9 x 10, 100 x 10, e 200 x 10 seringas pré-carregadas.
Pode ser que apenas alguns tamanhos de envase sejam comercializados.
Título da autorização de comercialização
sanofi-aventis, S.A.
C/ Roselló i Porcel, 21
08016 Barcelona
Espanha
Responsável pela fabricação
Sanofi Winthrop Industrie
Boulevard Industriel
76580 Le Trait,
França
Ou
Sanofi Winthrop Industrie
180 rue Jean Jaurès
94700 Maisons-Alfort
França
Ou
Chinoin Pharmaceutical and Chemical Works Private Co. Ltd
Csanyikvölgy site
Miskolc, Csanyikvölgy
H-3510
Hungria
Ou
Sanofi-Aventis GmbH
Turm A, 29. OG, Wienerbergstraße 11
1100 Viena
Áustria
Ou
Sanofi-Aventis Private Co. Ltd
Budapest Logistics and Distribution Platform
Bdg. DC5, Campona utca1.
Budapeste, 1225
Hungria
Ou
Sanofi-Aventis Deutschland GmbH
Industriepark Höchst-Brüningstraße 50
65926 Frankfurt am Main
Alemanha
Este medicamento está autorizado nos estados membros do Espaço Econômico Europeu com os seguintes nomes:
Áustria, França, Portugal: Lovenox.
Bélgica, Bulgária, Croácia, Chipre, República Checa, Estônia, Alemanha, Grécia, Hungria, Irlanda, Itália, Letônia, Luxemburgo, Malta, Polônia, Romênia, Eslováquia, Eslovênia, Espanha, Reino Unido: Clexane.
Itália: Clexane T.
Finlândia, Islândia, Noruega, Suécia: Klexane.
Data da última revisão deste prospecto:fevereiro 2022
Outras fontes de informação
A informação detalhada deste medicamento está disponível na página web da Agência Española de Medicamentos y Productos Sanitarios (AEMPS) http://www.aemps.gob.es/

Quanto custa o CLEXANE 6.000 UI (60 mg)/0,6 ml SOLUÇÃO INJETÁVEL EM SERINGA PREENCHIDA em Espanha em 2025?
O preço médio do CLEXANE 6.000 UI (60 mg)/0,6 ml SOLUÇÃO INJETÁVEL EM SERINGA PREENCHIDA em novembro de 2025 é de cerca de 54.34 EUR. Os valores podem variar consoante a região, a farmácia e a necessidade de receita. Confirme sempre com uma farmácia local ou fonte online para obter informações atualizadas.
- País de registo
- Preço médio em farmácia54.34 EUR
- Substância ativa
- Requer receita médicaSim
- Fabricante
- Esta informação é apenas para referência e não constitui aconselhamento médico. Consulte sempre um médico antes de tomar qualquer medicamento. A Oladoctor não se responsabiliza por decisões médicas baseadas neste conteúdo.
- Alternativas a CLEXANE 6.000 UI (60 mg)/0,6 ml SOLUÇÃO INJETÁVEL EM SERINGA PREENCHIDAForma farmacêutica: INJETÁVEL, 100 mg (10000 UI) enoxaparina sódica/mlSubstância ativa: enoxaparinFabricante: Sanofi Aventis S.A.Requer receita médicaForma farmacêutica: INJETÁVEL, 120 mg (12000 UI) /0,8 mlSubstância ativa: enoxaparinFabricante: Sanofi Aventis S.A.Requer receita médicaForma farmacêutica: INJETÁVEL, 150 mg (15000 UI) /1 mlSubstância ativa: enoxaparinFabricante: Sanofi Aventis S.A.Requer receita médica
Alternativas a CLEXANE 6.000 UI (60 mg)/0,6 ml SOLUÇÃO INJETÁVEL EM SERINGA PREENCHIDA noutros países
As melhores alternativas com o mesmo princípio ativo e efeito terapêutico.
Alternativa a CLEXANE 6.000 UI (60 mg)/0,6 ml SOLUÇÃO INJETÁVEL EM SERINGA PREENCHIDA em Polónia
Alternativa a CLEXANE 6.000 UI (60 mg)/0,6 ml SOLUÇÃO INJETÁVEL EM SERINGA PREENCHIDA em Ukraine
Médicos online para CLEXANE 6.000 UI (60 mg)/0,6 ml SOLUÇÃO INJETÁVEL EM SERINGA PREENCHIDA
Avaliação de posologia, efeitos secundários, interações, contraindicações e renovação da receita de CLEXANE 6.000 UI (60 mg)/0,6 ml SOLUÇÃO INJETÁVEL EM SERINGA PREENCHIDA – sujeita a avaliação médica e regras locais.














