
GLUCOSALINO HIPERTONICO PHYSAN SOLUTION FOR INFUSION

How to use GLUCOSALINO HIPERTONICO PHYSAN SOLUTION FOR INFUSION
Translated with AI
This page provides general information and does not replace a doctor’s consultation. Always consult a doctor before taking any medication. Seek urgent medical care if symptoms are severe.
Show originalContents of the leaflet
- Introduction
- What is Glucosalino Hipertónico Physan and what is it used for
- What you need to know before you start using Glucosalino Hipertónico Physan
- How to use Glucosalino Hipertónico Physan
- Possible side effects
- Storage of Glucosalino Hipertónico Physan
- Container Content and Additional Information
Introduction
Package Leaflet: Information for the User
Glucosalino Hipertónico Physan Solution for Infusion
Sodium Chloride, Anhydrous Glucose
Read all of this leaflet carefully before you start using this medicine, because it contains important information for you.
- Keep this leaflet, you may need to read it again.
- If you have any further questions, ask your doctor, pharmacist, or nurse.
- If you experience any side effects, talk to your doctor, pharmacist, or nurse, even if they are not listed in this leaflet. See section 4.
Contents of the Package Leaflet
- What is Glucosalino Hipertónico Physan and what is it used for
- What you need to know before you start using Glucosalino Hipertónico Physan
- How to use Glucosalino Hipertónico Physan
- Possible side effects
- Storage of Glucosalino Hipertónico Physan
- Contents of the pack and other information
1. What is Glucosalino Hipertónico Physan and what is it used for
Glucosalino Hipertónico Physan belongs to the group of medicines called solutions that affect the electrolyte balance. Electrolytes associated with carbohydrates.
It is used as a supply of salts and water in cases where there is dehydration with moderate loss of salts and water: vomiting, diarrhea, fistulas, excessive sweating, in cases where administration of water, carbohydrates, and salts is needed, and altered sugar metabolism: ketonemic vomiting, insulin coma.
2. What you need to know before you start using Glucosalino Hipertónico Physan
Do not use Glucosalino Hipertónico Physan:
If you are allergic to sodium chloride, anhydrous glucose, or any of the other components of this medicine (listed in section 6).
If you have:
- Extracellular hyperhydration or hypervolemia
- Fluid and sodium retention
- Severe kidney disease
- Heart disease
- Hypernatremia (excess sodium in the blood)
- Hyperchloremia (excess chloride in the blood)
- General edema or ascitic cirrhosis
- It should not be administered in the 24 hours following a head injury.
- Uncontrolled diabetes or other known glucose intolerance, hyperosmolar coma, hyperglycemia, and hyperlactacidemia.
Warnings and precautions
Consult your doctor, pharmacist, or nurse before starting to use Glucosalino Hipertónico Physan.
The solution is hypertonic with an approximate osmolarity of 586 mosmol/l.
Perfusion of large volumes should be done under specific monitoring in patients with heart, lung, or kidney failure.
If you have cardiovascular decompensation or are receiving treatment with corticosteroids or corticotropin.
Sodium salts should be administered with caution to patients with hypertension, heart failure, peripheral or pulmonary edema, renal dysfunction, preeclampsia, or other conditions associated with sodium retention.
Due to immature renal function, premature and full-term infants may retain excess sodium. Therefore, in premature and full-term infants, repeated infusions of sodium chloride should only be given after determining serum sodium levels.
Perfusion of glucose solutions is contraindicated in the first 24 hours after head injury, and blood glucose concentration should be carefully monitored during episodes of intracranial hypertension.
In case of acute ischemic attacks (decreased or absent circulation in arteries), since hyperglycemia has been related to increased ischemic brain damage and difficulty in recovery.
If you have diabetes or kidney disease, your doctor may request blood tests to monitor your condition, as it is necessary to control the balance of water, glucose, and salts in the body.
In diabetes, glucose solutions can be used as long as appropriate treatment (insulin) has been established. Blood glucose should be regularly monitored in diabetic patients and insulin requirements modified.
If hyperglycemia occurs, the perfusion rate should be adjusted or insulin administered.
In prolonged treatments, the patient should be provided with adequate nutritional treatment.
To avoid hypokalemia produced during prolonged parenteral administration of glucosaline, potassium may be added to the glucosaline solution as a safety measure.
Do not administer blood simultaneously using the same infusion equipment due to the risk of pseudoagglutination and/or hemolysis.
Glucose solutions for intravenous infusion are generally isotonic. However, in the body, glucose solutions can become extremely hypotonic physiologically due to the rapid metabolism of glucose.
Depending on the tonicity of the solution, the volume and rate of perfusion, and the patient's initial clinical condition and ability to metabolize glucose, intravenous administration of glucose can cause electrolyte disturbances, the most important of which is hyperosmolar hypnatremia.
Hyponatremia:
Patients with non-osmotic release of vasopressin (e.g., in critical states, pain, postoperative stress, infections, burns, and CNS diseases), patients with heart, liver, and kidney disease, and patients exposed to vasopressin agonists are at special risk of experiencing acute hyponatremia after perfusion of hypotonic solutions.
Acute hyponatremia can cause acute hypnatremic encephalopathy (brain edema) characterized by headache, nausea, seizures, lethargy, and vomiting. Patients with brain edema are at special risk of suffering severe, irreversible, and potentially fatal brain damage.
Children, women of childbearing age, and patients with reduced cerebral distensibility (e.g., in cases of meningitis, intracranial hemorrhage, and brain contusion) are at special risk of suffering severe and potentially fatal brain edema caused by acute hyponatremia.
Using Glucosalino Hipertónico Physan with other medicines
Tell your doctor or pharmacist if you are using, have recently used, or might use any other medicines.
Sodium chloride interacts with lithium salts, whose renal excretion is directly proportional to sodium levels in the body. Thus, administration of solutions containing sodium chloride can accelerate renal excretion of lithium, leading to a decrease in its therapeutic effect.
Glucose solutions can reduce the therapeutic effect of insulin or oral antidiabetics (biguanides, sulfonylureas).
Administration with corticosteroids can lead to high glucose levels (hyperglycemic effect) and water and sodium retention.
If glucose administration coincides with treatment with digitalis glycosides (digoxin), an increase in digitalis activity can occur, with a risk of developing intoxication due to hypokalemia that can be caused by administration of this solution if potassium is not added.
Glucose solutions should not be administered through the same infusion equipment as whole blood, due to the risk of hemolysis and agglutination.
In any case, the doctor should check the compatibility of the added medicines.
Medicines that potentiate the effect of vasopressin
The following medicines increase the effect of vasopressin, which reduces renal excretion of water without electrolytes and increases the risk of hospital hyponatremia after inadequately balanced treatment with intravenous infusion solutions.
- Medicines that stimulate the release of vasopressin; e.g.: chlorpropamide, clofibrate, carbamazepine, vincristine, selective serotonin reuptake inhibitors, 3,4-methylenedioxy-N-methamphetamine, ifosfamide, antipsychotics, narcotics
- Medicines that potentiate the action of vasopressin; e.g.: chlorpropamide, non-steroidal anti-inflammatory drugs, cyclophosphamide
- Vasopressin analogues; e.g.: desmopressin, oxytocin, vasopressin, terlipressin
Other medicines that are known to increase the risk of hyponatremia are diuretics in general and antiepileptics such as oxcarbazepine.
Pregnancy and breastfeeding
Glucosalino Hipertónico Physan should be administered with special caution in pregnant women during labor, especially if administered in combination with oxytocin, due to the risk of hyponatremia.
If you are pregnant or breastfeeding, think you may be pregnant, or are planning to have a baby, ask your doctor or pharmacist for advice before using this medicine.
Provided that administration is correct and controlled, no adverse effects are expected during pregnancy and breastfeeding.
Currently, there are no relevant epidemiological data available, so it is recommended that if used during this period, it should be done with caution.
Driving and using machines:
This is not applicable, due to the characteristics of its use.
3. How to use Glucosalino Hipertónico Physan
Your doctor will indicate the most suitable dose for your needs. It is usually recommended to administer intravenously, drop by drop, according to your age, weight, clinical situation, and metabolic state.
The recommended dosage is:
-for adults, elderly, and adolescents: 500 ml to 3 liters every 24 hours.
-for infants and children:
from 0 to 10 kg of body weight: 100 ml/kg/24 h.
from 10 to 20 kg of body weight: 1000 ml + (50 ml/kg above 10 kg)/24 h.
>20 kg of body weight: 1500 ml + (20 ml/kg above 20 kg)/24 h.
The perfusion rate is normally 40 ml/kg/24 h in adults, elderly, and adolescents.
In pediatric patients, the perfusion rate is 5 ml/kg/h on average, but this value varies with age: 6-8 ml/kg/h for children under 12 months, 4-6 ml/kg/h for children from 12 to 23 months, and 2-4 ml/kg/h for school-age children (2-11 years).
The perfusion rate should not exceed the patient's glucose oxidation capacity in order to avoid hyperglycemia (excess sugar in the blood). Therefore, the maximum dose ranges from 5 mg/kg/min for adults to 10-18 mg/kg/min for infants and children, depending on age and total body mass.
If administered continuously in the same infusion site, thrombophlebitis (inflammation of the veins) may occur.
Special attention should be paid if used in elderly patients, as they may have affected liver and/or kidney function.
Sodium salts should be administered with caution to patients with hypertension, heart failure, peripheral or pulmonary edema, renal dysfunction, convulsions, or other conditions associated with sodium retention.
It is recommended that controls of water, salt, and glucose balance be performed, especially if there is cardiovascular decompensation or if treatment with corticosteroids or corticotropin is received.
If you have been administered more Glucosalino Hipertónico Physan solution for infusion than you should have:
- In case of overdose, hyperglycemia (high blood sugar concentration), glucosuria (sugar in urine), hyperhydration, or hypernatremia (high sodium concentration in the blood) and generalized edema (fluid accumulation) may occur. Administration will be discontinued, and symptomatic treatment will be provided.
- Prolonged or rapid administration of large volumes of glucose-containing solutions can lead to hyperosmolarity (risk of loss of consciousness or mental confusion), dehydration, hyperglycemia, hyperglycosuria, and osmotic diuresis (due to hyperglycemia).
- Hyperglycemia should be especially monitored in severe cases of diabetes mellitus, and can be avoided by reducing the dose and perfusion rate or administering insulin.
- Abuse or too rapid administration can lead to an excess of water and sodium (hypernatremia) with a risk of edema, particularly when there is defective renal excretion of sodium. In this case, extrarenal dialysis may be necessary.
- Rarely, hypernatremia occurs after therapeutic doses of sodium chloride. The most serious effect of hypernatremia is dehydration of the brain, causing somnolence and confusion that progresses to seizures, coma, respiratory failure, and death. Other symptoms include reduced thirst, salivation, and lacrimation, fever, tachycardia, hypertension, headache, dizziness, fatigue, irritability, and weakness.
- Excessive administration of chloride salts can produce a loss of bicarbonate with an acidifying effect.
In case of overdose or accidental ingestion, consult the Toxicology Information Service. Telephone: 915 620 420.
4. Possible side effects
Like all medicines, this medicine can cause side effects, although not everybody gets them.
When administering this solution, it has been observed that hyperhydration (fluid retention) and heart failure in patients with heart disease or pulmonary edema, and asymptomatic electrolyte disturbances, occur frequently.
Too rapid administration can cause hyperglycemia and hyperosmolar syndrome (risk of loss of consciousness or mental confusion), especially in glucose intolerant patients.
Adverse reactions can be associated with the administration technique, including fever, infection at the injection site, local reaction or pain, venous irritation, venous thrombosis, or phlebitis extending from the injection site, extravasation, and hypervolemia.
Adverse reactions can be associated with the medicines added to the solution; the nature of the added medicine will determine the possibility of any other undesirable effect.
Adverse reactions
Metabolic and nutritional disorders with hospital hyponatremia** of unknown frequency.
Nervous system disorders with hypnatremic encephalopathy** of unknown frequency.
** Hospital hyponatremia can cause irreversible brain damage and death due to the occurrence of acute hypnatremic encephalopathy.
Reporting of side effects
If you experience any side effects, talk to your doctor, pharmacist, or nurse, even if they are not listed in this leaflet. You can also report them directly through the Spanish Pharmacovigilance System for Human Use Medicines: www.notificaRAM.es. By reporting side effects, you can help provide more information on the safety of this medicine.
5. Storage of Glucosalino Hipertónico Physan
Keep this medicine out of the sight and reach of children.
Glass vials: No special storage conditions are required.
Polypropylene vials: Store below 30°C.
Do not use this medicine after the expiry date stated on the label after EXP. The expiry date is the last day of the month indicated.
Do not use this medicine if you notice visible signs of deterioration.
Medicines should not be disposed of via wastewater or household waste. Ask your pharmacist how to dispose of medicines no longer required. This will help protect the environment.
6. Container Content and Additional Information
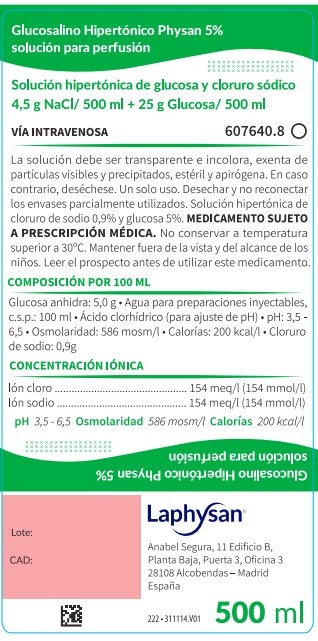
Composition of Glucosalino Hipertónico Laphysan
- The active ingredients are: per 100 ml, sodium chloride 0.9g, anhydrous glucose 5g.
- The other components (excipients) are: water for injectable preparations and hydrochloric acid (for pH adjustment).
The electrolyte composition is:
Sodium ion 154 mmol/l, (154 meq/l).
Chloride ion 154 mmol/l, (154 meq/l).
Theoretical osmolality: 586 mosm/l.
Theoretical calories: 200 kcal/l.
pH: 3.5-6.5.
Appearance of the Product and Container Content
Transparent and colorless solution, without visible particles, sterile and apyrogenic.
Glucosalino Hipertónico Physan is a solution for perfusion that comes in containers of 100 ml containing 50 ml or 100 ml of solution, containers of 250 ml, 500 ml, and 1000 ml.
It is presented in type II glass vials, Polypropylene vials (Flip Off cap), Polypropylene vials (twin head cap), with the following capacities:
- Vials of 100 ml containing 50 ml or 100 ml of solution.
- Vials of 250 ml
- Vials of 500 ml
- Vials of 1000 ml.
Clinical containers are also available with the following presentations:
- 30 vials of 100 ml containing 50 ml or 100 ml of solution.
- 24 vials of 250 ml
- 10 vials of 500 ml
- 20 vials of 500 ml
- 10 vials of 1000 ml.
Marketing Authorization Holder and Manufacturer
Marketing Authorization Holder:
LAPHYSAN, S.A.U.
Anabel Segura, 11 Edificio A, Planta 4, Puerta D
28108 Alcobendas – Madrid, Spain
Manufacturer:
S.M. FARMACEUTICI SRL
Zona industriale
85050 TITO – POTENZA, Italy
or
Laboratórios Basi - Indústria Farmacêutica S.A.
Parque Industrial Manuel Lourenço Ferreira, Lotes 8, 15 e 16
3450-232 Mortágua
Portugal
Date of the Last Revision of this Prospectus:October 2022
------------------------------------------------------------------------------------------------------
This information is intended only for healthcare professionals:
This medication will always be administered by specialized personnel. It will be administered by perfusion, through a central or peripheral vein.
The solution must be transparent, without particles, and not contain precipitates. Do not administer otherwise.
The content of each vial is for a single perfusion, the unused fraction must be discarded.
Use an aseptic method to administer the solution and in case of preparation of mixtures.
Before adding medications to the solution or administering simultaneously with other medications, it must be checked that there are no incompatibilities.
Discard after a single use.
Discard partially used containers.
Do not reconnect partially used containers.
It may be necessary to monitor the fluid balance, serum glucose, serum sodium, and other electrolytes
before and during administration, especially in patients with increased non-osmotic release of vasopressin (syndrome of inappropriate antidiuretic hormone secretion, SIADH) and in patients who receive concomitant medication with vasopressin agonists due to the risk of hyponatremia.
Monitoring of serum sodium is especially important when administering physiologically hypotonic solutions. Glucosalino hipertónico Physan can become extremely hypotonic after administration due to the metabolism of glucose in the body.
- Country of registration
- Active substance
- Prescription requiredYes
- Manufacturer
- This information is for reference only and does not constitute medical advice. Always consult a doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to GLUCOSALINO HIPERTONICO PHYSAN SOLUTION FOR INFUSIONDosage form: INJECTABLE INFUSION, 0.09 g / 0.07 g / 1.6 g / 0.17 g / 12.5 g / 0.19 g / 1.23 gActive substance: electrolytes with carbohydratesManufacturer: Fresenius Kabi España, S.A.U.Prescription requiredDosage form: INJECTABLE PERFUSION, 0.31 g / 21.9 mg / 0.03 g / 0.6 gActive substance: electrolytes with carbohydratesManufacturer: Fresenius Kabi España, S.A.U.Prescription requiredDosage form: INJECTABLE PERFUSION, NAActive substance: electrolytes with carbohydratesManufacturer: Fresenius Kabi España, S.A.U.Prescription required
Online doctors for GLUCOSALINO HIPERTONICO PHYSAN SOLUTION FOR INFUSION
Discuss questions about GLUCOSALINO HIPERTONICO PHYSAN SOLUTION FOR INFUSION, including use, safety considerations and prescription review, subject to medical assessment and local regulations.
Frequently Asked Questions















