
GLUCOSA BAXTER 10% PERFUSION SOLUTION

How to use GLUCOSA BAXTER 10% PERFUSION SOLUTION
Translated with AI
This page provides general information and does not replace a doctor’s consultation. Always consult a doctor before taking any medication. Seek urgent medical care if symptoms are severe.
Show originalContents of the leaflet
Introduction
Package Leaflet: Information for theuser
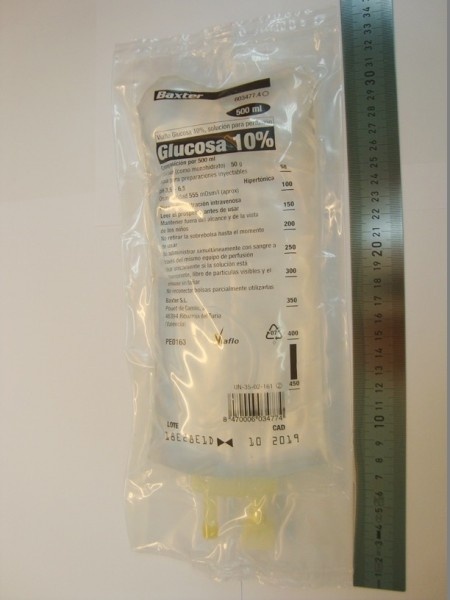
Glucose Baxter 10%solution for infusion
Active ingredient: Glucose
Read all of this leaflet carefully before you start using this medicine, because it contains important information for you.
- Keep this leaflet, you may need to read it again.
- If you have any further questions, ask your doctor, pharmacist, or nurse.
- If you experience side effects, consult your doctor, pharmacist, or nurse, even if they are not listed in this leaflet. See section 4.
This medicine is called “Glucose Baxter 10% solution for infusion”, but will be referred to as “Glucose Baxter 10%” throughout this leaflet.
Contents of the package leaflet:
- What is Glucose Baxter 10% and what is it used for
- What you need to know before you are given Glucose Baxter 10%
- How Glucose Baxter 10% will be given to you
- Possible side effects
- Storage of Glucose Baxter 10%
- Contents of the pack and further information
1. What is Glucose Baxter 10% and what is it used for
Glucose Baxter 10% is a solution of sugar (glucose) in water. Glucose is one of the main sources of energy for the body. This solution for infusion provides 400 kilocalories per liter.
Glucose Baxter 10% is used to:
- provide a source of sugar (carbohydrates) alone or, if required, for parenteral nutrition. Parenteral nutrition is used to feed patients who cannot eat. It is given through a slow injection (infusion) into a vein.
- prevent or treat low blood sugar levels (hypoglycemia, which causes symptoms but is not fatal).
- provide the patient with extra fluid when the body does not have enough water (dehydration) and you need extra sugar (carbohydrates).
- dilute other medicines with water that are to be given intravenously.
2. What you need to know before you are given Glucose Baxter 10%
You will not be given Glucose Baxter 10% if you have any of the following conditions:
- if you have diabetes that is not being treated, so that your blood glucose levels are higher than normal (uncontrolled diabetes),
- loss of consciousness (hyperosmolar coma). This is a type of coma that can occur if you have diabetes and are not receiving adequate medication,
- thinning of the blood due to the addition of too much fluid (hemodilution),
- when there is too much fluid in the body's extracellular spaces (extracellular hyperhydration),
- when there is more blood volume in the blood vessels than there should be (hypervolemia),
- high blood glucose levels (hyperglycemia),
- high blood lactate levels (hyperlactatemia),
- severe kidney failure (when the kidneys are not working well and dialysis is needed)
- uncompensated heart failure. If heart failure has not been treated adequately and causes symptoms such as:
- difficulty breathing,
- swelling of the ankles,
- if there is fluid accumulation under the skin, affecting the entire body, including the brain and lungs (generalized edema),
- liver disease that causes fluid accumulation in the abdomen (ascitic cirrhosis),
- any other condition that affects how your body controls blood sugar levels,
- intolerance (hypersensitivity) to glucose. This can occur in patients with corn allergies.
If another medicine is added to your infusion solution, read its package leaflet. This will ensure that you can take that medicine.
Warnings and precautions
Glucose Baxter 10% is a hypertonic (concentrated) solution. Your doctor will take this into account when calculating the amount of solution to be administered.
If you develop or have developed any of the following conditions, inform your doctor.
- Diabetes,
- kidney failure,
- a life-threatening illness (critical acute illness),
- tell your doctor if you have had a head injury in the last 24 hours,
- increased pressure inside the skull (intracranial hypertension),
- stroke due to a blood clot in a blood vessel (cerebral stroke),
- heart disease (heart failure),
- lung disease (respiratory failure),
- reduced urine production (oliguria or anuria),
- excess water in the body (water intoxication),
- low sodium levels in the blood (hyponatremia),
- allergy to corn (Glucose Baxter 10% contains corn-derived sugar).
- If you have a condition that could cause high levels of vasopressin, a hormone that regulates your body's fluid. You may have too much vasopressin in your body because, for example:
- you have had a sudden and severe illness,
- you are in pain,
- you have had surgery,
- you have infections, burns, or head injuries
- you have diseases related to your heart, liver, kidneys, or central nervous system,
- you are taking certain medications (see Other medicines and Glucose Baxter 10%).
This can increase the risk of low sodium levels in the blood and can cause headache, nausea, seizures, lethargy, coma, brain inflammation, and death. Brain inflammation increases the risk of death and brain damage. People at higher risk of brain inflammation are:
- children
- women (particularly if they are of childbearing age)
- people who have problems with their brain fluid levels, for example, due to meningitis, bleeding in the skull, or a head injury.
When you receive this infusion, your doctor will monitor:
- the amount of electrolytes such as sodium and potassium in your blood (plasma electrolytes),
- the amount of sugar (glucose),
- the amount of fluid in your body (fluid balance),
- the acidity of your blood and urine (acid-base balance).
Your doctor will adjust the amount of infusion solution to be administered according to the results of the tests. These tests will indicate to the doctor if you need additional potassium, a blood chemical. If necessary, it can be administered intravenously.
Since Glucose Baxter 10% contains sugar (glucose), it can cause high blood sugar levels (hyperglycemia). If this occurs, the doctor may:
- adjust the infusion rate,
- administer insulin to reduce blood sugar levels,
- if necessary, administer more potassium.
This is very important:
- if you have diabetes,
- if your kidneys are not working as well as normal,
- if you have recently had a stroke (acute ischemic stroke). High blood sugar levels can worsen the effects of the stroke and affect recovery,
- if you have metabolic disorders due to starvation or a diet that does not provide the proper proportion of necessary nutrients (malnutrition),
- if you have low thiamine (vitamin B1) levels. This can occur if you suffer from chronic alcoholism.
This solution will not be administered using the same needle as a blood transfusion, as it could damage red blood cells or cause them to clump.
Children
Glucose Baxter 10% should be administered with special care in children.
Children should receive Glucose Baxter 10% from a doctor or nurse. The amount administered will be determined by a doctor specializing in pediatric treatment and will depend on the child's age, weight, and condition. If it is used to administer or dilute another medicine, or if other medicines are administered at the same time, the dose may also be affected.
When administering the infusion to children, the doctor will take blood and urine samples to monitor the amount of electrolytes such as potassium in the blood (plasma electrolytes).
Newborns - especially premature and low-birth-weight babies - are at higher risk of developing low or high blood sugar levels (hypo- or hyperglycemia). Therefore, they need close monitoring during treatment with intravenous glucose solutions to ensure adequate blood sugar level control and prevent potential long-term adverse effects. Low blood sugar levels in newborns can cause prolonged seizures, coma, and brain damage. High blood sugar levels can cause brain hemorrhages, bacterial or fungal infections, eye damage (retinopathy of prematurity), intestinal infections (necrotizing enterocolitis), lung problems (bronchopulmonary dysplasia), prolonged hospital stay, and death.
When administering to a newborn, the solution bag may be connected to an infusion pump device, which allows for the exact administration of the necessary amount over a defined time interval. Your doctor or nurse will monitor the device to ensure safe administration.
Children (including neonates and older children) who receive Glucose Baxter 10% are at higher risk of having low sodium levels in the blood (hyponatremic hypoosmotic syndrome) and a brain disorder due to low plasma sodium levels (hyponatremic encephalopathy).
Other medicines and Glucose Baxter 10%
Tell your doctor or nurse if you are using, have recently used, or might use any other medicines.
Glucose Baxter 10% and any other medicine taken at the same time may affect each other.
Do not use Glucose Baxter 10% with certain hormones (catecholamines) including adrenaline or steroids, as they increase blood sugar levels.
Some medicines affect the vasopressin hormone. These may include:
- antidiabetic medication (chlorpropamide)
- cholesterol medication (clofibrate)
- certain cancer medications (vincristine, ifosfamide, cyclophosphamide)
- selective serotonin reuptake inhibitors (used to treat depression)
- antipsychotics
- opioids for severe pain relief
- medicines for pain and/or inflammation (also known as NSAIDs)
- medicines that mimic or enhance the effects of vasopressin, such as desmopressin (used to treat increased thirst and urination), terlipressin (used to treat esophageal bleeding), and oxytocin (used to induce labor)
- antiepileptic medications (carbamazepine and oxcarbazepine)
- diuretics
Using Glucose Baxter 10% with food and drinks
You should ask your doctor what you can eat or drink.
Pregnancy, breastfeeding, and fertility
If you are pregnant or breastfeeding, think you may be pregnant, or plan to become pregnant, consult your doctor before using this medicine.
Pregnancy
Glucose Baxter 10% can be used during pregnancy. However, caution should be exercised when using a glucose solution during labor.
Fertility
There is not enough data on the effect of glucose on fertility, although no effect is expected.
Breastfeeding
There is not enough data on the use of a glucose solution during breastfeeding, although no effect is expected. Glucose Baxter 10% can be used during breastfeeding.
However, if another medicine is added to the infusion solution during pregnancy or breastfeeding, you should:
- Consult your doctor.
- Read the package leaflet of the medicine to be added.
Driving and using machines
Consult your doctor or nurse before driving or using machines.
3. How Glucose Baxter 10% will be given to you
Glucose Baxter 10% will be administered to you by a doctor or nurse. Your doctor will decide how much you need and when it should be administered. This will depend on your age, weight, physical condition, and the reason for treatment. The amount you receive may also be influenced by other treatments you are receiving.
You must not receive Glucose Baxter 10% if there are particles floating in the solution or if the container is damaged in any way.
Glucose Baxter 10% is usually administered through a plastic tube attached to a needle inserted into a vein. A vein in the arm is usually used to administer the infusion. However, your doctor may administer the medicine in another way.
Before and during the infusion, your doctor will monitor:
- the amount of fluid in your body
- the acidity of your blood and urine
- the amount of electrolytes in your body (particularly sodium, in patients with high levels of the vasopressin hormone, or those taking other medicines that increase the effect of vasopressin).
Any unused solution should be discarded. You must not receive Glucose Baxter 10% from a started bottle.
If you receive more Glucose Baxter 10% than you should
If you receive too much Glucose Baxter 10% (overdose) or if it is administered too quickly or too frequently, the following symptoms may occur:
- fluid accumulation in the tissues, causing swelling (edema) or water intoxication, with lower than normal sodium levels in the blood (hyponatremia),
- higher than normal blood sugar levels (hyperglycemia),
- excessive blood concentration (hyperosmolarity),
- glucose in the urine (glucosuria),
- increased urine production (osmotic diuresis),
- water loss in the body (dehydration),
If you experience any of these symptoms, inform your doctor immediately. Your infusion will be stopped or the infusion rate will be reduced. Insulin will be administered, and you will receive treatment according to the symptoms.
If another medicine has been added to Glucose Baxter 10% before the overdose, that medicine may also cause symptoms. You should read the list of possible symptoms in the package leaflet of the added medicine.
If you stop the infusion with Glucose Baxter 10%
Your doctor will decide when you should stop this infusion.
If you have any further questions about the use of this product, ask your doctor or nurse.
4. Possible side effects
Like all medicines, this medicine can cause side effects, although not everybody gets them.
Side effects may include:
- Hypersensitivity reactions, including a severe allergic reaction called anaphylaxis (potential manifestation in patients with corn allergies),
- difficulty breathing,
- swelling of the face and lips or throat inflammation,
- fever,
- hives (urticaria),
- skin rash,
- redness of the skin (cutaneous erythema),
- chills,
- changes in blood electrolyte levels (electrolyte disturbances), including
- low sodium levels in the blood that can be acquired during hospitalization (nosocomial hyponatremia) and related neurological disorder (acute hyponatremic encephalopathy). Hyponatremia can cause irreversible brain damage and death due to brain edema/inflammation (see also the section “Warnings and precautions”).
- low potassium levels in the blood (hypokalemia),
- low magnesium levels in the blood (hypomagnesemia),
- low phosphate levels in the blood (hypophosphatemia),
- high blood sugar levels (hyperglycemia),
- excess fluid in the blood vessels (hemodilution and hypervolemia),
- glucose in the urine (glucosuria),
- reactions related to the administration route:
- fever, febrile reaction (pyrexia),
- infection at the injection site,
- leakage of the infusion solution into the tissues surrounding the vein (extravasation). This can damage tissues and cause scarring,
- blood clot formation (thrombosis) at the infusion site, causing pain, inflammation, or redness in the area of the clot,
- irritation and inflammation of the vein through which the infusion is administered (phlebitis). This can cause redness, pain, or itching or swelling in the infusion vein,
- local reaction or pain (redness or swelling at the infusion site),
- sweating.
If another medicine has been added to the infusion solution, it may also cause side effects. These will depend on the added medicine. You should read the package leaflet of that medicine to get a list of possible symptoms.
If a side effect occurs, the infusion should be stopped.
Reporting side effects
If you experience any side effects, consult your doctor, pharmacist, or nurse, even if they are not listed in this leaflet. You can also report them directly through the Spanish Medicines Monitoring System for Human Use: https://www.notificaram.es. By reporting side effects, you can help provide more information on the safety of this medicine.
5. Storage of Glucose Baxter 10%
Keep this medicine out of the sight and reach of children.
Do not store above 25°C.
Glucose Baxter 10% should not be administered after the expiry date stated on the bag and carton after “EXP”. The expiry date is the last day of the month shown.
Glucose Baxter 10% should not be administered if there are particles floating in the solution or if the unit is damaged in any way.
6. Container Contents and Additional Information
Composition ofBaxter Glucose 10%
The active ingredient is glucose (as monohydrate): 100 g per liter.
The only other component is water for injectable preparations.
Formula per 250 ml
Glucose (as monohydrate): 25 g
Formula per 500 ml
Glucose (as monohydrate): 50 g
Formula per 1000 ml
Glucose (as monohydrate): 100 g
Appearance of Baxter Glucose 10% and Container Contents
Baxter Glucose 10% is a clear solution, without visible particles. It is presented in type II glass vials. Each vial is closed by a type I chlorobutyl stopper, which is covered with an aluminum cap.
The vial sizes are: 250 ml, 500 ml, or 1000 ml.
The vials are supplied in boxes, each containing the following quantities:
- 1 vial of 250 ml
- 10 vials of 500 ml
- 1 vial of 500 ml
- 1 vial of 1000 ml
Only some package sizes may be marketed.
Marketing Authorization Holder and Manufacturers
Marketing Authorization Holder:
Baxter, S.L.
Pouet de Camilo 2, 46394 Ribarroja del Turia (Valencia)
Spain
Manufacturer:
Bieffe Medital S.p.A.
Via Nuova Provinciale
23034 Grosotto (SO)
Italy
Date of Last Revision of this Leaflet: June 2019
Detailed and updated information on this medicinal product is available on the website of the Spanish Agency for Medicines and Health Products (AEMPS) http://www.aemps.gob.es/
This information is intended only for healthcare professionals:
Handling and Preparation
The solution for infusion should be visually inspected before use.
Parenteral solutions should be inspected visually for particles and discoloration before administration, whenever the solution and container permit. Use the vial only if the solution is clear, does not contain visible particles, and the container is not damaged. It should be administered immediately after insertion of the infusion equipment.
The solution should be administered with sterile equipment using an aseptic technique. The equipment should be primed with the solution to prevent air from entering the system.
The addition of electrolytes may be indicated based on the patient's clinical needs.
Medications can be added before infusion or during it through the injection port. When used, the final osmolarity should be checked before parenteral administration. The mixture should be aseptic and performed carefully and meticulously. Solutions containing added medications should not be stored and should be used immediately.
In order to avoid a potentially fatal overdose during the infusion of intravenous solutions in newborns, special attention should be paid to the administration method. When using a syringe pump to administer fluids or medications intravenously to newborns, a liquid vial should not be left connected to the syringe.
When using an infusion pump, all clamps on the intravenous administration equipment should be closed before removing the administration set from the pump or changing it. This is required regardless of whether the administration equipment has an anti-free flow device.
The complete device equipment and its administration via infusion should be frequently monitored.
Discard after single use.
Discard unused remnants.
Do not reconnect partially used vials.
Do not store solutions containing other medications.
An aseptic technique should be used when adding medications to Baxter Glucose 10%.
Mix the solution well when adding medications.
- To open
- Remove the aluminum cap that protects the closure
- Check the transparency of the solution and the absence of foreign particles. Discard the solution if it is not transparent or contains foreign particles.
- Preparation for administration
Use sterile material for preparation and administration.
- Hang the container by the hanger that accompanies the shipping box.
- Use an antisepsis method to prepare the infusion.
- Connect the administration equipment. Consult the instructions accompanying the equipment for connection, priming, and administration of the solution.
- Techniques for injecting added medications
Warning: Added medications may be incompatible.
To add medication before administration
- Disinfect the injection point.
- Using a syringe with a 19 (1.10 mm) to 22 (0.70 mm) gauge needle, puncture the resealable injection point and inject.
- Mix the medication and solution carefully. For high-density medications, such as potassium chloride, gently move the tubes while in a vertical position and mix.
Precaution: Do not store vials with added medication.
To add medication during administration
- Close the equipment clamp.
- Disinfect the injection point.
- Using a syringe with a 19 (1.10 mm) to 22 (0.70 mm) gauge needle, puncture the resealable injection point and inject.
- Remove the container from the intravenous support and/or turn it to put it in a vertical position.
- Mix the solution and medication carefully.
- Put the container back in the operating position, reopen the clamp, and continue with the administration.
- In-use stability (added medications)
The chemical and physical stability of added medications in the pH of Baxter Glucose 10% in the glass vial should be determined before use.
From a microbiological point of view, the diluted product should be used immediately unless the reconstitution has been carried out under controlled and validated aseptic conditions. If not used immediately, the storage conditions and times are the responsibility of the user.
- Incompatibilities of added medications
The glucose solution should not be administered simultaneously with, before, or after a blood transfusion through the same infusion equipment, as hemolysis and clot formation may occur.
The incompatibility of medications to be added with Baxter Glucose 10% should be evaluated before adding them.
In the absence of incompatibility studies, this product should not be mixed with others.
The leaflet of the medication to be added should be consulted.
Before adding a medication, verify that it is soluble and stable in water within the pH range of Baxter Glucose 10% (pH 3.5 to 6.5).
When compatible medication is added to Baxter Glucose 10%, the solution should be administered immediately.
Incompatible added medications should not be used.
- Country of registration
- Active substance
- Prescription requiredYes
- Manufacturer
- This information is for reference only and does not constitute medical advice. Always consult a doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to GLUCOSA BAXTER 10% PERFUSION SOLUTIONDosage form: INJECTABLE INFUSION, 50 g glucoseActive substance: carbohydratesManufacturer: Fresenius Kabi España, S.A.U.Prescription requiredDosage form: INJECTABLE PERFUSION, 11 gActive substance: carbohydratesManufacturer: Fresenius Kabi España, S.A.U.Prescription requiredDosage form: INJECTABLE INFUSION, Glucose Monohydrate 5.5 gActive substance: carbohydratesManufacturer: Fresenius Kabi España, S.A.U.Prescription required
Online doctors for GLUCOSA BAXTER 10% PERFUSION SOLUTION
Discuss questions about GLUCOSA BAXTER 10% PERFUSION SOLUTION, including use, safety considerations and prescription review, subject to medical assessment and local regulations.
Frequently Asked Questions















