
ETHINYLESTRADIOL/DROSPIRENONE EXELTIS 0.02 mg/3 mg FILM-COATED TABLETS (24+4) Generic


How to use ETHINYLESTRADIOL/DROSPIRENONE EXELTIS 0.02 mg/3 mg FILM-COATED TABLETS (24+4) Generic
Translated with AI
This page provides general information and does not replace a doctor’s consultation. Always consult a doctor before taking any medication. Seek urgent medical care if symptoms are severe.
Show originalContents of the leaflet
- Introduction
- What is Ethinylestradiol/Drospirenone Exeltis and what is it used for
- What you need to know before taking Etinilestradiol/Drospirenona Exeltis
- How to take Etinilestradiol/Drospirenona Exeltis
- Possible Adverse Effects
- Storage of Ethinylestradiol/Drospirenone Exeltis
- Package Contents and Additional Information
Introduction
Package Leaflet: Information for the Patient
Ethinylestradiol/Drospirenone Exeltis 0.02 mg/3 mg film-coated tablets (24+4) EFG
Read this package leaflet carefully before you start taking this medicine because it contains important information for you
- Keep this package leaflet, you may need to read it again.
- If you have any further questions, ask your doctor, pharmacist, or nurse.
- This medicine has been prescribed for you only. Do not pass it on to others, even if they have the same symptoms as you, as it may harm them.
- If you experience any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this package leaflet. See section 4.
Important things to know about combined hormonal contraceptives (CHCs):
- They are one of the most reliable reversible contraceptive methods if used correctly.
- They slightly increase the risk of having a blood clot in the veins and arteries, especially in the first year or when you start using a combined hormonal contraceptive again after a break of 4 weeks or more.
- Be alert and see your doctor if you think you might have symptoms of a blood clot (see section 2 “Blood clots”).
Contents of the package leaflet:
- What is Ethinylestradiol/Drospirenone Exeltis and what is it used for
- What you need to know before you start taking Ethinylestradiol/Drospirenone Exeltis
Do not take Ethinylestradiol/Drospirenone Exeltis
Warnings and precautions
Blood clots
Ethinylestradiol/Drospirenone Exeltisand cancer
Irregular bleeding
What to do if you do not have your period during the placebo days
Other medicines and Ethinylestradiol/Drospirenone Exeltis
Laboratory tests
Pregnancy and breastfeeding
Driving and using machines
Ethinylestradiol/Drospirenone Exeltiscontains lactose
- How to take Ethinylestradiol/Drospirenone Exeltis
Preparation of the blister
When you can start with the first blister
If you take more Ethinylestradiol/Drospirenone Exeltisthan you should
If you forget to take Ethinylestradiol/Drospirenone Exeltis
What to do in case of vomiting or severe diarrhea
Delayed menstrual period: what you should know
Change of the first day of your menstrual period: what you should know
If you stop taking Ethinylestradiol/Drospirenone Exeltis
- Possible side effects
- Storage of Ethinylestradiol/Drospirenone Exeltis
- Contents of the pack and further information
1. What is Ethinylestradiol/Drospirenone Exeltis and what is it used for
- Ethinylestradiol/drospirenone is a contraceptive pill used to prevent pregnancy.
- Each of the 24 pink tablets contains a small amount of two different female hormones, called drospirenone and ethinylestradiol.
- The 4 white tablets do not contain active substances and are also called placebo tablets.
- Contraceptives that contain two hormones are called combined contraceptives.
2. What you need to know before taking Etinilestradiol/Drospirenona Exeltis
General considerations Before starting to take etinilestradiol/drospirenona, you should read the information about blood clots in section 2. It is particularly important that you read the symptoms of a blood clot (see section 2 "Blood clots"). Before starting to take etinilestradiol/drospirenona, your doctor will ask you some questions about your personal and family medical history. The doctor will also measure your blood pressure and, depending on your personal situation, may carry out some other tests. In this prospectus, several situations are described in which you should interrupt the use of etinilestradiol/drospirenona or in which the reliability of etinilestradiol/drospirenona may decrease. In such situations, you should not have sexual intercourse or should take additional non-hormonal contraceptive precautions, for example, use of a condom or another barrier method. Do not use the rhythm method or the temperature method. These methods may not be reliable since etinilestradiol/drospirenona alters the monthly changes in body temperature and cervical mucus. Ethinylestradiol/drospirenona, like other hormonal contraceptives, does not protect against HIV infection (AIDS) or any other sexually transmitted disease. |
Do not take Etinilestradiol/Drospirenona Exeltis
You should not take etinilestradiol/drospirenona if you have any of the conditions listed below. Inform your doctor if you have any of the conditions listed below. Your doctor will discuss with you what other form of contraception would be more suitable.
- If you have (or have ever had) a blood clot in a blood vessel of the legs (deep vein thrombosis, DVT), in the lungs (pulmonary embolism, PE) or in other organs.
- If you have ever had a heart attack or a stroke.
- If you have (or have ever had) angina pectoris (a condition that causes severe chest pain and may be the first sign of a heart attack) or a transient ischemic attack (TIA, temporary stroke symptoms).
- If you have any of the following diseases that may increase your risk of forming a blood clot in the arteries:
- Severe diabetes with blood vessel damage.
- Very high blood pressure.
- Very high levels of fat in the blood (cholesterol or triglycerides).
- A condition called hyperhomocysteinemia.
- If you know you have a disorder that affects blood clotting: for example, protein C deficiency, protein S deficiency, antithrombin III deficiency, factor V Leiden or antiphospholipid antibodies.
- If you have (or have ever had) a type of migraine called "migraine with aura".
- If you have (or have ever had) a liver disease and your liver function has not yet normalized.
- If your kidneys do not work well (renal failure).
- If you have (or have had in the past) a tumor in the liver.
- If you have (or have had in the past) or are suspected to have breast cancer or cancer of the genital organs.
- If you have vaginal bleeding, of unknown cause.
- If you need an operation or if you spend a lot of time without getting up (see section 2 "Blood clots").
- If you are allergic to etinilestradiol or drospirenona, or any of the other components of this medicine (listed in section 6). This may manifest as itching, rash or inflammation.
- Do not take etinilestradiol/drospirenona if you have hepatitis C and are taking medications that contain ombitasvir/paritaprevir/ritonavir, dasabuvir, glecaprevir/pibrentasvir or sofosbuvir/velpatasvir/voxilaprevir (see also the section "Other medicines and Etinilestradiol/Drospirenona Exeltis").
Children and adolescents
This medicine is not indicated for use in women who have not yet had their first menstrual period.
Older women
This medicine is not indicated for use after menopause.
Women with liver failure
Do not take this medicine if you suffer from liver disease. See sections "Do not take Etinilestradiol/Drospirenona Exeltis" and "Warnings and precautions".
Women with kidney failure
Do not take this medicine if you are suffering from kidney malfunction or acute kidney failure. See sections "Do not take Etinilestradiol/Drospirenona Exeltis" and "Warnings and precautions".
Warnings and precautions
When should you consult your doctor? Seek urgent medical attention
To obtain a description of the symptoms of these serious side effects, see "How to recognize a blood clot". |
In some situations, you will need to be particularly careful while using etinilestradiol/drospirenona or any other combined hormonal contraceptive and it may be necessary for your doctor to examine you periodically.
Consult your doctor if any of the following conditions develop or worsen while you are using etinilestradiol/drospirenona.
Consult your doctor before taking etinilestradiol/drospirenona:
- If a close relative has or has had breast cancer.
- If you have cancer.
- If you have any liver or gallbladder disease.
- If you have other kidney problems and are taking medications that increase blood potassium levels.
- If you have diabetes.
- If you have depression.
- If you have Crohn's disease or ulcerative colitis (chronic inflammatory bowel disease).
- If you have hemolytic uremic syndrome (HUS, a blood clotting disorder that causes kidney failure).
- If you have sickle cell anemia (a hereditary disease of red blood cells).
- If you have epilepsy (see "Other medicines and Etinilestradiol/Drospirenona Exeltis").
- If you have systemic lupus erythematosus (SLE, a disease that affects your natural defense system).
- If you have high levels of fat in the blood (hypertriglyceridemia) or a known family history of this condition. Hypertriglyceridemia has been associated with an increased risk of pancreatitis (inflammation of the pancreas).
- If you need an operation or spend a lot of time without getting up (see section 2 "Blood clots").
- If you have just given birth, you are at a higher risk of blood clots. You should ask your doctor when you can start taking etinilestradiol/drospirenona after childbirth.
- If you have inflammation of the veins that are under the skin (superficial thrombophlebitis).
- If you have varicose veins.
- If you have some diseases that appeared for the first time during pregnancy or in a previous use of sex hormones (e.g., hearing loss), a blood disease called porphyria, blistering skin rash during pregnancy (herpes gestationalis), a nervous disease in which involuntary movements appear (Sydenham's chorea).
- If you have high blood pressure during treatment, which is not controlled with medication.
- If you have or have had brownish patches (chloasma), also called "pregnancy patches", especially on the face. In this case, avoid direct exposureto the sun or ultraviolet rays while taking this medicine.
- If you have hereditary angioedema. If you experience symptoms of angioedema, such as swelling of the face, tongue and/or throat, and/or difficulty swallowing or urticaria, with possible difficulty breathing, contact a doctor immediately. Products containing estrogens may induce or worsen the symptoms of hereditary or acquired angioedema.
Blood clots
The use of a combined hormonal contraceptive like etinilestradiol/drospirenona increases your risk of having a blood clot compared to not using it. In rare cases, a blood clot can block blood vessels and cause serious problems.
Blood clots can form:
- In the veins (this is called "venous thrombosis", "venous thromboembolism" or VTE).
- In the arteries (this is called "arterial thrombosis", "arterial thromboembolism" or ATE).
Recovery from blood clots is not always complete. In rare cases, there can be serious lasting effects or, very rarely, they can be fatal.
It is important to remember that the overall risk of a harmful blood clot due to etinilestradiol/drospirenona is small.
How to recognize a blood clot
Seek urgent medical attention if you notice any of the following signs or symptoms.
Are you experiencing any of these signs? | What might you be suffering from? |
| Deep vein thrombosis |
If you are unsure, consult a doctor, as some of these symptoms such as cough or shortness of breath can be confused with a milder condition such as a respiratory infection (e.g., a "common cold"). | Pulmonary embolism |
Symptoms that occur more frequently in one eye:
| Retinal vein thrombosis (blood clot in the eye) |
| Heart attack |
Sometimes, the symptoms of a stroke can be brief, with almost immediate and complete recovery, but you should still seek urgent medical attention, as you may be at risk of having another stroke. | Stroke |
| Blood clots that block other blood vessels. |
Blood clots in a vein
What can happen if a blood clot forms in a vein?
- The use of combined hormonal contraceptives has been associated with an increased risk of blood clots in the veins (venous thrombosis). However, these side effects are rare. They occur more frequently in the first year of use of a combined hormonal contraceptive.
- If a blood clot forms in a vein in the leg or foot, it can cause deep vein thrombosis (DVT).
- If a blood clot moves from the leg and lodges in the lung, it can cause a pulmonary embolism.
- In very rare cases, a blood clot can form in a vein of another organ such as the eye (retinal vein thrombosis).
When is the risk of a blood clot in a vein higher?
The risk of a blood clot in a vein is higher during the first year in which you take a combined hormonal contraceptive for the first time. The risk may also be higher if you start taking a combined hormonal contraceptive (the same medicine or a different one) after an interruption of 4 weeks or more.
After the first year, the risk decreases, but it is always slightly higher than if you were not taking a combined hormonal contraceptive.
When you stop taking etinilestradiol/drospirenona, your risk of a blood clot returns to normal within a few weeks.
What is the risk of a blood clot?
The risk depends on your natural risk of VTE and the type of combined hormonal contraceptive you are taking.
The overall risk of a blood clot in the leg or lung (DVT or PE) with etinilestradiol/drospirenona is small.
- Out of 10,000 women who do not use a combined hormonal contraceptive and are not pregnant, about 2 will have a blood clot in a year.
- Out of 10,000 women who use a combined hormonal contraceptive that contains levonorgestrel, norethisterone or norgestimate, about 5-7 will have a blood clot in a year.
- Out of 10,000 women who use a combined hormonal contraceptive that contains drospirenona like etinilestradiol/drospirenona, between about 9 and 12 women will have a blood clot in a year.
- The risk of a blood clot will depend on your personal history (see "Factors that increase your risk of a blood clot" below).
Risk of a blood clot in a year | |
Women who do not usea combined hormonal contraceptive pill/patch/ring and are not pregnant | About 2 out of 10,000 women |
Women who use a combined hormonal contraceptive pill that contains levonorgestrel, norethisterone or norgestimate | About 5-7 out of 10,000 women |
Women who use etinilestradiol/drospirenona | About 9-12 out of 10,000 women |
Factors that increase your risk of a blood clot in a vein
The risk of a blood clot with etinilestradiol/drospirenona is small, but some conditions increase the risk. Your risk is higher:
- If you are overweight (body mass index or BMI over 30 kg/m2).
- If any of your close relatives have had a blood clot in the leg, lung or other organ at a young age (i.e., before the age of 50, approximately). In this case, you may have a hereditary disorder of blood clotting.
- If you need to have surgery or spend a lot of time without getting up due to an injury or illness or if you have a leg in a cast. You may need to stop using etinilestradiol/drospirenona several weeks before surgery or while you have reduced mobility. If you need to stop using etinilestradiol/drospirenona, ask your doctor when you can start using it again.
- As you get older (especially above 35 years).
- If you have given birth in the last few weeks.
The risk of a blood clot increases with the number of conditions you have.
Long-distance air travel (more than 4 hours) may temporarily increase the risk of a blood clot, especially if you have any of the other risk factors listed.
It is important to inform your doctor if you suffer from any of the above conditions, even if you are not sure. Your doctor may decide that you should stop using etinilestradiol/drospirenona.
If any of the above conditions change while you are using etinilestradiol/drospirenona, for example, a close relative experiences a thrombosis without known cause or you gain a lot of weight, inform your doctor.
Blood clots in an artery
What can happen if a blood clot forms in an artery?
Like a blood clot in a vein, a blood clot in an artery can cause serious problems. For example, it can cause a heart attack or a stroke.
Factors that increase your risk of a blood clot in an artery
It is important to note that the risk of a heart attack or stroke due to etinilestradiol/drospirenona is very small, but it can increase:
- With age (above 35 years).
- If you smoke. When using a combined hormonal contraceptive like etinilestradiol/drospirenona, you are advised to stop smoking. If you are unable to stop smoking and are over 35 years old, your doctor may advise you to use a different type of contraceptive.
- If you are overweight.
- If you have high blood pressure.
- If any of your close relatives have had a heart attack or stroke at a young age (less than 50 years, approximately). In this case, you may also be at higher risk of having a heart attack or stroke.
- If you or any of your close relatives have a high level of fat in the blood (cholesterol or triglycerides).
- If you have migraines, especially migraines with aura.
- If you have a heart problem (valve disorder, heart rhythm disorder called atrial fibrillation).
- If you have diabetes.
If you have one or more of these conditions or if any of them are particularly severe, the risk of a blood clot may be increased even further.
If any of the above conditions change while you are using etinilestradiol/drospirenona, for example, you start smoking, a close relative experiences a thrombosis without known cause or you gain a lot of weight, inform your doctor.
Ethinylestradiol/Drospirenona Exeltis and cancer
It has been observed that breast cancer occurs slightly more frequently in women who use combined contraceptives, but it is not known if this is due to the treatment. For example,
3. How to take Etinilestradiol/Drospirenona Exeltis
Follow exactly the administration instructions indicated by your doctor or pharmacist for this medication. In case of doubt, consult your doctor or pharmacist again.
Each blister pack contains 24 active pink pills and 4 white placebo pills.
The pills of etinilestradiol/drospirenona of two different colors are ordered. A blister pack contains 28 pills.
Take one pill of etinilestradiol/drospirenona every day, with some water if necessary. You can take the pills with or without food, but every day at approximately the same time.
Do not confuse the pills: take a pink pill for the first 24 days and then a white pill for the last 4 days. After that, you should start another blister pack immediately (24 pink pills and then 4 white pills). Therefore, there is no interval between two blister packs.
Since the composition of the pills is different, you must start with the pill from the top left corner and take the pills every day. Follow the direction of the arrows on the blister pack to take the pills in the correct order.
Preparing the blister pack
To help you follow the order of intake, each blister pack of etinilestradiol/drospirenona contains 7 self-adhesive strips with the 7 days of the week. Choose the strip of the week that starts with the day you take the first pill. For example, if you take your first pill on a Wednesday, use the strip that starts with "WED".
Stick the self-adhesive strip of the week on the top of the blister pack of etinilestradiol/drospirenona, where it says "Start". Now you will have a day marked above each pill and you can visually check if you have taken your pill. The arrows indicate the order of taking the pills.
During the 4 days when you take the placebo pills (the placebo days), you should have your period (the so-called withdrawal bleeding). It usually starts on the 2nd or 3rd day after taking the last active pink pill of etinilestradiol/drospirenona. After taking the last white pill, start the next blister pack, even if your period has not finished. This means you should start the next blister pack on the same day of the weekyou started the previous one, and your withdrawal bleeding should occur during the same days every month.
If you use etinilestradiol/drospirenona in this way, you are also protected against pregnancy during the 4 days when you take the placebo pill.
When can you start with the first blister pack
- If you have not taken any hormonal contraceptive in the previous month.
Start taking etinilestradiol/drospirenona on the first day of your cycle (i.e., the first day of your period). If you start etinilestradiol/drospirenona on the first day of your period, you are immediately protected against pregnancy. You can also start on days 2-5 of your cycle, but in that case, you should use additional contraceptive methods (e.g., condoms) during the first 7 days.
- Switching from a combined hormonal contraceptive, vaginal ring, or patch.
You should start taking etinilestradiol/drospirenona preferably the day after taking the last active pill (the last pill that contains active ingredients) of your previous contraceptive, but no later than the day after the pill-free days (or after the last inactive pill) of your previous contraceptive. When switching from a vaginal ring or patch, follow your doctor's instructions.
- Switching from a progestin-only method (mini-pill, injection, implant, or intrauterine system (IUS) of progestin).
You can switch from the mini-pill at any time; from an implant or IUS on the day of its removal; if it is an injectable, when the next injection is due. In all cases, it is recommended that you use additional contraceptive measures (e.g., condoms) during the first 7 days of pill taking.
- After an abortion or miscarriage.
Follow your doctor's recommendations.
- After having a baby.
After having a baby, you can start taking etinilestradiol/drospirenona between 21 and 28 days later. If you start later, you should use a barrier method (e.g., condoms) during the first 7 days of taking etinilestradiol/drospirenona.
If, after having a baby, you have had sexual intercourse, before starting to take etinilestradiol/drospirenona, you should be sure you are not pregnant or wait for your next period.
- If you are breastfeeding and want to start taking etinilestradiol/drospirenona (again) after having a baby.
Read the section "Breastfeeding".
Consult your doctor if you have doubts about when to start.
If you take more Etinilestradiol/Drospirenona Exeltis than you should
No cases have been reported where an overdose of etinilestradiol/drospirenona has caused serious harm.
If you take many pills at the same time, you may feel unwell, vomit, or experience vaginal bleeding. This bleeding can occur even in girls who have not yet had their first period, if they accidentally take this medication.
If you have taken too many etinilestradiol/drospirenona pills, or discover that a child has taken them, consult your doctor or pharmacist.
In case of overdose or accidental ingestion, consult your doctor or pharmacist immediately or call the Toxicology Information Service, phone: 91 562 04 20, indicating the medication and the amount ingested.
If you forget to take Etinilestradiol/Drospirenona Exeltis
The last 4 pills of the 4th rowof the blister pack are placebo pills. If you forget one of these pills, you do not lose the contraceptive effect of etinilestradiol/drospirenona. You should discard the forgotten placebo pill.
If you forget an active pink pill (pills 1-24 of the blister pack), you should follow these instructions:
- If you are less than 24 hourslate in taking a pill, the protection against pregnancy does not decrease. Take the pill as soon as you remember and the following pills at the usual time.
- If you are more than 24 hourslate in taking a pill, the protection against pregnancy may be reduced. The more pills you have forgotten, the higher the risk of becoming pregnant.
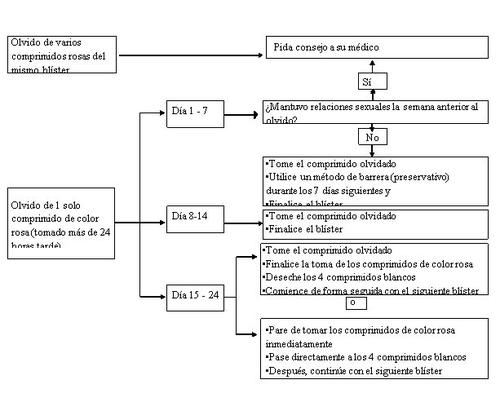
The risk of incomplete protection against pregnancy is highest if you forget to take a pink pill at the beginning or end of the blister pack. The following recommendations should be followed in this situation (see also the diagram below):
- Forgetfulness of more than one pill from the blister pack
Consult your doctor.
- Forgetfulness of a pill during days 1-7 (first row)
Take the forgotten pill as soon as you remember, even if it means taking two pills at the same time. Continue taking the following pills at the usual time and use additional precautions, such as condoms, for the next 7 days. If you have had sexual intercourse in the week before forgetting the pill, you should know that there is a risk of pregnancy. In that case, consult your doctor.
- Forgetfulness of a pill during days 8-14 (second row)
Take the forgotten pill as soon as you remember, even if it means taking two pills at the same time. Continue taking the following pills at the usual time. The protection against pregnancy does not decrease, and you do not need to take additional precautions.
- Forgetfulness of a pill between days 15 and 24 (third or fourth row)
You can choose between two options:
- Take the forgotten pill as soon as you remember, even if it means taking two pills at the same time. Continue taking the following pills at the usual time. Instead of continuing with the white placebo pills, discard them and start taking the next blister pack (the day you take the first pill will be different).
You will probably have your period at the end of the second blister pack – during the taking of the white placebo pills – although you may experience spotting or intermenstrual bleeding during the taking of the second blister pack.
- You can also stop taking the active pink pills and go directly to the 4 white placebo pills (including the days you forgot the pills, before taking the placebo pills, note the day you forgot to take your pill).If you want to start a new blister pack on your fixed start day, take the placebo pills for less than 4 days.
If you follow one of these two recommendations, you will remain protected against pregnancy.
- If you have forgotten to take a pill from a blister pack and do not have your period during the placebo days, this may mean that you are pregnant. In this case, you should consult your doctor before continuing with the next blister pack.
The following diagram describes how to proceed if you forget to take a pill (s):
What to do in case of vomiting or severe diarrhea
If you vomit within 3-4 hours after taking an active pink pill or if you have severe diarrhea, there is a risk that the active ingredients of the pill may not be fully absorbed by your body, in which case you may need to use additional protection (such as a condom) to avoid pregnancy. This is similar to what happens when you forget a pill. After vomiting or diarrhea, you should take another pink pill from a reserve blister pack as soon as possible. If possible, take it within 24 hours after the usual time you take your contraceptive. If it is not possible or more than 24 hours have passed, follow the instructions in the section "If you forget to take Etinilestradiol/Drospirenona Exeltis".
Delayed menstrual period: what you should know
Although it is not recommended, it is possible to delay your menstrual period if you do not take the white placebo pills from the 4th row and start directly taking the pills from a new blister pack of etinilestradiol/drospirenona until you finish this new blister pack. You may experience spotting or intermenstrual bleeding during the use of the second blister pack. Finish this second blister pack by taking the 4 white pills from the 4th row. Then, start the next blister pack.
Before deciding to delay your menstrual period, you should ask your doctor.
Changing the first day of your menstrual period: what you should know
If you take the pills according to the instructions, your menstrual period will start during the placebo days. If you need to change this day, you can do so by reducing the placebo days (the days you take the white pills), but never extending – 4 days is the maximum!For example, if you start the placebo days on a Friday and want to change it to Tuesday (3 days earlier), you should start a new blister pack 3 days earlier than usual. You may not have bleeding during these placebo days. Then, you may experience spotting or intermenstrual bleeding.
If you are not sure how to proceed, consult your doctor.
If you interrupt treatment with Etinilestradiol/Drospirenona Exeltis
You can stop taking etinilestradiol/drospirenona whenever you want. If you do not want to become pregnant, consult your doctor about other effective methods of birth control. If you want to become pregnant, it is advisable to stop taking etinilestradiol/drospirenona and wait until your next menstrual period before trying to become pregnant. This way, you can more easily calculate the estimated date of delivery.
If you have any other doubts about the use of this medication, ask your doctor or pharmacist.
4. Possible Adverse Effects
Like all medicines, this medicine can cause adverse effects, although not all people suffer from them.
If you experience any adverse effect, especially if it is severe and persistent or if you have any change in health that you think may be due to ethinylestradiol/drospirenone, consult your doctor.
All women who take combined hormonal contraceptives are at a higher risk of developing blood clots in the veins (venous thromboembolism (VTE)) or blood clots in the arteries (arterial thromboembolism (ATE)). For more detailed information on the different risks of taking combined hormonal contraceptives, see section 2 "What you need to know before taking Ethinylestradiol/Drospirenone Exeltis".
Contact your doctor immediately if you experience any of the following symptoms of angioedema: swelling of the face, tongue, and/or throat, and/or difficulty swallowing or urticaria, with possible difficulty breathing (see also the "Warning and Precautions" section).
If you experience any of the following adverse effects, you may need urgent medical attention. Stop taking ethinylestradiol/drospirenone and consult your doctor or go to the nearest hospital:
Rare(may affect up to 1 in 1,000 people):
- Inflammation of the gallbladder.
- Hypersensitivity (allergic reactions with signs such as swelling of the face, tongue, and/or throat and/or difficulty swallowing, or urticaria along with difficulty breathing).
- Formation of blood clots in a vein or artery, for example:
- In a leg or foot (i.e., deep vein thrombosis (DVT)).
- In a lung (i.e., pulmonary embolism (PE)).
- Heart attack.
- Stroke.
- Mini-stroke or symptoms similar to a transient ischemic attack (TIA).
- Blood clots in the liver, stomach/intestine, kidneys, or eyes.
The likelihood of having a blood clot may be higher if you have other conditions that increase this risk (see section 2 for more information on conditions that increase the risk of blood clots and symptoms of a blood clot).
Conditions that may occur or worsen during pregnancy or with previous use of the pill include:
- Systemic lupus erythematosus (SLE, a disease that affects the immune system).
- Inflammation of the colon or other parts of the intestine (with signs such as bloody diarrhea, pain when passing stools, abdominal pain) (Crohn's disease and ulcerative colitis).
- Epilepsy.
- Uterine fibroids (non-cancerous tumors that grow inside the uterine muscle tissue).
- Blood disorder (porphyria).
- Blisters like skin rash (gestational herpes) during pregnancy.
- Sydenham's chorea (a nerve disease characterized by sudden movements of the body).
- Certain blood disorders that cause kidney damage (hemolytic uremic syndrome, with signs such as decreased urine output, blood in the urine, low red blood cell count, nausea, vomiting, confusion, and diarrhea).
- Yellowing of the skin or whites of the eyes due to bile duct obstruction (icteric cholestasis).
Additionally, breast cancer (see section 2 Ethinylestradiol/Drospirenone Exeltis and cancer) and benign and malignant liver tumors (with signs such as abdominal swelling, weight loss, abnormal liver function, which can be seen in blood tests) and chloasma (brownish-yellow spots on the skin, particularly on the face, known as "pregnancy spots") have been observed, which may be permanent, especially in women who have had chloasma during pregnancy.
Other Adverse Effects
- Frequent(may affect up to 1 in 10 people):
- Mood changes.
- Headache.
- Nausea.
- Breast pain, menstrual problems such as irregular periods, absence of periods.
- Infrequent(may affect up to 1 in 100 people):
- Depression, nervousness, drowsiness.
- Dizziness, tingling.
- Migraine, varicose veins, increased blood pressure.
- Stomach pain, vomiting, indigestion, intestinal gas, stomach inflammation, diarrhea.
- Acne, itching, skin rash.
- Discomfort and pain such as back pain, pain in the limbs, muscle cramps.
- Vaginal yeast infection, pain in the lower abdominal region (pelvic), breast enlargement, benign breast lumps, uterine/vaginal bleeding (which usually subsides during treatment), vaginal discharge, hot flashes, vaginal inflammation (vaginitis), menstrual problems, painful periods, shorter periods, heavy periods, vaginal dryness, abnormal cervical smear, loss of libido.
- Lack of energy, increased sweating, fluid retention (with signs such as swelling of the face and limbs).
- Weight gain.
- Rare(may affect up to 1 in 1,000 people):
- Candidiasis (a fungal infection).
- Anemia, increased platelet count in blood.
- Allergic reaction.
- Hormonal disorder (endocrine).
- Increased appetite, loss of appetite, high potassium levels in blood, low sodium levels in blood.
- Loss of orgasm, insomnia.
- Vertigo, tremors.
- Eye disorders such as eyelid inflammation, dry eyes.
- Abnormal heart rate, unusually fast.
- Inflammation of a vein, nosebleeds, fainting.
- Abdominal enlargement, intestinal disorder, feeling of bloating, hiatal hernia, oral thrush, constipation, dry mouth.
- Pain in the bile ducts or gallbladder.
- Eczema, hair loss, acne-like skin inflammation, dry skin, skin inflammation with swelling, excessive hair growth, skin disorders, stretch marks on the skin, skin inflammation, skin inflammation due to photosensitivity, skin nodules.
- Difficult or painful intercourse, vaginal inflammation (vulvovaginitis), post-coital bleeding, intermenstrual bleeding, breast cysts, increased breast cell count (hyperplasia), abnormal growth of the mucous membrane of the cervix, contraction or atrophy of the uterine mucosa, ovarian cysts, uterine enlargement.
- General malaise.
- Weight loss.
- Frequency not known(cannot be estimated from available data):
- Erythema multiforme (skin rash with target-like redness or ulcers).
Reporting of Adverse Effects
If you experience any adverse effect, consult your doctor, pharmacist, or nurse, even if it is a possible adverse effect that is not listed in this leaflet. You can also report them directly through the Spanish Pharmacovigilance System for Human Use Medicines: https://www.notificaram.es. By reporting adverse effects, you can contribute to providing more information on the safety of this medicine.
5. Storage of Ethinylestradiol/Drospirenone Exeltis
Keep this medicine out of the sight and reach of children.
Store below 30°C.
Do not use this medicine after the expiration date stated on the packaging, after CAD or EXP. The expiration date is the last day of the month indicated.
Medicines should not be disposed of via wastewater or household waste. Deposit the packaging and medicines you no longer need at the SIGRE collection point in your pharmacy. If in doubt, ask your pharmacist how to dispose of the packaging and medicines you no longer need. This will help protect the environment.
6. Package Contents and Additional Information
Composition of Ethinylestradiol/Drospirenone Exeltis
- The active ingredients are ethinylestradiol and drospirenone.
Each pink film-coated tablet contains 0.02 mg of ethinylestradiol and 3 mg of drospirenone.
The white film-coated tablets do not contain active ingredients.
- The other ingredients are:
Active pink film-coated tablets: lactose monohydrate, pregelatinized corn starch, povidone (E-1201), sodium croscarmellose, polysorbate 80, magnesium stearate (E-572), polyvinyl alcohol (E-1203), titanium dioxide (E-171), macrogol, talc (E-553b), yellow iron oxide (E-172), red iron oxide (E-172), black iron oxide (E-172).
Inactive white film-coated tablets: anhydrous lactose, povidone (E-1201), magnesium stearate (E-572), partially hydrolyzed polyvinyl alcohol (E-1203), titanium dioxide (E-171), macrogol, talc (E-553b).
Appearance of the Product and Package Contents
- Each Ethinylestradiol/Drospirenone Exeltis blister pack contains 24 active pink film-coated tablets in the 1st, 2nd, 3rd, and 4th rows of the blister pack and 4 white placebo film-coated tablets in the 4th row.
- Ethinylestradiol/Drospirenone Exeltis tablets, both pink and white, are film-coated tablets; the core of the tablet is coated.
- Ethinylestradiol/Drospirenone Exeltis is available in boxes of 1, 3, 6, and 13 blister packs, each containing 28 (24 + 4) tablets.
Only some pack sizes may be marketed.
Marketing Authorization Holder and Manufacturer
Marketing Authorization Holder
Exeltis Healthcare S.L.
Avenida de Miralcampo, 7.
Polígono Industrial Miralcampo.
19200 Azuqueca de Henares.
Guadalajara, Spain.
Manufacturer
Laboratorios León Farma, S.A.
C/ La Vallina, s/n, Pol. Ind. Navatejera
–24193 - Villaquilambre, León
Spain
or
McDermott Laboratories Ltd T/A Gerard Laboratories T/A Mylan Dublin
35/36 Baldoyle Industrial Estate, Grange Road
Dublin 13
Ireland
or
Mylan Hungary Kft
2900 Komárom, Mylan utca 1
Hungary
This medicine is authorized in the Member States of the European Economic Area under the following names:
Belgium: Marliesexeltis 0.02 mg/3 mg film-coated tablets
Spain: Ethinylestradiol/Drospirenone Exeltis 0.02 mg/3 mg film-coated tablets (24+4) EFG
Italy: Mycyclamen
Netherlands: Ethinylestradiol/Drospirenon Xiromed 24+4 0.02 mg/3 mg, film-coated tablets
Portugal: Drosdiol
This leaflet was last revised in: December 2022
Detailed information on this medicine is available on the website of the Spanish Agency for Medicines and Health Products (AEMPS) https://www.aemps.gob.es/
- Country of registration
- Active substance
- Prescription requiredYes
- Manufacturer
- This information is for reference only and does not constitute medical advice. Always consult a doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to ETHINYLESTRADIOL/DROSPIRENONE EXELTIS 0.02 mg/3 mg FILM-COATED TABLETS (24+4) GenericDosage form: TABLET, 3 mg/0.03 mgActive substance: drospirenone and ethinylestradiolManufacturer: Laboratorios Cinfa S.A.Prescription requiredDosage form: TABLET, 3 mg/0.03 mgActive substance: drospirenone and ethinylestradiolManufacturer: Laboratorios Cinfa S.A.Prescription requiredDosage form: TABLET, 3 mg/0.02 mgActive substance: drospirenone and ethinylestradiolManufacturer: Laboratorios Cinfa S.A.Prescription required
Online doctors for ETHINYLESTRADIOL/DROSPIRENONE EXELTIS 0.02 mg/3 mg FILM-COATED TABLETS (24+4) Generic
Discuss questions about ETHINYLESTRADIOL/DROSPIRENONE EXELTIS 0.02 mg/3 mg FILM-COATED TABLETS (24+4) Generic, including use, safety considerations and prescription review, subject to medical assessment and local regulations.
Frequently Asked Questions






