METHOFILL 10 mg/0.20 ml Injectable Solution in Pre-filled Syringe


How to use METHOFILL 10 mg/0.20 ml Injectable Solution in Pre-filled Syringe
Introduction
Package Leaflet: Information for the User
Methofill 10 mg/0.20 ml Solution for Injection in Pre-filled Syringe EFG
Methotrexate
Read all of this leaflet carefully before you start using this medicine because it contains important information for you.
- Keep this leaflet, you may need to read it again.
- If you have any further questions, ask your doctor or pharmacist.
- This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours.
- If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet. See section 4.
Contents of the pack
- What Methofill is and what it is used for
- What you need to know before you use Methofill
- How to use Methofill
- Possible side effects
- Storage of Methofill
- Contents of the pack and other information
1. What Methofill is and what it is used for
Methofill contains methotrexate as the active substance.
Methotrexate is a substance with the following properties:
- it interferes with the growth of certain cells in the body that reproduce quickly,
- it reduces the activity of the immune system (the body's defense mechanism),
- it has anti-inflammatory effects.
Methofill is indicated for the treatment of:
- active rheumatoid arthritis in adult patients,
- severe active polyarticular forms of juvenile idiopathic arthritis, when the response to non-steroidal anti-inflammatory drugs (NSAIDs) has not been adequate,
- severe recalcitrant and disabling psoriasis that does not respond adequately to other treatments such as phototherapy, PUVA, and retinoids, and severe psoriatic arthritis in adult patients,
- mild to moderate Crohn's disease in adult patients when adequate treatment with other medications is not possible.
Rheumatoid arthritis (RA) is a chronic disease of the connective tissue, characterized by inflammation of the synovial membranes (joint membranes). These membranes produce a fluid that acts as a lubricant in many joints. Inflammation causes the membrane to thicken and the joint to swell.
Juvenile arthritis affects children and adolescents under the age of 16. Polyarticular forms are indicated if there is involvement of 5 or more joints in the first 6 months of the disease.
Psoriatic arthritis is a type of arthritis with psoriatic lesions on the skin and nails, especially in the joints of the hands and feet.
Psoriasis is a chronic and frequent skin disease, characterized by red patches covered with thick, dry, silvery, and adherent scales.
Methofill modifies and slows down the progression of the disease.
Crohn's disease is a type of inflammatory bowel disease that can affect any part of the gastrointestinal tract, causing symptoms such as abdominal pain, diarrhea, vomiting, or weight loss.
2. What you need to know before you use Methofill
Do not use Methofill
- if you are allergic to methotrexate or any of the other ingredients of this medicine (listed in section 6),
- if you have severe liver or kidney disease or blood diseases,
- if you regularly drink large amounts of alcohol,
- if you have a severe infection, such as tuberculosis, HIV, or other immunodeficiency syndromes,
- if you have ulcers in the mouth, stomach ulcers, or intestinal ulcers,
- if you are pregnant or breastfeeding (see section "Pregnancy, breastfeeding, and fertility"),
- if you are receiving live vaccines at the same time.
Warnings and precautions
Methotrexate can make your skin more sensitive to sunlight. Avoid intense sunlight and do not use sunbeds or UV lamps without medical advice. To protect your skin from intense sunlight, wear suitable clothing or use a sunscreen with a high protection factor.
Consult your doctor or pharmacist before starting treatment with Methofill if:
- you are elderly or generally feel unwell and weak,
- you have impaired liver function,
- you have dehydration problems (loss of fluids).
Special precautions for treatment with Methofill
Methotrexate temporarily affects the production of sperm and eggs, which is reversible in most cases. Methotrexate can cause abortions and severe birth defects. If you are a woman, you must avoid becoming pregnant if you are receiving methotrexate and for at least 6 months after stopping treatment with methotrexate. If you are a man, you must avoid fathering a child if you are receiving methotrexate and for at least 3 months after stopping treatment. See also section "Pregnancy, breastfeeding, and fertility".
Recommended follow-up tests and safety measures:
Even when Methofill is administered at low doses, severe side effects can occur. To detect them in time, it is necessary for your doctor to perform blood tests and check-ups.
Before starting treatment with Methofill:
Before starting treatment, you will have blood tests to check that you have enough blood cells, and tests will be performed to check liver function and to find out if you have hepatitis. Additionally, the concentration of serum albumin (a blood protein) will be checked, as well as the state of hepatitis (liver infection) and kidney function. Your doctor may also decide to perform other liver tests, some of which may involve imaging of your liver, and others may require taking a small tissue sample from your liver to examine it more closely. Your doctor will also check if you have tuberculosis (an infectious disease with small nodules in the affected tissue) and will perform a chest X-ray or a lung function test.
During treatment:
Your doctor will perform the following tests:
- examination of the oral cavity and pharynx to detect changes in the mucous membrane, such as inflammation or ulceration
- blood count with number of blood cells and measurement of serum methotrexate levels
- blood tests to monitor liver function
- imaging tests to monitor liver condition
- small tissue sample taken from the liver to examine it more closely
- blood tests to monitor kidney function
- review of the respiratory system and, if necessary, lung function test
It is very important that you attend these scheduled tests.
If the results of any of these tests are remarkable, your doctor will adjust your treatment accordingly.
Acute pulmonary hemorrhage has been reported with methotrexate in patients with underlying rheumatological disease. If you cough up blood or spit up blood, you should contact your doctor immediately.
Methotrexate can affect the immune system and the results of vaccination. It can also affect the results of immunological tests. It can exacerbate chronic inactive infections (e.g., herpes zoster ["shingles"], tuberculosis, hepatitis B or C). During treatment with Methofill, you should not receive live vaccines.
During treatment with methotrexate, radiation-induced dermatitis and sunburn (memory reactions) may recur. Psoriatic lesions may worsen during UV radiation and concurrent administration of methotrexate.
An increase in the size of lymph nodes (lymphoma) may occur, and in such cases, treatment should be discontinued.
Diarrhea can be a toxic effect of Methofill that requires discontinuation of treatment. If you have diarrhea, talk to your doctor.
Certain brain disorders (encephalopathy/leukoencephalopathy) have been reported in cancer patients treated with methotrexate. It cannot be ruled out that these adverse effects may occur when methotrexate is used to treat other diseases.
If you, your partner, or your caregiver notice the appearance or worsening of neurological symptoms, such as general muscle weakness, vision changes, changes in thinking, memory, and orientation that cause confusion and changes in personality, contact your doctor immediately because these may be symptoms of a rare and severe brain infection called progressive multifocal leukoencephalopathy (PML).
Elderly patients
Elderly patients treated with methotrexate should be closely monitored by a doctor to detect any possible side effects as soon as possible.
The deterioration of liver and kidney function related to age, as well as the low body reserves of folic acid in the elderly, require a relatively low dose of methotrexate.
Other medicines and Methofill
Tell your doctor or pharmacist if you are using, have recently used, or might use any other medicines. Also, keep this in mind for medicines that you might take in the future.
The effect of treatment may be affected if Methofill is administered at the same time as certain medicines:
- Antibioticssuch as: tetracyclines, chloramphenicol, non-absorbable broad-spectrum antibiotics, penicillins, glycopeptides, sulfonamides, ciprofloxacin, and cefalotin (medicines to prevent or combat certain infections).
- Amoxicillin(penicillins may reduce the excretion of methotrexate, causing a potential increase in side effects).
- Non-steroidal anti-inflammatory drugsor salicylates(medicines for pain or inflammation, such as acetylsalicylic acid, diclofenac, or ibuprofen, or pyrazolones)
- Probenecid(medicine for gout).
- Weak organic acids such as loop diuretics
- Medicines that may cause adverse effects on the bone marrow, such as trimethoprim-sulfamethoxazole (an antibiotic) and pyrimethamine
- Other medicines used to treat rheumatoid arthritissuch as leflunomide, sulfasalazine, and azathioprine.
- Mercaptopurine (a cytostatic).
- Retinoids (medicines for psoriasisand other dermatological diseases)
- Theophylline (medicine for bronchial asthmaand other pulmonary diseases)
- Certain medicines for stomach problemssuch as omeprazole and pantoprazole.
- Hypoglycemics (medicines used to lower blood sugar levels).
- Metamizol (synonyms novaminsulfon and dipyrone)(medicine for intense pain and/or fever);
Vitamins containing folic acidmay alter the effect of your treatment and should only be taken when advised by your doctor.
Vaccination with live vaccines should be avoided.
Using Methofill with food, drinks, and alcohol
During treatment with Methofill, you should avoid consuming alcohol and large amounts of coffee, caffeinated soft drinks, and black tea.
Pregnancy, breastfeeding, and fertility
Pregnancy
Do not use Methofill during pregnancy or if you are trying to become pregnant. Methotrexate can cause birth defects, harm the fetus, or cause abortions. It is associated with malformations of the skull, face, heart, and blood vessels, brain, and limbs. Therefore, it is very important that methotrexate is not administered to pregnant patients or those planning to become pregnant. In women of childbearing age, any possibility of pregnancy should be excluded with appropriate measures, such as a pregnancy test before starting treatment. You should avoid becoming pregnant while taking methotrexate and for at least 6 months after stopping treatment, using reliable contraceptive methods during this time (see also section "Warnings and precautions").
If you become pregnant during treatment or suspect you may be pregnant, consult your doctor as soon as possible. You should be offered information about the risk of harmful effects on the child during treatment.
If you wish to become pregnant, consult your doctor, who may refer you to a specialist for information before the planned start of treatment.
Breastfeeding
Stop breastfeeding before and during treatment with Methofill.
Male fertility
Available data do not indicate an increased risk of malformations or abortions if the father takes a dose of methotrexate less than 30 mg/week. However, this risk cannot be completely ruled out. Methotrexate can be genotoxic, which means it can cause genetic mutations. Methotrexate can affect sperm production and cause birth defects. Therefore, you should avoid fathering a child or donating sperm while taking methotrexate and for at least 3 months after stopping treatment.
Driving and using machines
Treatment with Methofill can cause adverse reactions that affect the central nervous system, such as fatigue and dizziness. Therefore, the ability to drive or use machines may be affected in certain cases. If you feel tired or drowsy, you should not drive or use machines.
Methofill contains sodium
This medicine contains less than 23 mg of sodium (1 mmol) per dose; this is essentially "sodium-free".
3. How to use Methofill
Follow the instructions for administration of this medicine exactly as prescribed by your doctor. If you are unsure, consult your doctor or pharmacist again.
Your doctor will determine the dose, which will be adjusted individually. Normally, the treatment takes between 4 and 8 weeks to take effect.
The injection of Methofill will be administered or supervised by your doctor or healthcare professional only once a week. Together with your doctor, you will choose a day of the week that is suitable for you to receive the injection. Methofill can be injected subcutaneously (under the skin).
At the beginning of treatment, Methofill may be injected by medical personnel. However, your doctor may decide that you can learn to inject Methofill yourself. You will receive the necessary training for this. Under no circumstances should you attempt to inject yourself unless you have been taught to do so.
Important warning about the dose of Methofill (methotrexate): Use Methofill only once a week for the treatment of rheumatoid arthritis, juvenile idiopathic arthritis, psoriasis, and Crohn's disease. Overuse of Methofill (methotrexate) can be fatal. Read section 3 of this leaflet carefully. If you have any doubts, consult your doctor or pharmacist before taking this medicine. |
Use in children and adolescents
Because the data on intravenous administration of the medicine in children and adolescents are very limited, it should only be administered by subcutaneous injection (under the skin).
The doctor decides what the appropriate dose is for children and adolescents with polyarticular forms of juvenile idiopathic arthritis.
Methofill is not recommended for use in children under 3 years of age because experience is limited in this age group.
Duration and method of administration
Methofill is injected once a week.
The doctor in charge will decide the duration of treatment. The treatment of rheumatoid arthritis, juvenile idiopathic arthritis, psoriasis vulgaris, psoriatic arthritis, and Crohn's disease with Methofill is long-term treatment.
At the start of treatment, Methofill may be injected by healthcare personnel. In certain cases, your doctor may decide to teach you how to inject Methofill yourself under the skin. If so, you will receive the necessary training.
Under no circumstances should you attempt to inject Methofill yourself before receiving such training.
See the instructions for use at the end of the leaflet.
The handling and disposal of the product will be carried out in accordance with the guidelines for other cytotoxic preparations, in accordance with local regulations. Pregnant healthcare personnel should not handle or administer Methofill.
Methotrexate should not come into contact with the skin or mucous membranes. If it does, the affected area should be rinsed immediately with plenty of water.
If you use more Methofill than you should
If you use more Methofill than you should, consult your doctor immediately.
If you forget to use Methofill
Do not take a double dose to make up for forgotten doses.
If you stop treatment with Methofill
If you stop treatment with Methofill, consult your doctor immediately.
If you think the effect of Methofill is too strong or too weak, consult your doctor or pharmacist.
In case of overdose or accidental ingestion, consult your doctor or pharmacist immediately or call the Toxicology Information Service, phone: 91 562 04 20.
4. Possible Adverse Effects
Like all medicines, this medicine can cause adverse effects, although not all people suffer from them.
The frequency and severity of adverse effects will depend on the dose and frequency of administration. It is essential that your doctor performs periodic checks, as severe adverse effects can occur even with the lowest doses. Your doctor will perform tests to control abnormalitiesthat occur in the blood (such as low levels of white blood cells, low platelets, and lymphoma) and changes in the kidneys and liver.
Tell your doctor immediatelyif you experience any of the following symptoms, as they may indicate a severe or potentially life-threatening adverse effect that may require urgent specific treatment:
- Dry cough, difficulty breathing, and fever;may be signs of lung inflammation [frequent]
- Blood when coughing or spitting;may be signs of pulmonary hemorrhage [unknown frequency]
- Symptoms of liver damage, such as yellowing of the skin or eyes; methotrexate can cause chronic liver damage (cirrhosis), scarring of liver tissue (hepatic fibrosis), fatty degeneration of the liver [all infrequent], acute liver inflammation (hepatitis) [rare], and liver failure [very rare]
- Allergic symptoms, such as skin rash including itching and redness of the skin, swelling of the hands, feet, ankles, face, lips, mouth, and throat (which can cause difficulty swallowing or breathing) and feeling of fainting;these may be signs of severe allergic reactions or anaphylactic shock [rare]
- Symptoms of kidney damage, such as swelling of the hands, ankles, or feet or changes in the frequency of urination or decreased (oliguria) or absence (anuria) of urine;these may be signs of renal failure [rare]
- Symptoms of infection, such as fever, chills, muscle pain, sore throat;methotrexate can make you more susceptible to infections. Severe infections, such as a type of pneumonia (Pneumocystis jirovecii pneumonia) or blood infection (sepsis), can occur [rare]
- Symptoms such as weakness on one side of the body (stroke) or pain, swelling, redness, and unusual heat in one leg (deep vein thrombosis);this can happen when a blood clot breaks loose and causes a blockage of a blood vessel [rare]
- Fever and severe deterioration of your general condition, or sudden fever accompanied by sore throat or mouth problems, or urinary problems; methotrexate can cause a sudden drop in the number of certain white blood cells (agranulocytosis) and severe bone marrow suppression [very rare].
- Unexpected bleeding, e.g., bleeding gums, blood in the urine, vomiting blood, or bruising;these may be signs of a severe decrease in the number of platelets caused by severe episodes of bone marrow depression [very rare]
- Symptoms such as severe headache, often in combination with fever, stiff neck, nausea, vomiting, disorientation, and sensitivity to lightmay indicate inflammation of the membranes of the brain (aseptic meningitis) [very rare]
- Certain brain disorders (encephalopathy/leukoencephalopathy) have been reported in cancer patients treated with methotrexate; these adverse effects cannot be ruled out when methotrexate treatment is used to treat other diseases; signs of this type of brain disorder may be altered mental state, movement disorders (ataxia), visual disorders, or memory disorders[unknown frequency]
Severe skin rash or blistering of the skin (this can also affect the mouth, eyes, and genitals); these may be signs of a condition called Stevens-Johnson syndrome or toxic epidermal necrolysis [very rare]
The following are other adverse effects that may occur:
Very common:may affect more than 1 in 10 people
- Inflammation of the mouth lining, indigestion, nausea, loss of appetite, abdominal pain.
- Abnormal results in liver function tests (ASAT, ALAT, bilirubin, alkaline phosphatase).
Common:may affect up to 1 in 10 people
- Mouth ulcers, diarrhea.
- Rash, redness of the skin, itching.
- Headache, fatigue, drowsiness.
- Decreased blood cell formation with a decrease in the number of white blood cells, red blood cells, or platelets
Uncommon:may affect up to 1 in 100 people
- Sore throat inflammation.
- Inflammation of the intestine, vomiting, pancreas inflammation, black or tarry stools, gastrointestinal ulcers, and bleeding.
- Reactions similar to sunburn due to increased skin sensitivity to sunlight, hair loss, increased number of rheumatoid nodules, skin ulcers, shingles, blood vessel inflammation, herpes-like rash, hives.
- Onset of diabetes mellitus.
- Dizziness, confusion, depression.
- Decreased serum albumin.
- Decreased number of all blood cells and platelets.
- Inflammation and ulceration of the urinary bladder or vagina, decreased kidney function, urinary disorders.
- Joint pain, muscle pain, reduced bone mass.
Rare:may affect up to 1 in 1,000 people
- Gingival tissue inflammation.
- Increased skin pigmentation, acne, bruising on the skin due to bleeding from blood vessels (ecchymosis, petechiae), allergic inflammation of blood vessels.
- Decreased number of antibodies in the blood.
- Infection (including reactivation of inactive chronic infections), red eyes (conjunctivitis).
- Mood changes (mood alterations).
- Visual disturbances.
- Inflammation of the sac around the heart, fluid accumulation in the sac around the heart, obstruction of heart filling due to fluid in the sac surrounding the heart.
- Low blood pressure.
- Scarring of lung tissue (pulmonary fibrosis), difficulty breathing, and bronchial asthma, fluid accumulation in the sac surrounding the lung.
- Stress fracture.
- Electrolyte disturbances.
- Fever, altered wound healing.
Very rare:may affect up to 1 in 10,000 people
- Toxic and acute dilation of the intestine (toxic megacolon).
- Increased nail pigmentation, inflammation of the cuticles (acute paronychia), deep infection of hair follicles (furunculosis), visible enlargement of small blood vessels.
- Local injury at the injection site (formation of sterile abscesses, changes in fatty tissue) after injection into a muscle or under the skin.
- Pain, loss of strength, or feeling of numbness or tingling/sensitivity to stimuli less than normal, altered taste (metallic taste), seizures, paralysis, meningism.
- Visual disturbance, non-inflammatory eye disorder (retinopathy).
- Loss of sexual desire, impotence, breast enlargement in men, altered sperm formation (oligospermia), menstrual disorders, vaginal discharge.
- Increased size of lymph nodes (lymphoma).
- Lymphoproliferative disorders (excessive increase in white blood cells).
Unknown frequency:cannot be estimated from available data
- Increased number of certain white blood cells.
- Nosebleeds.
- Protein in the urine.
- Feeling of weakness.
- Jawbone injury (secondary to excessive increase in white blood cells).
- Tissue destruction at the injection site.
- Redness and peeling of the skin.
- Swelling
When methotrexate is administered intramuscularly, local adverse reactions (burning sensation) or injuries (sterile abscess formation, fatty tissue destruction) at the injection site can occur frequently. Subcutaneous administration of methotrexate is well tolerated locally. Only mild local skin reactions were observed, which decreased during treatment.
Reporting of adverse effects
If you experience any type of adverse effect, consult your doctor or pharmacist, even if it is a possible adverse effect not listed in this leaflet. You can also report them directly through www.notificaRAM.es. By reporting adverse effects, you can contribute to providing more information on the safety of this medicine.
5. Storage of Methofill
Keep this medicine out of sight and reach of children.
Store below 30 °C.
Keep the pre-filled syringes in the outer packaging to protect them from light.
Do not use this medicine after the expiration date stated on the packaging. The expiration date is the last day of the month indicated.
Medicines should not be disposed of via wastewater or household waste. Place the packaging and medicines you no longer need in the SIGRE collection point at the pharmacy. Ask your pharmacist how to dispose of the packaging and medicines you no longer need. This will help protect the environment.
6. Package contents and additional information
Composition of Methofill
- The active ingredient is methotrexate. 1 ml of solution contains methotrexate disodium equivalent to 50 mg of methotrexate.
- The other ingredients are sodium chloride, sodium hydroxide, water for injectable preparations.
Appearance of the product and package contents
The pre-filled syringes of Methofill contain a clear yellow-brown solution. Pre-filled syringes with a fixed safety protector for the needle. The packaging contains the pre-filled syringe with a blister pack and an alcohol-impregnated swab.
The following package sizes are marketed:
Pre-filled syringes containing 0.15 ml, 0.20 ml, 0.25 ml, 0.30 ml, 0.35 ml, 0.40 ml, 0.45 ml, 0.50 ml, 0.55 ml, and 0.60 ml of injectable solution, available in packages of 1 or 4 pre-filled syringes, with subcutaneous injection needles attached and covered with rigid needle protectors and graduated. Additionally, the pre-filled syringes come with a safety protector for the needle.
Not all package sizes may be marketed.
Marketing authorization holder and manufacturer
Marketing authorization holder:
Accord Healthcare S.L.U.
World Trade Center
Moll de Barcelona, s/n
Edifici Est 6ª planta,
08039 Barcelona,
Spain
Manufacturer:
Accord Healthcare B.V.
Winthontlaan 200,
Utrecht, 3526KV
Netherlands
or
Laboratori Fundació DAU
C/ C, 12-14 Pol. Ind. Zona Franca,
Barcelona, Spain
Local representative:
Laboratorios Rubió, S.A.
Industria 29
Polígono Industria Comte de Sert
08755 Castellbisbal
(Barcelona)
Spain
Date of last revision of this leaflet: August 2024
Detailed and updated information on this medicine is available on the website of the Spanish Agency for Medicines and Health Products (AEMPS) http://www.aemps.es
Instructions for use
Read the instructions carefully before starting to administer the injection, and always use the application technique advised by your doctor, nurse, or pharmacist.
If you have any problems or questions, contact your doctor, nurse, or pharmacist.
Preparation
Select a clean, flat, and well-lit work surface.
Wash your hands carefully. Before using it, inspect the methotrexate syringe for visible defects (or cracks).
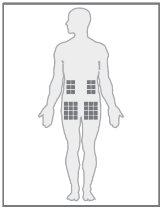
Injection site
| The best places for injection are:
|
|
Injecting the solution
- Open the box containing the pre-filled methotrexate syringe and read the leaflet carefully. Remove the pre-filled syringe from the packaging at room temperature.
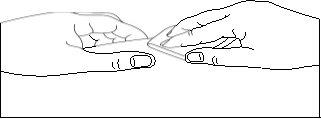
| Select an injection site and disinfect it with the alcohol-impregnated swab. Wait 60 seconds for the disinfectant to dry. |
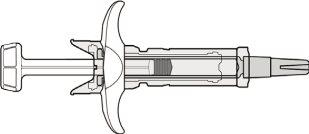
| Check the integrity of the system Do not use the device:
In general, the device cannot be used if it does not match the figure on the left. If so, discard the device in a biological hazard container (sharps) |
|
|
|
|
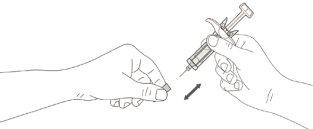
| -Place your thumb over the plunger rod; -Press the plunger rod and push firmlyat the end of the injection to ensure that the syringe is completely empty. Hold the skin securely until the injection is complete. |
| The safety system will be activated once the plunger rod is fully contracted: -Keep the syringe still and slowly lift your thumb off the plunger rod; -The plunger rod will move up with your thumb, and the spring will retract the needle from the site into the needle safety protector. |
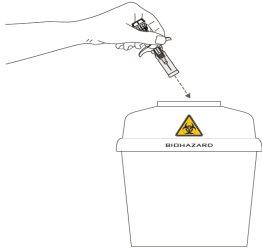
| Once the syringe has been used, immediately discard the device in the biological hazard container (sharps). Do not throw away the used needle safety protector in household waste. |
Methotrexate should not come into contact with skin or mucous membranes. In case of contamination, the affected area should be rinsed immediately with plenty of water.
If you or someone around you is injured with the needle, consult your doctor immediately and do not use this pre-filled syringe.
Elimination and other handling
Handling and disposal of the medicine and pre-filled syringe will be carried out in accordance with local regulations. Pregnant healthcare personnel should not handle or administer methotrexate.

How much does METHOFILL 10 mg/0.20 ml Injectable Solution in Pre-filled Syringe cost in Spain ( 2025)?
The average price of METHOFILL 10 mg/0.20 ml Injectable Solution in Pre-filled Syringe in November, 2025 is around 13.49 EUR. Prices may vary depending on the region, pharmacy, and whether a prescription is required. Always check with a local pharmacy or online source for the most accurate information.
- Country of registration
- Average pharmacy price13.49 EUR
- Active substance
- Prescription requiredYes
- Manufacturer
- This information is for reference only and does not constitute medical advice. Always consult a licensed doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to METHOFILL 10 mg/0.20 ml Injectable Solution in Pre-filled SyringeDosage form: INJECTABLE, 10 mg/ 1 mlActive substance: methotrexateManufacturer: Ebewe Pharma Ges.M.B.H. Nfg.KgPrescription requiredDosage form: INJECTABLE, 15 mgActive substance: methotrexateManufacturer: Ebewe Pharma Ges.M.B.H. Nfg.KgPrescription requiredDosage form: INJECTABLE, 20 mgActive substance: methotrexateManufacturer: Ebewe Pharma Ges.M.B.H. Nfg.KgPrescription required
Alternatives to METHOFILL 10 mg/0.20 ml Injectable Solution in Pre-filled Syringe in other countries
The best alternatives with the same active ingredient and therapeutic effect.
Alternative to METHOFILL 10 mg/0.20 ml Injectable Solution in Pre-filled Syringe in Poland
Alternative to METHOFILL 10 mg/0.20 ml Injectable Solution in Pre-filled Syringe in Ukraine
Online doctors for METHOFILL 10 mg/0.20 ml Injectable Solution in Pre-filled Syringe
Discuss dosage, side effects, interactions, contraindications, and prescription renewal for METHOFILL 10 mg/0.20 ml Injectable Solution in Pre-filled Syringe – subject to medical assessment and local rules.