LUCENTIS 10 mg/ml Injectable Solution in Pre-filled Syringe


How to use LUCENTIS 10 mg/ml Injectable Solution in Pre-filled Syringe
Translated with AI
This page provides general information and does not replace a doctor’s consultation. Always consult a doctor before taking any medication. Seek urgent medical care if symptoms are severe.
Show originalContents of the leaflet
Introduction
Package Leaflet:information for the patient
Lucentis 10mg/ml solution for injection in a pre-filled syringe
ranibizumab
Read all of this leaflet carefully before you are given this medicine because it contains important information for you.
- Keep this leaflet, you may need to read it again.
- If you have any further questions, ask your doctor.
- If you experience any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet. See section 4.
Contents of the pack
- What is Lucentis and what is it used for
- What you need to know before you are given Lucentis
- How Lucentis is given
- Possible side effects
- Storing Lucentis
- Contents of the pack and other information
1. What is Lucentis and what is it used for
What is Lucentis
Lucentis is a solution that is injected into the eye. Lucentis belongs to a group of medicines called anti-angiogenic agents. It contains the active substance called ranibizumab.
What Lucentis is used for
Lucentis is used in adults to treat several eye diseases that cause vision problems.
These diseases are the result of damage to the retina (the light-sensitive layer at the back of the eye) caused by:
- The growth of abnormal blood vessels that leak fluid. This is seen in diseases such as age-related macular degeneration (AMD) and proliferative diabetic retinopathy (PDR, a disease caused by diabetes). It may also be associated with choroidal neovascularization (CNV) due to pathological myopia (PM), angioid streaks, central serous chorioretinopathy, or inflammatory CNV.
- Macular edema (swelling of the center of the retina). The cause of this swelling may be diabetes (a disease known as diabetic macular edema, DME) or a blockage of the retinal veins in the retina (a disease known as retinal vein occlusion, RVO).
How Lucentis works
Lucentis recognizes and binds specifically to a protein called vascular endothelial growth factor A (VEGF-A) in the eyes. In excess, VEGF-A causes the growth of abnormal blood vessels and swelling in the eye that can lead to vision problems in diseases such as AMD, DME, PDR, RVO, PM, and CNV. By binding to VEGF-A, Lucentis can prevent it from working and prevent such abnormal growth and swelling.
In these diseases, Lucentis can help stabilize and, in many cases, improve your vision.
2. What you need to know before you are given Lucentis
You should not be given Lucentis
- If you are allergic to ranibizumab or any of the other ingredients of this medicine (listed in section 6).
- If you have an infection in or around the eye.
- If you have pain or redness (severe intraocular inflammation) in the eye.
Warnings and precautions
Talk to your doctor before you are given Lucentis
- Lucentis is given by injection into the eye. Occasionally, after treatment with Lucentis, an infection in the inner eye, pain, or redness (inflammation), detachment, or tear of a layer in the back of the eye (retinal detachment and retinal pigment epithelial tear), or clouding of the lens (cataract) may occur. It is essential to identify and treat such an infection or retinal detachment as soon as possible. Tell your doctor immediately if you notice signs such as eye pain or increased discomfort in the eye, if redness in the eye worsens, blurred vision, or decreased vision, an increase in the number of small spots in your vision, or increased sensitivity to light.
- In some patients, after the injection, the pressure in the eye may increase for a short period. You may not be aware of this, so your doctor may monitor your eye pressure after each injection.
- Tell your doctor if you have had eye diseases or have received any eye treatment before, or if you have had a stroke or have had transient stroke-like symptoms (weakness or paralysis of a limb or face, difficulty speaking or understanding). This information will be taken into account to assess whether Lucentis is the right treatment for you.
For more detailed information on the side effects that may occur during treatment with Lucentis, see section 4 ("Possible side effects").
Children and adolescents (under 18 years)
Lucentis is not recommended for use in children and adolescents, as it has not been established in these age groups.
Other medicines and Lucentis
Tell your doctor if you are using, have recently used, or might use any other medicines.
Pregnancy and breastfeeding
- Women who may become pregnant should use an effective method of birth control during treatment and for at least three months after the last injection of Lucentis.
- There is no experience with the use of Lucentis in pregnant women. Lucentis should not be used during pregnancy unless the potential benefit outweighs the potential risk to the fetus. If you are pregnant, think you may be pregnant, or plan to become pregnant, consult your doctor before treatment with Lucentis.
- Small amounts of Lucentis may pass into breast milk, so it is not recommended to use Lucentis during breastfeeding. Consult your doctor or pharmacist before treatment with Lucentis.
Driving and using machines
After treatment with Lucentis, you may experience temporary blurred vision. If this happens, do not drive or use machines until this symptom disappears.
3. How Lucentis is given
Lucentis is given by an ophthalmologist as a single injection into the eye under local anesthesia. The usual dose of an injection is 0.05 ml (which contains 0.5 mg of the active substance). The pre-filled syringe contains more than the recommended dose of 0.5 mg. The extra volume should be expelled before injection. If the entire volume of the pre-filled syringe is injected, it may lead to an overdose.
The interval between two doses given in the same eye should be at least four weeks. All injections will be given by an ophthalmologist.
To prevent infection, before the injection, your doctor will carefully clean your eye. Your doctor will also give you a local anesthetic to reduce or prevent any pain you may feel with the injection.
Treatment is started with an injection of Lucentis every month. Your doctor will monitor the disease in your eye and, depending on how you respond to treatment, will decide whether you need further treatment and when you need to be treated.
At the end of the leaflet, in the section "How to prepare and administer Lucentis", detailed instructions for use are given.
Elderly patients (65 years and over)
Lucentis can be used in people 65 years of age or older, and no dose adjustment is necessary.
Before stopping treatment with Lucentis
If you are considering stopping treatment with Lucentis, go to your next appointment and discuss it with your doctor beforehand. Your doctor will advise and decide how long you should be treated with Lucentis.
If you have any further questions on the use of this medicine, ask your doctor.
4. Possible side effects
Like all medicines, this medicine can cause side effects, although not everybody gets them.
The side effects associated with the use of Lucentis are either due to the medicine itself or the injection procedure, and most affect the eye.
The following are the most serious side effects:
Common serious side effects(may affect up to 1 in 10 patients): Detachment or tear of a layer in the inner eye (retinal detachment and retinal pigment epithelial tear), resulting in flashes of light with floating particles progressing to transient vision loss or clouding of the lens (cataract).
Uncommon serious side effects(may affect up to 1 in 100 patients): Blindness, infection of the eyeball (endophthalmitis) with inflammation of the inner eye.
The symptoms you may experience are eye pain or increased discomfort in the eye, if redness in the eye worsens, blurred vision, or decreased vision, an increase in the number of small spots in your vision, or increased sensitivity to light. Tell your doctor immediately if you experience any of these side effects.
The following are the most commonly reported side effects:
Very common side effects(may affect more than 1 in 10 patients)
Eye side effects include: Eye inflammation, bleeding in the back of the eye (retinal hemorrhage), visual disturbances, eye pain, small particles or spots in the vision (floaters), blood in the eye, eye irritation, feeling of having something in the eye, increased tear production, inflammation or infection of the eyelid margin, dry eye, redness or itching of the eye, and increased pressure in the eye.
Non-eye side effects include: Sore throat, nasal congestion, runny nose, headache, and joint pain.
The following are other side effects that may occur after treatment with Lucentis:
Common side effects
Eye side effects include: Decreased sharpness of vision, swelling of a section of the eye (uvea, cornea), inflammation of the cornea (front part of the eye), small marks on the surface of the eye, blurred vision, bleeding at the injection site, bleeding in the eye, eye discharge with itching, redness, and swelling (conjunctivitis), sensitivity to light, eye discomfort, swelling of the eyelid, eyelid pain.
Non-eye side effects include: Urinary tract infection, low red blood cell count (with symptoms such as fatigue, difficulty breathing, dizziness, paleness), anxiety, cough, nausea, allergic reactions such as rash, hives, itching, and redness of the skin.
Uncommon side effects
Eye side effects include: Inflammation and bleeding in the front part of the eye, accumulation of pus in the eye, changes in the central part of the eye surface, pain or irritation at the injection site, abnormal sensation in the eye, eyelid irritation.
Reporting of side effects
If you experience any side effects, talk to your doctor, even if they are not listed in this leaflet. You can also report side effects directly via the national reporting system listed in Appendix V. By reporting side effects, you can help provide more information on the safety of this medicine.
5. Storing Lucentis
- Keep this medicine out of the sight and reach of children.
- Do not use this medicine after the expiry date which is stated on the carton after CAD and on the label of the pre-filled syringe after EXP. The expiry date is the last day of the month shown.
- Store in a refrigerator (2°C - 8°C). Do not freeze.
- Before use, the sealed tray can be stored at room temperature (25°C) for a maximum of 24 hours.
- Store the pre-filled syringe in its original sealed tray in the carton to protect it from light.
- Do not use any packaging that is damaged.
6. Container Contents and Additional Information
Lucentis Composition
- The active substance is ranibizumab. Each ml contains 10 mg of ranibizumab. A pre-filled syringe contains 0.165 ml, equivalent to 1.65 mg of ranibizumab. This provides a usable amount that delivers a single dose of 0.05 ml, which contains 0.5 mg of ranibizumab.
- The other ingredients are α,α-trehalose dihydrate; histidine hydrochloride monohydrate; histidine; polysorbate 20; water for injections.
Product Appearance and Container Contents
Lucentis is an injectable solution contained in a pre-filled syringe. The pre-filled syringe contains 0.165 ml of a sterile, clear, colorless to pale yellowish solution. The pre-filled syringe contains more than the recommended dose of 0.5 mg. The extractable volume will not be administered in its entirety. The excess volume must be expelled before injection. If the entire volume of the pre-filled syringe is injected, it may result in an overdose.
The packaging size is a single pre-filled syringe, packaged in a sealed container tray. The pre-filled syringe is for single use.
Marketing Authorization Holder
Novartis Europharm Limited
Vista Building
Elm Park, Merrion Road
Dublin 4
Ireland
Manufacturer
Novartis Pharma GmbH
Roonstrasse 25
90429 Nuremberg
Germany
Novartis Manufacturing NV
Rijksweg 14
2870 Puurs-Sint-Amands
Belgium
Novartis Pharma GmbH
Sophie-Germain-Strasse 10
90443 Nürnberg
Germany
For further information about this medicinal product, please contact the local representative of the marketing authorization holder:
België/Belgique/Belgien Novartis Pharma N.V. Tél/Tel: +32 2 246 16 11 | Lietuva SIA Novartis Baltics Lietuvos filialas Tel: +370 5 269 16 50 |
Novartis Bulgaria EOOD Тел.: +359 2 489 98 28 | Luxembourg/Luxemburg Novartis Pharma N.V. Tél/Tel: +32 2 246 16 11 |
Ceská republika Novartis s.r.o. Tel: +420 225 775 111 | Magyarország Novartis Hungária Kft. Tel.: +36 1 457 65 00 |
Danmark Novartis Healthcare A/S Tlf: +45 39 16 84 00 | Malta Novartis Pharma Services Inc. Tel: +356 2122 2872 |
Deutschland Novartis Pharma GmbH Tel: +49 911 273 0 | Nederland Novartis Pharma B.V. Tel: +31 88 04 52 111 |
Eesti SIA Novartis Baltics Eesti filiaal Tel: +372 66 30 810 | Norge Novartis Norge AS Tlf: +47 23 05 20 00 |
Ελλάδα Novartis (Hellas) A.E.B.E. Τηλ: +30 210 281 17 12 | Österreich Novartis Pharma GmbH Tel: +43 1 86 6570 |
España Novartis Farmacéutica, S.A. Tel: +34 93 306 42 00 | Polska Novartis Poland Sp. z o.o. Tel.: +48 22 375 4888 |
France Novartis Pharma S.A.S. Tél: +33 1 55 47 66 00 | Portugal Novartis Farma - Produtos Farmacêuticos, S.A. Tel: +351 21 000 8600 |
Hrvatska Novartis Hrvatska d.o.o. Tel. +385 1 6274 220 | România Novartis Pharma Services Romania SRL Tel: +40 21 31299 01 |
Ireland Novartis Ireland Limited Tel: +353 1 260 12 55 | Slovenija Novartis Pharma Services Inc. Tel: +386 1 300 75 50 |
Ísland Vistor hf. Sími: +354 535 7000 | Slovenská republika Novartis Slovakia s.r.o. Tel: +421 2 5542 5439 |
Italia Novartis Farma S.p.A. Tel: +39 02 96 54 1 | Suomi/Finland Novartis Finland Oy Puh/Tel: +358 (0)10 6133 200 |
Κύπρος Novartis Pharma Services Inc. Τηλ: +357 22 690 690 | Sverige Novartis Sverige AB Tel: +46 8 732 32 00 |
Latvija SIA Novartis Baltics Tel: +371 67 887 070 |
Date of Last Revision of this Leaflet:
Other Sources of Information
Detailed information on this medicinal product is available on the European Medicines Agency website: http://www.ema.europa.eu
This information is intended only for healthcare professionals:
See also section 3 “How to Administer Lucentis”.
How to Prepare and Administer Lucentis
Single-use pre-filled syringe. For intravitreal use only.
Lucentis should be administered by an ophthalmologist experienced in administering intravitreal injections.
In exudative age-related macular degeneration (AMD), choroidal neovascularization (CNV), pathologic myopia (PM), and macular edema secondary to retinal vein occlusion (RVO), the recommended dose of Lucentis is 0.5 mg administered via a single intravitreal injection. This corresponds to an injection volume of 0.05 ml. The interval between two doses injected into the same eye should be at least four weeks.
Treatment is initiated with one injection per month until maximum visual acuity is achieved and/or there are no signs of disease activity, i.e., no change in visual acuity or other signs and symptoms of the disease under continued treatment. In patients with exudative AMD, PM, and RVO, three or more consecutive monthly injections may be necessary initially.
From that point on, monitoring and treatment intervals should be determined based on medical judgment and the activity of the disease, as assessed by visual acuity and/or anatomical parameters.
Treatment with Lucentis should be discontinued if, in the physician's judgment, the patient is not benefiting from continued treatment, as evidenced by visual and anatomical parameters.
Monitoring to determine the activity of the disease may include clinical examination, functional testing, or imaging techniques (e.g., optical coherence tomography or fluorescein angiography).
If patients are being treated according to a treat-and-extend regimen, once maximum visual acuity is achieved and/or there are no signs of disease activity, treatment intervals may be gradually extended until signs of disease activity or visual impairment recur. For exudative AMD, the treatment interval should not be extended by more than two weeks at a time, and for macular edema, it may be extended up to one month at a time. For RVO, treatment intervals may also be gradually extended; however, available data are insufficient to determine the duration of these intervals. If disease activity recurs, the treatment interval should be shortened accordingly.
Treatment of visual impairment due to CNV should be determined on an individual basis, taking into account the activity of the disease. Some patients may require only one injection during the first 12 months; others may require more frequent treatment, including monthly injections. In the case of CNV secondary to pathologic myopia, many patients may require only one or two injections during the first year.
Lucentis and Laser Photocoagulation in Macular Edema and Macular Edema Secondary to Retinal Vein Occlusion
There is some experience with Lucentis administered concomitantly with laser photocoagulation. When administered on the same day, Lucentis should be administered at least 30 minutes after laser photocoagulation. Lucentis may be administered in patients who have previously received laser photocoagulation.
Lucentis and Photodynamic Therapy with Verteporfin in CNV Secondary to Pathologic Myopia
There is no experience with the concomitant administration of Lucentis and verteporfin.
Before administering Lucentis, the absence of particles and discoloration should be checked visually.
The injection procedure should be carried out under aseptic conditions, including surgical hand washing, use of sterile gloves, a sterile field, a sterile eyelid speculum (or equivalent), and the availability of a sterile paracentesis (if necessary). Before performing the intravitreal injection procedure, the patient's medical history should be thoroughly evaluated for hypersensitivity reactions. Before injection, adequate anesthesia and a broad-spectrum topical microbicidal agent should be administered to disinfect the skin of the periocular area, eyelid, and ocular surface, according to local practice.
The pre-filled syringe is for single use. The pre-filled syringe is sterile. Do not use the product if the packaging is damaged. The sterility of the pre-filled syringe can only be guaranteed if the tray is kept sealed. Do not use the pre-filled syringe if the solution has changed color, is cloudy, or contains particles.
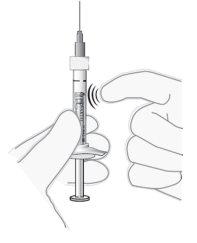
The pre-filled syringe contains more than the recommended dose of 0.5 mg. The extractable volume of the pre-filled syringe (0.1 ml) will not be administered in its entirety. The excess volume must be expelled before injection. If the entire volume of the pre-filled syringe is injected, it may result in an overdose. To expel air bubbles and excess medication, slowly press the plunger until the lower edge of the rubber stopper is aligned with the black dosing line on the syringe (equivalent to 0.05 ml, i.e., 0.5 mg of ranibizumab).
For intravitreal injection, a sterile 30G x ½″ injection needle should be used.
For preparation of Lucentis for intravitreal administration, follow the instructions for use:
Introduction | Read all instructions carefully before using the pre-filled syringe. The pre-filled syringe is for single use. The pre-filled syringe is sterile. Do not use the product if the packaging is damaged. Opening the sealed tray and the following steps should be performed under aseptic conditions. Note: The dose to be administered should be adjusted to 0.05 ml. | |
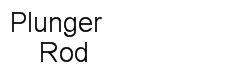
Pre-filled Syringe Description |
| |
Prepare |
| |
Check the Syringe |
| |
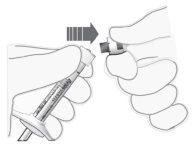
Remove the Syringe Closure Cap |
|
Figure 2
Figure 3 |
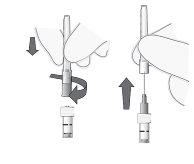
Attach the Needle |
Note: Never wipe the needle. |
Figure 4 Figure 5 |
Expel Air Bubbles |
|
Figure 6 |
Adjust the Dose |
Note: The plunger is not attached to the rubber stopper – this is to prevent air from entering the syringe. |
Figure 7 |
Inject | The injection procedure should be carried out under aseptic conditions.
|
- Country of registration
- Active substance
- Prescription requiredYes
- Manufacturer
- This information is for reference only and does not constitute medical advice. Always consult a doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to LUCENTIS 10 mg/ml Injectable Solution in Pre-filled SyringeDosage form: INJECTABLE, 10 mg/mLActive substance: ranibizumabManufacturer: Samsung Bioepis Nl B.V.Prescription requiredDosage form: INJECTABLE, 10 mg/mLActive substance: ranibizumabManufacturer: Novartis Europharm LimitedPrescription requiredDosage form: INJECTABLE, 10 mg/mlActive substance: ranibizumabManufacturer: Midas Pharma GmbhPrescription required
Online doctors for LUCENTIS 10 mg/ml Injectable Solution in Pre-filled Syringe
Discuss questions about LUCENTIS 10 mg/ml Injectable Solution in Pre-filled Syringe, including use, safety considerations and prescription review, subject to medical assessment and local regulations.
Frequently Asked Questions