
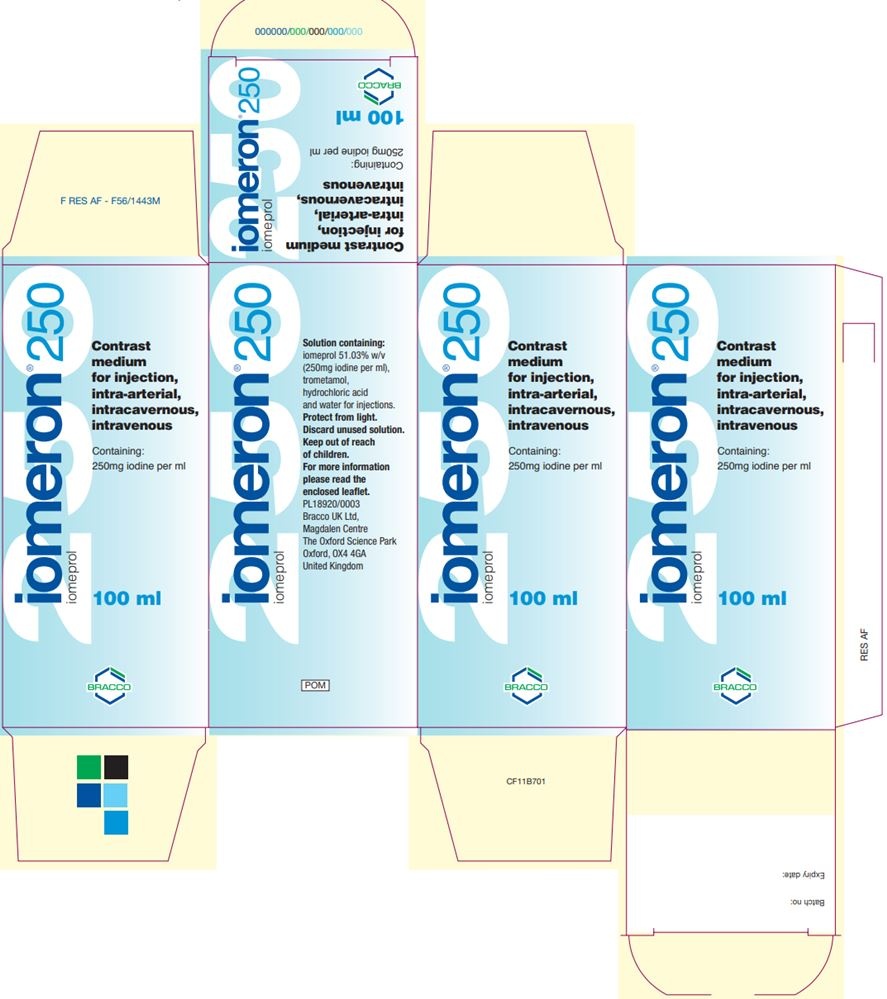
IOMERON 250 MG IODO/ML INJECTABLE SOLUTION

How to use IOMERON 250 MG IODO/ML INJECTABLE SOLUTION
Translated with AI
This page provides general information and does not replace a doctor’s consultation. Always consult a doctor before taking any medication. Seek urgent medical care if symptoms are severe.
Show originalContents of the leaflet
- Introduction
- What Iomeron 250 mg Iodo/ml injectable solution is and what it is used for
- What you need to know before you use Iomeron 250 mg Iodo/ml injectable solution
- How to use Iomeron 250 mg Iodo/ml injectable solution
- Possible side effects
- Storage of Iomeron 250 mg Iodo/ml injectable solution
- Contents of the container and additional information
Introduction
PACKAGE LEAFLET: INFORMATION FOR THE USER
Iomeron250 mg Iodo/ml injectable solution
Iomeprol
Read all of this leaflet carefully before you start using this medicine because it contains important information for you.
- Keep this leaflet, you may need to read it again.
- If you have any further questions, ask your doctor or pharmacist.
- This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours.
- If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet. See section 4.
Contents of the pack and other information
- What Iomeron 250 mg Iodo/ml injectable solution is and what it is used for
- What you need to know before you use Iomeron 250 mg Iodo/ml injectable solution
- How to use Iomeron 250 mg Iodo/ml injectable solution
- Possible side effects
- Storage of Iomeron 250 mg Iodo/ml injectable solution
- Contents of the pack and other information
1. What Iomeron 250 mg Iodo/ml injectable solution is and what it is used for
This medicinal product is for diagnostic use only.
Iomeron belongs to a group of medicines called low osmolar, water-soluble, nephrotropic X-ray contrast media.
Iomeron is used to improve the visualization of different body areas by means of certain radiological techniques. In adults, it is used for intravenous urography, computed tomography (CT) of the head and body, peripheral phlebography, digital subtraction phlebography, digital subtraction angiography, and myelography. In children from 0 to 18 years for intravenous urography, computed tomography (CT) of the head and body, digital subtraction phlebography, and peripheral angiography.
2. What you need to know before you use Iomeron 250 mg Iodo/ml injectable solution
Do not use Iomeron 250 mg Iodo/ml injectable solution
- If you are allergic to iomeprol or any of the other ingredients of this medicinal product (listed in section 6).
- If you have Waldenström's paraproteinemia.
- If you have severe hepatic or renal disorders.
- If you have multiple myeloma.
Investigations of female genitals are contraindicated in case of suspected or confirmed pregnancy and in case of acute inflammation.
Immediate repetition of Iomeron administration if a technical failure occurs is contraindicated in myelography.
Warnings and precautions
- Before starting the examination, you should be adequately hydrated and should avoid eating food for two hours before the examination.
- In states of anxiety and pain, as they may intensify adverse reactions related to the contrast medium. In these cases, a sedative may be administered.
- If you are elderly.
- If you have asthma.
- If you have ever developed a severe skin rash or skin peeling, blisters, and/or sores in the mouth after receiving iodinated contrast media.
- If you have hay fever, urticaria, or food allergies, as patients with a history of allergy are more likely to suffer adverse reactions to iodinated contrast media.
- If you have hyperthyroidism and/or nodular goiter, as the use of non-ionic contrast media may trigger thyroid crises.
- If you have renal insufficiency.
- If you have diabetes mellitus; these patients may develop lactic acidosis if they are being treated with biguanides (e.g., metformin). As a precaution, in patients with moderate renal insufficiency, biguanides should be discontinued at the time of or 48 hours before the examination with a contrast medium and reinstated only after it has been checked that renal function has recovered.
- If you have pheochromocytoma (a type of tumor), as hypertensive crises may occur after using the contrast medium intravascularly. Premedication with alpha-adrenergic blockers is recommended.
- If you have sickle cell anemia (a type of anemia), as contrast media may worsen your disease.
- If you have myasthenia gravis (a disease that causes muscle weakness), as your disease may worsen.
- In case of severe cardiovascular disease, especially if you suffer from heart failure, coronary arteriopathy (disease of the heart's blood vessels), pulmonary hypertension, and coronary valvulopathy.
- When you have central nervous system disorders, as convulsive crises may occur.
- In case of alcoholism and drug addiction.
Fluoroscopy is recommended to minimize extravasation during injection.
You may experience a short-term brain disorder, called encephalopathy, during or shortly after the imaging procedure. Inform your doctor immediately if you notice any symptoms related to this condition, described in section 4.
Thyroid disorders have been observed after Iomeron administration in both children and adults. Infants may also be exposed through the mother during pregnancy. Your doctor may need to perform thyroid function tests before and/or after Iomeron administration.
Severe skin reactions, including Stevens-Johnson syndrome (SJS), toxic epidermal necrolysis (TEN), acute generalized exanthematous pustulosis (AGEP), and drug reaction with eosinophilia and systemic symptoms (DRESS) have been reported in association with the use of Iomeron. Go to your doctor immediately if you observe any of the symptoms related to these severe skin reactions described in section 4.
Consult your doctor before starting to use Iomeron 250 mg Iodo/ml injectable solution.
Children
Children under one year of age, especially neonates, are particularly susceptible to electrolyte imbalances and hemodynamic alterations.
Other medicines and Iomeron 250 mg Iodo/ml injectable solution
Tell your doctor if you are using, have recently used, or might use any other medicines.
Do not interrupt treatment with anticonvulsant drugs and ensure their administration in optimal doses.
In patients treated with immunomodulatory drugs, such as Interleukin-2, allergic reactions to contrast media are more frequent and may manifest as late reactions.
This medicinal product must not be mixed with other medicines.
Interference with laboratory tests:
Iodinated contrast media may interfere with thyroid function studies, as the thyroid's ability to capture radioisotopes will be reduced for periods of two weeks or more.
High concentrations of contrast media in plasma and urine may alter the results of laboratory tests for bilirubin, proteins, and inorganic substances (e.g., iron, copper, calcium, phosphate).
Use of Iomeron 250 mg Iodo/ml injectable solution with food and drinks
If there are no specific instructions from your doctor, you can follow a normal diet on the day of the examination. Confirm adequate fluid intake. However, you should avoid eating food for two hours before the examination.
Pregnancy and breastfeeding
If you are pregnant or breastfeeding, think you may be pregnant, or plan to become pregnant, consult your doctor before using this medicinal product.
Pregnancy
You should inform your doctor if you are pregnant or think you may be pregnant.
As with other non-ionic contrast media, there are no controlled studies in pregnant women that confirm the safety of the product in humans. Since, whenever possible, exposure to radiation should be avoided during pregnancy, the risk/benefit ratio of any X-ray examination, with or without contrast media, should be carefully evaluated.
If you are pregnant and have received Iomeron during pregnancy, it is recommended to analyze the thyroid function of your newborn.
Breastfeeding
Contrast media are barely excreted in breast milk, and the possibility of the infant suffering any harm is remote.
Driving and using machines
No effects on the ability to drive and use machines have been reported.
3. How to use Iomeron 250 mg Iodo/ml injectable solution
This medicinal product will always be administered by qualified and properly trained personnel, in hospitals or clinics that have the necessary personnel and equipment.
The dose that will be administered to you will vary depending on the type of examination, age, body weight, cardiac output, and general condition you present, as well as the technique used.
If you use more Iomeron 250 mg Iodo/ml injectable solution than you should
Overdose can cause severe adverse reactions, mainly through effects on the cardiovascular and pulmonary systems.
Treatment of an overdose is aimed at maintaining all vital functions and providing rapid symptomatic therapy. Iomeron can be eliminated from the body through dialysis.
In case of overdose or accidental ingestion, consult your doctor or pharmacist or call the Toxicology Information Service, telephone 91 562 04 20, indicating the medicinal product and the amount ingested.
If you have any doubts about the use of this product, consult your doctor or pharmacist.
4. Possible side effects
Like all medicines, this medicinal product can cause side effects, although not everybody gets them.
Generally, side effects are mild to moderate and are of a transient nature. However, severe and potentially life-threatening reactions have been reported, sometimes with a fatal outcome. In most cases, reactions occur within minutes of administration, although they may sometimes appear later.
Inform your doctor immediately if you suffer from any of the following symptoms: sudden wheezing, difficulty breathing, swelling of the eyelids, face, or lips, skin rash or itching that affects the whole body.
The following side effects have been reported:
Intravascular administration
Frequent(may affect up to 1 in 10 people):
- feeling of heat
Uncommon(may affect up to 1 in 100 people):
- headache
- dizziness
- increase in blood pressure
- difficulty breathing
- nausea, vomiting
- flushing, urticaria, itching
- chest pain, heat, and pain at the injection site
Rare(may affect up to 1 in 1,000 people)
- fainting
- slow or fast heart rate
- decrease in blood pressure
- skin rash
- back pain
- asthenia, stiffness, fever
- increase in creatinine in blood
Frequency not known(cannot be estimated from the available data):
- Contact a doctor as soon as possible if you experience a severe skin reaction, such as:
- blisters, skin peeling, ulcers in the mouth, throat, nose, genitals, and eyes. These severe skin reactions may be preceded by fever and flu-like symptoms (Stevens-Johnson syndrome, toxic epidermal necrolysis).
- a red and scaly rash with bumps under the skin and blisters, accompanied by fever. The symptoms usually appear at the start of treatment (acute generalized exanthematous pustulosis).
- a widespread rash, high body temperature, and swollen lymph nodes (DRESS syndrome or drug hypersensitivity syndrome)
- anxiety, hyperkinetic syndrome (increased motor activity), confusion
- allergic reactions
- hyperthyroidism
- loss of appetite (anorexia)
- alteration of taste, difficulty speaking, disease affecting brain function, cerebral edema (fluid in the brain), transient problems in blood supply to the brain with few or no sequelae (transient ischemic attacks), memory loss, somnolence, altered sensitivity (tingling, itching) apoplexy, loss of consciousness, tremors, coma, convulsions, alteration of the sense of smell
- brain disorder (encephalopathy) with symptoms that include headache, vision difficulties, loss of vision, confusion, convulsions, loss of coordination, loss of movement in a part of the body, speech problems, and loss of consciousness
- temporary blindness, vision impairment, conjunctivitis, increased tearing, photopsia (seeing lights)
- myocardial infarction, cardiac arrest, chest oppression, heart rhythm disorders, angina pectoris, heart failure, formation of clots in the coronary arteries (after catheter insertion), irregular heartbeat, conduction disorders, rapid and weak pulse
- flushing, shock (severe drop in blood pressure), pallor, fatigue, cool and moist skin, reduced consciousness) caused by sudden and severe dilation of blood vessels, blue discoloration of the skin and mucous membranes, clots, vasospasm, and consequent ischemia.
- circulatory failure (circulatory collapse)
- coronary artery obstruction (after catheter insertion)
- respiratory arrest, cough, acute respiratory distress syndrome (ARDS), wheezing, asthma attacks, fluid accumulation in the throat, fluid in the lungs, inflammation of the nasal mucosa characterized by a stuffy nose, sneezing, and discharge (rhinitis), hoarseness (dysphonia), insufficient oxygen supply to tissues (hypoxia), sore throat and larynx, sudden constriction of the airways (bronchospasm)
- intestinal incontinence, diarrhea, abdominal pain, excessive salivation, difficulty swallowing, inflammation of the pancreas along with severe pain in the upper abdomen that radiates to the back with nausea and vomiting (pancreatitis), enlargement of the salivary glands, intestinal obstruction
- severe hypersensitivity reactions, characterized by symptoms such as increased sweat production, dizziness, itching, pulsating headache, throat oppression, inflammation of the mouth and throat mucosa, which makes breathing difficult
- eczema, skin rash, increased sweat production, sudden accumulation of fluid in the skin and mucous membranes (e.g., throat or tongue), possibly with difficulty breathing and/or itching and skin rash (angioedema), appearance of circular blisters on the skin (whose center is usually paler) (erythema multiforme)
- joint pain, muscle stiffness
- acute renal failure, urinary incontinence, urine abnormalities, decreased urine production
- general feeling of illness (malaise), chills, localized feeling of cold, thirst, reaction at the injection site, hematoma at the injection site
- blood disorders (decrease in platelet count) accompanied by bruising and propensity to bleed (thrombocytopenia)
- hemolytic anemia (abnormal decrease in red blood cells that can cause fatigue, rapid heart rate, and difficulty breathing)
Transient hypothyroidism may occur in children under 3 years of age.
In some cases, alterations are detected during medical examinations (blood values, cardiac and hepatic function tests).
Intrathecal administration
Very common(more than 1 in 10 people):
- headache
Common(more than 1 in 100 people and less than 1 in 10 people):
- dizziness
- increase in blood pressure
- nausea, vomiting
- back pain, pain in the limbs
- reaction at the injection site
Uncommon(more than 1 in 1,000 people and less than 1 in 100 people):
- loss of consciousness
- altered sensitivity
- somnolence
- decrease in blood pressure
- flushing
- muscle stiffness
- neck pain
- feeling of heat
- chest pain
- fever
Frequency not known(cannot be estimated from the available data):
- allergic reactions
- epilepsy
- skin rash
- general feeling of illness
- brain disorder (encephalopathy) with symptoms that include headache, vision difficulties, loss of vision, confusion, convulsions, loss of coordination, loss of movement in a part of the body, speech problems, and loss of consciousness
Consult your doctor if you experience severe symptoms or allergic reactions (hypersensitivity), or if the symptoms persist for long periods of time.
The safety profile of iomeprol is similar in adults and children for all routes of administration.
Reporting of side effects
If you experience any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet. You can also report side effects directly through the Spanish Medicines Monitoring System for Human Use http://www.notificaRam.es. By reporting side effects, you can help provide more information on the safety of this medicinal product.
5. Storage of Iomeron 250 mg Iodo/ml injectable solution
Keep this medicinal product out of the sight and reach of children.
Store the vial in the outer packaging to protect it from light.
Although iomeprol's sensitivity to X-rays is low, it is advisable to store the product out of the reach of ionizing radiation.
Do not use this medicinal product after the expiry date that appears on the packaging after EXP. The expiry date is the last day of the month indicated.
Medicines should not be disposed of via wastewater or household waste. Ask your pharmacist how to dispose of medicines no longer required. This will help protect the environment.
6. Contents of the container and additional information
Composition of Iomeron 250 mg Iodo/ml injectable solution
- The active ingredient is iomeprol. 1 ml of injectable solution contains 510.3 mg of iomeprol, equivalent to 250 mg of iodine.
- The other components are trometamol, hydrochloric acid to adjust the pH, and water for injectable preparations c.s.p.
Appearance of the product and container contents
Iomeron is packaged in glass vials closed with halobutyl stoppers and an aluminum cap.
Single-dose vials of 50 ml, 100 ml, and 200 ml.
Only some package sizes may be marketed.
Marketing authorization holder and manufacturer
Marketing authorization holder
Bracco Imaging s.p.a.
Via E. Folli 50
20134 (Milan - Italy)
Manufacturer
Patheon Italia s.p.a.
2nd Trav. SX Via Morolense, 5
03013 Ferentino (Italy)
BIPSO GmbH
Robert-Gerwig-Strasse 4
78224 Singen (Germany)
Bracco Imaging S.p.A.
Bioindustry Park - Via Ribes, 5
10010 Colleretto Giacosa (TO) (Italy)
You can request more information about this medication by contacting the local representative of the marketing authorization holder:
Laboratorios Farmacéuticos ROVI, S.A.
Julián Camarillo, 35
28037 Madrid
Tel: 913756230
Date of the last revision of this prospectus:September 2023
Detailed and updated information on this medication is available on the website of the Spanish Agency for Medicines and Health Products (AEMPS) http://www.aemps.gob.es/
<-------------------------------------------------------------------------------------------------------------->
This information is intended only for healthcare professionals:
Iomeron 250 mg Iodo/ml is an injectable solution for intravenous, intra-arterial, and intrathecal administration.
Whenever possible, intravascular administration of contrast media should be performed with the patient lying down. The patient should be kept under observation for at least 30 minutes after administration.
Indication | Route of administration | Proposed dosages | |
Intravenous urography | Intravenous | Adults:50 - 150 ml Neonates:3 - 4.8 ml Children: < 1 year: 2.5 - 4 ml/kg > 1 year: 1 - 2.5 ml/kg | |
Head computed tomography | Intravenous | Adults:50 - 200 ml Children | |
Body computed tomography | Intravenous | Adults:100 - 200 ml Children | |
Conventional angiography | |||
Peripheral phlebography | Intravenous | Adults:10 - 100 ml, repeat if necessary (10 - 50 ml upper limbs; 50 - 100 ml lower limbs) | |
Digital subtraction angiography | |||
Abdomen | Intra-arterial | Adults | |
Peripheral arteriography | Intra-arterial | Adults:5 - 10 ml for selective injections, up to 250 ml Children | |
Digital subtraction phlebography | Intravenous | Adults:100 - 250 ml Children | |
Myelography | Intrathecal | Adults:10 - 18 ml | |
a According to body weight and age, and is established by the doctor responsible for the test. b Do not exceed 250 ml. The volume of each single injection depends on the vascular area to be examined. c Do not exceed 350 ml. |
Before use, the solution must be visually inspected. Only solutions without visible signs of deterioration or particles will be used.
The disposal of unused medication and all materials that have come into contact with it will be carried out in accordance with local regulations.
Precautions
- Regarding the patient:
Hydration- Any severe alteration of the hydroelectrolytic balance must be corrected. Before the medical examination, ensure adequate hydration, especially in patients with severe functional impairment of the kidneys, multiple myeloma, or other paraproteinemias, sickle cell anemia, diabetes mellitus, polyuria, oliguria, hyperuricemia, as well as in neonates, children, and elderly patients.
Dietary suggestions- If there are no specific instructions from the doctor, a normal diet can be followed. Confirm adequate fluid intake. However, the patient should abstain from eating food in the two hours prior to the examination.
Hypersensitivity- In patients with a predisposition to allergies, with known hypersensitivity to iodinated contrast media, and with a history of asthma, premedication with antihistamines and/or corticosteroids may be considered to prevent possible anaphylactoid reactions.
Severe cutaneous adverse reactions- Severe cutaneous adverse reactions (SCARs), including Stevens-Johnson syndrome (SJS), toxic epidermal necrolysis (TEN), acute generalized exanthematous pustulosis (AGEP), and drug reaction with eosinophilia and systemic symptoms (DRESS), which can be fatal or potentially fatal, have been reported in patients who received iodinated contrast media intravascularly. At the time of administration, patients should be warned of the signs and symptoms, and closely monitored for the appearance of skin reactions. If signs and symptoms suggesting the appearance of these reactions occur, the administration of Iomeron should be immediately suspended. If a patient has developed a severe reaction such as SJS, TEN, AGEP, or DRESS with the use of Iomeron, Iomeron should not be administered to that patient again.
Anxiety- States of excitement, anxiety, and pain can cause side effects or intensify reactions related to the contrast medium. In these cases, a sedative can be administered.
Concomitant treatments- Consider interrupting treatment with drugs that reduce the convulsive threshold up to 24 hours after the intervention, in the case of intrathecal use, and in patients with disorders of the blood-brain barrier (see "Neurological symptoms").
- Regarding the procedure:
Coagulation, catheterization- A property of non-ionic contrast media is the minimal interference with physiological functions. As a consequence, non-ionic contrast media have, in vitro, a lower anticoagulant activity than ionic contrast media. The medical and paramedical personnel performing vascular catheterization should be informed of this and should pay particular attention to the angiographic technique. Non-ionic contrast media should not come into contact with blood in the syringe, and intravascular catheters should be frequently cleaned to minimize the risk of thromboembolism related to the procedure.
Patient observation- Whenever possible, intravascular administration of contrast media should be performed with the patient lying down. The patient should be kept under observation for at least 30 minutes after administration.
Sensitivity test- A sensitivity test is practically useless, as the occurrence of severe or fatal reactions due to contrast media cannot be predicted with such a test.
Risk of inflammation andextravasation- Caution is recommended during the injection of contrast media to avoid extravasation.
Warnings
- Common to all forms of administration
Considering the possible serious side effects, the use of iodinated contrast media should be limited to specific needs for contrastographic examinations.
This need should be considered according to the patient's clinical conditions, especially in relation to cardiovascular, urinary, and hepatobiliary pathologies.
Contrast media for angiocardio graphic examinations should be used in hospitals or clinics with competent personnel and necessary equipment for intensive care in case of emergency. In centers where other diagnostic tests that require the use of iodinated contrast media are performed, it is necessary that the radiology services where these tests are performed have therapeutic measures and resuscitation equipment that experience has confirmed to be suitable (Ambu bag, oxygen, antihistamines, vasoconstrictors, etc.).
Use in:
Pediatric population- Children under one year of age, and especially neonates, are particularly susceptible to electrolyte imbalances and hemodynamic alterations. Attention should be paid to the doses to be used, the procedure technique, and the patient's condition. Hypothyroidism or transient thyroid suppression may be observed after exposure to iodinated contrast media. Special attention should be paid to pediatric patients under 3 years of age, as an episode of low thyroid activity during the first years of life can be harmful to motor, auditory, and cognitive development and may require temporary replacement treatment with T4. The incidence of hypothyroidism in patients under 3 years of age exposed to iodinated contrast media has been reported to be between 1.3% and 15%, depending on the age of the subjects and the dose of the iodinated contrast medium, and is more frequent in neonates and premature infants. Thyroid function should be evaluated in all pediatric patients under 3 years of age after exposure to iodinated contrast media. If hypothyroidism is detected, the need for treatment should be considered, and thyroid function should be monitored until it normalizes.
Elderly- Elderly patients should be considered at special risk for reactions due to excessive dosing of the contrast medium. The frequent association of neurological disorders and vascular pathologies constitutes an aggravating factor.
Patients with particular pathological conditions
- Hypersensitivity to iodinated contrast media- Hypersensitivity or previous reactions to iodinated contrast media also increase the risk of recurrence of a severe reaction, even with non-ionic contrast media.
- Allergic predisposition- It is known that adverse reactions to iodinated contrast media are more common in patients with a history of allergy: hay fever, urticaria, and food allergies.
- Asthmatic patients- Patients taking beta-adrenergic blockers, particularly asthmatic patients, may have a lower threshold for bronchospasm and a lower response to treatment with beta-agonists and adrenaline, which may require the use of higher doses.
- Thyroid function and thyroid function tests- Iodinated contrast media may contain small amounts of free inorganic iodide that could have effects on thyroid function. These effects are more evident in patients with latent or overt hyperthyroidism or goiter. Hyperthyroidism or even thyroid crisis has been reported after the administration of iodinated contrast media.
- Intra-arterial and intravenous administration
Use in patients with special pathological conditions
Renal impairment- In patients with compromised renal function, the administration of contrast media can cause episodes of renal failure. Preventive measures include: identifying high-risk patients; ensuring adequate hydration before administration of the contrast medium, preferably maintaining intravenous infusion before, during the procedure, and until the contrast medium has been eliminated by the kidneys; avoiding, if possible, the administration of nephrotoxic drugs and subjecting the patient to major surgical interventions or procedures such as renal angioplasty until the contrast medium has been completely eliminated; postponing a new examination with contrast medium until renal function returns to pre-examination levels. Patients on dialysis can receive contrast media, such as iomeprol, that are easily dialyzable.
Diabetes mellitus- The presence of renal damage in diabetic patients is one of the factors that predisposes to renal dysfunction as a consequence of the administration of contrast media.
Renal impairment can cause lactic acidosis in diabetic patients with renal damage treated with biguanides (metformin). To prevent this, treatment with biguanides should be suspended in the following cases: before intra-arterial administration of a contrast medium with first-pass renal exposure, in patients with eGFR less than 30 ml/min/1.73 m2 who receive a contrast medium intravenously or a contrast medium intra-arterially with second-pass renal exposure, or in patients with acute kidney injury, and should only be resumed after 48 hours, provided that renal function has not changed significantly.
Pheochromocytoma- These patients can develop severe hypertensive crises (rarely uncontrollable) after using intravascular contrast medium during radiological procedures.
In patients with pheochromocytoma, premedication with alpha-receptor blockers is recommended due to the risk of hypertensive crises.
Myasthenia gravis- The administration of iodinated contrast media can exacerbate the signs and symptoms of myasthenia.
Cardiac disease and pulmonary hypertension- There is a high risk of severe reactions in patients with severe cardiovascular pathology, particularly in those with heart failure and coronary arteriopathy. The intravascular injection of contrast media can cause pulmonary edema in patients with overt or incipient cardiac decompensation, while the administration of contrast medium in cases of pulmonary hypertension and valvulopathy can favor hemodynamic alterations. The appearance of signs of ischemia on the ECG and severe arrhythmias is more common in older patients and those with pre-existing cardiopathy: their frequency and severity seem to be related to the severity of the cardiac pathology.
Neurological symptoms- Particular attention should be paid when administering a contrast medium to patients with acute cerebral infarction, intracranial hemorrhage, and those with alterations of the blood-brain barrier, cerebral edema, or acute demyelination. The presence of intracranial tumors or metastases and a history of epilepsy can increase the probability of seizures. The administration of contrast media can exacerbate neurological symptoms due to degenerative, ischemic, inflammatory, or neoplastic cerebrovascular pathologies. These patients have a higher risk of transient neurological complications. Intravascular injections of contrast media can cause angiospasm and episodes of cerebral ischemia.
Alcoholism- It has been demonstrated, experimentally and clinically, that acute or chronic alcoholism increases the permeability of the blood-brain barrier. It facilitates the passage of iodinated agents to the brain tissue, which can produce CNS disorders. A possible reduction in the epileptic threshold in alcoholics should be considered.
Contrast-induced encephalopathy- Contrast-induced encephalopathy has been reported with the use of iomeprol.
Contrast-induced encephalopathy can manifest with symptoms and signs of neurological dysfunction such as headache, visual disturbances, cortical blindness, confusion, seizures, loss of coordination, hemiparesis, aphasia, unconsciousness, coma, and cerebral edema in the minutes to hours following the administration of iomeprol, and usually disappears within a few days.
The product should be used with caution in patients with diseases that affect the integrity of the blood-brain barrier (BBB), which could cause greater permeability of the contrast medium through the BBB and increase the risk of encephalopathy. If contrast-induced encephalopathy is suspected, the administration of iomeprol should be suspended, and adequate medical monitoring should be initiated.
Drug addiction- Drug-addicted patients require special attention due to the possible reduction of the convulsive threshold.
Fluoroscopy is recommended to minimize extravasation during injection.
Overdose
In case of accidental intravascular overdose of the contrast medium, the patient's hydration and electrolyte balance should be monitored and corrected if necessary. In this situation, renal function should be monitored for at least three days.
In case of accidental intrathecal overdose, the patient should be carefully monitored for at least 24 hours to detect signs and symptoms of CNS disorders. These signs may include: increased hyperreflexia or tonic-clonic spasms, and even generalized seizures, hyperthermia, stupor, and respiratory depression.
- Country of registration
- Availability in pharmacies
Supply issue reported
Data from the Spanish Agency of Medicines (AEMPS) indicates a supply issue affecting this medicine.<br><br>Availability may be limited in some pharmacies.<br><br>For updates or alternatives, consult your pharmacist. - Active substance
- Prescription requiredYes
- Manufacturer
- This information is for reference only and does not constitute medical advice. Always consult a doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to IOMERON 250 MG IODO/ML INJECTABLE SOLUTIONDosage form: INJECTABLE, 30.62 g/100 mlActive substance: iomeprolManufacturer: Bracco Imaging S.P.A.Prescription requiredDosage form: INJECTABLE, 40.82 g/100 mlActive substance: iomeprolManufacturer: Bracco Imaging S.P.A.Prescription requiredDosage form: INJECTABLE, 61.24 g iomeprol/100 mlActive substance: iomeprolManufacturer: Bracco Imaging S.P.A.Prescription required
Online doctors for IOMERON 250 MG IODO/ML INJECTABLE SOLUTION
Discuss questions about IOMERON 250 MG IODO/ML INJECTABLE SOLUTION, including use, safety considerations and prescription review, subject to medical assessment and local regulations.
Frequently Asked Questions















