
DUOFEMME FILM-COATED TABLETS


How to use DUOFEMME FILM-COATED TABLETS
Translated with AI
This page provides general information and does not replace a doctor’s consultation. Always consult a doctor before taking any medication. Seek urgent medical care if symptoms are severe.
Show originalContents of the leaflet
Introduction
Package Leaflet: Information for the User
Duofemme film-coated tablets
estradiol/norethisterone acetate
Read this package leaflet carefully before you start taking this medicine, because it contains important information for you.
Keep this package leaflet, you may need to read it again.
- Keep this package leaflet, you may need to read it again.
- If you have any further questions, ask your doctor or pharmacist.
- This medicine has been prescribed for you, do not pass it on to others, it may harm them, even if their symptoms are the same as yours.
because it may harm them.
- If you experience any side effects, talk to your doctor or pharmacist, even if it is not listed in this package leaflet. See section 4.
Contents of the package leaflet:
- What is Duofemme and what is it used for
- What you need to know before taking Duofemme
- How to take Duofemme
- Possible side effects
- Storing Duofemme
- Contents of the pack and other information
1. What is Duofemme and what is it used for
Duofemme is a combined sequential Hormone Replacement Therapy (HRT) that is taken every day without interruption. Duofemme is used in postmenopausal women who have had their last natural period at least 6 months ago.
Duofemme contains 2 hormones, an estrogen (estradiol) and a progestogen (norethisterone acetate). The estradiol in Duofemme is identical to the estradiol produced by the ovaries in women, and is classified as a natural estrogen. Norethisterone acetate is a synthetic progestogen that acts in a similar way to progesterone, another important female sex hormone.
Duofemme is indicated for:
Relief of symptoms occurring after menopause
During menopause, the amount of estrogens produced by women decreases. This can cause symptoms such as hot flushes.
Duofemme relieves these symptoms after menopause. Duofemme will only be prescribed if your symptoms seriously affect your daily life.
Prevention of osteoporosis
After menopause, some women may develop fragile bones (osteoporosis).
You should discuss all possible options with your doctor.
If you have a high risk of fractures due to osteoporosis and cannot use other medicines for this purpose, you may use Duofemme to prevent osteoporosis after menopause.
Experience in treating women over 65 years of age is limited.
2. What you need to know before taking Duofemme
Medical history and regular check-ups:
The use of HRT carries risks that need to be evaluated before starting treatment or if treatment is to continue.
Experience in treating women with premature menopause (due to ovarian failure or surgery) is limited. If you have premature menopause, the risks of using HRT may be different. Consult your doctor.
Before starting (or restarting) HRT, your doctor will ask you about your medical history and that of your family. Your doctor may decide to perform a physical examination. This may include an examination of your breasts and/or an internal examination, if necessary.
Once you have started taking Duofemme, you should see your doctor for regular medical check-ups (at least once a year). During these check-ups, your doctor will discuss the benefits and risks of continuing treatment with Duofemme.
Regularly attend breast examinations as recommended by your doctor.
Do not take Duofemme
If any of the following conditions apply to you. If you are not sure about any of the following points, consult your doctorbefore taking Duofemme.
Do not take Duofemme:
- If you have or have had breast cancer, or if you suspect you may have it
- If you have or have had cancer of the lining of the uterus (endometrial cancer), or if endometrial cancer is suspected
or if it is suspected that you have cancer that is dependent on estrogens
- If you have unexpected vaginal bleeding
- If you have excessive thickening of the lining of the uterus (endometrial hyperplasia) that is not being treated
If you have or have had blood clots in a vein (venous thromboembolism), in the legs (deep vein thrombosis) or lungs (pulmonary embolism)
- If you have a blood clotting disorder (such as protein C, S or antithrombin deficiency)
If you have or have had a disease caused by blood clots in the arteries, such as a heart attack, stroke or angina.
- If you have or have had liver disease and your liver function tests have not returned to normal
If you are allergic (hypersensitive) to estradiol, norethisterone acetate or any of the other ingredients of Duofemme (see section 6, Contents of the pack and other information)
- If you have a rare blood disorder called porphyria
If any of the above conditions occur for the first time while taking Duofemme, stop taking it and consult your doctor immediately.
Warnings and precautions
Tell your doctor if you have ever had any of the following problems, before you start treatment, as they may come back or get worse during treatment with Duofemme. If so, you may need to go to your doctor more often for check-ups:
- Fibroids in the uterus
- Growth of the lining of the uterus outside the uterus (endometriosis) or excessive growth of the lining of the uterus (endometrial hyperplasia)
High risk of developing blood clots (see "blood clots in a vein (venous thromboembolism)")
- High risk of having an estrogen-related cancer (if you have a mother, sister or grandmother who has had breast cancer)
High blood pressure
- Liver disease, such as a benign liver tumor
- Diabetes
- Gallstones
- Migraine or severe headaches
- A disease that affects the immune system and many organs of the body (systemic lupus erythematosus, SLE)
Epilepsy
- Asthma
- A disease that affects the membrane of the eardrum and the ear (otosclerosis)
- If you have high levels of fat in the blood (triglycerides)
- Fluid retention due to heart or kidney problems
- A condition where your thyroid gland does not produce enough thyroid hormone (hypothyroidism) and you are taking thyroid hormone replacement therapy
A hereditary condition that causes recurrent episodes of severe inflammation (hereditary angioedema) or if you have had episodes of rapid swelling of the hands, face, feet, lips, tongue, throat (obstruction of the airways) or digestive tract (acquired angioedema)
- Lactose intolerance
Stop taking Duofemme and contact your doctor immediately
if you experience any of the following:
- Any of the conditions mentioned in the "Do not take Duofemme" section
- Yellowing of the skin or whites of the eyes (jaundice), which can be a sign of liver disease
Swelling of the face, tongue and/or throat and/or difficulty swallowing or hives, together with difficulty breathing, which are symptoms of angioedema
- A large increase in your blood pressure (symptoms may be headache, fatigue and dizziness)
Severe headache for the first time
- If you become pregnant
- If you notice signs of a blood clot, such as:
- swelling with pain and redness of the legs,
- sudden chest pain
- difficulty breathing
For more information, see "blood clots in a vein (venous thromboembolism)"
Note: Duofemme is not a contraceptive. If it has been less than 12 months since your last menstrual period or you are under 50 years old, you may need to use a contraceptive to prevent pregnancy. Consult your doctor.
HRT and cancer
Excessive thickening of the lining of the uterus (endometrial hyperplasia) and cancer of the lining of the uterus (endometrial cancer)
If you take estrogen-only HRT, you will have an increased risk of excessive thickening of the lining of the uterus (endometrial hyperplasia) and cancer of the lining of the uterus (endometrial cancer).
The progestogen in Duofemme protects you from this additional risk.
Comparison
In women aged 50-65 years with an intact uterus who do not take HRT, the average number of new cases of endometrial cancer could be 5 per 1000 users.
In women aged 50-65 years with an intact uterus who take estrogen-only HRT, between 10 and 60 per 1000 users will be diagnosed with endometrial cancer, depending on the dose and duration of treatment (between 5 and 55 additional cases).
Unexpected bleeding
You will have a monthly bleed (called a withdrawal bleed) while taking Duofemme. But if you have unexpected bleeding or blood loss (spotting) in addition to your monthly bleed, which:
- continues for more than the first 6 months
- starts after 6 months of taking Duofemme
- or continues after stopping treatment with Duofemme
Tell your doctor as soon as possible.
Breast cancer
Existing data show that the use of hormone replacement therapy (HRT) with combined estrogen-progestogen or estrogen-only therapy increases the risk of breast cancer. The additional risk depends on the duration of HRT use. The additional risk becomes apparent after 3 years of use. After stopping HRT, the additional risk will decrease over time, but the risk may persist for 10 years or more if HRT has been used for more than 5 years.
Comparison
In women aged 50-54 years who do not take HRT, 13-17 per 1000 will be diagnosed with breast cancer over a 5-year period.
In women aged 50 years who start estrogen-only HRT for 5 years, there will be between 16 and 17 cases per 1000 users (i.e., between 0 and 3 additional cases). In women aged 50 years who start taking combined estrogen-progestogen HRT for 5 years, there will be between 21 per 1000 users (i.e., between 4 and 8 additional cases).
In women aged 50-59 years who do not take HRT, an average of 27 cases of breast cancer per 1000 women will be diagnosed over a 10-year period.
In women aged 50 years who start estrogen-only HRT for 10 years, there will be 34 cases per 1000 users (i.e., 7 additional cases). In women aged 50 years who start taking combined estrogen-progestogen HRT for 10 years, there will be 48 cases per 1000 users (i.e., 21 additional cases).
Examine your breasts regularly. See your doctor if you notice any changes, such as:
- skin dimpling
- nipple changes
- any lump that you can see or feel
In addition, it is recommended to participate in breast screening programs when they are offered.
In breast screenings, it is important to inform your nurse/healthcare professional that you are taking HRT when you have a mammogram, as this medicine may increase breast density, which can affect the result of the mammogram. When breast density is higher, it may be that the mammogram will not detect all lumps.
Ovarian cancer
Ovarian cancer is less common than breast cancer. The use of HRT with estrogen-only or combined estrogen-progestogen therapy has been associated with a slightly increased risk of ovarian cancer.
The risk of ovarian cancer varies with age. For example, in women aged 50-54 years who do not take HRT, there will be about 2 cases of ovarian cancer per 2000 women over a 5-year period. In women taking HRT for 5 years, there will be about 3 cases per 2000 users (i.e., about 1 additional case).
Effect of HRT on the heart and circulation
Blood clots in a vein (venous thromboembolism)
The risk of blood clots in the veins is about 1.3 to 3 times higher in HRT users than in non-users, especially in the first year of taking it.
Blood clots can be serious, and if one reaches the lungs, it can cause chest pain, difficulty breathing, collapse, or even death.
You are more likely to get a blood clot if you are older and if any of the following apply to you. Tell your doctor if you experience any of the following:
- You are unable to walk for a long time due to surgery, injury or illness (see also section 3, "If you need to have surgery")
If you are seriously overweight (BMI >30 kg/m²)
- If you have a blood clotting disorder that needs long-term treatment with a medicine to prevent blood clots
If you have a close relative who has had a blood clot in the legs, lungs or other organs
- If you have systemic lupus erythematosus (SLE)
- If you have cancer
In case of signs of a blood clot, see "Stop taking Duofemme" and contact your doctor immediately.
Comparison
In women aged 50 years who do not take HRT, 4-7 per 1000 will have a blood clot in the veins over a 5-year period.
In women aged 50 years who take combined estrogen-progestogen HRT, there will be 9-12 cases per 1000 users over a 5-year period (up to 5 additional cases).
Heart disease (heart attack)
There is no evidence that HRT prevents heart attacks. In women over 60 years old who use combined estrogen-progestogen HRT, there is a slightly increased risk of heart disease compared to non-HRT users.
Stroke
The risk of stroke is about 1.5 times higher in HRT users than in non-users. As a result, the number of additional stroke cases due to HRT use will increase with age.
Comparison
In women aged 50 years who do not take HRT, an average of 8 per 1000 will have a stroke over a 5-year period.
In women aged 50 years who take HRT, there will be 11 cases per 1000 users over a 5-year period (up to 3 additional cases).
Other conditions
HRT does not prevent memory loss. There is some evidence of an increased risk of memory loss in women who start HRT after the age of 65. Tell your doctor.
Using other medicines
Some medicines may interfere with the effect of Duofemme.
This could lead to irregular bleeding. This applies to the following medicines:
- Medicines for epilepsy (such as phenobarbital, phenytoin and carbamazepine)
- Medicines for tuberculosis (such as rifampicin and rifabutin)
- Medicines for HIV infection (such as nevirapine, efavirenz, ritonavir and nelfinavir)
- Medicines for hepatitis C infection (such as telaprevir)
- Herbal products that contain St. John's Wort (Hypericum perforatum)
HRT may affect the performance of certain medicines:
- Medicines for epilepsy (lamotrigine), as it may increase the frequency of seizures.
- Medicines for hepatitis C (such as the combination of ombitasvir/paritaprevir/ritonavir with or without dasabuvir, as well as a regimen with glecaprevir/pibrentasvir) may cause increases in liver function blood test results (increase in liver enzyme ALT) in women who use combined hormonal contraceptives (CHC) that contain ethinylestradiol. Duofemme contains estradiol instead of ethinylestradiol. It is not known whether an increase in liver enzyme ALT can occur when using Duofemme with this combination regimen against hepatitis C.
Other medicines may increase the effects of Duofemme:
- Medicines that contain ketoconazole (an antifungal)
Duofemme may affect treatment with the concomitant use of cyclosporin.
Tell your doctor or pharmacistif you are taking or have recently taken any other medicines, including those obtained without a prescription, herbal medicines or other natural products. Your doctor will advise you.
Lab tests
If you need to have a blood test, tell your doctor that you are taking Duofemme, as this medicine may affect the results of some tests.
Taking Duofemme with food and drinks
The tablets can be taken with or without food and drinks.
Pregnancy and breastfeeding
Pregnancy: Duofemme is only for postmenopausal women. If you are pregnant, stop taking Duofemme immediately and contact your doctor.
Breastfeeding: Do not take Duofemme if you are breastfeeding.
Driving and using machines
Duofemme has no known effect on the ability to drive or use machines.
Important information about some of the ingredients of Duofemme
Duofemme contains lactose monohydrate. If your doctor has told you that you have an intolerance to some sugars, consult your doctor before taking this medicine.
3. How to take Duofemme
Always take this medicine exactly as your doctor has told you. Ask your doctor
or pharmacist if you have any doubts.
If you are not taking any other hormone replacement therapy, you can start treatment with
Duofemme on the day you consider convenient. If you are already taking another type of hormone
replacement therapy, your doctor will tell you when to start treatment with Duofemme.
You will take one tablet once a day, approximately at the same time every day.
Each box contains 28 tablets
Days 1-16 Take one red tabletevery day for 16 days
Days 17-28 Take one white tabletevery day for 12 days
Take the tablets with a glass of water.
Once you have finished the box, start a new one, continuing treatment without interruption.
A menstrual-type bleeding (period) usually occurs at the beginning of a new box.
For more information on using the calendar dial, see "INSTRUCTIONS FOR USE" at the end of the prospectus.
Your doctor will prescribe the lowest dose to treat your symptoms for the shortest time
necessary.
Consult your doctor if you do not show improvement after 3 months of treatment. You should only
continue treatment when the benefit outweighs the risk.
If you take more Duofemme than you should
If you have taken more Duofemme than you should, consult your doctor or pharmacist. An
overdose of estrogens can cause breast tenderness, nausea, vomiting, and/or irregular vaginal bleeding
(metrorrhagia). An overdose of progestogens can lead to depression, fatigue, acne, and excessive hair
growth on the face or body (hirsutism).
In case of overdose or accidental ingestion, consult your doctor or pharmacist immediately or
call the Toxicology Information Service, phone 915 620 420, indicating the medicine and the amount
ingested.
If you forget to take Duofemme
If you forget to take the tablet at the usual time, take it within the next 12 hours. If more than 12
hours have passed, take it the next day at the usual time. Do not take a double dose to make up for the
missed dose.
Forgetting to take a tablet may increase the likelihood of intermenstrual bleeding and spotting.
If you stop taking Duofemme
If you want to stop taking Duofemme, first talk to your doctor. Your doctor will explain the effects of
stopping treatment and other possibilities for you.
If you have any other questions about the use of this medicine, ask your doctor or pharmacist.
If you need to have surgery
If you are going to have surgery, inform the surgeon that you are taking Duofemme. You may need to
stop taking Duofemme approximately 4 to 6 weeks before the operation to reduce the risk of a blood
clot (see section 2, "blood clots in a vein (venous thromboembolism)"). Ask your doctor when you can
start taking Duofemme again.
4. Possible side effects
Like all medicines, this medicine can cause side effects, although not everybody gets them.
The following diseases occur more frequently in women using HRT compared to women not using
HRT:
- breast cancer
- abnormal growth or cancer of the uterine lining (endometrial hyperplasia or cancer)
- ovarian cancer
- blood clots in the veins of the legs or lungs (venous thromboembolism)
- heart disease
- stroke
- possible memory loss if HRT is started after the age of 65
For more information about these side effects, see section 2, "What you need to know before taking
Duofemme".
Hypersensitivity/allergic reaction (uncommon side effect that affects between 1 and 10 users per 1000)
Although it is an uncommon side effect, hypersensitivity/allergic reaction can occur: The signs of
hypersensitivity/allergic reaction may include one or more of the following symptoms: hives, itching,
swelling, difficulty breathing, low blood pressure (pallor and cooling of the skin, rapid heartbeat),
dizziness, sweating, which can be signs of anaphylactic reaction. If one of the mentioned symptoms
appears, stop treatment with Duofemme and seek immediate medical help.
Very common side effects (may affect more than 1 in 10 people)
??Headache
??Breast pain
Common side effects (may affect up to 1 in 10 people)
??Increased blood pressure and worsening of hypertension
??Vaginal fungal infection (e.g., candidiasis)
??Dizziness, insomnia, depression
??Dyspepsia (indigestion), abdominal pain, flatulence
??Nausea (dizziness)
??Rash, itching
??Vaginal bleeding (see section 2, subsection "Unexpected bleeding")
??Worsening of uterine fibroids (benign tumor of the uterus)
??Edema (swelling of hands, wrists, and feet)
??Weight gain
Uncommon side effects (may affect up to 1 in 100 people)
??Migraine
??Changes in libido (change in sexual desire)
??Peripheral embolism and thrombosis (blood clots)
??Vomiting (dizziness)
??Gallbladder disease or gallstones
??Hair loss (alopecia)
??Muscle cramps
Rare side effects (may affect up to 1 in 1000 people)
??Allergic reactions
??Nervousness
??Vertigo (dizziness)
??Diarrhea
??Abdominal swelling
??Acne
??Uterine fibroid (benign tumor of the uterus)
Unknown frequency (cannot be estimated from available data)
??Endometrial hyperplasia (excessive growth of uterine cells)
??Increased facial and body hair
??Anxiety
??Visual disturbances
??Seborrhea
??Vaginal itching
Other side effects of combined HRT
The following side effects have been reported with other HRT medications:
- Various skin disorders:
- Skin discoloration, especially on the face or neck, known as chloasma
- Painful red nodules on the skin (erythema nodosum)
- Red, target-shaped rash or blisters (erythema multiforme)
- Purple-colored skin discolorations (vascular purpura)
??Dry eyes
??Changes in the composition of the tear film
Reporting side effects
If you experience any side effects, consult your doctor or pharmacist, even if it is a possible side
effect not listed in this prospectus. You can also report them directly through the Spanish Pharmacovigilance
System for Human Use http://www.notificaram.es.
By reporting side effects, you can help provide more information on the safety of this medicine.
5. Storage of Duofemme
Keep this medicine out of the sight and reach of children.
Do not use this medicine after the expiration date stated on the label and carton after "EXP". The
expiration date refers to the last day of the month.
Do not store above 25°C. Do not refrigerate. Keep the container in the outer packaging to protect it
from light.
Medicines should not be disposed of via wastewater or household waste. Dispose of the container and
any unused medicine in the pharmacy's SIGRE collection point. If in doubt, ask your pharmacist how to
dispose of the container and any unused medicine. This will help protect the environment.
6. Package contents and information
What Duofemme contains
The active ingredients are estradiol and norethisterone acetate.
The red film-coated tablets contain: estradiol 1 mg (as estradiol hemihydrate).
The white film-coated tablets contain: estradiol 1 mg (as estradiol hemihydrate) and norethisterone acetate
1 mg.
The other ingredients are: lactose monohydrate, cornstarch, hydroxypropylcellulose, talc, and magnesium
stearate.
Coating (red tablets): hypromellose, talc, titanium dioxide (E171), propylene glycol, and iron oxide red
(E172).
Coating (white tablets): hypromellose, triacetin, and talc.
Appearance of Duofemme and package contents
The film-coated tablets are round with a diameter of 6 mm. The red tablets are engraved with NOVO 282.
The white tablets are engraved with NOVO 283.
Each box of 28 tablets contains 16 red tablets and 12 white tablets.
Package sizes:
1x28 film-coated tablets
3x28 film-coated tablets
Not all package sizes may be marketed.
Marketing authorization holder and manufacturer
Holder:
Isdin S.A.
Provençals, 33
08019 Barcelona
Spain
Manufacturer:
Novo Nordisk A/S
Novo Allé
DK-2880 Bagsvaerd
Denmark
This medicine is authorized in the Member States of the European Economic Area and in the United Kingdom (Northern Ireland) under the following names:
EEA Member States:Novofem
Except:
France: Novofemme
Spain: Duofemme
Date of last revision of this prospectus: September 2024
Other sources of information
Detailed and updated information on this medicine is available on the website of the Spanish Agency
for Medicines and Health Products (AEMPS): http://www.aemps.gob.es/
INSTRUCTIONS FOR USE
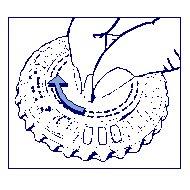
How to use the calendar dial
- Place the day indicator
Turn the inner dial and fix the day of the week in front of the closed opening with a tab.
- How to remove the first tablet
Break the plastic tab and remove the first tablet.
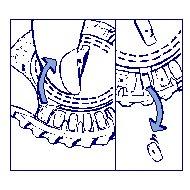
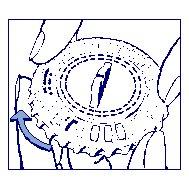
Move the dial every day:The next day, simply turn the transparent dial one space in the direction of the clock hands, as indicated by the arrow. Remove the next tablet. Remember to take only 1 tablet per day.
The transparent dial can only be turned once the corresponding tablet has been removed.
- Country of registration
- Average pharmacy price7.66 EUR
- Active substance
- Prescription requiredYes
- Manufacturer
- This information is for reference only and does not constitute medical advice. Always consult a doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to DUOFEMME FILM-COATED TABLETSDosage form: TABLET, -Active substance: norethisterone and estrogenManufacturer: Isdin S.A.Prescription requiredDosage form: TABLET, 1 mg/10 mgActive substance: dydrogesterone and estrogenManufacturer: Theramex Ireland LimitedPrescription requiredDosage form: TABLET, 2 mg/10mgActive substance: dydrogesterone and estrogenManufacturer: Theramex Ireland LimitedPrescription required
Online doctors for DUOFEMME FILM-COATED TABLETS
Discuss questions about DUOFEMME FILM-COATED TABLETS, including use, safety considerations and prescription review, subject to medical assessment and local regulations.
Frequently Asked Questions






