
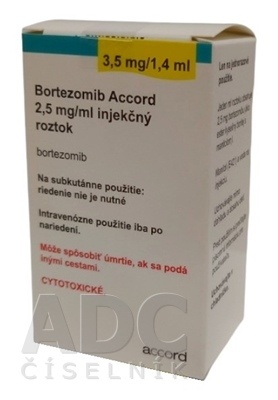
BORTEZOMIB ACCORD 2.5 mg/mL INJECTABLE SOLUTION

How to use BORTEZOMIB ACCORD 2.5 mg/mL INJECTABLE SOLUTION
Translated with AI
This page provides general information and does not replace a doctor’s consultation. Always consult a doctor before taking any medication. Seek urgent medical care if symptoms are severe.
Show originalContents of the leaflet
Introduction
Package Leaflet: Information for the User
Bortezomib Accord 2.5 mg solution for injection EFG
bortezomib
Read all of this leaflet carefully before you start using this medicine because it contains important information for you
- Keep this leaflet, you may need to read it again.
- If you have any further questions, ask your doctor or pharmacist.
- If you experience any side effects, talk to your doctor or pharmacist, even if they are not listed in this leaflet. See section 4.
Contents of the pack
- What is Bortezomib Accord and what is it used for
- What you need to know before you use Bortezomib Accord
- How to use Bortezomib Accord
- Possible side effects
- Storage of Bortezomib Accord
- Contents of the pack and other information
1. What is Bortezomib Accord and what is it used for
Bortezomib Accord contains the active substance bortezomib, a "proteasome inhibitor". Proteasomes play an important role in controlling cell function and growth. Bortezomib can destroy cancer cells by interfering with their function.
Bortezomib Accord is used to treat multiple myeloma (a type of bone marrow cancer) in patients over 18 years of age:
- alone or with the medicines doxorubicin liposomal pegylated or dexamethasone, for patients whose disease is worsening (in progression) after receiving at least one previous treatment and for those patients whose stem cell transplant did not work or is not suitable.
- in combination with the medicines melphalan and prednisone, for patients whose disease has not been previously treated and who are not suitable to receive high-dose chemotherapy prior to a stem cell transplant.
- in combination with the medicines dexamethasone or dexamethasone plus thalidomide, in patients whose disease has not been previously treated and who are receiving high-dose chemotherapy prior to a stem cell transplant (induction treatment).
Bortezomib Accord is used to treat mantle cell lymphoma (a type of cancer that affects the lymph nodes) in patients over 18 years of age in combination with the medicines rituximab, cyclophosphamide, doxorubicin, and prednisone, in patients whose disease has not been previously treated and for those patients who are not considered suitable for a stem cell transplant.
2. What you need to know before you use Bortezomib Accord
Do not use Bortezomib Accord
- if you are allergic to bortezomib, boron, or any of the other ingredients of this medicine (listed in section 6).
- if you have certain severe lung or heart problems.
Warnings and precautions
Tell your doctor if you have:
- low red or white blood cell count.
- bleeding problems and/or low platelet count in the blood.
- diarrhea, constipation, nausea, or vomiting.
- a history of fainting, dizziness, or lightheadedness.
- kidney problems.
- moderate to severe liver problems.
- numbness, tingling, or pain in the hands or feet (neuropathy) in the past.
- heart problems or high blood pressure.
- difficulty breathing or coughing.
- seizures.
- shingles (localized, including around the eyes, or widespread).
- symptoms of tumor lysis syndrome, such as muscle cramps, muscle weakness, confusion, vision loss, or difficulty breathing.
- memory loss, thought disturbances, difficulty walking, or vision loss. These may be signs of a serious brain infection, and your doctor may advise further tests and monitoring.
You will need to have regular blood tests before and during treatment with Bortezomib Accord to check your blood cell count regularly.
You must tell your doctor if you have mantle cell lymphoma and are given rituximab with Bortezomib Accord:
Before starting treatment with Bortezomib Accord, you should read the package leaflets of all the medicines you need to take with Bortezomib Accord for information related to those medicines.
When using thalidomide, special attention should be paid to pregnancy testing and prevention measures (see Pregnancy and Breastfeeding in this section).
Children and adolescents
Bortezomib Accord should not be used in children and adolescents because it is not known how it will affect them.
Other medicines and Bortezomib Accord
Tell your doctor or pharmacist if you are taking, have recently taken, or might take any other medicines.
In particular, tell your doctor if you are using medicines that contain any of the following active substances:
- ketoconazole, to treat fungal infections.
- ritonavir, to treat HIV infection.
- rifampicin, an antibiotic to treat bacterial infections.
- carbamazepine, phenytoin, or phenobarbital, used to treat epilepsy.
- St. John's Wort, used for depression or other conditions.
- oral antidiabetics.
Pregnancy and breastfeeding
Do not use Bortezomib Accord if you are pregnant unless clearly necessary.
Both men and women using Bortezomib Accord must use effective contraception during and up to 3 months after treatment. If, despite these measures, you become pregnant, inform your doctor immediately.
Do not breastfeed while using Bortezomib Accord. Ask your doctor when it is safe to restart breastfeeding after finishing your treatment.
Thalidomide causes birth defects and fetal death. When Bortezomib Accord is given with thalidomide, you should follow the thalidomide pregnancy prevention program (see the thalidomide package leaflet).
Driving and using machines
Bortezomib Accord may cause fatigue, dizziness, fainting, or blurred vision. Do not drive or use tools or machines if you experience these side effects; even if you do not experience them, you should still be cautious.
3. How to use Bortezomib Accord
Your doctor will tell you the dose of Bortezomib Accord according to your height and weight (body surface area). The usual starting dose of Bortezomib Accord is 1.3 mg/m2 of body surface area twice a week. Your doctor may change the dose and the total number of treatment cycles depending on your response to treatment, the occurrence of certain side effects, and your underlying condition (e.g., liver problems).
Progressive multiple myeloma
When Bortezomib Accord is given alone, you will receive 4 doses of Bortezomib Accord by intravenous or subcutaneous injection on days 1, 4, 8, and 11, followed by a 10-day "rest" period without treatment. This 21-day period (3 weeks) is one treatment cycle. You may receive up to 8 cycles (24 weeks).
You may also receive Bortezomib Accord with the medicines doxorubicin liposomal pegylated or dexamethasone.
When Bortezomib Accord is given with doxorubicin liposomal pegylated, you will receive Bortezomib Accord by intravenous or subcutaneous injection in a 21-day treatment cycle, and doxorubicin liposomal pegylated 30 mg/m2 will be given on day 4 of the 21-day Bortezomib Accord treatment cycle by intravenous infusion after the Bortezomib Accord injection.
You may receive up to 8 cycles (24 weeks).
When Bortezomib Accord is given with dexamethasone, you will receive Bortezomib Accord by intravenous or subcutaneous injection in a 21-day treatment cycle, and dexamethasone 20 mg will be given orally on days 1, 2, 4, 5, 8, 9, 11, and 12 of the 21-day Bortezomib Accord treatment cycle.
You may receive up to 8 cycles (24 weeks).
Previously untreated multiple myeloma
If you have not been previously treated for multiple myeloma and are nota candidate to receive a stem cell transplant, you will receive Bortezomib Accord with the medicines melphalan and prednisone.
In this case, the duration of one treatment cycle is 42 days (6 weeks). You will receive 9 cycles (54 weeks).
- In cycles 1 to 4, Bortezomib Accord will be given twice a week on days 1, 4, 8, 11, 22, 25, 29, and 32.
- In cycles 5 to 9, Bortezomib Accord will be given once a week on days 1, 8, 22, and 29. Melphalan (9 mg/m2) and prednisone (60 mg/m2) will be given orally during days 1, 2, 3, and 4 of the first week of each cycle.
If you have not received previous treatment for multiple myeloma and area candidate to receive a stem cell transplant, you will receive Bortezomib Accord by intravenous or subcutaneous injection with the medicines dexamethasone, or dexamethasone and thalidomide, as induction treatment.
When Bortezomib Accord is given with dexamethasone, you will receive Bortezomib Accord by intravenous or subcutaneous injection in a 21-day treatment cycle, and dexamethasone will be given orally at a dose of 40 mg on days 1, 2, 3, 4, 8, 9, 10, and 11 of the 21-day Bortezomib Accord treatment cycle.
You may receive up to 4 cycles (12 weeks).
When Bortezomib Accord is given with thalidomide and dexamethasone, the duration of one treatment cycle is 28 days (4 weeks).
Dexamethasone 40 mg will be given orally on days 1, 2, 3, 4, 8, 9, 10, and 11 of the 28-day Bortezomib Accord treatment cycle, and thalidomide will be given orally once daily at a dose of 50 mg until day 14 of the first cycle, and if tolerated, the thalidomide dose may be increased to 100 mg on days 15-28 and from the second cycle onwards may be further increased to 200 mg daily.
You may receive up to 6 cycles (24 weeks).
Previously untreated mantle cell lymphoma
If you have not been previously treated for mantle cell lymphoma, you will receive Bortezomib Accord by intravenous or subcutaneous injection with the medicines rituximab, cyclophosphamide, doxorubicin, and prednisone.
Bortezomib Accord will be given by intravenous or subcutaneous injection on days 1, 4, 8, and 11, followed by a "rest" period without treatment. The duration of one treatment cycle is 21 days (3 weeks). You may receive up to 8 cycles (24 weeks).
The following medicines will be given by intravenous infusion on day 1 of the 21-day Bortezomib Accord treatment cycle:
Rituximab at a dose of 375 mg/m2, cyclophosphamide at a dose of 750 mg/m2, and doxorubicin at a dose of 50 mg/m2.
Prednisone will be given orally at a dose of 100 mg/m2 on days 1, 2, 3, 4, and 5 of the 21-day Bortezomib Accord treatment cycle.
How Bortezomib Accord is given
Bortezomib Accord must be administered by a healthcare professional experienced in the use of cytotoxic medicines.
This medicine is for subcutaneous use (injection under the skin), and after dilution, also for intravenous use (injection into a vein). The injection into a vein is rapid and lasts between 3 and 5 seconds. The injection under the skin is given into the thighs or abdomen.
If you receive more Bortezomib Accord than you should
This medicine will be administered by your doctor or nurse, so it is unlikely that you will receive too much. In the unlikely event of an overdose, your doctor will monitor you for side effects.
4. Possible side effects
Like all medicines, this medicine can cause side effects, although not everybody gets them. Some of these effects may be serious.
If you are given Bortezomib Accord for multiple myeloma or mantle cell lymphoma, tell your doctor immediately if you notice any of the following symptoms:
- muscle cramps, muscle weakness.
- confusion, vision loss, or changes in vision, blindness, seizures, headaches.
- difficulty breathing, swelling of the feet, or changes in heart rhythm, high blood pressure, fatigue, fainting.
- coughing and difficulty breathing or chest tightness.
Treatment with Bortezomib Accord may very commonly cause a decrease in the number of red and white blood cells and platelets in the blood. Therefore, you will need to have regular blood tests before and during treatment with Bortezomib Accord to check your blood cell count regularly. You may experience a reduction in the number of:
- platelets, which can make you more prone to bruising (bruises) or bleeding without apparent injury (e.g., intestinal, stomach, mouth, and gum bleeding, or bleeding in the brain or liver bleeding).
- red blood cells, which can cause anemia, with symptoms such as fatigue and paleness.
- white blood cells, which can make you more prone to infections or flu-like symptoms.
If you are given Bortezomib Accord for the treatment of multiple myeloma, the side effects you may experience are listed below:
Very common side effects (may affect more than 1 in 10 patients)
- Sensitivity, numbness, tingling, or burning sensation in the skin or pain in the hands or feet due to nerve damage.
- Decrease in the number of red and/or white blood cells (see above).
- Fever.
- Feeling sick (nausea) or vomiting, loss of appetite.
- Constipation with or without swelling (can be severe).
- Diarrhea: if it occurs, it is important to drink more water than usual. Your doctor may give you another medicine to control diarrhea.
- Exhaustion (fatigue), feeling weak.
- Muscle pain, bone pain.
Frequent Adverse Effects (may affect up to 1 in 10 patients)
- Low blood pressure, sudden drop in blood pressure when standing, which may lead to fainting
- High blood pressure
- Decreased kidney function
- Headache
- Feeling of general discomfort, pain, dizziness, drowsiness, feeling of weakness or loss of consciousness
- Chills
- Infections, including pneumonia, respiratory infections, bronchitis, fungal infections, cough with phlegm, flu-like illness
- Herpes zoster (localized, including around the eyes or spread throughout the body)
- Chest pain or difficulty breathing when exercising
- Various types of rashes
- Itching of the skin, skin bumps, or dry skin
- Facial flushing or rupture of small blood vessels
- Redness of the skin
- Dehydration
- Heartburn, bloating, belching, flatulence, stomach pain, intestinal or stomach bleeding
- Abnormal liver function
- Sores in the mouth or lip, dry mouth, mouth ulcers, or sore throat
- Weight loss, loss of taste
- Infection of the outer layer of the eye and the inner surface of the eyelids (conjunctivitis)
- Nosebleeds
- Difficulty sleeping or sleep disorders, sweating, anxiety, mood changes, depressed mood, restlessness, or agitation, changes in mental state, disorientation
- Swelling of the body, including around the eyes and in other parts of the body
Infrequent Adverse Effects (may affect up to 1 in 100 patients)
- Heart failure, heart attack, chest pain, chest discomfort, increased or decreased heart rate
- Kidney failure
- Inflammation of a vein, blood clots in the veins and lungs
- Blood coagulation problems
- Insufficient circulation
- Inflammation of the heart lining or fluid around the heart
- Infections, including urinary tract infections, flu, herpes virus infection, ear infection, and cellulitis
- Bleeding in the digestive tract or bleeding in the mucous membranes, for example, in the mouth or vagina
- Cerebrovascular disorders
- Paralysis, seizures, falls, movement disorders, alterations or changes in sensitivity (touch, hearing, taste, smell), attention disorders, tremors, shaking
- Arthritis, including inflammation of the joints of the hands and feet and jaw
- Disorders affecting the lungs, preventing the body from receiving enough oxygen. Some of these include difficulty breathing, shortness of breath, shortness of breath without exercise, shallow, difficult, or stopped breathing, panting
- Hiccup, speech disorders
- Increased or decreased urine production (due to kidney damage), pain when urinating, or blood/protein in the urine, fluid retention
- Altered level of consciousness, confusion, altered or lost memory
- Hypersensitivity
- Hearing loss, deafness, or ringing in the ears, ear discomfort
- Hormonal changes that can affect salt and water absorption
- Overactivity of the thyroid gland
- Inability to produce enough insulin or resistance to normal insulin levels
- Eye irritation or inflammation, watery eyes, eye pain, dry eyes, eye infections, eyelid cyst (chalazion), red and swollen eyelids, tearing, abnormal vision, eye bleeding
- Swelling of lymph nodes
- Stiffness of the joints or muscles, feeling of heaviness, pain in the groin
- Hair loss and abnormal hair texture
- Allergic reactions
- Redness or pain at the injection site
- Mouth pain
- Mouth or esophagus, stomach, and intestine infections or inflammation, sometimes associated with pain or bleeding, decreased intestinal movement (including obstruction), abdominal or esophageal discomfort, difficulty swallowing, vomiting blood
- Skin infections
- Bacterial and viral infections
- Dental infections
- Pancreatitis, obstruction of the bile ducts
- Genital pain, difficulty achieving an erection
- Weight gain
- Thirst
- Hepatitis
- Disorders at the injection site or related to the injection device
- Skin reactions and disorders (which can be severe and life-threatening), skin ulcers
- Bruises, falls, and injuries
- Inflammation or bleeding of blood vessels that can appear as small red or purple spots (usually on the legs) to large bruise-like patches under the skin or tissue
- Benign cysts
- A severe and reversible brain disorder that includes seizures, high blood pressure, headaches, fatigue, confusion, blindness, or other vision problems
Rare Adverse Effects (may affect up to 1 in 1,000 patients)
- Heart problems, including heart attack, angina pectoris
- Severe nerve inflammation, which can cause paralysis and breathing difficulties (Guillain-Barré syndrome)
- Flushing
- Discoloration of the veins
- Inflammation of the spinal nerves
- Ear problems, ear bleeding
- Underactive thyroid gland
- Budd-Chiari syndrome (clinical symptoms caused by obstruction of the hepatic veins)
- Changes or anomalies in intestinal function
- Cerebral hemorrhage
- Yellowing of the eyes and skin (jaundice)
- Severe allergic reaction (anaphylactic shock), whose signs can be difficulty breathing, pain or pressure in the chest and/or feeling of dizziness/fainting, intense itching of the skin or skin bumps, swelling of the face, lips, tongue, and/or throat, which can cause difficulty swallowing, collapse
- Breast disorders
- Vaginal tear
- Genital inflammation
- Inability to tolerate alcohol consumption
- Emaciation or loss of body mass
- Increased appetite
- Fistula
- Joint effusion
- Cysts in the joint lining (synovial cysts)
- Fracture
- Breakdown of muscle fibers that causes other complications
- Liver swelling, liver bleeding
- Kidney cancer
- Skin disease similar to psoriasis
- Skin cancer
- Pale skin
- Increased platelets or plasma cells (a type of white blood cell) in the blood
- Blood clot in small blood vessels (thrombotic microangiopathy)
- Abnormal reaction to blood transfusions
- Partial or total loss of vision
- Loss of libido
- Drooling
- Bulging eyes
- Sensitivity to light
- Rapid breathing
- Rectal pain
- Bile duct stones
- Hernia
- Wounds
- Weak or brittle nails
- Abnormal protein deposits in vital organs
- Coma
- Intestinal ulcers
- Multi-organ failure
- Death
If you are administered Bortezomib Accord along with other medications for the treatment of mantle cell lymphoma, the adverse effects you may experience are included below:
Very Frequent Adverse Effects (may affect more than 1 in 10 patients)
- Pneumonia
- Loss of appetite
- Sensitivity, numbness, tingling, or burning sensation in the skin or pain
of hands or feet due to nerve damage
- Nausea or vomiting
- Diarrhea
- Mouth ulcers
- Constipation
- Muscle pain, bone pain
- Hair loss and abnormal hair texture
- Exhaustion, feeling of weakness
- Fever
Frequent Adverse Effects (may affect up to 1 in 10 patients)
- Herpes zoster (localized, including around the eyes or spread throughout the body)
- Herpes virus infection
- Bacterial and viral infections
- Respiratory infections, bronchitis, cough with phlegm, flu-like illness
- Fungal infections
- Hypersensitivity (allergic reaction)
- Inability to produce enough insulin or resistance to normal insulin levels
- Fluid retention
- Difficulty sleeping or sleep disorders
- Loss of consciousness
- Altered level of consciousness, confusion
- Dizziness
- Increased heart rate, high blood pressure, sweating
- Abnormal vision, blurred vision
- Heart failure, heart attack, chest pain, chest discomfort, increased or decreased heart rate
- High or low blood pressure
- Sudden drop in blood pressure when standing, which may lead to fainting
- Difficulty breathing when exercising
- Cough
- Hiccup
- Ringing in the ears, ear discomfort
- Intestinal or stomach bleeding
- Heartburn
- Stomach pain, bloating
- Difficulty swallowing
- Stomach or intestine infection or inflammation
- Stomach pain
- Sores in the mouth or lip, sore throat
- Abnormal liver function
- Itching of the skin
- Redness of the skin
- Rash
- Muscle spasms
- Urinary tract infection
- Pain in the limbs
- Swelling of the body, including around the eyes and in other parts of the body
- Chills
- Redness and pain at the injection site
- Feeling of general discomfort
- Weight loss
- Weight gain
Infrequent Adverse Effects (may affect up to 1 in 100 patients)
- Hepatitis
- Severe allergic reaction (anaphylactic reaction), whose signs can be difficulty breathing, pain or pressure in the chest and/or feeling of dizziness/fainting, intense itching of the skin or skin bumps, swelling of the face, lips, tongue, and/or throat, which can cause difficulty swallowing, collapse
- Movement disorders, paralysis, shaking
- Dizziness
- Hearing loss, deafness
- Disorders affecting the lungs, preventing the body from receiving enough oxygen. Some of these include difficulty breathing, shortness of breath, shortness of breath without exercise, shallow, difficult, or stopped breathing, panting
- Blood clots in the lungs
- Yellowing of the eyes and skin (jaundice)
- Cyst in the eyelid (chalazion), red and swollen eyelids
Rare Adverse Effects (may affect up to 1 in 1,000 patients)
- Blood clot in small blood vessels (thrombotic microangiopathy)
- Severe nerve inflammation, which can cause paralysis and breathing difficulties (Guillain-Barré syndrome)
Reporting of Adverse Effects
If you experience any type of adverse effect, consult your doctor or pharmacist, even if it is a possible adverse effect that is not listed in this leaflet. You can also report them directly through the national reporting system included in Appendix V. By reporting adverse effects, you can contribute to providing more information on the safety of this medication.
5. Storage of Bortezomib Accord
Keep this medication out of sight and reach of children.
Do not use this medication after the expiration date shown on the vial and on the packaging after CAD.
Store in a refrigerator (between 2°C and 8°C).
Keep the vial in the outer packaging to protect it from light.
Diluted Solution
The chemical and physical stability of the diluted solution at a concentration of 1mg/ml has been shown to be stable for 24 hours at 20°C - 25°C. From a microbiological point of view, unless the opening/dilution method eliminates the risk of microbial contamination, the diluted solution should be used immediately after preparation. If not used immediately, the storage times and conditions before use are the responsibility of the user.
Bortezomib Accord is for single use only. The disposal of unused medication and all materials that have come into contact with it will be carried out in accordance with local regulations.
6. Package Contents and Additional Information
Composition of Bortezomib Accord
- The active ingredient is bortezomib. Each 1 ml or 1.4 ml vial of injectable solution contains 2.5 mg/ml of bortezomib (as boronic acid ester of mannitol).
- The other components are mannitol (E421) and water for injections.
Intravenous route:
after dilution, 1 ml of the solution for intravenous injection contains 1 mg of bortezomib.
Subcutaneous route:
1 ml of the solution for subcutaneous injection contains 2.5 mg of bortezomib.
Appearance of Bortezomib Accord and Package Contents
Bortezomib Accord powder for injectable solution is a clear, colorless solution.
Transparent glass vial Type 1 with gray rubber stopper, aluminum seal, and orange cap, containing 1 ml of injectable solution.
Transparent glass vial Type 1 with gray bromobutyl rubber stopper, aluminum seal, and red cap, containing 1.4 ml of injectable solution.
Package Sizes
1 vial x 1 ml
4 vials x 1 ml
1 vial x 1.4 ml
4 vials x 1.4 ml
Not all package sizes may be marketed.
Marketing Authorization Holder
Accord Healthcare S.L.U.
World Trade Center, Moll de Barcelona, s/n, Edifici Est 6ª planta,
08039 Barcelona,
Spain
Manufacturer
Accord Healthcare Polska Sp.z o.o., ul. Lutomierska 50, 95-200 Pabianice, Poland
Accord Healthcare B.V., Winthontlaan 200, 3526 KV Utrecht, Netherlands
Date of Revision of this Leaflet
Other Sources of Information
Detailed information about this medication is available on the European Medicines Agency website: http://www.ema.europa.eu
- Country of registration
- Availability in pharmacies
Supply issue reported
Data from the Spanish Agency of Medicines (AEMPS) indicates a supply issue affecting this medicine.<br><br>Availability may be limited in some pharmacies.<br><br>For updates or alternatives, consult your pharmacist. - Active substance
- Prescription requiredYes
- Manufacturer
- This information is for reference only and does not constitute medical advice. Always consult a doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to BORTEZOMIB ACCORD 2.5 mg/mL INJECTABLE SOLUTIONDosage form: INJECTABLE, 1 mgActive substance: bortezomibManufacturer: Accord Healthcare S.L.U.Prescription requiredDosage form: INJECTABLE, 3.5 mgActive substance: bortezomibManufacturer: Accord Healthcare S.L.U.Prescription requiredDosage form: INJECTABLE, 3.5 mgActive substance: bortezomibManufacturer: Eugia Pharma (Malta) LimitedPrescription required
Online doctors for BORTEZOMIB ACCORD 2.5 mg/mL INJECTABLE SOLUTION
Discuss questions about BORTEZOMIB ACCORD 2.5 mg/mL INJECTABLE SOLUTION, including use, safety considerations and prescription review, subject to medical assessment and local regulations.
Frequently Asked Questions






