AMBIRIX SUSPENSION FOR INJECTION IN PRE-FILLED SYRINGE


How to use AMBIRIX SUSPENSION FOR INJECTION IN PRE-FILLED SYRINGE
Translated with AI
This page provides general information and does not replace a doctor’s consultation. Always consult a doctor before taking any medication. Seek urgent medical care if symptoms are severe.
Show originalContents of the leaflet
Introduction
Package Leaflet: Information for the User
Ambirix, injectable suspension in a pre-filled syringe
Vaccine (HAB) (adsorbed) against hepatitis A (inactivated) and hepatitis B (ADNr)
Read all of this leaflet carefully before you or your child start receiving this vaccine, because it contains important information for you.
- Keep this leaflet, you may need to read it again.
- If you have any further questions, ask your doctor, pharmacist, or nurse.
- This vaccine has been prescribed for you or your child, do not pass it on to others.
- If you or your child experience any side effects, talk to your doctor, pharmacist, or nurse, even if they are not listed in this leaflet. See section 4.
This leaflet has been written assuming that the person receiving the vaccine is the one reading it. However, the vaccine can be administered to children and adolescents, so you may be reading it on behalf of your child.
Contents of the package leaflet
- What is Ambirix and what is it used for
- What you need to know before receiving Ambirix
- How to administer Ambirix
- Possible side effects
- Storage of Ambirix
- Contents of the pack and further information
1. What is Ambirix and what is it used for
Ambirix is a vaccine used in infants, children, and young people from 1 year of age up to and including 15 years of age. It is used to prevent two diseases: hepatitis A and hepatitis B.
- Hepatitis A:Infection with the hepatitis A virus can cause liver inflammation. The virus is acquired from food or drinks that contain the virus. However, it can sometimes be acquired through other means, such as swimming in sewage or from another infected person. The virus is present in body fluids such as feces, serum, or saliva.
Symptoms start between 3 and 6 weeks after infection. Some people may have nausea, fever, and pain. After several days, they may feel very tired, have dark urine, pale face, and yellowish skin or eyes (jaundice). The severity and type of symptoms can vary. It is possible that young children may not experience all the symptoms. Most children recover completely from the disease, although it is usually severe enough to make children ill for about a month.
- Hepatitis B:Infection with the hepatitis B virus can cause liver inflammation. The virus is usually acquired from another infected person. It is found in body fluids such as blood, semen, vaginal secretions, or saliva (sputum).
It is possible that no symptoms are observed during the 6 weeks or 6 months after infection. Infected people do not always feel or appear ill. Some people may have nausea, fever, and pain. However, others may become very ill. They may be very tired, have dark urine, pale face, and yellowish skin or eyes (jaundice). Some people may need to go to the hospital.
Most adults recover completely from the disease, although some people (particularly children) who have not had symptoms may remain infected. These people are known as "carriers" of hepatitis B and can continue to infect others throughout their lives. Additionally, carriers are at risk of serious liver problems, such as liver damage (cirrhosis) or liver cancer.
How Ambirix works
- Ambirix helps the body produce its own protection (antibodies) against these diseases. The vaccine does not contain live viruses (see section 6 for the content of the vaccine) and therefore cannot cause infections with the hepatitis A or B virus.
- As with all vaccines, some people may not respond as well to a vaccine as others.
- Ambirix may not protect you from the disease if you have already acquired the hepatitis A or B virus.
- Ambirix can only help protect you against infections with the hepatitis A or B virus. It cannot protect against other infections that can affect the liver, even if those infections have similar signs to those caused by the hepatitis A or B virus.
2. What you need to know before receiving Ambirix
Ambirix must not be administered if:
- you are allergic to Ambirix or any of the other components of this vaccine (listed in section 6). The signs of an allergic reaction can include a skin rash with itching, difficulty breathing, and swelling of your face or tongue.
- you have previously had an allergic reaction to any vaccine against hepatitis A or hepatitis B.
- you have a severe infection with a high fever. The vaccine can be administered once you have recovered. A minor infection, such as a cold, should not be a problem for vaccination, but consult your doctor first.
Ambirix must not be administered if you are in any of the above circumstances. If you are not sure, consult your doctor, pharmacist, or nurse before receiving Ambirix.
Warnings and precautions
Consult your doctor, pharmacist, or nurse before receiving Ambirix if:
- you need to be fully protected against hepatitis A and B infection within the next 6 months (your doctor may recommend a different vaccine).
- you have any bleeding problems or bruise easily (the injection can be given just under the skin instead of into a muscle to reduce bleeding or bruising).
- you have immune system problems (such as those caused by disease, medication, or dialysis), the vaccine may not work completely. This means you may not be protected against one or both of the hepatitis A and B viruses. Your doctor will perform blood tests to check if you need additional injections to help you be better protected.
- you have fainted in the past or during a previous injection, to prevent it from happening again. Fainting (especially in adolescents) can occur before or after any injection.
If you are in any of the above circumstances (or are unsure), consult your doctor, pharmacist, or nurse before receiving Ambirix.
Other medicines and Ambirix
Tell your doctor if you are using, have recently used, or might use any other medicines or vaccines. This includes medicines obtained without a prescription and herbal medicines. Ask your doctor, pharmacist, or nurse if you have any questions.
Although you are taking medicines that affect your body's immune response, you can receive Ambirix if it is considered necessary. However, the vaccine may not work completely. This means you may not be protected against one or both of the hepatitis A and B viruses. Your doctor will perform blood tests to determine if you need additional injections to help you be better protected.
Ambirix can be administered at the same time as other vaccines against measles, mumps, rubella, diphtheria, tetanus, pertussis, poliomyelitis, Haemophilus influenzaetype b, or some types of treatments for liver infections called "immunoglobulins". Your doctor will ensure that the vaccines are injected into different parts of your body.
Pregnancy, breastfeeding, and fertility
If you are pregnant or breastfeeding, think you may be pregnant, or plan to become pregnant, consult your doctor, pharmacist, or nurse before receiving this vaccine. Ambirix is not normally administered to pregnant or breastfeeding women.
Driving and using machines
You may feel drowsy or dizzy after receiving Ambirix. If this happens, do not drive or ride a bicycle or use tools or machines.
Ambirix contains neomycin and sodium
This vaccine contains neomycin (an antibiotic). Ambirix must not be administered if you are allergic to neomycin.
This vaccine contains less than 1 mmol of sodium (23 mg) per dose; it is essentially "sodium-free".
3. How to administer Ambirix
How the injection is administered
- Your doctor or nurse will administer Ambirix as an injection into a muscle, usually in the upper arm.
- They will make sure that Ambirix is not administered into a vein.
- In very young children, the injection can be administered into the thigh muscle.
How much to administer
- You will normally receive a total of two injections. Each one is administered on a separate visit.
- The injections will be administered within a period of 12 months:
- The first injection - on a date agreed with your doctor.
- The second injection - between 6 and 12 months after the first injection.
Your doctor will advise you on the need for additional doses and future booster doses.
If you miss a dose
- If you miss the second injection, talk to your doctor to schedule another visit as soon as possible.
- Make sure you complete the full series of two injections. Otherwise, you may not be protected against the diseases.
4. Possible side effects
Like all medicines, this vaccine can cause side effects, although not everybody gets them.
Serious side effects
- Tell your doctor immediately if you notice any of the following serious side effects (you may need urgent medical treatment):anaphylactic and allergic reactions: the signs can include a skin rash with itching or blisters, swelling of the eyes and face, difficulty breathing or swallowing, sudden drop in blood pressure, and loss of consciousness.
Tell your doctor immediately if you notice any of the serious side effects listed above.
The side effects that occurred during clinical trials with Ambirix were the following:
Very common(may occur in more than 1 in 10 doses of the vaccine): headache, loss of appetite, feeling tired or irritable, pain and redness at the injection site.
Common(may occur in up to 1 in 10 doses of the vaccine): fever, feeling drowsy, stomach and digestive problems, swelling at the injection site.
Additional side effects reported during clinical trials with combined hepatitis A and hepatitis B vaccines very similar to this one include:
Common(may occur in up to 1 in 10 doses of the vaccine): general feeling of being unwell, diarrhea, nausea, reaction at the injection site.
Uncommon(may occur in up to 1 in 100 doses of the vaccine): feeling dizzy, stomach pain, vomiting, upper respiratory tract infections, muscle pain (myalgia).
Rare(may occur in up to 1 in 1,000 doses of the vaccine): low blood pressure, joint pain (arthralgia), itching (pruritus), skin rash, tingling (paresthesia), swelling of the lymph nodes in the neck, armpits, and groin (lymphadenopathy), flu-like symptoms such as high temperature, sore throat, runny nose, cough, and chills.
Very rare(may occur in up to 1 in 10,000 doses of the vaccine): hives (urticaria).
Contact your doctor if you experience any side effects similar to these.
Side effects that occurred during routine use of Ambirix were the following:fainting, loss of skin sensitivity to pain or touch (hypoesthesia).
Additional side effects that occurred during routine use of combined or individual hepatitis A and hepatitis B vaccines very similar to this one were the following:multiple sclerosis, spinal cord swelling (myelitis), abnormal liver test results, brain swelling or infection (encephalitis), inflammation of some blood vessels (vasculitis), a degenerative brain disease (encephalopathy), swelling of the face, mouth, and throat (angioneurotic edema), severe headache with stiff neck and sensitivity to light (meningitis), a temporary inflammation of the nerves that causes pain, weakness, and paralysis in the arms and legs and often progresses to the chest and face (Guillain-Barré syndrome), seizures or fits, nerve inflammation (neuritis), eye nerve disease (optic neuritis), numbness or weakness of the arms and legs (neuropathy), immediate pain at the injection site, burning sensation, paralysis, drooping eyelid and dropped muscles on one side of the face (facial paralysis), a disease that mainly affects the joints with pain and swelling (arthritis), muscle weakness, purple or reddish-purple spots on the skin (lichen planus), severe skin rashes (erythema multiforme), reduction of blood platelets, which increases the risk of bleeding or bruising (thrombocytopenia), purple or brownish-purple spots visible through the skin (thrombocytopenic purpura).
Reporting side effects
If you experience any side effects, talk to your doctor or pharmacist, even if they are not listed in this leaflet. You can also report them directly through the national reporting system included in Appendix V. By reporting side effects, you can help provide more information on the safety of this medicine.
5. Storage of Ambirix
Keep this vaccine out of the sight and reach of children.
Do not use this vaccine after the expiry date stated on the packaging. The expiry date is the last day of the month stated.
Store in a refrigerator (between 2°C and 8°C). Do not freeze. Freezing destroys the vaccine.
Store in the original packaging to protect it from light.
Medicines should not be disposed of via wastewater or household waste. Ask your pharmacist how to dispose of medicines no longer required. This will help protect the environment.
6. Container contents and additional information
Ambirix composition
- The active ingredients are:
- Hepatitis A virus (inactivated)1,2 720 ELISA Units
- Hepatitis B surface antigen3,4 20 micrograms
1Produced in human diploid cells (MRC-5)
2Adsorbed on hydrated aluminum hydroxide 0.05 milligrams Al3+
3Produced by recombinant DNA technology in yeast cells (Saccharomyces cerevisiae)
4Adsorbed on aluminum phosphate 0.4 milligrams Al3+
- The other components of Ambirix are: sodium chloride and water for injections.
Product appearanceand container contents
Ambirix is a white and slightly milky liquid.
Ambirix is available in a pre-filled syringe with or without separate needles, in pack sizes of 1, 10, and 50.
Only some pack sizes may be marketed.
Marketing authorization holder and manufacturer
GlaxoSmithKline Biologicals s.a.
Rue de l’Institut 89
B-1330 Rixensart
Belgium
For further information on this medicinal product, please contact the local representative of the marketing authorization holder:
België/Belgique/Belgien GlaxoSmithKline Pharmaceuticals SA/NV Tél/Tel: + 32 10 85 52 00 | Lietuva GlaxoSmithKline Biologicals SA Tel. + 370 80000334 |
България GlaxoSmithKline Biologicals SA Тел.: + 359 80018205 | Luxembourg/Luxemburg GlaxoSmithKline Pharmaceuticals SA/NV Tél/Tel: + 32 10 85 52 00 |
Ceská republika GlaxoSmithKline s.r.o. Tel: + 420 2 22 00 11 11 | Magyarország GlaxoSmithKline Biologicals SA Tel.: + 36 80088309 |
Danmark GlaxoSmithKline Pharma A/S Tlf: + 45 36 35 91 00 | Malta GlaxoSmithKline Biologicals SA Tel: + 356 80065004 |
Deutschland GlaxoSmithKline GmbH & Co. KG Tel: + 49 (0)89 360448701 | Nederland GlaxoSmithKline BV Tel: + 31 (0)33 2081100 |
Eesti GlaxoSmithKline Biologicals SA Tel: + 372 8002640 | Norge GlaxoSmithKline AS Tlf: + 47 22 70 20 00 |
Ελλάδα GlaxoSmithKline Μονοπρ?σωπη A.E.B.E. Τηλ: + 30 210 68 82 100 | Österreich GlaxoSmithKline Pharma GmbH. Tel: + 43 (0)1 97075-0 |
España GlaxoSmithKline, S.A. Tel: + 34 900 202 700 | Polska GSK Services Sp. z o.o. Tel.: + 48 (22) 576 9000 |
France Laboratoire GlaxoSmithKline Tél: + 33 (0) 1 39 17 84 44 Hrvatska GlaxoSmithKline Biologicals SA Tel.: + 385 800787089 | Portugal Smith Kline & French Portuguesa - Produtos Farmacêuticos, Lda. Tel: + 351 21 412 95 00 România GlaxoSmithKline Biologicals SA Tel: + 40 800672524 |
Ireland GlaxoSmithKline (Ireland) Ltd Tel: + 353 (0)1 495 5000 | Slovenija GlaxoSmithKline Biologicals SA Tel: + 386 80688869 |
Ísland Vistor hf. Sími: + 354 535 7000 | Slovenská republika GlaxoSmithKline Biologicals SA Tel: + 421 800500589 |
Italia GlaxoSmithKline S.p.A. Tel: + 39 (0)45 7741 111 | Suomi/Finland GlaxoSmithKline Oy Puh/Tel: + 358 (0)10 30 30 30 |
Κύπρος GlaxoSmithKline Biologicals SA Τηλ: + 357 80070017 | Sverige GlaxoSmithKline AB Tel: + 46 (0)8 638 93 00 |
Latvija GlaxoSmithKline Biologicals SA Tel: + 371 80205045 | United Kingdom(Northern Ireland) GlaxoSmithKline Biologicals SA Tel: + 44 (0)800 221441 |
Date of last revision of this leaflet:
Other sources of information
Detailed information on this medicinal product is available on the European Medicines Agency website: http://www.ema.europa.eu, and on the website of the Spanish Agency for Medicines and Health Products (AEMPS) (http://www.aemps.gob.es/).
---------------------------------------------------------------------------------------------------------------------
This information is intended only for healthcare professionals:
During storage, a fine white deposit with a clear and colorless layer on top may be observed.
The vaccine should be resuspended before use. Once resuspended, the vaccine will have a white, cloudy, and uniform appearance.
Resuspension of the vaccine to obtain a white, cloudy, and uniform suspension
The vaccine should be resuspended by following the steps below.
- Hold the syringe upright with the hand closed.
- Shake the syringe by turning it upside down and then back upright.
- Repeat this action vigorously for at least 15 seconds.
- Inspect the vaccine again:
- If the vaccine appears as a white, cloudy, and uniform suspension, it is ready to use (it should not have a clear appearance).
- If the vaccine still does not appear as a white, cloudy, and uniform suspension, turn it upside down and then back upright for at least another 15 seconds and then inspect again.
Before administration, the vaccine should be visually inspected for any foreign particles and/or abnormal physical appearance. If any of these circumstances are observed, do not administer the vaccine.
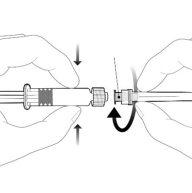
Instructions for the pre-filled syringe after resuspension
| Hold the syringe by the body, not by the plunger. Unscrew the syringe cap by turning it counterclockwise. | |
| To insert the needle, connect the base to the Luer-Lock adapter and turn it a quarter turn clockwise until it clicks. Do not pull the plunger out of the syringe body. If this happens, do not administer the vaccine. |
Disposal of waste
Disposal of unused medicinal products and all materials that have come into contact with them should be done in accordance with local regulations.
- Country of registration
- Active substance
- Prescription requiredYes
- Manufacturer
- This information is for reference only and does not constitute medical advice. Always consult a doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to AMBIRIX SUSPENSION FOR INJECTION IN PRE-FILLED SYRINGEDosage form: INJECTABLE, UnknownActive substance: combinationsManufacturer: Glaxosmithkline BiologicalsPrescription requiredDosage form: INJECTABLE, UnknownActive substance: combinationsManufacturer: Glaxosmithkline BiologicalsPrescription requiredDosage form: INJECTABLE, UnknownActive substance: combinationsManufacturer: Glaxosmithkline BiologicalsPrescription required
Online doctors for AMBIRIX SUSPENSION FOR INJECTION IN PRE-FILLED SYRINGE
Discuss questions about AMBIRIX SUSPENSION FOR INJECTION IN PRE-FILLED SYRINGE, including use, safety considerations and prescription review, subject to medical assessment and local regulations.
Frequently Asked Questions