
ROPSINE 10 mg/ml INJECTABLE SOLUTION


How to use ROPSINE 10 mg/ml INJECTABLE SOLUTION
Translated with AI
This page provides general information and does not replace a doctor’s consultation. Always consult a doctor before taking any medication. Seek urgent medical care if symptoms are severe.
Show originalContents of the leaflet
Introduction
Package Leaflet: Information for the User
Ropsine10 mg/ml injectable solution EFG
Ropivacaine, hydrochloride
Read all of this leaflet carefully before you start using this medicine.
- Keep this leaflet, you may need to read it again.
- If you have any further questions, ask your doctor or pharmacist.
- This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their symptoms are the same as yours.
- If you experience any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet. See section 4.
Contents of the pack:
- What Ropsine is and what it is used for
- What you need to know before you use Ropsine
- How to use Ropsine
- Possible side effects
- Storage of Ropsine 6. Contents of the pack and further information
1. What Ropsine is and what it is used for
Ropsine contains the active substance ropivacaine hydrochloride, which belongs to a class of medicines called local anesthetics.
Ropsine 10 mg/ml injectable solution is used in adults and adolescents over 12 years of age to numb (anesthetize) parts of the body. It is used to stop or relieve pain. It can be used for:
- Numbing a part of the body during surgery, including having a baby by cesarean section.
- Relieving pain during childbirth, after surgery, or after an accident.
2. What you need to know before you use Ropsine
Do not useRopsine
- if you are allergic(hypersensitive) to ropivacaine hydrochloride, to any other amide-type local anesthetic, or to any of the other ingredients of Ropsine (listed in section 6),
- if you have a reduced blood volume(hypovolemia). This will be measured by healthcare personnel,
- to inject it into a blood vesselto numb a specific area of your body,
- to inject it into the cervixto relieve pain during childbirth.
Warnings and precautions
Talk to your doctor or pharmacist before you start using Ropsine
In children up to 12 years of age, other concentrations (2 mg/ml, 5 mg/ml) may be more suitable.
Special care should be taken to avoid any injectionof Ropsine directly into a blood vesselto prevent any immediate toxic effects. The injection should not be performed in an inflamed area.
Tell your doctor:
- if you have a poor general conditiondue to age or other factors,
- if you have heart problems(partial or complete heart block),
- if you have an advanced liver problem,
- if you have severe kidney problems.
Tell your doctor if you have any of these problems, as your doctor will need to adjust your dose of Ropsine.
Tell your doctor:
- if you have acute porphyria(problems with the production of red blood cell pigments, sometimes resulting in neurological symptoms).
Tell your doctor if you or a family member has porphyria, as your doctor may need to use another anesthetic.
Using Ropsine with other medicines
Tell your doctor or pharmacist if you are using, have recently used, or might use any other medicines.
Caution should be exercised if you are receiving:
- Other local anesthetics(e.g., lidocaine) or structurally related agents to amide-type local anesthetics, e.g., certain medicines used to treat irregular heartbeats (arrhythmia), such as mexiletine or amiodarone,
- General anestheticsor opioids, such as morphine or codeine,
- Medicines used to treat depression(e.g., fluvoxamine),
- Certain antibiotics(e.g., enoxacin).
Pregnancy and breastfeeding
If you are pregnant or breastfeeding, think you may be pregnant, or are planning to have a baby, ask your doctor or pharmacist for advice before using this medicine. It is not known if ropivacaine hydrochloride affects pregnancy or if it passes into breast milk.
Driving and using machines
Ropsine may cause drowsiness and affect your reaction speed. Do not drive or use tools or machines after taking Ropsine, until the next day.
Ask your doctor or pharmacist if you have any questions.
Important information about some of the ingredients of Ropsine
This medicine contains 2.8 mg of sodium (a major component of table/cooking salt) in each ml. This is equivalent to 0.14% of the maximum recommended daily sodium intake for an adult.
3. How to use Ropsine
Method of administration
Ropsine will be administered to you by your doctor. It will be given to you by injection.
Dose
The recommended dose will depend on what it is being used for and also on your health, age, and weight.
The smallest dose that can produce a numbing effect (anesthesia) of the required area should be used.
The usual dose
- for adultsand adolescents over 12 years of ageis between 2 mg and 300 mgof ropivacaine hydrochloride.
- in infants and children(from 0 to 12 years, inclusive) is between 1-3 mg per kilogramof body weight.
Duration of treatment
The administration of ropivacaine hydrochloride usually lasts between 2 and 10 hoursin the case of anesthesiabefore certain surgeries and can last up to 72 hoursin the case of pain relief during or after surgery.
If you are given too much Ropsine
The first symptoms of being given too much ropivacaine hydrochloride are usually problems related to:
- hearing and vision,
- numbness around the mouth,
- dizziness or fainting,
- tingling,
- speech disorders characterized by poor articulation (dysarthria),
- muscle stiffness, muscle spasms, seizures (convulsions),
- low blood pressure,
- slow or irregular heartbeat.
These symptoms can precede a heart attack, respiratory arrest, or severe seizures.
If you experience any of these symptoms or think you may have been given too much Ropsine, tell your doctor or healthcare personnel immediately.
In case of acute toxicity, the appropriate corrective measures will be taken immediately by healthcare personnel.
If you have any further questions on the use of this product, ask your doctor or pharmacist.
4. Possible side effects
Like all medicines, Ropsine can cause side effects, although not everybody gets them.
Important side effects to look out for:
Sudden and potentially life-threatening allergic reactions (e.g., anaphylaxis, including anaphylactic shock) are rare and affect 1 to 10 people in every 10,000. Possible symptoms include:
- sudden onset of rash, itching, or hives (urticaria);
- swelling of the face, lips, tongue, or other parts of the body;
- shortness of breath, wheezing, or difficulty breathing;
- and a feeling of loss of consciousness.
If you think you are having an allergic reaction to Ropsine, tell your doctor or healthcare personnel immediately.
Other possible side effects:
Very common(may affect more than 1 in 10 people)
- Low blood pressure (hypotension). This may make you feel dizzy or faint.
- Feeling sick (nausea).
Common(may affect up to 1 in 10 people)
- Headache, tingling (paresthesia), feeling dizzy.
- Slow or fast heartbeat (bradycardia, tachycardia).
- High blood pressure (hypertension).
- Feeling sick (vomiting).
- Difficulty urinating (urinary retention).
- Back pain, high temperature, muscle stiffness.
Uncommon(may affect up to 1 in 100 people)
- Anxiety.
- Some symptoms may appear if the injection was accidentally given into a blood vessel or if you were given too much Ropsine (see also section 3 "If you are given too much Ropsine" above). These include seizures (convulsions), feeling dizzy or faint, numbness of the lips and around the mouth, numbness of the tongue, hearing problems, vision problems (vision), speech problems (dysarthria), muscle stiffness, and tremors, decreased sense of touch (hypoesthesia).
- Fainting (syncope).
- Difficulty breathing (dyspnea).
- Low body temperature.
Rare(may affect up to 1 in 1,000 people)
- Heart attack, irregular heartbeat (arrhythmias).
Other possible side effects that may be caused by Ropsine include:
- Numbness due to irritation of the nerves caused by the needle or the injection. This usually does not last long.
- Nerve damage. Rarely, it can cause permanent problems.
- If too much Ropsine is administered into the spinal fluid, it can numb the entire body (anesthetize it).
Additional side effects in children
In children, the side effects are the same as in adults, except for low blood pressure, which is less common in children (affects less than 1 in 10 children), and feeling sick, which is more common in children (affects more than 1 in 10 children).
If you think any of the side effects you are experiencing are serious or if you notice any side effects not listed in this leaflet, tell your doctor or pharmacist.
Reporting side effects
If you experience any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet. You can also report side effects directly through the Spanish Medicines Monitoring System for Human Use: https://www.notificaram.es. By reporting side effects, you can help provide more information on the safety of this medicine.
5. Storage of Ropsine
Keep this medicine out of the sight and reach of children.
Do not use Ropsine after the expiry date stated on the ampoule or carton. The expiry date is the last day of the month stated.
Do not freeze.
Do not use Ropsine if you notice any precipitation in the injection solution.
Normally, your doctor or hospital will store Ropsine and are responsible for the quality of the product if it is not used immediately after opening. They are also responsible for disposing of any unused Ropsine properly.
Medicines should not be disposed of via wastewater or household waste. Ask your pharmacist how to dispose of medicines no longer required. This will help protect the environment.
6. Container Contents and Additional Information
Composition ofRopsine
- The active ingredient is ropivacaine hydrochloride 10 mg/ml. Each 10 ml polypropylene ampoule contains 100 mg of ropivacaine (as hydrochloride).
Each 20 ml polypropylene ampoule contains 200 mg of ropivacaine (as hydrochloride).
- The other components are sodium chloride, sodium hydroxide (for pH adjustment), and water for injectable preparations.
Appearance of the Product and Container Contents
Ropsine injectable solution is a clear, colorless, sterile, isotonic, isobaric aqueous solution.
Ropsine 10 mg/ml injectable solution EFG is available in 10 ml and 20 ml transparent polypropylene ampoules.
Package size:
10 sterile ampoules in a plastic blister pack.
Marketing Authorization Holder and Manufacturer
Marketing Authorization Holder:
Sintetica GmbH
Albersloher Weg 11
48155 Münster
Germany
Manufacturer:
Sintetica GmbH
Albersloher Weg 11
48155 Münster
Germany
Date of Last Revision of this Leaflet:September 2023.
Detailed and updated information on this medicinal product is available on the website of the Spanish Agency for Medicines and Health Products (AEMPS) http://www.aemps.gob.es/.
-----------------------------------------------------------------------------------------------------------------------
This information is intended solely for doctors or healthcare professionals:
Handling
Ropsine should be used by, or under the supervision of, experienced anesthesiologists (see section 3)
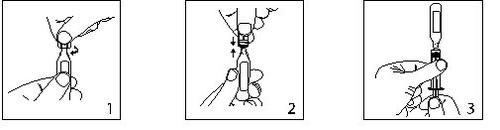
- Keep the ampoule in a vertical position and twist the neck to eliminate any remaining solution.
Open by twisting the top of the ampoule sharply.
- The ampoule can be connected directly to the syringe as shown in fig.2.
The ampoules fit both Luerfit and LuerLock syringes.
- Hold the syringe with the ampoule upwards. Without squeezing the ampoule, withdraw the solution. Maintain downward pressure on the syringe plunger once the solution has been withdrawn and until the empty ampoule is discarded.
Shelf Life before Opening
3 years
Shelf Life after Opening
From a microbiological point of view, the product should be used immediately. If not used immediately, the storage conditions during use and before administration are the responsibility of the user and generally should not exceed 24 hours at 2-8°C.
Ropsine medicines are preservative-free products intended for single use. Discard any unused solution.
The medicinal product should be inspected visually before use. The solution should only be used if the solution is clear, practically free of particles, and the container is intact.
The intact container should not be re-introduced into the autoclave.
Posology
Adults and Adolescents over 12 years of age
The table below is a guide to the most commonly used doses in different types of blocks. The smallest dose required to produce an effective block should be used. Clinical experience and knowledge of the patient's clinical condition are important factors in deciding the dose.
Indication | Concentration mg/ml | Volume ml | Dose mg | Onset of Action minutes | Duration hours |
Surgical Anesthesia | |||||
Lumbar Epidural Administration | |||||
Surgery | 7.5 | 15-25 | 113-188 | 10-20 | 3-5 |
10.0 | 15-20 | 150-200 | 10-20 | 4-6 | |
Cesarean Section | 7.5 | 15-20 | 113-150 | 10-20 | 3-5 |
Thoracic Epidural Administration | |||||
Establishing a block for postoperative pain relief | 7.5 | 5-15 (depending on the level of injection) | 38-113 | 10-20 | -- |
Nerve Trunk Block | |||||
Brachial Plexus Block | 7.5 | 30-40 | 225-300 | 10-25 | 6-10 |
Peripheral Block | |||||
For example, minor nerve block and infiltration | 7.5 | 1-30 | 7.5-225 | 1-15 | 2-6 |
The doses shown in the table are those considered necessary to produce an adequate block and should be considered as recommendations for use in adults. There are individual variations in the onset and duration of action. The figures in the "Dose" column reflect the expected average dose range. Suitable literature should be consulted for factors affecting specific block techniques and the requirements of each patient. |
- Regarding nerve trunk block, a dosing recommendation can only be given for the brachial plexus. For other nerve trunk blocks, lower doses may be required. However, there is currently no experience for specific dosing recommendations for other blocks.
- The dose should be administered in a stepwise manner. The initial dose of approximately 100 mg (97.5 mg = 13 ml; 105 mg = 14 ml) should be administered over 3-5 minutes, and if necessary, two additional doses of up to 50 mg each may be administered.
- The dose used for nerve trunk block should be adjusted according to the site of administration and the patient's condition. Interscalene and supraclavicular brachial plexus blocks may be associated with a higher frequency of serious adverse reactions, regardless of the local anesthetic used (see section 4.4).
Generally, surgical anesthesia (e.g., epidural administration) requires the use of higher concentrations and doses. For surgical procedures requiring deep motor block, epidural anesthesia using the Ropsine 10 mg/ml formulation is recommended. For analgesia (e.g., epidural administration for acute pain treatment), lower concentrations and doses are recommended.
Method of Administration
Perineural and epidural administration by injection.
Before and during injection, careful aspiration is recommended to prevent intravascular injection. When a higher dose is to be injected, a test dose of 3-5 ml of 2% lidocaine (lignocaine) with adrenaline (epinefrine) 1:200,000 is recommended. Accidental intravascular injection can be recognized by a temporary increase in heart rate, and accidental intrathecal injection by signs of spinal block.
Aspiration should be performed before and during administration of the main dose, which should be injected slowly or in increasing doses, at a rate of 25-50 mg/minute, while constantly monitoring the patient's vital functions and maintaining verbal contact with them. If toxic symptoms appear, administration of the medicinal product should be discontinued immediately.
In epidural block for surgery, single doses of up to 250 mg of ropivacaine hydrochloride have been well tolerated.
In brachial plexus block in a limited number of patients, a single dose of 300 mg has been well tolerated.
When prolonged blocks are required, either through continuous infusion or repeated bolus administration, the risks of achieving a toxic plasma concentration or inducing local neural injury should be considered. Accumulated doses of up to 675 mg of ropivacaine hydrochloride for surgery and postoperative analgesia administered over 24 hours were well tolerated in adults, as well as continuous postoperative epidural infusions at rates of up to 28 mg/hour over 72 hours. In a limited number of patients, higher doses of up to 800 mg/day have been administered with relatively few adverse reactions.
For the treatment of postoperative pain, the following technique is recommended: Unless treatment with Ropivacaine is started before the intervention, an epidural block is induced with it at a concentration of 7.5 mg/ml using an epidural catheter. Analgesia is maintained with a Ropsine 2 mg/ml infusion. Infusion rates of 6-14 ml (12-28 mg) per hour provide adequate analgesia with only slight and non-progressive motor block in most cases with moderate to severe postoperative pain. The maximum duration of epidural block is 3 days. However, close monitoring of the analgesic effect should be performed to remove the catheter as soon as the pain allows. With this technique, a significant reduction in the need for opioids has been observed.
In clinical studies, an epidural infusion of 2 mg/ml ropivacaine hydrochloride alone or mixed with 1-4 μg/ml fentanyl for the treatment of postoperative pain over a period of up to 72 hours has been administered. This combination of ropivacaine hydrochloride and fentanyl provided better pain relief but caused opioid-like side effects; this combination has only been investigated for ropivacaine hydrochloride 2 mg/ml.
When prolonged peripheral nerve blocks are applied, either through continuous infusion or repeated injections, the risks of achieving a toxic plasma concentration or inducing local neural injury should be considered. In clinical studies, a femoral nerve block was established with 300 mg of ropivacaine hydrochloride 7.5 mg/ml and an interscalene block with 225 mg of ropivacaine hydrochloride 7.5 mg/ml, respectively, before surgery; then analgesia was maintained with ropivacaine hydrochloride 2 mg/ml. Infusion rates or intermittent injections of 10-20 mg per hour over 48 hours provided adequate analgesia and were well tolerated.
Pediatric Population from 0 to 12 years of age inclusive
The use of Ropsine 10 mg/ml may be associated with systemic and central toxic events in children. Lower concentrations (2 mg/ml, 5 mg/ml) are more suitable for administration in this population.
The use of ropivacaine hydrochloride in premature neonates has not been studied in any of the administration forms.
Method of Administration
Epidural administration by injection.
Careful aspiration is recommended before and during injection to prevent intravascular injection. The patient's vital functions should be closely monitored during injection. If toxic symptoms occur, the injection should be discontinued immediately.
A single epidural caudal injection of 2 mg/ml ropivacaine hydrochloride provides adequate post-surgical analgesia below T12 in most patients when a dose of 2 mg/kg in a volume of 1 ml/kg is used. The volume of the epidural caudal injection can be adjusted to achieve a different distribution of the sensory block, as recommended in the literature. Doses of up to 3 mg/kg of a ropivacaine hydrochloride concentration of 3 mg/ml have been studied in children over 4 years; however, this concentration is associated with a higher incidence of motor block.
It is recommended to fractionate the calculated dose of local anesthetic, regardless of the route of administration.
In case an infusion of ropivacaine hydrochloride is recommended, Ropsine injectable solution can be used.
Incompatibilities
Compatibilities with other solutions have not been investigated, so this medicinal product should not be mixed with other medicines.
Precipitation can occur in alkaline solutions since ropivacaine hydrochloride shows poor solubility at pH > 6.0.
Disposal
Disposal of unused medicinal products and all materials that have come into contact with them should be carried out in accordance with local regulations.
- Country of registration
- Active substance
- Prescription requiredYes
- Manufacturer
- This information is for reference only and does not constitute medical advice. Always consult a doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to ROPSINE 10 mg/ml INJECTABLE SOLUTIONDosage form: INJECTABLE, 100 mgActive substance: ropivacaineManufacturer: Altan Pharmaceuticals SaPrescription requiredDosage form: INJECTABLE PERFUSION, 2 mg/mlActive substance: ropivacaineManufacturer: Altan Pharmaceuticals SaPrescription requiredDosage form: INJECTABLE, 75 mgActive substance: ropivacaineManufacturer: Altan Pharmaceuticals SaPrescription required
Online doctors for ROPSINE 10 mg/ml INJECTABLE SOLUTION
Discuss questions about ROPSINE 10 mg/ml INJECTABLE SOLUTION, including use, safety considerations and prescription review, subject to medical assessment and local regulations.
Frequently Asked Questions















