

Optirai 300

Ask a doctor about a prescription for Optirai 300

How to use Optirai 300
PATIENT INFORMATION LEAFLET
Information for the user: package leaflet
Optiray 300 solution for injection and infusion, 636 mg/ml
(Ioversol)
Read the leaflet carefully before using the medicine, as it contains important information for the patient.
- Keep this leaflet, you may need to read it again.
- Consult a doctor or pharmacist if you have any further questions.
- If you experience any side effects, including any not listed in this leaflet, tell your doctor or pharmacist.
Table of contents of the leaflet
- 1. What is Optiray and what is it used for
- 2. Important information before using Optiray
- 3. How to use Optiray
- 4. Possible side effects
- 5. How to store Optiray
- 6. Package contents and other information
1. What is Optiray and what is it used for
Optiray is used in various radiological examinations, including:
- vascular imaging, both arterial and venous (in adults and children)
- kidney imaging(in adults and children)
- computed tomography(in adults)
Optiray is a contrast agent containing iodine. Iodine blocks X-ray radiation, which allows visualization of blood vessels and internal organs through which blood flows.
2. Important information before using Optiray
When not to use Optiray:
- if the patient is allergicto iodine-containing contrast agentsor any of the other ingredients of this medicine (listed in section 6).
- if the patient has hyperthyroidism
Warnings and precautions
Before starting Optiray, consult a doctor if the patient has:
- asthma or a history of allergic reactions, such as nausea, vomiting, low blood pressure, skin symptoms
- heart failure, high blood pressure, circulatory disorders, or stroke, and if the patient is elderly
- diabetes
- kidney or liver disease
- brain disorders
- bone marrow disorders, such as certain blood cancers, called paraproteinemia, multiple myeloma
- certain red blood cell disorders, called sickle cell anemia
- adrenal gland tumor affecting blood pressure, called pheochromocytoma
- increased homocysteine levels due to metabolic disorders
- recent gallbladder examination using a contrast agent
- planned thyroid examination using an iodine-containing substance. It should be postponed, as Optiray may affect the results for up to 16 days.
- In patients who received Optiray, severe skin reactions have been reported, such as eosinophilia and systemic symptoms (DRESS), Stevens-Johnson syndrome (SJS), toxic epidermal necrolysis (Lyell's syndrome or TEN), and acute generalized exanthematous pustulosis (AGEP), which can be life-threatening.
- During or shortly after the imaging procedure, a temporary brain disorder called encephalopathy may occur. Immediately inform the doctor if any symptoms related to this condition described in section 4 are noticed.
Severe skin reactions have been reported in patients who received Optiray, such as eosinophilia and systemic symptoms (DRESS), Stevens-Johnson syndrome (SJS), toxic epidermal necrolysis (Lyell's syndrome or TEN), and acute generalized exanthematous pustulosis (AGEP), which can be life-threatening. During or shortly after the imaging procedure, a temporary brain disorder called encephalopathy may occur. Immediately inform the doctor if any symptoms related to this condition described in section 4 are noticed.
Children and adolescents under 18 years of age
Children under 18 years of age
Optiray 300 is used for vascular or kidney imaging in this age group.
However, it is not recommended for use in children undergoing computed tomography. In
newborns, especially premature infants, thyroid hormone levels, called TSH and T4, should be monitored. This monitoring is done 7-10 days and 1 month after Optiray administration.
In children under 3 years of age, including newborns, whose mothers received an iodine-containing contrast agent during pregnancy, thyroid hormone levels, called TSH and T4, should be monitored. These checks are performed 7-10 days and 1 month after Optiray administration.
Optiray and other medicines
Tell the doctor or radiologist about all medicines currently being taken or recently taken, as well as any planned medicines.
The following medicinesmay affect Optirayor Optiray may affect them:
- metformin:a medicine used to treat diabetes. The doctor will check kidney function before and after using Optiray. Depending on kidney function, the doctor may consider stopping metformin 48 hours before the examination and not restarting it for at least 48 hours after the examination, unless kidney function returns to normal.
- interleukins:medicines used to treat certain tumors
- certain blood pressure-increasing medicinesdue to vasoconstriction. To prevent the risk of neurological disorders, Optiray should never be used while taking these medicines.
- general anestheticsIncreased frequency of adverse reactions has been reported.
- diuretics:medicines that increase urine production and lower blood pressure. In the case of dehydration caused by diuretics, the use of iodine-containing contrast agents may increase the risk of acute kidney failure.
Optiray with food and drink
Consult a doctor. In patients with existing kidney disease, water intake should not be restricted, as it may further impair kidney function.
Pregnancy and breastfeeding
- PregnancyTell the doctor if you are pregnant or think you may be pregnant. The doctor will only give Optiray to a pregnant woman if it is absolutely necessary, as the medicine may harm the unborn child.
- Breastfeeding
Stop breastfeeding for one dayafter injection, as there is not enough data on safety. Consult a doctor or radiologist.
Driving and using machines
Driving or operating machinery is not recommended for 1 hour after
injection.
Additionally, symptoms such as dizziness, drowsiness, weakness, and vision disturbances have been observed. If such symptoms occur, do not attempt to perform any activities that require concentration and reaction.
Optiray contains sodium.
The medicine contains less than 1 mmol (23 mg) of sodium per dose, which means it is considered "sodium-free".
3. How to use Optiray
Examinations with Optiray will be performed only by a doctor or radiologist
who will also decide on the dose.
Optiray is injected into a blood vesseland distributed in the body through the bloodstream. Before use, the medicine is heated to body temperature, then injected once or several times during the radiological examination.
The dose depends on the type of examination and other factors, such as the patient's condition and age.
The smallest dose that allows for images of sufficient quality to be obtained is used.
Using more than the recommended dose of Optiray
Overdose is potentially dangerous and may affect breathing, heart, and circulation. Immediately inform the doctor or radiologist if the patient notices any such symptoms after receiving Optiray.
If you have any further questions about using this medicine, consult a doctor or radiologist.
4. Possible side effects
Like all medicines, Optiray can cause side effects, although not everybody gets them.
Side effects related to Optiray are generally dose-independent. In most cases, they are mild or moderate and very rarely severe or life-threatening.
Immediately consult a doctorif any of the following serious side effectsoccur:
- cardiac arrest or respiratory arrest
- vascular spasms or blood clots
- stroke, cyanosis, fainting
- memory loss
- speech disorders
- sudden movements
- temporary blindness
- acute kidney failure
- skin rash, redness, or blisters that can develop into life-threatening skin reactions, including widespread skin peeling (toxic epidermal necrolysis) or drug reaction with eosinophilia and systemic symptoms (DRESS)
- allergic reaction symptoms, such as anaphylactic shock, bronchospasm, laryngeal edema, throat tightness, difficulty breathing, coughing, sneezing, redness, and (or) facial swelling
Side effects may occur with the following frequency:
very common, occurring in more than 1 in 10 users
- feeling of heat
common, occurring in 1 to 10 in 100 users
- pain
- nausea
uncommon, occurring in 1 to 10 in 1,000 users
- hives
- skin redness, itching,
- dizziness
- headache
- taste disorders
- sensory disturbances, such as tingling, numbness
- vomiting
- sneezing
- high blood pressure
rare, occurring in 1 to 10 in 10,000 users
- fainting
- dizziness
- blurred vision
- pulsating heartbeat
- low blood pressure
- sudden facial flushing
- laryngeal spasms
- respiratory distress, including wheezing
- nasal congestion, runny nose
- cough, throat irritation
- dry mouth
- rash
- urinary urgency
- facial swelling, including eye swelling
- chills,
- uncontrolled shaking
- feeling cold
very rare, occurring in less than 1 in 10,000 users
- severe allergic reaction
- disorientation, anxiety, nervousness
- loss of consciousness, numbness
- paralysis
- drowsiness
- stupor
- speech disorders
- voice disorders
- decreased sensitivity to touch or sensation
- allergic conjunctivitis causing redness, tearing, and eye itching
- ringing or buzzing in the ears
- irregular heartbeat, slow pulse
- chest pain
- changes in heart activity measured by ECG
- disorders affecting blood flow to the brain
- high blood pressure
- phlebitis, vasodilation
- fluid accumulation in the lungs
- sore throat
- low oxygen levels in the blood
- abdominal pain
- salivary gland inflammation, tongue swelling
- difficulty swallowing, increased saliva production
- usually painful, severe swelling of deep skin layers, mainly on the face
- increased sweating
- muscle spasms
- acute kidney failure or impaired kidney function
- urinary incontinence, blood in urine, impaired urination
- edema due to excess fluid
- reactions at the injection site, including pain, redness, bleeding, or tissue degeneration
- general feeling of being unwell, fatigue, lethargy
unknown: frequency cannot be estimated from available data
- severe allergic reaction with anaphylactic shock
- transient hypothyroidism
- seizures
- temporary brain disorders (encephalopathy), which can cause disorientation, hallucinations, vision disturbances, blindness, seizures, loss of coordination, loss of movement on one side of the body, speech problems, and loss of consciousness.
- movement disorders
- memory loss
- temporary blindness
- cardiac arrest, life-threatening irregular heartbeat
- extra heartbeats
- coronary artery spasms, rapid heartbeat
- blue discoloration of the skin (cyanosis) due to low oxygen levels in the blood
- shock
- blood clots or spasms in blood vessels
- pallor
- respiratory arrest, asthma, bronchospasm
- reduced vocal ability using vocal organs
- diarrhea
- severe reaction involving skin, blood, and internal organs (drug reaction with eosinophilia and systemic symptoms, also known as DRESS or hypersensitivity syndrome)
- red, peeling, widespread rash with nodules under the skin and blisters, accompanied by fever at the beginning of treatment (acute generalized exanthematous pustulosis)
- red bumps (papules or nodules)
- life-threatening reaction with flu-like symptoms and painful rash/blisters on the skin, mouth, eyes, and genitals (Stevens-Johnson syndrome/toxic epidermal necrolysis)
- urinary incontinence, blood in urine, impaired urination
- hypothyroidism in newborns
- fever
Reporting side effects
If you experience any side effects, including any not listed in this leaflet, tell your doctor or pharmacist. Side effects can be reported directly to the Department of Adverse Reaction Monitoring of Medicinal Products, Medical Devices, and Biocidal Products, Al. Jerozolimskie 181C, 02-222 Warsaw, tel.: +48 22 49 21 301, fax: +48 22 49 21 309
Website: https://smz.ezdrowie.gov.pl
Side effects can also be reported to the marketing authorization holder. By reporting side effects, you can help provide more information on the safety of this medicine.
5. How to store Optiray
Keep the medicine out of sight and reach of children.
Do not use this medicine after the expiry date stated on the label. The expiry date refers to the last day of the month.
Store the containers in the outer packaging to protect from light.
Protect from X-rays.
Do not store above 30°C.
Optiray 300 can be stored for one month at 37°C in a contrast agent storage warmer with air circulation.
Do not use this medicine if you notice discoloration or solid particles.
6. Package contents and other information
What Optiray contains:
- The active substance is ioversol. One milliliter of Optiray 300 contains 636 mg of ioversol, which corresponds to 300 mg of organically bound iodine.
- Other ingredients are: sodium calcium edetate (stabilizer), trometamol, and trometamol hydrochloride (buffer) and water for injections. Sodium hydroxide and/or hydrochloric acid may be used to adjust the pH to 6.0-7.4.
What Optiray looks like and what the pack contains
Optiray 300 is packaged in:
- colorless vials of 10 or 20 ml, equipped with bromobutyl rubber closures and aluminum cap protectors. The box contains 10 vials.
- colorless bottles of 50, 75, 100, 150, or 200 ml, equipped with bromobutyl rubber closures and aluminum cap protectors. The box contains the following number of bottles: 50 ml - 10 or 25 bottles, 100 ml - 10 or 12 bottles, 75 ml, 150 ml, or 200 ml - 10 bottles.
- colorless bottles of 500 ml, equipped with bromobutyl rubber closures and aluminum cap protectors. The box contains 5, 6, or 10 bottles.
Optiray 300 is also supplied in pre-filled syringes and syringes with a pressure injector, made of polypropylene. The syringe tip and plunger are made of natural rubber.
Pre-filled syringes of 30 or 50 ml. The box contains 10 syringes. Pre-filled syringes of 50 ml. The box contains 20 syringes.
Syringes with a pressure injector of 50 ml or 100 ml. The box contains 10 or 20 syringes. 125 ml. The box contains 10 syringes.
Not all pack sizes and boxes may be marketed in all countries.
Marketing authorization holder and manufacturer:
- Marketing authorization holder's addressGuerbet BP 57400 95943 Roissy CDG Cedex France For more information on this medicine, contact the representative of the marketing authorization holder: Guerbet Poland Sp. z o.o., tel. (22) 6684110.
- Manufacturer
Guerbet
BP 57400
95943 Roissy CDG Cedex
France
Manufacturing site: 16-24 rue Jean Chaptal, 93600 Aulnay sous Bois, France
Date of last revision of the leaflet:
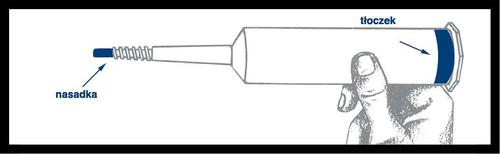
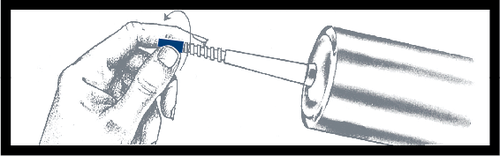
Instructions for use of pre-filled syringes
Pre-filled syringe
Assembly and inspection
Caution: The outer surface of the syringe is not sterile.
The contents of the syringe and the surface under the blue cap and the plunger ribs are
sterileand therefore require caution during assembly.
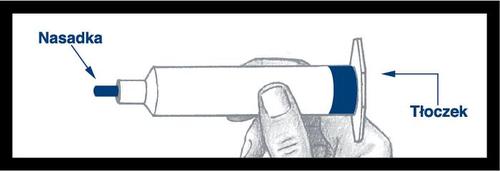
Remove the syringe from the base and
check for leaks around the blue capand on the outside of the plunger. Do not use the syringe if a leak is detected.
After screwing the plunger into the syringe,
it is essential to turn the plunger an additional ½ turn so that the blue plungermoves freely.
Before using the syringe, unscrew the blue capand discard it.
The surface under the cap is sterile; be careful not to touch it during further handling.
The syringe is now ready for needle or infusion tube attachment.
After use, discard the syringe and any unused portion of the medicine.
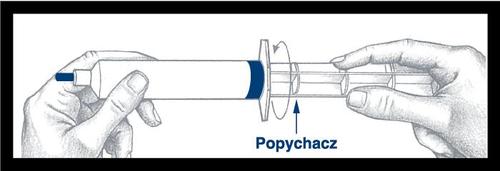
Instructions for use of syringes with a pressure injector
Pre-filled syringe
Assembly and inspection
Caution: The outer surface of the syringe is not sterile.
The contents of the syringe and the surface under the blue cap and the plunger ribs are
sterileand therefore require caution during assembly.
Remove the syringe from the base and
check for leaks around the blue capand on the outside of the plunger. Do not use the syringe if a leak is detected. Place the syringe in the pressure injector shield.
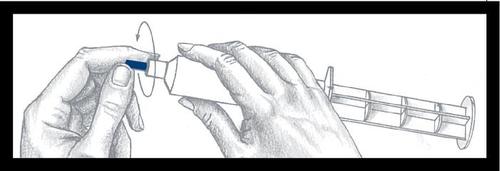
To remove the blue cap, press and turn it, then discard it after removal. The surface under the cap is sterile; be careful during further handling.
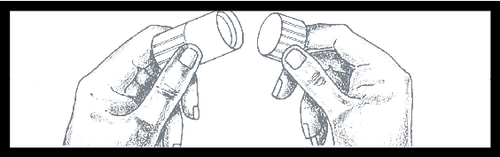
Then, remove the cap from the protective dust shield of the Luer connector by twisting it to break the visible seal. Discard the cap.
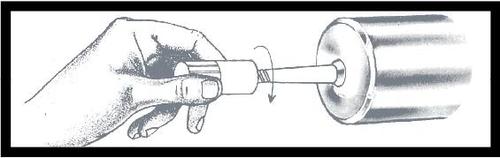
Screw the Luer connector onto the syringe, holding the protective dust shield and tightening it firmly. Remove and discard the protective dust shield immediately before attaching a sterile connector.
After use, discard the syringe and any unused portion of the medicine.
- Country of registration
- Active substance
- Prescription requiredYes
- ImporterGuerbet
- This information is for reference only and does not constitute medical advice. Always consult a licensed doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to Optirai 300Dosage form: Solution, 678 mg/ml (320 mg iodine/ml)Active substance: ioversolPrescription requiredDosage form: Solution, 741 mg/ml (350 mg iodine/ml)Active substance: ioversolPrescription requiredDosage form: Solution, 250 mg iodine/mlActive substance: iomeprolManufacturer: BIPSO GmbH Bracco Imaging S.p.A. Patheon Italia S.p.A.Prescription not required
Alternatives to Optirai 300 in other countries
The best alternatives with the same active ingredient and therapeutic effect.
Alternative to Optirai 300 in Іспанія
Online doctors for Optirai 300
Discuss dosage, side effects, interactions, contraindications, and prescription renewal for Optirai 300 – subject to medical assessment and local rules.














