
Iomeron 250
Ask a doctor about a prescription for Iomeron 250

How to use Iomeron 250
PATIENT INFORMATION LEAFLET: USER INFORMATION
Iomeron 250, solution for injection, 250 mg iodine/ml
Iomeron 300, solution for injection, 300 mg iodine/ml
Iomeron 350, solution for injection, 350 mg iodine/ml
Iomeron 400, solution for injection, 400 mg iodine/ml
Jomeprol (Iomeprolum)
Read the leaflet carefully before using the medicine.
- Keep this leaflet, you may need to read it again.
- In case of further doubts, consult a doctor or pharmacist.
- This medicine has been prescribed specifically for you. Do not pass it on to others. It may harm them, even if their symptoms are the same as yours.
- If you experience any side effects, including any not listed in this leaflet, tell your doctor or nurse. See section 4.
Table of contents of the leaflet:
- 1. What Iomeron is and what it is used for
- 2. Important information before using Iomeron
- 3. How to use Iomeron
- 4. Possible side effects
- 5. How to store Iomeron
- 6. Contents of the pack and other information
1. What Iomeron is and what it is used for
Medicinal product intended exclusively for diagnostic purposes.
Iomeronis a sterile aqueous solution of iomeprol in concentrations ranging from 200 to 400 mg iodine/ml.
The active substance of the medicine is iomeprol - a triiodinated, non-ionic, water-soluble contrast agent used in radiological diagnosis of various body regions.
After intravenous administration of Iomeron, most of it is excreted in the urine within the first 24 hours, and small amounts are excreted between 24 and 38 hours after administration.
2. Important information before using Iomeron
When not to use Iomeron:
Do not administer Iomeron:
- if the patient is allergic to the active substance or any of the other ingredients of this medicine (listed in section 6),
- if there is a repeat myelography, due to the possibility of overdose of the contrast agent.
Warnings and precautions
Before starting treatment with Iomeron, discuss it with your doctor or nurse.
- if the patient is an allergic person, has asthma and especially if they are taking blood pressure regulating medications (beta-adrenolytics).
- if the patient has thyroid function disorders.
- if the patient has ever experienced severe rash or skin peeling after taking an iodine-containing contrast agent, blistering and (or) mouth ulcers after receiving an iodine-containing contrast agent.
Pregnancy and breastfeeding
Since, if possible, exposure to radiation during pregnancy should be avoided, the benefit of performing an X-ray examination with or without a contrast agent should be carefully considered in the context of possible risk.
If a pregnant patient has received Iomeron during pregnancy, it is recommended to monitor the child's thyroid function after birth.
Similarly, X-ray examination with contrast agent should be avoided in breastfeeding women. Contrast agents are excreted in small amounts in the milk of breastfeeding women. Based on current experience, the occurrence of side effects in the breastfed infant is unlikely. Breastfeeding can be continued after the examination with Iomeron.
Elderly
Due to the deterioration of physiological functions in the elderly, there is a particular risk of side effects, especially when large doses of contrast agents are used.
Children
After administration of Iomeronin both children and adults, thyroid function disorders may occur. Infants may also be exposed through their mother during pregnancy. It may be necessary for the doctor to perform thyroid function tests before and (or) after administration of Iomeron.
Hypersensitivity to iodine-containing contrast agents
Diagnosed hypersensitivity or previous reaction to iodine-containing contrast agents also increases the risk of recurrence of a severe reaction to non-ionic agents. In these patients, it is recommended to administer glucocorticoids and antihistamines to prevent another reaction.
Predisposition to allergic reactions
Side effects of iodine-containing contrast agents occur more frequently in patients with a history of allergies: hay fever, urticaria, and food allergies.
Asthma
Patients using beta-adrenolytics, especially those with asthma, may have a lower threshold for bronchospasm and may respond less to beta-agonist and adrenaline treatment, which may require the use of higher doses of adrenaline.
Thyroid function and thyroid function tests
Small amounts of free inorganic iodine that may be present in contrast agents can affect thyroid function. This effect is more pronounced in patients with latent or overt hyperthyroidism or goiter. There have been reports of hyperthyroidism or even thyroid crisis after administration of iodine-containing contrast agents.
Renal impairment
Previous renal impairment may predispose to the occurrence of acute renal dysfunction after administration of contrast agents. Preventive measures include:
- identification of patients at high risk;
- ensuring adequate hydration before administration of contrast agents, it is recommended to maintain intravenous fluid infusion before and during the procedure until the contrast agent is fully excreted by the kidneys;
- avoiding, whenever possible, the use of nephrotoxic drugs or performing extensive procedures or procedures such as renal angioplasty until the contrast agent is fully excreted;
- delaying the next contrast agent examination until renal function returns to pre-examination levels. In dialyzed patients, contrast agents such as iomeprol can be administered before dialysis.
Diabetes
Diabetic nephropathy is one of the factors that predispose to the development of renal function disorders after administration of contrast agents. Biguanide derivatives (e.g., metformin) may accelerate the development of lactic acidosis.
Pheochromocytoma
In order to reduce the risk of hypertensive crisis, it is recommended to use alpha-adrenergic blockers in these patients.
Myasthenia gravis
The administration of iodine-containing contrast agents may exacerbate the symptoms of the disease.
Severe cardiovascular diseases
The risk of severe reactions in patients with serious heart diseases, especially in the case of heart failure and coronary artery disease, is increased.
Intravascular injection of a contrast agent may accelerate the onset of pulmonary edema in patients with overt or initial heart failure. Administration of a contrast agent in the case of pulmonary hypertension and valvular defects may lead to significant hemodynamic changes.
CNS disorders
Particular attention should be paid to the intravascular administration of contrast agents in patients with acute cerebral ischemia, acute intracranial hemorrhage, conditions with blood-brain barrier disruption, cerebral edema, and acute demyelination.
The presence of intracranial tumors or metastases and a history of epilepsy may increase the likelihood of seizures.
Neurological symptoms caused by coexisting degenerative, inflammatory, or neoplastic changes may worsen after administration of a contrast agent.
Intravascular injection of a contrast agent may cause vasospasm and resulting ischemia symptoms.
During imaging or shortly after, the patient may experience a transient cerebral disturbance, called encephalopathy. If the patient experiences any symptoms related to this disorder, as described in section 4, they should immediately inform their doctor.
Alcoholism
It has been proven that both acute and chronic alcoholism leads to increased permeability of the blood-brain barrier, facilitating the penetration of iodine-containing contrast agents into brain tissue, potentially leading to CNS disorders. Due to the possibility of lowering the seizure threshold, caution should be exercised in individuals addicted to alcohol.
Drug dependence, drug addiction
Caution should be exercised in individuals addicted to drugs or narcotics, due to the possibility of lowering the seizure threshold.
States of excitement
States of severe anxiety, excitement, and pain can cause or exacerbate side effects caused by the administration of contrast agents.
Extravasation
Care should be taken when injecting a contrast agent to avoid extravasation.
Particular caution should be exercised when using Iomeron
Severe skin reactions, including Stevens-Johnson syndrome (SJS), toxic epidermal necrolysis (TEN), acute generalized exanthematous pustulosis (AGEP), and drug reaction with eosinophilia and systemic symptoms (DRESS), have been reported in association with the use of Iomeron. If any symptoms of severe skin reactions occur, as described in section 4, immediate medical attention should be sought.
Iomeron and other medicines
The doctor will consider discontinuing treatment with medications that lower the seizure threshold. Treatment will be resumed 24 hours after the procedure.
Antiepileptic therapy should not be discontinued, and medications should be administered in optimal doses.
Biguanide derivatives (e.g., metformin) may accelerate the development of lactic acidosis. As a precaution, it is recommended to discontinue biguanide derivatives during or 48 hours before the examination with contrast agents and resume them only after checking renal function and confirming that it has returned to normal.
An increased risk of side effects, especially delayed ones (rash, erythema, fever, flu-like symptoms), occurs in patients treated with interleukin-2 (IL-2) and interferon.
Thyroid function tests
The uptake of radioactive isotopes in diagnostic tests of thyroid function disorders is reduced for up to 16 days after administration of iodine-containing contrast agents.
Thyroid test results independent of iodine levels, i.e., T3, T4 levels, are not changed. All tests whose results depend on iodine levels should be performed before contrast agent examination. The above observations do not depend on clinical symptoms.
Laboratory tests
High concentrations of contrast agents in serum and urine can affect the results of laboratory tests for bilirubin, protein, or inorganic substances (e.g., iron, copper, calcium, phosphates).
Driving and operating machinery
The effect on the ability to drive and operate machinery is not known.
3. How to use Iomeron
Details on dosing can be found at the end of the leaflet in the section Information for healthcare professionals or healthcare workers. Diagnostic tests using contrast agents should be performed by appropriately trained medical personnel.
Overdose
Overdose can lead to life-threatening side effects, mainly due to the effect on the respiratory and cardiovascular systems. Treatment of overdose focuses on maintaining vital functions and symptomatic therapy. Dialysis or hemodialysis can also be used.
In case of overdose after intravascular administration, careful observation is necessary to check for CNS disorders. Symptoms include: ascending enhancement of deep reflexes, tonic-clonic seizures, generalized seizures, increased body temperature, stupor, respiratory depression.
4. Possible side effects
Like any contrast agent, Iomeroncan cause side effects, although they do not occur in everyone.
Side effects are usually mild to moderate and transient. However, severe and life-threatening reactions leading to death have also been reported. Reactions usually occur within a few minutes of administration, but may occur much later.
Anaphylaxis (anaphylactoid/anaphylactic reactions) manifests in different ways, very rarely in one patient showing all possible symptoms. Usually within 1 to 15 minutes (rarely longer than 2 hours) the patient complains of malaise, excitement, hot flashes, feeling of heat, increased sweating, dizziness, increased lacrimation, nasal congestion, palpitations, paresthesia, itching, feeling of pulsation in the head, sore throat, and feeling of constriction in the throat, difficulty swallowing, coughing, sneezing, urticaria, erythema, mild local edema, angioedema, dyspnea caused by tongue and laryngeal edema and (or) its spasm, which manifests as wheezing and bronchospasm.
There have also been reports of nausea, vomiting, abdominal pain, and diarrhea.
These reactions, which occur regardless of dose and route of administration, may be the first symptoms of circulatory failure.
Administration of the contrast agent should be stopped immediately and, if necessary, appropriate treatment should be initiated intravenously.
Severe reactions from the cardiovascular system, such as vasodilation with a drop in blood pressure, tachycardia, dyspnea, excitement, cyanosis, loss of consciousness progressing to cardiac arrest and respiratory arrest, can be fatal. These reactions may occur quickly and require full and intensive cardiopulmonary resuscitation (restoration of cardiovascular and respiratory function).
Primary circulatory collapse may occur as the only and (or) initial reaction without additional respiratory symptoms or other symptoms mentioned earlier.
Side effects after intravascular administration
Adults
Frequent (occurring in 1 to 10 out of 100 patients):
feeling of heat
Uncommon (occurring in 1 to 10 out of 1,000 patients):
dizziness, headache, hypertension, dyspnea, vomiting, nausea, erythema, urticaria, itching, chest pain, pain and feeling of heat at the injection site
Rare (occurring in 1 to 10 out of 10,000 patients):
pre-syncopal states, bradycardia (rare rhythm), tachycardia (significant acceleration of heart rate), extra systoles, hypotension, rash, back pain, asthenia (decreased or absent natural physical and nervous resistance), chills, fever, increased creatinine levels in serum.
Frequency not known (frequency cannot be estimated from available data):
you should immediately consult a doctor if the patient experiences severe skin reactions, such as:
- blisters, skin peeling, mouth ulcers, genital and eye ulcers. These serious skin changes may be preceded by fever and flu-like symptoms (Stevens-Johnson syndrome, toxic epidermal necrolysis).
- red, peeling rash with nodules under the skin and blisters, accompanied by fever. Symptoms usually appear at the beginning of treatment (acute generalized exanthematous pustulosis).
- widespread rash, high fever, and swollen lymph nodes (DRESS syndrome or drug hypersensitivity syndrome).
Other side effects with unknown frequency:
Thrombocytopenia, hemolytic anemia (abnormal breakdown of red blood cells, which can cause fatigue, rapid heart rate, and shortness of breath), anaphylactic reaction, anxiety, confusion, coma, transient ischemic attacks, paralysis, fainting, seizures, loss of consciousness, dysarthria (speech disorders), paresthesia, amnesia, somnolence, taste disorders, transient blindness, vision disorders, conjunctivitis, increased lacrimation, photopsia (sensation of flashes or colors), cardiac arrest, myocardial infarction, heart failure, angina pectoris, atrial fibrillation or atrial flutter, atrioventricular block, cyanosis, respiratory arrest, acute respiratory distress syndrome (ARDS), pulmonary edema, laryngeal edema, pharyngeal edema, bronchospasm, asthma, cough, throat discomfort, laryngeal discomfort, rhinorrhea, dysphonia (voice disorders), diarrhea, abdominal pain, excessive salivation, difficulty swallowing, salivary gland enlargement, angioedema, sweating, acute renal failure, reaction at the injection site*, malaise, ST segment elevation, ECG abnormalities, hyperthyroidism, cyanosis of the skin and mucous membranes, blood clots, vasospasm and consequent ischemia, erythema multiforme (development of round skin blisters, whose center is often lighter).
Brain disorder (encephalopathy) with symptoms including headache, vision disorders, loss of vision, confusion, seizures, loss of coordination, loss of movement of one side of the body, speech difficulties, and loss of consciousness.
* Reactions at the injection site include pain and swelling at the injection site. In most cases, they are caused by extravasation of the contrast agent. These reactions are usually transient and do not cause permanent consequences. There have been reports of extravasation associated with inflammation, skin necrosis, and even the development of compartment syndrome.
Thrombosis and embolism of coronary arteries have been reported as complications of coronary angiography.
During intravascular administration of a contrast agent, vasospasm and consequent ischemia have been observed, especially after angiography of blood vessels and the brain, often related to the technique of the examination and presumably caused by the action of the catheter tip or excessive pressure in the catheter.
Children
Experience with the use of iomeprol in children is limited. The safety profile of iomeprol is similar in children and adults. In children under 3 years of age, transient hypothyroidism may occur.
Side effects after intravascular administration
Adults
The most commonly reported side effects after intravascular administration of iomeprol are: headache, dizziness, nausea, vomiting, and back pain. These side effects are mild to moderate and transient. In rare cases, headache may last for several days. Most side effects occur within 3-6 hours after administration, depending on the rate of distribution of the contrast agent from the injection site to the blood vessels. Most reactions occur within 24 hours of administration.
Very common (occurring in more than 1 in 10 patients):
headache.
Common (occurring in 1 to 10 out of 100 patients):
dizziness, hypertension, nausea, vomiting, back pain, pain in the limbs, reaction at the injection site*.
Uncommon (occurring in 1 to 10 out of 1,000 patients):
loss of consciousness, paralysis, paresthesia, numbness, hypotension, sudden flushing, sweating, itching, stiffness of muscles and joints, neck pain, feeling of heat, fever.
Frequency not known:
anaphylactic reaction, seizures, rash.
* Reactions at the injection site include pain and swelling at the injection site.
Children
The safety profile of this medicine in children is similar to that in adults.
No side effects have been reported after intravascular administration of iomeprol in children.
Side effects after administration into body cavities
After administration of iodine-containing contrast agents into body cavities, the contrast agents are slowly absorbed from the injection site into the bloodstream and then excreted by the kidneys.
An increase in amylase levels often occurs after endoscopic retrograde cholangiopancreatography (ERCP). Rare cases of pancreatitis have been reported.
Reactions reported during arthrography and fistulography are related to irritation symptoms, which occur in previously inflamed tissues.
Hypersensitivity reactions are rare, mild, or in the form of dermatitis. However, severe anaphylactic reactions cannot be ruled out.
As with other iodine-containing contrast agents, after hysterosalpingography (a radiological examination aimed at visualizing the uterus and fallopian tubes), pelvic pain and malaise may occur.
Reporting side effects
If you experience any side effects, including any not listed in this leaflet, tell your doctor or pharmacist.
Side effects can be reported directly to the Department of Monitoring of Adverse Reactions to Medicinal Products of the Office for Registration of Medicinal Products, Medical Devices, and Biocidal Products, Al. Jerozolimskie 181C, 02-222 Warsaw, phone:
- (22) 49 21 301, fax: (22) 49 21 309, website: https://smz.ezdrowie.gov.pl Side effects can also be reported to the marketing authorization holder. By reporting side effects, you can help provide more information on the safety of this medicine.
5. How to store Iomeron
Store at a temperature below 30°C.
Store in the outer packaging to protect from light.
Although iomeprol is slightly sensitive to X-rays, it is recommended to store the medicine out of the reach of ionizing radiation.
Vials containing the contrast agent solution are not intended for multiple use.
The contrast agent should not be drawn into a syringe until immediately before use. Unused solutions and residues in syringes should be discarded after a single examination.
Do not use Iomeronif signs of spoilage are visible.
Do not use after the expiry date stated on the packaging.
Before administration, check for visible mechanical contamination and changes in the color of the medicine, if the packaging allows.
6. Contents of the pack and other information
What Iomeron contains
The active substance is iomeprol.
Iomeronsolution contains (per 100 ml) the following excipients:
trometamol
100 mg
hydrochloric acid (d = 1.18)
24 mg
water for injections q.s.
100 ml
What Iomeron looks like and what the pack contains
Iomeronis packaged in vials/bottles of colorless glass, closed with a rubber stopper, metal cap, and plug, placed in cardboard boxes.
Available packs:
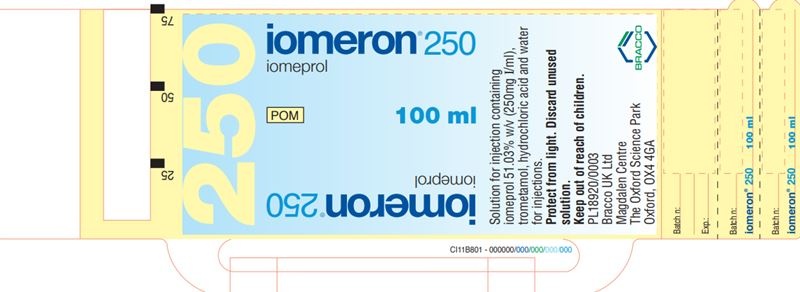
Iomeron 250
Bottles of 50 ml, 100 ml, 150 ml, or 200 ml
Iomeron 300
Vials of 20 ml
Bottles of 50 ml, 100 ml, 150 ml, 200 ml, or 500 ml
Iomeron 350
Vials of 20 ml
Bottles of 50 ml, 100 ml, 150 ml, 200 ml, 250 ml, or 500 ml
Iomeron 400
Bottles of 50 ml, 100 ml, 150 ml, 200 ml, 250 ml, or 500 ml
Marketing authorization holder and manufacturer
Marketing authorization holder:
Bracco Imaging Deutschland GmbH
Max-Stromeyer-Strasse 116
D-78467 Konstanz
Germany
Manufacturer:
Patheon Italia S.p.A
2nd Trav. SX Via Morolense 5
03013 Ferentino
Italy
BIPSO GmbH
Robert-Gerwig-Strasse 4
78224 Singen
Germany
Bracco Imaging S.p.A.
Bioindustry Park
via Ribes, 5
10010 Colleretto Giacosa (TO)
Italy
Representative of the marketing authorization holder:
Bracco Imaging Polska Sp. z o.o.
ul. Domaniewska 39 A
02-672 Warsaw
phone: + 48 22 208 24 20
Date of last revision of the leaflet: 09/2023
-------------------------------------------------------------------------------------------------------------------------
INFORMATION FOR HEALTHCARE PROFESSIONALS OR HEALTHCARE WORKERS
1 ml of Iomeroncontains:
Indications
Iomeron 250Intravenous urography, peripheral phlebography, computed tomography (CT) (brain and body), intravenous digital subtraction angiography (DSA), cavernosography, conventional angiography, intra-arterial digital subtraction angiography (DSA), cardiac angiography (in adults and children), conventional selective coronary arteriography, interventional coronary arteriography, endoscopic retrograde cholangiopancreatography (ERCP), arthrography, hysterosalpingography, fistulography, discography, galactography, cholangiography, dacryocystography, sialography, retrograde urethrography, retrograde pyeloureterography, myelography.
Iomeron 300Intravenous urography (in adults and children), peripheral phlebography, computed tomography (CT) (brain and body), intra-arterial digital subtraction angiography (DSA), conventional angiography, intra-arterial digital subtraction angiography (DSA), cardiac angiography (in adults and children), conventional selective coronary arteriography, interventional coronary arteriography, endoscopic retrograde cholangiopancreatography (ERCP), arthrography, hysterosalpingography, fistulography, galactography, cholangiography, dacryocystography, sialography, urethrography, pyeloureterography, myelography.
Iomeron 350Intravenous urography (in adults and children), computed tomography (CT) (body), intravenous digital subtraction angiography (DSA), conventional angiography, intra-arterial digital subtraction angiography (DSA), cardiac angiography (in adults and children), conventional selective coronary arteriography, interventional coronary arteriography, arthrography, hysterosalpingography, fistulography, galactography, cholangiography, dacryocystography, sialography.
Iomeron 400Intravenous urography (in adults, including those with impaired renal function or diabetes), computed tomography (CT) (body), conventional angiography, intra-arterial digital subtraction angiography (DSA), cardiac angiography (in adults and children), conventional selective coronary arteriography, interventional coronary arteriography, fistulography, galactography, dacryocystography, sialography.
Dosage
| Iomeron | Iomeprol (mg) | which corresponds to the amount of iodine (mg) |
| Iomeron 250 | 510.3 | 250 |
| Iomeron 300 | 612.4 | 300 |
| Iomeron 350 | 714.4 | 350 |
| Iomeron 400 | 816.5 | 400 |
| Indication | Product (mg iodine/ml) | Recommended dosage |
| Intravenous urography | 250, 300, 350, 400 | Adults: 50-150 ml Newborns: 3-4.8 ml/kg body weight Infants: 2.5-4 ml/kg body weight Children: 1-2.5 ml/kg body weight |
| Peripheral phlebography | 250, 300 | Adults: 10-100 ml, repeat if necessary (10-50 ml for upper limbs; 50-100 ml for lower limbs) |
| CT of the brain | 250, 300 | Adults: 50-200 ml Children: |
| CT of the body | 250, 300, 350, 400 | Adults: 100-200 ml Children: |
| Cavernosography | 300 | Adults: up to 100 ml |
| Intravenous DSA | 250, 300, 350, 400 | Adults: 100-250 ml Children: |
| Conventional angiography Arteriography of upper limbs | 300, 350 | Adults: |
| Arteriography of pelvis and lower limbs | 300, 350, 400 | Adults: |
| Abdominal arteriography | 300, 350, 400 | Adults: |
| Arteriography of descending aorta | 300, 350 | Adults: |
| Pulmonary angiography | 300, 350, 400 | Adults: up to 170 ml |
| Cerebral angiography | 300, 350 | Adults: up to 100 ml |
| Arteriography in pediatrics | 300 | Children: up to 130 ml |
| Interventional intra-arterial DSA | 300, 350, 400 | Adults: Children: |
| Cerebral | 300, 350 | Adults: 30-60 ml - total dose 5-10 ml - selective injection Children: |
| Chest | 300 | Adults: 20-25 ml (aorta) if necessary repeat, 20 ml (pulmonary arteries) |
| Aortic arch | 300, 350 | Adults: |
| Abdomen | 250, 300 | Adults: |
| Aortography | 300, 350 | Adults: |
| Translumbar aortography | 300 | Adults: |
| Peripheral arteriography | 250, 300 | Adults: 5-10 ml for selective injection, up to 250 ml Children: |
| Interventional procedures | 300 | Adults: 10-30 ml for selective injection, up to 250 ml Children: |
| Cardiac angiography | 300, 350, 400 | Adults: Children: 3-5 ml/kg body weight |
| Conventional selective coronary arteriography | 300, 350, 400 | Adults: 4-10 ml per artery, if necessary repeat |
| Interventional coronary arteriography | 300, 350, 400 | Adults: 4-10 ml per artery, if necessary repeat |
| ERCP | 300 | Adults: up to 100 ml |
| Arthrography | 300, 350 | Adults: up to 10 ml per injection |
| Hysterosalpingography | 300, 350 | Adults: up to 35 ml |
| Fistulography | 300, 350, 400 | Adults: up to 100 ml |
| Discography | 300 | Adults: up to 4 ml |
| Galactography | 300, 350, 400 | Adults: 0.15-1.2 ml per injection |
| Dacryocystography | 300, 350, 400 | Adults: 2.5-8 ml per injection |
| Sialography | 300, 350, 400 | Adults: 1-3 ml per injection |
| Cholangiography | 300, 350 | Adults: up to 60 ml |
| Retrograde urethrography | 300 | Adults: 20-100 ml |
| Retrograde pyeloureterography | 300 | Adults: 10-20 ml per injection |
| Myelography | 250, 300 | Adults: 10-18 ml 8-15 ml |
The recommended doses for adults were calculated for an average body weight of 70 kg. Each time before administration, the dose should be adjusted to the patient's current body weight and other relevant factors (e.g., clinical condition).
The recommended doses for newborns, infants, and children are given per single injection/kg body weight and are as follows:
= in accordance with body weight and age
= do not exceed 250 ml. The volume of a single injection depends on the vascularized area to be examined
= do not exceed 350 ml
= do not exceed 4500 mg of iodine and a concentration above 300 mg I/ml when administered intravascularly
= newborns 0-27 days old
= infants from 28 days to 12 months old
= includes children and adolescents (1-17 years old)
Instructions for use
Contrast agents administered intravascularly and intravascularly should have body temperature during injection.
Before administration, check for visible mechanical contamination and changes in the color of the medicine, if the packaging allows.
Never mix other medicines with contrast agents.
The contrast agent is drawn from the packaging under sterile conditions and with a sterile syringe.
Sterile conditions and technique should be maintained when performing intravascular injection, administration via catheters, and guidewires.
Once opened, packaging must be used immediately. The rubber stopper should never be punctured more than once.
It is recommended to use suitable cannulas for piercing the stopper and drawing the contrast agent from the packaging.
Contrast agents in packaging intended for multiple use and with a capacity of 500 ml should be used with appropriate injection devices. After the examination, all parts intended for single use should be discarded. The instructions provided by the manufacturer of the injection device should be followed.
Iomeprol, like other contrast agents, may react with metal surfaces containing copper, e.g., brass, so it is recommended to avoid using equipment made of this type of material.
Contraindications to intravascular administration:
Repeat myelography is contraindicated due to the possibility of overdose of the contrast agent.
Special warnings and precautions for use
Diagnostic tests using contrast agents should be performed by appropriately trained medical personnel (especially in the treatment of anaphylactic shock and maintenance of vital functions).
General precautions for use in relation to the patient
Hydration
Patients must be well-hydrated, and any significant water-electrolyte imbalance should be corrected before and after administration of the contrast agent. Patients with severe renal, hepatic, or cardiac functional impairment, multiple myeloma, or other paraproteinemia, sickle cell anemia, diabetes, polyuria, oliguria, hyperuricemia, infants, elderly patients, and patients with severe systemic disease should not be exposed to dehydration. Caution should be exercised in patients who are hydrated and whose condition may worsen with the administration of excessive fluid, including those with congestive heart failure.
Dietary recommendations
Unless the doctor advises otherwise, a normal diet can be followed on the day of the examination. Adequate fluid intake should be ensured before and after intravascular administration.
Allergy test
In patients with suspected or known hypersensitivity to contrast agents, an allergy test is not recommended, as severe or fatal reactions to contrast agents are unpredictable based on the results of allergy tests.
Hypersensitivity
In patients with a tendency to allergies, hypersensitivity reactions to iodine-containing contrast agents, and (or) asthma, it is recommended to administer antihistamines and (or) glucocorticoids to reduce the risk of pseudo-anaphylactic reactions.
Anxiety
Severe anxiety, excitement, and pain can cause or exacerbate side effects associated with the administration of contrast agents.
Newborns, infants, children
Infants (<1 year old), especially newborns, are particularly susceptible to electrolyte imbalance and hemodynamic changes. attention should be paid planned dosing, details of the procedure, patient's condition.< p>
General precautions for use in relation to the procedure
Intravascular administration
As with other contrast agents, Iomeronshould be administered with particular caution to patients with increased intracranial pressure or suspected tumor, abscess, or hemorrhage in the brain. In patients with a history of seizures, antiepileptic drugs should be administered before and after myelographic examination.
Catheterization
Non-ionic contrast agents show weaker anticoagulant activity in vitro than ionic agents. Medical personnel performing catheterization should be informed about this. The angiographic procedure and catheter flushing should be performed very carefully to minimize the risk of thrombosis and embolism associated with the procedure. To maintain catheter patency, it can be flushed with a physiological saline solution (if necessary, with the addition of heparin).
Patient monitoring
Intravascular administration - contrast agents should, if possible, be administered to a patient in a supine position. The patient should be monitored for at least 30 minutes after administration of the contrast agent.
Intravascular administration - after completion of direct administration to the cervical or lumbar region, the head of the bed should be elevated (about 45°) for about 2 minutes to allow the contrast agent to fill the lower parts of the spinal canal. For the first hours after the examination, the patient should avoid excessive, sudden movements and remain under special observation. They should then lie on their back with their head elevated.
Administration into the basal cisterns or ventricles - direct administration is not recommended when using conventional radiography without computer enhancement.
The label torn from the vial or bottle should be attached to the patient's chart to allow proper recording of the administered medicinal product. The dose should also be recorded.
- Country of registration
- Active substance
- Prescription requiredNo
- Manufacturer
- ImporterBIPSO GmbH Bracco Imaging S.p.A. Patheon Italia S.p.A.
- This information is for reference only and does not constitute medical advice. Always consult a licensed doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to Iomeron 250Dosage form: Solution, 300 mg iodine/mlActive substance: iomeprolManufacturer: BIPSO GmbH Bracco Imaging S.p.A. Patheon Italia S.p.A.Prescription not requiredDosage form: Solution, 350 mg iodine/mlActive substance: iomeprolManufacturer: BIPSO GmbH Bracco Imaging S.p.A. Patheon Italia S.p.A.Prescription not requiredDosage form: Solution, 400 mg iodine/mlActive substance: iomeprolManufacturer: BIPSO GmbH Bracco Imaging S.p.A. Patheon Italia S.p.A.Prescription not required
Alternatives to Iomeron 250 in other countries
The best alternatives with the same active ingredient and therapeutic effect.
Alternative to Iomeron 250 in Spain
Online doctors for Iomeron 250
Discuss dosage, side effects, interactions, contraindications, and prescription renewal for Iomeron 250 – subject to medical assessment and local rules.














