
Numeta G16%e
Ask a doctor about a prescription for Numeta G16%e

How to use Numeta G16%e
Leaflet accompanying the packaging: information for the user
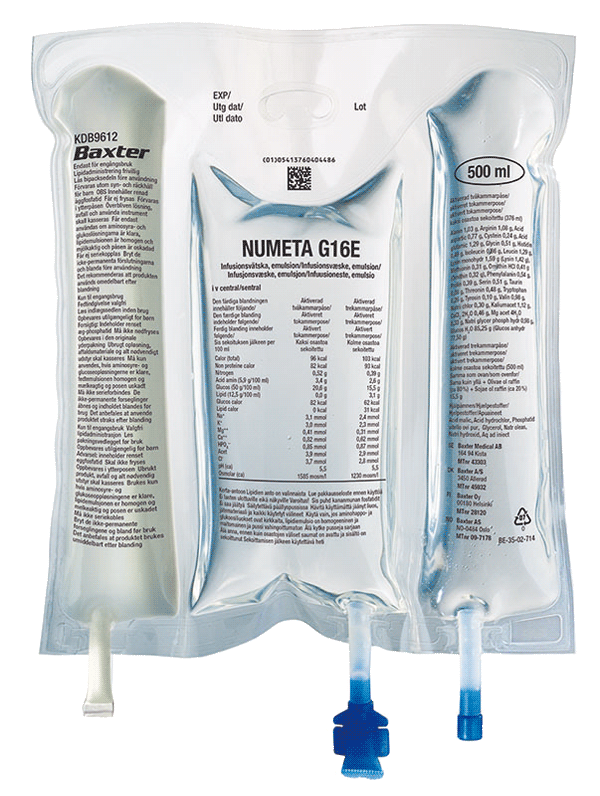
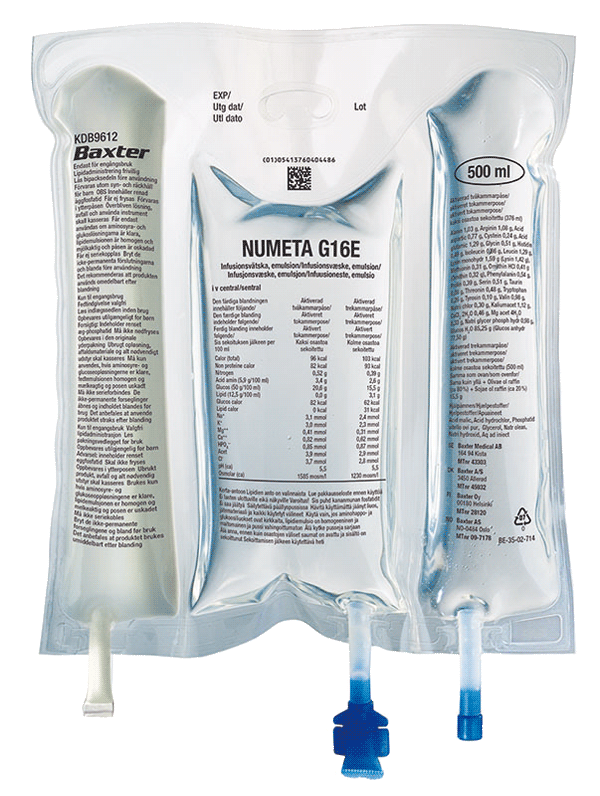
NUMETA G16%E, infusion emulsion
Read the leaflet carefully before using the medicine, as it contains
important information for the patient.
- Keep this leaflet, you may need to read it again.
- In case of any doubts, consult your child's doctor, pharmacist, or nurse.
- If your child experiences any side effects, including any not listed in this leaflet, tell your doctor or nurse. See section 4.
Table of contents of the leaflet
- 1. What is NUMETA G16%E and what is it used for
- 2. Important information before giving NUMETA G16%E to your child
- 3. How to use NUMETA G16%E
- 4. Possible side effects
- 5. How to store NUMETA G16%E
- 6. Contents of the packaging and other information
1. What is NUMETA G16%E and what is it used for
NUMETA G16%E is a specialized nutrition emulsion for infants born at term and children up to 2 years of age. It is administered through a tube inserted into the child's vein when the child cannot take all the necessary nutrients by mouth.
NUMETA G16%E comes in a triple-chamber bag, where each chamber contains: glucose solution 50%; pediatric amino acid solution with electrolytes 5.9%; and fat emulsion 12.5%. Depending on the child's needs, two or three of these solutions are mixed in the bag before administration to the child.
NUMETA G16%E should only be used under medical supervision.
2. Important information before giving NUMETA G16%E to your child
When should NUMETA G16%E not be given to your child:
In the case of 2 solutions mixed in the bag ("2 in 1"):
In the case of 3 solutions mixed in the bag ("3 in 1"):
In all cases, the doctor will decide whether to administer the medicine, taking into account the child's age, weight, and clinical condition. The doctor will also consider the results of all tests performed.
Warnings and precautions
Before starting NUMETA G16%E, discuss it with your doctor or nurse.
In the case of newborns and children under 2 years of age, the solution (in bags and administration sets) should be protected from light until the end of administration. Exposure of NUMETA G16%E to ambient light, especially after mixing with trace elements and/or vitamins, causes the formation of peroxides and other degradation products, which can be reduced by protecting it from light.
Allergic reactions:
If any signs or symptoms of an allergic reaction occur (such as fever, sweating, chills, headache, skin rash, or difficulty breathing), the infusion should be stopped immediately.
This medicine contains soybean oil, which can rarely cause hypersensitivity reactions. In some people allergic to peanut proteins, soy protein allergy has also been observed. NUMETA G16%E contains glucose produced from cornstarch. Therefore, NUMETA G16%E should be used with caution in patients with known allergy to corn or corn-containing products.
Risk of precipitate formation with ceftriaxone (antibiotic):
The antibiotic ceftriaxone should not be mixed or administered simultaneously with any calcium-containing solutions (including NUMETA G16%E) by intravenous infusion.
However, the doctor may administer calcium and ceftriaxone sequentially, one after the other, if the infusion lines are inserted into different sites or are changed or thoroughly flushed with physiological saline solution between infusions to avoid precipitate formation.
Formation of small particles in blood vessels in the lungs:
Breathing difficulties may also be a sign that small particles have formed, blocking blood vessels in the lungs (pulmonary vascular precipitates). If your child experiences any breathing difficulties, tell your doctor or nurse. They will decide on the appropriate action.
Infection and sepsis:
The doctor will carefully monitor your child for signs of infection.
Aseptic procedures (procedures that protect against microorganisms) when inserting and maintaining the catheter, as well as when preparing the nutritional mixture, can reduce the risk of infection.
Sometimes, if a tube is inserted into a vein (central venous catheter), your child may develop an infection and sepsis (presence of bacteria in the blood). Some medications and diseases can increase the risk of infection or sepsis.
Fat overload syndrome:
Similar medicines have been reported to cause fat overload syndrome.
Reduced or limited ability to eliminate fats contained in NUMETA G16%E or overdose can lead to fat overload syndrome (see sections 3 and 4).
Changes in blood chemical composition:
The doctor will check and monitor your child's fluid status, blood chemical composition, and the content of other substances, as nutrition of severely malnourished individuals can sometimes cause changes in blood chemical composition.
Additional fluid may also appear in tissues and swelling. It is recommended to start parenteral nutrition slowly and cautiously.
Elevated magnesium levels in the blood:
The amount of magnesium in NUMETA G16%E may cause elevated magnesium levels in the blood.
In such cases, the following symptoms may occur: weakness, slowed reflexes, nausea, vomiting, low calcium levels in the blood, breathing difficulties, low blood pressure, and irregular heartbeat.
Symptoms may be difficult to detect, so the doctor may monitor your child's magnesium levels, especially in children with risk factors for elevated magnesium levels in the blood, including kidney function disorders.
If magnesium levels are elevated, the infusion will be stopped or the rate of administration of the medicine will be reduced.
Monitoring and adjustment:
The doctor will carefully monitor and adjust the administration of NUMETA G16%E according to your child's individual needs in the following situations:
- severe trauma;
- severe diabetes;
- shock;
- heart attack;
- severe infection;
- certain types of coma.
Use with caution:
NUMETA G16%E should be used with caution if your child has:
- pulmonary edema (fluid in the lungs) or heart failure;
- severe liver function disorders;
- malabsorption;
- high blood sugar levels;
- kidney disease;
- severe metabolic disorders (when the breakdown process does not proceed normally);
- bleeding disorders.
The fluid content in your child's body, liver test results, and/or blood test results will be carefully monitored.
NUMETA G16%E and other medicines
Tell your doctor about all medicines your child is currently taking or has recently taken, as well as any medicines your child will be taking.
NUMETA G16%E must not be administered at the same time as:
- ceftriaxone(antibiotic), even in separate infusion lines, due to the risk of precipitate formation;
- bloodthrough the same infusion set, due to the risk of pseudoagglutination (red blood cells sticking together);
- ampicillin, phenytoin, or furosemidethrough the same infusion line, due to the risk of precipitate formation.
Warfarin and coumarin (anticoagulants):
The doctor will carefully monitor your child if they are taking warfarin or coumarin.
Vitamin K1 is a natural component of oil and soybean oil. Vitamin K1 may interact with medicines such as warfarin and coumarin.
Lab tests:
Lipids in this emulsion may affect the results of certain lab tests.
Lab tests should be performed 5 to 6 hours after the last lipid administration.
Interactions between NUMETA G16%E and medicines that may affect potassium levels/metabolism:
NUMETA G16%E contains potassium. High potassium levels in the blood can cause abnormal heart rhythms.
Patients taking diuretics (medicines that reduce fluid retention) or ACE inhibitors (medicines used for high blood pressure) or angiotensin II receptor antagonists (medicines used for high blood pressure) or immunosuppressive medicines (medicines that can reduce the body's normal immune response) should be closely monitored.
These types of medicines can increase potassium levels.
3. How to use NUMETA G16%E
NUMETA G16%E should always be administered to your child according to the doctor's instructions. In case of doubts, consult your doctor.
Age group
NUMETA G16%E is designed to meet the nutritional needs of infants born at term and children up to 2 years of age.
The doctor will decide if this medicine is suitable for your child.
Administration
This medicine is an infusion emulsion. It is administered through a plastic tube into a vein in the arm or a large vein in the chest.
The doctor may decide not to administer lipids to your child. The NUMETA G16%E bag is designed so that, if necessary, the partitions between the amino acid/electrolyte chamber and the glucose chamber can be broken, while the partition between the amino acid chamber and the lipid chamber remains intact.
In the case of newborns and children under 2 years of age, the solution (in bags and administration sets) should be protected from light until the end of administration (see section 2).
Dose and duration of treatment
The doctor will decide on the dose of the medicine and how long it will be administered. The dose depends on your child's nutritional needs.
The dose will be determined based on your child's weight, clinical condition, and ability to break down and utilize the components of NUMETA G16%E.
Additional nutritional components or proteins may also be administered orally or enterally.
Administration of a higher dose of NUMETA G16%E than recommended to your child
Symptoms
Too high a dose of the medicine or too rapid administration can cause:
- nausea (vomiting);
- vomiting;
- seizures;
- electrolyte disturbances (abnormal amounts of electrolytes in the blood);
- symptoms of hypervolemia (increased circulating blood volume);
- acidosis (increased blood acidity).
In such situations, the infusion should be stopped immediately. The doctor will decide if additional actions are required.
Overdose of fats contained in NUMETA G16%E can lead to fat overload syndrome, which usually resolves after stopping the infusion.
In newborns (infants) and small children (children under 2 years of age), fat overload syndrome is associated with respiratory disorders leading to reduced oxygen levels in the body (respiratory failure) and conditions leading to increased blood acidity (acidosis).
To prevent such situations, the doctor will systematically monitor your child's condition and perform blood tests during treatment.
4. Possible side effects
Like all medicines, NUMETA G16%E can cause side effects, although not all children will experience them.
If you notice any changes in your child's condition during or after treatment, tell your doctor or nurse immediately.
Tests performed by the doctor during your child's treatment should minimize the risk of side effects.
If symptoms of an allergic reaction occur, the infusion should be stopped and your doctor should be contacted immediately. This can be serious, and symptoms may include:
- sweating
- chills
- headache
- skin rash
- difficulty breathing
Other observed side effects:
Common: may affect 1 in 10 people
- Low phosphate levels in the blood (hypophosphatemia)
- High blood sugar levels (hyperglycemia)
- High calcium levels in the blood (hypercalcemia)
- High triglyceride levels in the blood (hypertriglyceridemia)
- Electrolyte disturbances (hyponatremia)
Uncommon: may affect 1 in 100 people
- High lipid levels in the blood (hyperlipidemia)
- A condition where bile cannot flow from the liver to the duodenum (cholestasis). The duodenum is part of the intestine.
Unknown: frequency cannot be determined from available data(These side effects have been reported only after peripheral administration of NUMETA G13%E Preterm and NUMETA G16%E with inadequate dilution).
- Necrosis of the skin
- Soft tissue damage
- Extravasation
The following side effects have been reported for other parenteral nutrition medicines:
Reduced or limited ability to eliminate lipids contained in NUMETA G16%E may lead to fat overload syndrome.
The following signs and symptoms of this syndrome usually resolve after stopping the fat emulsion infusion:
- Sudden and severe deterioration of the patient's condition
- High levels of fats in the blood (hyperlipidemia)
- Fever
- Fatty liver (hepatomegaly)
- Impaired liver function
- Reduced red blood cell count, which can cause paleness and weakness or shortness of breath (anemia)
- Reduced white blood cell count, which can increase the risk of infection (leukopenia)
- Reduced platelet count, which can increase the risk of bruising and/or bleeding (thrombocytopenia)
- Blood clotting disorders, which affect the blood's ability to form clots
- Respiratory disorders leading to reduced oxygen levels in the body (respiratory failure)
- Conditions leading to increased blood acidity (acidosis)
- Coma requiring hospitalization
Formation of small particles that can block blood vessels in the lungs (pulmonary vascular precipitates) or breathing difficulties.
Reporting side effects
If your child experiences any side effects, tell your doctor or nurse. This includes any side effects not listed in this leaflet.
Side effects can be reported directly to the Department of Adverse Reaction Monitoring of Medicinal Products, Medical Devices, and Biocidal Products
Al. Jerozolimskie 181 C
PL 02-222 Warsaw
Tel.: +48 22 49 21 301
Fax: +48 22 49 21 309
Website: https://smz.ezdrowie.gov.pl
Side effects can also be reported to the marketing authorization holder.
Reporting side effects will help gather more information on the safety of the medicine.
5. How to store NUMETA G16%E
Keep the medicine out of sight and reach of children when not in use.
In the case of newborns and children under 2 years of age, the solution (in bags and administration sets) should be protected from light until the end of administration (see section 2).
Do not use this medicine after the expiration date stated on the bag and outer packaging (MM/RRRR). The expiration date refers to the last day of the specified month.
Do not freeze.
Store in a protective bag.
Medicines should not be disposed of via wastewater or household waste. Ask your pharmacist how to dispose of medicines no longer required. This will help protect the environment.
6. Contents of the packaging and other information
What NUMETA G16%E looks like and what the packaging contains
NUMETA G16%E is in a triple-chamber bag. Each bag contains a sterile solution of glucose, pediatric amino acid solution with electrolytes, and fat emulsion, as described below.
| Container size | 50% glucose solution | 5.9% amino acid solution with electrolytes | 12.5% fat emulsion |
| 500 ml | 155 ml | 221 ml | 124 ml |
Appearance before preparation:
- The solutions in the amino acid and glucose chambers are clear, colorless, or slightly yellow
- The fat emulsion chamber is a uniform, milky white liquid
Appearance after preparation:
- The "2 in 1" infusion solutions are clear, colorless, or slightly yellow
- The "3 in 1" infusion emulsion is uniform and milky white
The triple-chamber bag is a multi-layer plastic bag.
To protect it from contact with air, the NUMETA bag is packaged in a protective bag that protects against oxygen, containing an oxygen absorber and an oxygen indicator.
Package sizes
500 ml bags: 6 bags in a cardboard box
1 bag of 500 ml
Not all package types may be marketed.
Marketing authorization holder and manufacturer
Marketing authorization holder
Baxter Polska Sp. z o.o.
ul. Kruczkowskiego 8
00-380 Warsaw
Manufacturer
Baxter S.A.
Boulevard Rene Branquart 80
7860 Lessines
Belgium
This medicinal product is authorized in the Member States of the European Economic Area under the following names:
| Austria Germany | Numeta G 16 % E Emulsion zur Infusion |
| Belgium Luxembourg | NUMETZAH G16%E, émulsion pour perfusion |
| France | NUMETAH G16 %E, émulsion pour perfusion |
| Denmark Norway Sweden | Numeta G16E |
| Czech Republic Greece | NUMETA G 16 % E |
| Netherlands | NUMETA G16%E emulsie voor infusie |
| Ireland United Kingdom | Numeta G16%E, Emulsion for Infusion |
| Italy | NUMETA G16%E emulsione per infusione |
| Finland | Numeta G16E infuusioneste, emulsio |
| Poland | NUMETA G16%E |
| Portugal | Numeta G16%E |
| Spain | NUMETA G16%E, emulsión para perfusión |
Date of last revision of the leaflet: May 2024
Information intended for healthcare professionals only
*In some cases, this medicine may be administered at home by parents or other caregivers.
In these cases, parents/caregivers should read the following information.
Do not add any additional components to the bag without first checking their compatibility.
This could cause the formation of particles or destabilization of the fat emulsion, leading to vein blockage.
NUMETA G16%E should reach room temperature before use.
Before administering NUMETA G16%E, prepare the bag as shown below.
Make sure the bag is not damaged. The bag can only be used if it is not damaged. The following are characteristics of an undamaged bag:
- The partitions are intact. This is indicated by the lack of mixing of the contents of any of the three chambers.
- The amino acid and glucose solutions are clear, colorless, or slightly yellow, without visible particles.
- The fat emulsion is a uniform, milky white liquid.
Before opening the protective bag, check the color of the oxygen indicator.
- Compare it with the reference color printed next to the OK symbol and shown on the labeled area of the oxygen indicator.
- Do not use the medicine if the color of the oxygen indicator does not match the reference color printed next to the OK symbol.
Figures 1 and 2 show how to remove the protective bag. Discard the protective bag, oxygen indicator, and oxygen absorber.














Figure 1
Figure 2
Preparing the mixed emulsion:
- Before breaking the seams, make sure the medicine has reached room temperature.
- Place the bag on a flat, clean surface.
Activating the triple-chamber bag (mixing 3 solutions by opening 2 breakable seams)
Step 1: Start rolling the bag from the side with the hanger.
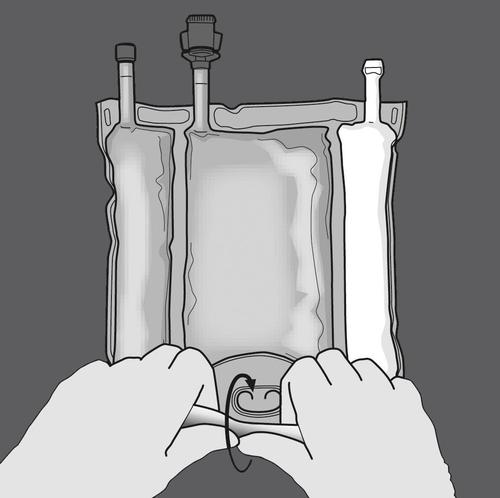
Step 2: Press until the seams open.
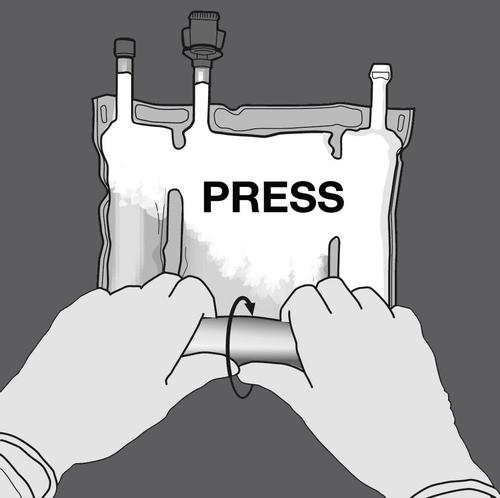
PRESS
Step 3: Change direction by rolling the bag towards the hanger. Continue until the seam is completely open.
Repeat the same procedure to completely open the second seam.


PRESS

Step 4: Rotate the bag at least three times to mix the contents thoroughly.
The mixed solution should have a milky white emulsion appearance.








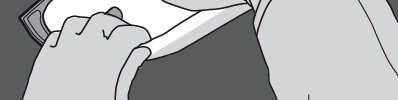
Step 5: Remove the protective cap from the administration port and insert the intravenous administration set.







Activating the double-chamber bag (mixing 2 solutions by opening the breakable seam between the amino acid and glucose chambers)
Step 1: To mix only 2 solutions, roll the bag starting from the top corner (with the hanger) next to the seam separating the solutions.
Press to open the seam separating the glucose and amino acid solutions.



PRESS

Step 2: Place the bag so that the fat emulsion chamber is closest to the user.
Roll the bag, protecting the fat emulsion chamber with your hands.
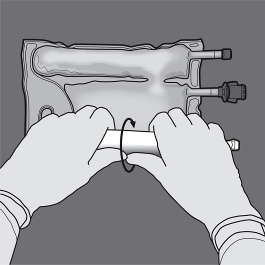
Step 3: Press with one hand and roll the bag towards the tubes.


PRESS


Step 4: Change direction by rolling the bag towards the hanger.
Press with the second hand until the seam separating the amino acid and glucose solutions is completely broken.


PRESS


Step 5: Turn the bag at least three times to mix the contents thoroughly.
The mixed solution should be clear, colorless, or slightly yellow.








Step 6: Remove the protective cap from the administration site and introduce the infusion set.
Within the first hour, the flow rate should be gradually increased. The infusion flow rate must be adjusted based on the following factors:








- administered dose
- daily intake volume
- infusion duration.
Administration method:
In the case of use in newborns and children under 2 years of age, the solution (in bags and infusion sets) should be protected from light until the end of administration.
It is recommended to use a 1.2 micron filter for the administration of NUMETA G16%E.
Due to the high osmolality, undiluted NUMETA G16%E can only be administered through a central vein. Appropriate dilution of NUMETA G16%E with water for injection reduces osmolality and allows infusion into a peripheral vessel.
The following formula illustrates the effect of dilution on the osmolality of the drug.
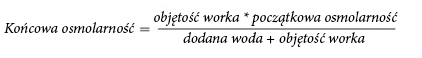
The following table shows examples of osmolality of activated two-chamber and three-chamber bags after addition of water for injection:
| Amino acids and glucose (activated W2K) | Amino acids, glucose, and lipids (activated W3K) | |
| Initial bag volume (ml) | 376 | 500 |
| Initial osmolality (mOsm/l approximately) | 1585 | 1230 |
| Added water volume (ml) | 376 | 500 |
| Final volume after addition (ml) | 752 | 1000 |
| Osmolality after addition (mOsm/l approximately) | 792.5 | 615 |
Introduction of additional components:
Exposure of parenteral nutrition solutions to light, especially after mixing with trace elements and/or vitamins, may have an adverse effect on clinical outcomes in newborns, due to the production of peroxides and other degradation products. In the case of use in newborns and children under 2 years of age, NUMETA G16%E should be protected from environmental light until the end of administration.
Compatible additional components can be added to the reconstituted mixture through the injection site (after opening the breakable seals and mixing the contents of two or three chambers).
Vitamins can also be added to the glucose-containing chamber before reconstituting the mixture (before opening the breakable seals and mixing the solutions and emulsions).
Possible additions of ready-to-use solutions of trace elements (identified as TE1, TE2, and TE4), vitamins (identified as lyophilized V1 and emulsion V2), and electrolytes in specified quantities are presented in Tables 1-6.
- 1.Compatibility with TE4, V1, and V2
Table 1: Compatibility of 3-in-1 (activated W3K) with water dilution and without dilution
| For 500 ml (after mixing 3 chambers, with lipids) | ||||||
| Addition without dilution | Addition with dilution | |||||
| Additional components | Contained amount | Maximum added amount | Maximum total amount | Contained amount | Maximum added amount | Maximum total amount |
| Sodium (mmol) | 12.0 | 25.6 | 37.6 | 12.0 | 25.6 | 37.6 |
| Potassium (mmol) | 11.4 | 26.2 | 37.6 | 11.4 | 26.2 | 37.6 |
| Magnesium (mmol) | 1.6 | 3.6 | 5.2 | 1.6 | 3.6 | 5.2 |
| Calcium (mmol) | 3.1 | 16.4 | 19.5 | 3.1 | 8.2 | 11.3 |
| Phosphates* (mmol) | 4.4 | 6.9 | 11.3 | 4.4 | 6.9 | 11.3 |
| Trace elements and vitamins | 10 ml TE4 + 1 vial V1 + 30 ml V2 | 10 ml TE4 + 1 vial V1 + 30 ml V2 | 5 mL TE4 + ½ vial V1 + 5 mL V2 | 5 ml TE4 + ½ vial V1 + 5 ml V2 | ||
| Water for injection | 350 ml | 350 ml | ||||
Table 2: Compatibility of 2-in-1 (activated W2K) with water dilution and without dilution
| For 376 ml (after mixing 2 chambers, without lipids) | ||||||
| Addition without dilution | Addition with dilution | |||||
| Additional components | Contained amount | Maximum added amount | Maximum total amount | Contained amount | Maximum added amount | Maximum total amount |
| Sodium (mmol) | 11.6 | 26.0 | 37.6 | 11.6 | 0.0 | 11.6 |
| Potassium (mmol) | 11.4 | 26.2 | 37.6 | 11.4 | 0.0 | 11.4 |
| Magnesium (mmol) | 1.6 | 3.6 | 5.2 | 1.6 | 0.0 | 1.6 |
| Calcium (mmol) | 3.1 | 8.2 | 11.3 | 3.1 | 0.0 | 3.1 |
| Phosphates* (mmol) | 3.2 |
| 11.3 | 3.2 | 0.0 | 3.2 |
| Trace elements and vitamins | 5ml TE4 + ½ vial V1 | 5ml TE4 + ½ vial V1 | 5ml TE4 + ½ vial V1 | 5ml TE4 + ½ vial V1 | ||
| Water for injection | 450 ml | 450 ml | ||||
- 2.Compatibility with TE1, V1, and V2Table 3: Compatibility of 3-in-1 (activated W3K) with water dilution and without dilution
| For 500 ml (after mixing 3 chambers, with lipids) | ||||||
| Addition without dilution | Addition with dilution | |||||
| Additional components | Contained amount | Maximum added amount | Maximum total amount | Contained amount | Maximum added amount | Maximum total amount |
| Sodium (mmol) | 12.0 | 4.0 | 16.0 | 12.0 | 0.0 | 12.0 |
| Potassium (mmol) | 11.4 | 6.2 | 17.6 | 11.4 | 0.0 | 11.4 |
| Magnesium (mmol) | 1.6 | 0 | 1.6 | 1.6 | 0.0 | 1.6 |
| Calcium (mmol) | 3.1 | 2.1 | 5.2 | 3.1 | 0.0 | 3.1 |
| Phosphates* (mmol) | 4.4 | 2.0 | 6.4 | 4.4 | 0.0 | 4.4 |
| Trace elements and vitamins | 5 ml TE1 + ½ vial V1 + 5 ml V2 | 5 ml TE1 + ½ vial V1 + 5 ml V2 | 5 ml TE1 + ½ vial V1 + 5 ml V2 | 5 ml TE1 + ½ vial V1 + 5 ml V2 | ||
| Water for injection | 350 ml | 350 ml | ||||
Table 4: Compatibility of 2-in-1 (activated W2K) with water dilution and without dilution
| For 376 ml (after mixing 2 chambers, without lipids) | ||||||
| Addition without dilution | Addition with dilution | |||||
| Additional components | Contained amount | Maximum added amount | Maximum total amount | Contained amount | Maximum added amount | Maximum total amount |
| Sodium (mmol) | 11.6 | 26.0 | 37.6 | 11.6 | 0.0 | 11.6 |
| Potassium (mmol) | 11.4 | 26.2 | 37.6 | 11.4 | 0.0 | 11.4 |
| Magnesium (mmol) | 1.6 | 3.6 | 5.2 | 1.6 | 0.0 | 1.6 |
| Calcium (mmol) | 3.1 | 8.2 | 11.3 | 3.1 | 0.0 | 3.1 |
| Phosphates* (mmol) | 3.2 | 8.1 | 11.3 | 3.2 | 0.0 | 3.2 |
| Trace elements and vitamins | 5 ml TE1 + ½ vial V1 | 5 ml TE1 + ½ vial V1 | 5 ml TE1 + ½ vial V1 | 5 ml TE1 + ½ vial V1 | ||
| Water for injection | 450 ml | 450 ml | ||||
- 3.Compatibility with TE2, V1, and V2Table 5: Compatibility of 3-in-1 (activated W3K) with water dilution and without dilution
| For 500 ml (after mixing 3 chambers, with lipids) | ||||||
| Addition without dilution | Addition with dilution | |||||
| Additional components | Contained amount | Maximum added amount | Maximum total amount | Contained amount | Maximum added amount | Maximum total amount |
| Sodium (mmol) | 12.0 | 4.0 | 16.0 | 12.0 | 0.0 | 12.0 |
| Potassium (mmol) | 11.4 | 6.2 | 17.6 | 11.4 | 0.0 | 11.4 |
| Magnesium (mmol) | 1.6 | 0 | 1.6 | 1.6 | 0.0 | 1.6 |
| Calcium (mmol) | 3.1 | 2.1 | 5.2 | 3.1 | 0.0 | 3.1 |
| Phosphates* (mmol) | 4.4 | 2.0 | 6.4 | 4.4 | 0.0 | 4.4 |
| Trace elements and vitamins | 5 ml TE2 + ½ vial V1 + 5 ml V2 | 5 ml TE2 + ½ vial V1 + 5 ml V2 | 5 ml TE2 + ½ vial V1 + 5 ml V2 | 5 ml TE2 + ½ vial V1 + 5 ml V2 | ||
| Water for injection | 350 ml | 350 ml | ||||
Table 6: Compatibility of 2-in-1 (activated W2K) with water dilution and without dilution
| For 376 ml (after mixing 2 chambers, without lipids) | ||||||
| Addition without dilution | Addition with dilution | |||||
| Additional components | Contained amount | Maximum added amount | Maximum total amount | Contained amount | Maximum added amount | Maximum total amount |
| Sodium (mmol) | 11.6 | 26.0 | 37.6 | 11.6 | 0.0 | 11.6 |
| Potassium (mmol) | 11.4 | 26.2 | 37.6 | 11.4 | 0.0 | 11.4 |
| Magnesium (mmol) | 1.6 | 3.6 | 5.2 | 1.6 | 0.0 | 1.6 |
| Calcium (mmol) | 3.1 | 8.2 | 11.3 | 3.1 | 0.0 | 3.1 |
| Phosphates* (mmol) | 3.2 | 8.1 | 11.3 | 3.2 | 0.0 | 3.2 |
| Trace elements and vitamins | 5 ml TE2 + ½ vial V1 | 5 ml TE2 + ½ vial V1 | 5 ml TE2 + ½ vial V1 | 5 ml TE2 + ½ vial V1 | ||
| Water for injection | 450 ml | 450 ml | ||||
The composition of the used ready-to-use preparations containing vitamins and trace elements is presented in Tables 7 and 8.
Table 7: Composition of the used ready-to-use preparation containing trace elements:
| Composition per vial of 10 ml | TE1 | TE2 | TE4 |
| Iron | 8.9 µmol or 0.5 mg | ||
| Zinc | 38.2 µmol or 2.5 mg | 15.3 µmol or 1 mg | 15.3 µmol or 1 mg |
| Selenium | 0.253 µmol or 0.02 mg | 0.6 µmol or 0.05 mg | 0.253 µmol or 0.02 mg |
| Copper | 3.15 µmol or 0.2 mg | 4.7 µmol or 0.3 mg | 3.15 µmol or 0.2 mg |
| Iodine | 0.0788 µmol or 0.01 mg | 0.4 µmol or 0.05 mg | 0.079 µmol or 0.01 mg |
| Fluorine | 30 µmol or 0.57 mg | 26.3 µmol or 0.5 mg | |
| Molybdenum | 0.5 µmol or 0.05 mg | ||
| Manganese | 0.182 µmol or 0.01 mg | 1.8 µmol or 0.1 mg | 0.091 µmol or 0.005 mg |
| Cobalt | 2.5 µmol or 0.15 mg | ||
| Chromium | 0.4 µmol or 0.02 mg |
Table 8: Composition of the used ready-to-use preparation containing vitamins:
Introduction of additional components:
- Aseptic conditions must be maintained.
- Prepare the injection site on the bag.
- Puncture the injection site and inject additional components using a syringe or a device for preparing the drug.
- Mix the contents of the bag with the additional components.
Preparation of infusion:
- Aseptic conditions must be maintained.
- Suspend the bag.
- Remove the plastic protector from the administration port.
- Insert the infusion set needle into the administration port with a firm motion.
Infusion administration:
- For single use only.
- Administer the drug only after breaking the seals between the two or three chambers and mixing the contents of the two or three chambers.
- Ensure that the activated three-chamber bag infusion emulsion does not separate phases or that the activated two-chamber bag infusion solution does not contain any solid particles.
- It is recommended to use the drug immediately after opening the breakable seals. NUMETA G16%E should not be stored for the next infusion.
- Do not connect partially used bags.
- To avoid air embolism caused by residual air in the first bag, do not connect bags in series.
- It is recommended to use a 1.2 micron filter for the administration of NUMETA G16%E.
- In the case of use in newborns and children under 2 years of age, protect from light until the end of administration. Exposure of NUMETA G16%E to environmental light, especially after mixing with trace elements and/or vitamins, causes the production of peroxides and other degradation products, which can be reduced by protecting from light.
- Any unused drug or its waste and the entire single-use set required should be disposed of properly.
| Composition per vial | V1 | V2 |
| Vitamin B1 | 2.5 mg | |
| Vitamin B2 | 3.6 mg | |
| Niacinamide | 40 mg | |
| Vitamin B6 | 4.0 mg | |
| Pantothenic acid | 15.0 mg | |
| Biotin | 60 µg | |
| Folic acid | 400 µg | |
| Vitamin B12 | 5.0 µg | |
| Vitamin C | 100 mg | |
| Vitamin A | 2300 IU | |
| Vitamin D | 400 IU | |
| Vitamin E | 7 IU | |
| Vitamin K | 200 µg |
Shelf life after mixing solutions:
The drug should be used immediately after opening the breakable seals between the two or three chambers.
Stability studies of mixtures were conducted for 7 days at a temperature of 2°C to 8°C, and then for 48 hours at 30°C.
Shelf life after introduction of additional components (electrolytes, trace elements, vitamins, water)
For specified additional components, the physical stability of NUMETA has been demonstrated for 7 days at a temperature of 2°C to 8°C, and then for 48 hours at 30°C.
From a microbiological point of view, the drug should be used immediately. If such a drug is not used immediately, the user is responsible for the time and conditions of storage until its use, but it is not recommended to exceed 24 hours at a temperature of 2°C to 8°C, unless the preparation/dissolution/introduction of additional components was carried out in controlled and validated aseptic conditions.
Do not use NUMETA G16%E if the bag is damaged. The following are characteristics of a damaged bag:
- Breakable seals are open
- Any of the chambers contains a mixture of solutions
- The amino acid and glucose solutions are not clear, colorless, or slightly yellow and/or contain visible particles
- The fat emulsion is not a uniform, milky liquid.
Medicines should not be disposed of via wastewater or household waste. Ask your pharmacist how to dispose of medicines that are no longer needed. This will help protect the environment.
What NUMETA G16%E contains
Active substances:
| Composition | ||
| Active substance | Activated W2K (376 ml) | Activated W3K (500 ml) |
| Amino acid chamber | ||
| Alanine | 1.03 g | 1.03 g |
| Arginine | 1.08 g | 1.08 g |
| Aspartic acid | 0.77 g | 0.77 g |
| Cysteine | 0.24 g | 0.24 g |
| Glutamic acid | 1.29 g | 1.29 g |
| Glycine | 0.51 g | 0.51 g |
| Histidine | 0.49 g | 0.49 g |
| Isoleucine | 0.86 g | 0.86 g |
| Leucine | 1.29 g | 1.29 g |
| Lysine monohydrate (equivalent to lysine) | 1.59 g (1.42 g) | 1.59 g (1.42 g) |
| Methionine | 0.31 g | 0.31 g |
| Ornithine hydrochloride (equivalent to ornithine) | 0.41 g (0.32 g) | 0.41 g (0.32 g) |
| Phenylalanine | 0.54 g | 0.54 g |
| Proline | 0.39 g | 0.39 g |
| Serine | 0.51 g | 0.51 g |
| Taurine | 0.08 g | 0.08 g |
| Threonine | 0.48 g | 0.48 g |
| Tryptophan | 0.26 g | 0.26 g |
| Tyrosine | 0.10 g | 0.10 g |
| Valine | 0.98 g | 0.98 g |
| Sodium chloride | 0.30 g | 0.30 g |
| Potassium acetate | 1.12 g | 1.12 g |
| Calcium chloride dihydrate | 0.46 g | 0.46 g |
| Magnesium acetate tetrahydrate | 0.33 g | 0.33 g |
| Sodium glycerophosphate hydrate | 0.98 g | 0.98 g |
| Glucose chamber | ||
| Glucose monohydrate (equivalent to anhydrous glucose) | 85.25 g (77.50 g) | 85.25 g (77.50 g) |
| Lipid chamber | ||
| Purified olive oil (about 80%) + purified soybean oil (about 20%) | 15.5 g | |
The solution/emulsion after mixing contains the following components:
| Composition | ||||
| Activated W2K | Activated W3K | |||
| Per unit of volume (ml) Nitrogen (g) Amino acids (g) Glucose (g) Lipids (g) Energy value Total energy value (kcal) Non-protein energy value (kcal) Glucose energy value (kcal) Lipid energy value (kcal) Non-protein energy value/nitrogen (kcal/g N) Lipid energy value/non-protein energy value (%) Lipid energy value/total energy value (%) Electrolytes Sodium (mmol) Potassium (mmol) Magnesium (mmol) Calcium (mmol) Phosphates* (mmol) | 376 2.0 13.0 77.5 0 362 310 310 0 158 Not applicable Not applicable 11.6 11.4 1.6 3.1 3.2 | 100 0.52 3.5 20.6 0 96 82 82 0 158 Not applicable Not applicable 3.1 3.0 0.41 0.82 0.85 | 500 2.0 13.0 77.5 15.5 517 465 310 155 237 33 30 12.0 11.4 1.6 3.1 4.4 | 100 0.39 2.6 15.5 3.1 103 93 62 31 237 33 30 2.4 2.3 0.31 0.62 0.87 |
| Acetates (mmol) Malates (mmol) Chlorides (mmol) | 14.5 4.3 13.8 | 3.9 1.1 3.7 | 14.5 4.3 13.8 | 2.9 0.86 2.8 |
| pH (approximately) Osmolality (approximately, mOsm/l) | 5.5 1585 | 5.5 1585 | 5.5 1230 | 5.5 1230 |
Including the energy value of egg phospholipids for injection.
Including phosphates from egg phospholipids for injection, which are a component of the lipid emulsion.
Other components:
L-malic acid
Hydrochloric acid
Egg phospholipids for injection
Glycerol
Sodium oleate
Sodium hydroxide
Water for injection
to adjust pH
Baxter, Numeta, Numetzah, and Numetah are trademarks of Baxter International Inc.
- Country of registration
- Active substance
- Prescription requiredYes
- Manufacturer
- ImporterBaxter S.A.
- This information is for reference only and does not constitute medical advice. Always consult a licensed doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to Numeta G16%eDosage form: Solution, -Active substance: combinationsPrescription not requiredDosage form: Solution, -Active substance: combinationsPrescription not requiredDosage form: Solution, -Active substance: combinationsPrescription not required
Alternatives to Numeta G16%e in other countries
The best alternatives with the same active ingredient and therapeutic effect.
Alternative to Numeta G16%e in Spain
Alternative to Numeta G16%e in Ukraine
Online doctors for Numeta G16%e
Discuss dosage, side effects, interactions, contraindications, and prescription renewal for Numeta G16%e – subject to medical assessment and local rules.














