

Fraxiparine

Ask a doctor about a prescription for Fraxiparine

How to use Fraxiparine
1. What is Fraxiparine and what is it used for
Fraxiparine is a medicine that helps prevent the formation of blood clots in blood vessels or treats existing blood clots. Medicines of this type are called anticoagulants.
The medicine is given by injection under the skin or into a vein.
Indications for use:
- prevention of venous thromboembolic disease in surgery and orthopedic surgery;
- prevention of venous thromboembolic disease in immobilized patients for reasons other than surgery, who have a high risk of thromboembolic complications (e.g. severe chronic obstructive pulmonary disease, heart failure, severe infections, etc.);
- prevention of clotting in the extracorporeal circulation system during hemodialysis;
- treatment of deep vein thrombosis with or without pulmonary embolism;
- treatment of unstable angina and myocardial infarction without Q-wave, in combination with acetylsalicylic acid.
2. Important information before using Fraxiparine
When not to use Fraxiparine
- if you are allergic to the active substance nadroparin calcium, heparin or a similar product (such as enoxaparin, bemiparin, dalteparin) or any of the other ingredients of this medicine (listed in section 6);
- if you have had a decrease in platelet count (thrombocytopenia) after using Fraxiparine in the past;
- if you have bleeding or any disease that affects blood clotting;
- if you have a medical condition that increases the risk of bleeding [e.g. active gastric or duodenal ulcer];
- if you have had a recent hemorrhagic stroke;
- if you have acute infectious endocarditis;
- if you have severe kidney dysfunction and are taking anticoagulant medications, e.g. for pulmonary embolism or deep vein thrombosis;
- if you have severe kidney dysfunction and are taking medications for heart disease (e.g. unstable angina or myocardial infarction without Q-wave).
Warnings and precautions
During treatment with Fraxiparine, a decrease in platelet count may rarely occur, which can sometimes be severe. During treatment, your doctor will prescribe blood tests to check for this effect.
Before using Fraxiparine, you should tell your doctor if:
- you have conditions that increase the risk of bleeding, in particular, if:
- you have gastric or duodenal ulcer,
- you have bleeding disorders,
- you have recently had surgery in the brain, spinal cord, or eye,
- you have high blood pressure;
- you have severe liver dysfunction;
- you have kidney dysfunction;
- you have eye diseases affecting blood vessels (vascular retinopathy);
- you are taking other medications that affect blood clotting (see "Fraxiparine and other medications").
In case of bleeding, you should immediately contact your doctor.
In case of skin necrosis, which may be preceded by minor subcutaneous bleeding or hard or painful redness of the skin, you should immediately stop taking the medicine and contact your doctor.
Using Fraxiparine may cause an increase in potassium levels in the blood. If you have diseases that may cause an increase in potassium levels, such as diabetes, severe kidney disease, previous metabolic acidosis, or if you are taking other medications that increase potassium levels in the blood, your doctor may prescribe regular blood tests. If you are not sure if you are taking such medications, you should ask your doctor.
If you are undergoing spinal or epidural anesthesia, or if you are having a lumbar puncture, there is a risk of bleeding into the spinal cord at the injection site, which can lead to serious consequences. During such procedures, your condition will be closely monitored to check for any worrying symptoms.
If you are elderly (over 65 years old), your doctor may prescribe blood tests before starting treatment with Fraxiparine.
The needle shield of the pre-filled syringe may contain latex [see "The packaging of the medicine contains latex (natural rubber)"].
Fraxiparine and other medications
Tell your doctor or pharmacist about all medications you are currently taking or have recently taken, as well as any medications you plan to take.
It is not recommended to use Fraxiparine with the following medications due to the risk of bleeding. If this cannot be avoided, your doctor will closely monitor your condition. This applies to the following medications:
- acetylsalicylic acid (e.g. aspirin),
- non-steroidal anti-inflammatory drugs (NSAIDs) (medications used to relieve pain, e.g. ibuprofen),
- antiplatelet agents (used to prevent blood clots, e.g. clopidogrel).
Fraxiparine should be used with caution with:
- oral anticoagulants (medications that prevent blood clotting, e.g. warfarin),
- glucocorticosteroids (steroid medications used to treat e.g. asthma),
- dextran (a medication given intravenously to increase blood volume).
Pregnancy, breastfeeding, and fertility
If you are pregnant or breastfeeding, think you may be pregnant, or plan to have a child, ask your doctor or pharmacist for advice before using this medicine.
Fraxiparine may only be used during pregnancy if your doctor considers that the expected benefits of using the medicine outweigh the possible risks.
It is not known whether the ingredients of Fraxiparine pass into breast milk, so you should not breastfeed during treatment with Fraxiparine.
There is no data on the effect of nadroparin on fertility.
Driving and using machines
There is no data on the effect of Fraxiparine on the ability to drive and use machines.
The packaging of the medicine may contain latex (natural rubber)
The packaging of the medicine (needle shield) may contain latex. This can cause severe allergic reactions.
3. How to use Fraxiparine
This medicine should always be used exactly as your doctor has told you. If you are not sure, ask your doctor or pharmacist.
Method of administration
Fraxiparine is given by injection under the skin or into a vein.
Fraxiparine should not be given by intramuscular injection.
The pre-filled syringe with graduated markings makes it easier to administer the correct dose, if dose adjustment is necessary based on the patient's body weight.
When administering the medicine by subcutaneous injection, the anterior abdominal wall is usually chosen as the injection site, alternating between the right and left side. Another injection site may be the thigh.
Detailed instructions for self-administration of subcutaneous injections of Fraxiparine can be found in the section "Instructions for self-administration of subcutaneous injections of Fraxiparine".
Recommended dosage
The dosage is determined by your doctor, individually for each patient, based on the indication, clinical condition, and body weight.
Use in children and adolescents
Fraxiparine should not be used in children and adolescents.
Elderly patients (over 65 years old)
In these patients, kidney function may be impaired. Therefore, your doctor may prescribe kidney function tests and adjust the dose of Fraxiparine accordingly.
Kidney dysfunction
Your doctor will adjust the dose of Fraxiparine according to the severity of kidney dysfunction.
Fraxiparine is contraindicated in patients with severe kidney dysfunction.
Using a higher dose of Fraxiparine than recommended
If a higher dose of Fraxiparine than recommended is used, you should immediately contact your doctor. The main symptom of overdose is bleeding.
Missing a dose of Fraxiparine
You should continue using the medicine, without increasing the next dose. Do not reduce the time interval between injections.
Do not take a double dose to make up for a missed dose.
Stopping treatment with Fraxiparine
Fraxiparine should be used for as long as your doctor has prescribed. Do not stop using Fraxiparine without consulting your doctor.
If you want to stop using Fraxiparine, you should discuss this with your doctor or pharmacist first.
If you have any further questions about using this medicine, ask your doctor or pharmacist.
4. Possible side effects
Like all medicines, Fraxiparine can cause side effects, although not everybody gets them.
You should immediately stop using the medicine and contact your doctor if you experience:
- an allergic reactionwith symptoms such as hives (red, itchy blisters on the skin), angioedema (swelling of the face or lips that can make breathing difficult),
- skin necrosis at the injection site -this is preceded by subcutaneous bleeding or hard or painful redness of the skin with or without general symptoms.
Very common side effects(may affect more than 1 in 10 people):
- bleeding at various sites, more common in patients with other risk factors,
- small hematomas at the injection site. In some cases, hard lumps may appear, which do not indicate heparin crystallization and should disappear after a few days.
Common side effects(may affect up to 1 in 10 people):
- skin reaction at the injection site,
- increased liver enzyme activity in the blood (aminotransferases), usually transient (visible in blood test results).
Rare side effects(may affect up to 1 in 1,000 people):
- decrease in platelet count (thrombocytopenia),
- increase in platelet count (thrombocytosis),
- rash, hives, redness, itching of the skin,
- calcification under the skin at the injection site.
Very rare side effects(may affect up to 1 in 10,000 people):
- allergic reactions, including angioedema and skin reactions,
- pseudoanaphylactic reaction (symptoms are similar to anaphylaxis -allergic
- see the beginning of this section),
- skin necrosis,
- increase in eosinophil count (a type of white blood cell) - transient after treatment (visible in blood test results),
- increase in potassium levels in the blood,
- prolonged, painful erection of the penis (priapism) - if this occurs, you should immediately contact your doctor, as you may need treatment to avoid serious complications.
Unknown(frequency cannot be estimated from available data)
- headache,
- migraine.
Reporting side effects
If you experience any side effects, including those not listed in this leaflet, please tell your doctor or pharmacist. Side effects can be reported directly to the Department of Drug Safety Monitoring, Office for Registration of Medicinal Products, Medical Devices, and Biocidal Products, Al. Jerozolimskie 181C, 02-222 Warsaw, tel.: +48 22 49 21 301, fax: +48 22 49 21 309, website: https://smz.ezdrowie.gov.pl
Side effects can also be reported to the marketing authorization holder.
By reporting side effects, you can help provide more information on the safety of this medicine.
5. How to store Fraxiparine
Keep the medicine out of the sight and reach of children.
Store in a temperature below 30°C.
Do not use this medicine after the expiry date stated on the packaging. The expiry date refers to the last day of the month.
Medicines and syringes should not be disposed of in the sewage system or household waste containers.
Ask your pharmacist how to dispose of medicines that are no longer needed. This will help protect the environment.
6. Contents of the pack and other information
What Fraxiparine contains
- The active substance of the medicine is: 2,850 IU AXa nadroparin calcium in 0.3 ml solution for injection, 3,800 IU AXa nadroparin calcium in 0.4 ml solution for injection, 5,700 IU AXa nadroparin calcium in 0.6 ml solution for injection, 7,600 IU AXa nadroparin calcium in 0.8 ml solution for injection, 9,500 IU AXa nadroparin calcium in 1 ml solution for injection
- The other ingredients are: calcium hydroxide solution or diluted hydrochloric acid to adjust pH, water for injections.
What Fraxiparine looks like and contents of the pack
Fraxiparine is a solution for injection. The pre-filled syringe contains a clear to slightly opalescent, colorless or slightly yellowish or slightly brownish or slightly dark yellow solution. The medicine is packaged in pre-filled syringes with a protective needle shield.
The pack contains 2 or 10 pre-filled syringes with a protective needle shield, in individual blisters, in a cardboard box.
Marketing authorization holder
Viatris Healthcare Sp. z o.o.
ul. Postępu 21B
02-676 Warsaw
tel.: 22 546 64 00
Manufacturer
Aspen Notre Dame de Bondeville
1, rue de l’Abbaye
76960 Notre-Dame de Bondeville
France
or
GlaxoSmithKline Pharmaceuticals S.A.
ul. Grunwaldzka 189
60-322 Poznań
Date of last revision of the leaflet: 02/2024
Information for healthcare professionals
Detailed dosage and administration instructions can be found in section 4.2 of the approved Summary of Product Characteristics.
INSTRUCTIONS FOR SELF-ADMINISTRATION OF SUBCUTANEOUS INJECTIONS OF FRAXIPARINE
FRAXIPARINE
- 1. Wash your hands thoroughly with soap and water and dry them with a towel.
- 2. Sit or lie down in a comfortable position. Choose an injection site on the side of your abdomen (Figure 1). Injections should be administered alternately on the left and right side.
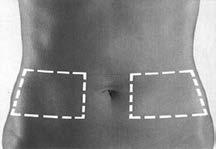
Figure 1
- 3. Clean the injection site with a swab soaked in spirit.
- 4. Remove the needle shield. The needle shield should be discarded.
Important notes
- Do not touch the needle and do not let the needle come into contact with other surfaces before injection.
- The presence of a small air bubble in the pre-filled syringe is normal. Do not remove the air bubble before administering the injection - this may lead to loss of part of the medicine.
- 5. Hold the previously cleaned skin with your fingers, creating a skin fold. Hold the skin fold between your thumb and index finger during the entire injection process (Figure 2).

Figure 2
- 6. Hold the pre-filled syringe with the grip firmly between your fingers. Insert the entire length of the needle into the skin fold at a right angle (Figure 3).

Figure 3
- 7.Inject the entire contents of the pre-filled syringe by pressing the plunger down until resistance is felt.
- 8. Remove the needle with the pre-filled syringe from the skin (Figure 4). Do not rub the injection site.

Figure 4
- 9. Appearance of the pre-filled syringe after injection (Figure 5).

Protective needle shield
Pre-filled syringe handle
Figure 5
- 10. After injection, slide the protective needle shield over the pre-filled syringe to protect against needlestick injury (Figure 6). Holding the pre-filled syringe handle firmly with one hand, use the other hand to grasp the outer shield of the pre-filled syringe and slide it towards the needle. The shield will unlock. Then, slide the shield to the position where it will lock, covering the entire needle. During shield release and locking, resistance is felt.

Figure 6
- 11. Appearance of the pre-filled syringe after sliding the protective needle shield (Figure 7).

Protective needle shield
Pre-filled syringe handle
Figure 7
- 12. The used pre-filled syringe should not be thrown away in household waste containers. It should be disposed of in accordance with the doctor's or pharmacist's instructions.
- Country of registration
- Active substance
- Prescription requiredYes
- Manufacturer
- ImporterAspen Notre Dame de Bondeville GlaxoSmithKline Pharmaceuticals S.A.
- This information is for reference only and does not constitute medical advice. Always consult a licensed doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to FraxiparineDosage form: Solution, 5700 IU/0.6 mlActive substance: nadroparinPrescription requiredDosage form: Solution, 9500 IU aXa/mlActive substance: nadroparinPrescription requiredDosage form: Solution, 2850 IU aXa/0.3 mlActive substance: nadroparinPrescription required
Alternatives to Fraxiparine in other countries
The best alternatives with the same active ingredient and therapeutic effect.
Alternative to Fraxiparine in Ukraine
Alternative to Fraxiparine in Spain
Online doctors for Fraxiparine
Discuss dosage, side effects, interactions, contraindications, and prescription renewal for Fraxiparine – subject to medical assessment and local rules.














