
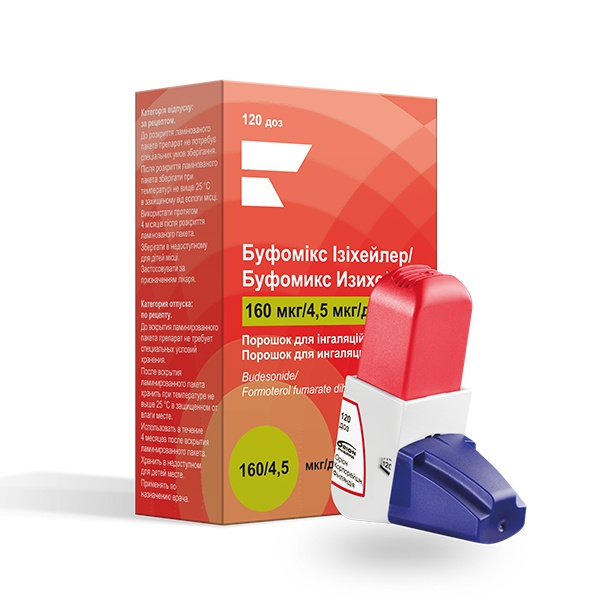
Bufomix Easihaler
Ask a doctor about a prescription for Bufomix Easihaler

How to use Bufomix Easihaler
CHARACTERISTICS OF THE MEDICINAL PRODUCT
1. NAME OF THE MEDICINAL PRODUCT
Bufomix Easyhaler, (320 micrograms + 9 micrograms)/inhalation dose, powder for inhalation.
2. QUALITATIVE AND QUANTITATIVE COMPOSITION
Each delivered dose (dose leaving the inhaler mouthpiece) contains 320 micrograms of budesonide and 9 micrograms of formoterol fumarate dihydrate per inhalation dose. For the Easyhaler inhaler, the delivered dose (from the metering valve) contains a similar amount of active substance as the metered dose (from the reservoir). Excipient with known effect: lactose monohydrate (7,600 micrograms in the delivered dose). Full list of excipients, see section 6.1.
3. PHARMACEUTICAL FORM
Powder for inhalation in a metered-dose inhaler (Easyhaler). White to yellowish powder.
4. CLINICAL PARTICULARS
4.1 Therapeutic Indications
Asthma
Bufomix Easyhaler is indicated for the regular treatment of asthma in adults and adolescents (12 years and older) where a combination of inhaled corticosteroid and long-acting β2-adrenergic agonist is appropriate: for patients not adequately controlled with inhaled corticosteroids and as-needed inhaled β2-adrenergic agonists, or for patients who are already being treated with a combination of inhaled corticosteroids and long-acting β2-adrenergic agonists.
- for patients who are not adequately controlled with inhaled corticosteroids and as-needed inhaled β2-adrenergic agonists, or
- for patients who are already being treated with a combination of inhaled corticosteroids and long-acting β2-adrenergic agonists.
COPD (Chronic Obstructive Pulmonary Disease)
Bufomix Easyhaler is indicated for the symptomatic treatment of COPD in adult patients (18 years and older) with a forced expiratory volume in one second (FEV1) <70% of the predicted normal value and with a history of repeated exacerbations, despite regular treatment with bronchodilators.
4.2 Posology and Method of Administration
Dosage
Asthma
Bufomix Easyhaler is not intended for the initial treatment of asthma. The dosage of Bufomix Easyhaler should be individualized and adjusted to the severity of the disease. The dose should be titrated to the lowest dose that effectively controls symptoms. If a patient requires doses other than those available in the Easyhaler inhaler, other combinations of β2-agonists and corticosteroids should be prescribed separately.
Recommended doses:
Adults (over 18 years): 1 inhalation twice daily. Some patients may need a dose of up to 2 inhalations twice daily.
Adolescents (12-17 years): 1 inhalation twice daily.
Patients should be regularly reviewed by a physician or healthcare provider to ensure that the dose of Bufomix Easyhaler is optimal. The dose should be titrated to the lowest effective dose that maintains adequate control of symptoms. Once control of asthma has been achieved, the dose of Bufomix Easyhaler should be gradually reduced to the lowest dose that maintains control.
In clinical practice, after achieving control of symptoms with twice-daily dosing, a reduction in dose to the lowest effective dose that maintains control may involve reducing the dose to once-daily dosing if, in the physician's judgment, a long-acting bronchodilator in combination with an inhaled corticosteroid is still required to maintain control.
Increasing use of short-acting relievers indicates deterioration of asthma control and warrants reassessment of the patient's therapeutic regimen.
Children (6 years and older): For children aged 6 to 11 years, a lower strength (80 micrograms + 4.5 micrograms)/inhalation dose is available.
Children under 6 years: Bufomix Easyhaler is not recommended for children under 6 years.
Bufomix Easyhaler, (320 micrograms + 9 micrograms)/inhalation dose, should only be used for maintenance therapy.
Lower strengths of the medicinal product (160 micrograms + 4.5 micrograms)/inhalation dose and 80 micrograms + 4.5 micrograms)/inhalation dose) are available for maintenance and reliever therapy.
For doses that cannot be achieved with Bufomix Easyhaler, other strengths of budesonide and formoterol are available.
COPD
Recommended dose:
Adults: 1 inhalation twice daily.
General Information
Special patient populations:
There are no special dosing requirements for elderly patients. There are no data available on the use of Bufomix Easyhaler in patients with impaired liver or kidney function. Since budesonide and formoterol are primarily eliminated by hepatic metabolism, increased exposure may be expected in patients with severe liver cirrhosis.
Method of administration:
Inhalation.
Instructions for proper use of Bufomix Easyhaler:
The inhaler is breath-actuated, which means that the substance is released when the patient inhales through the mouthpiece.
Caution! Patients should be instructed to:
- read the patient information leaflet carefully before using Bufomix Easyhaler;
- shake and prime the inhaler before each use;
- breathe strongly and deeply through the mouthpiece to ensure optimal delivery of the dose to the lungs;
- never exhale through the mouthpiece, as this may reduce the delivered dose. In such cases, the patient should tap the mouthpiece on a table or hand to remove the powder and repeat the dosing procedure;
- never activate the inhaler more than once without inhaling the powder. In such cases, the patient should tap the mouthpiece on a table or hand to remove the powder and repeat the dosing procedure;
- always replace the cover (and protective cap, if used) after use to prevent accidental activation of the inhaler (which may lead to overdose or underdose at the next use);
- rinsing the mouth with water after inhalation of the maintenance dose to minimize the risk of oral thrush and throat infections. Patients who develop oral thrush should also rinse their mouths after reliever inhalations;
- regularly cleaning the mouthpiece with a dry cloth. Water should not be used for cleaning, as the powder should not come into contact with moisture;
- replacing the Bufomix Easyhaler inhaler when the counter shows zero, even if powder is still visible in the inhaler.
4.3 Contraindications
Hypersensitivity to the active substances or to the excipient listed in section 6.1 (lactose, which contains small amounts of milk proteins).
4.4 Special Warnings and Precautions for Use
It is recommended to taper the dose before discontinuing treatment. Treatment should not be stopped abruptly.
If a patient believes that their treatment is not effective or is taking the highest recommended dose of Bufomix Easyhaler, they should consult their doctor (see section 4.2). Increasing use of short-acting relievers indicates deterioration of the underlying condition and justifies reassessment of the asthma treatment.
Sudden and progressive worsening of asthma control or COPD may be life-threatening. Patients should be reviewed by a physician and, if necessary, alternative treatment should be initiated. A paradoxical bronchospasm may occur, which can lead to immediate worsening of wheezing and shortness of breath after inhalation. If paradoxical bronchospasm occurs, treatment with Bufomix Easyhaler should be discontinued immediately, the patient should be reviewed, and, if necessary, alternative treatment should be initiated. Paradoxical bronchospasm responds to a short-acting inhaled bronchodilator (see section 4.8).
Systemic effects may occur with all inhaled corticosteroids, particularly at high doses for prolonged periods. The risk of systemic effects is less with inhaled corticosteroids than with oral corticosteroids. Possible systemic effects include Cushing's syndrome, Cushingoid features, adrenal suppression, growth retardation in children and adolescents, decreased bone mineral density, cataracts, and glaucoma, as well as a range of psychological and behavioral effects, including psychomotor hyperactivity, sleep disturbances, anxiety, depression, or aggression (particularly in children) (see section 4.8).
Visual disturbances may occur due to systemic or local use of corticosteroids. If a patient presents with symptoms such as blurred vision or other visual disturbances, an ophthalmological examination should be considered to rule out causes such as cataract, glaucoma, or rare conditions such as central serous chorioretinopathy (CSCR), which have been reported after systemic and local use of corticosteroids.
Potential impact on bone mineral density should be considered, particularly for patients taking high doses for prolonged periods and those with risk factors for osteoporosis.
Long-term studies with inhaled budesonide in children at doses up to 400 micrograms/day (metered dose) or in adults at doses up to 800 micrograms/day (metered dose) have not shown any significant effects on bone mineral density.
There are no data on the effects of higher doses.
If adrenal insufficiency is suspected due to previous systemic steroid therapy, caution should be exercised when initiating treatment with Bufomix Easyhaler.
The benefits of inhaled budesonide generally minimize the need for oral steroids; however, patients transferring from oral steroids may remain at risk of adrenal insufficiency for some time. Recovery may take longer after stopping oral steroid therapy. Therefore, in patients dependent on oral steroids, transferring to inhaled budesonide, the risk of adrenal insufficiency may persist for some time. Regular monitoring of adrenal function is recommended.
Prolonged treatment with high doses of inhaled corticosteroids may lead to clinically significant adrenal suppression. Therefore, during stress (e.g., severe infections or planned surgery), consideration should be given to additional oral corticosteroid therapy. Abrupt reduction of oral corticosteroid dose may precipitate an acute adrenal crisis.
Symptoms and signs that may be associated with an acute adrenal crisis include anorexia, abdominal pain, weight loss, fatigue, headache, nausea, vomiting, decreased consciousness, seizures, hypotension, and hypoglycemia.
Oral corticosteroid therapy should not be stopped abruptly or reduced rapidly.
During the transition from oral to inhaled corticosteroid therapy, patients may experience systemic corticosteroid withdrawal symptoms, such as joint pain, allergic reactions, or skin reactions. Specific treatment should be initiated if such reactions occur.
Generalized glucocorticoid insufficiency should be suspected if symptoms such as fatigue, headache, nausea, and vomiting occur, and temporary increase in oral glucocorticoid dose may be necessary.
To minimize the risk of oral thrush (see section 4.8), patients should be instructed to rinse their mouths with water after inhalation of the maintenance dose.
Concomitant use of itraconazole, ritonavir, or other potent CYP3A inhibitors should be avoided (see section 4.5). If this is not possible, the time interval between administration of the inhibitor and budesonide should be as long as possible.
Bufomix Easyhaler should be used with caution in patients with thyrotoxicosis, phaeochromocytoma, diabetes, untreated hypokalemia, hypertrophic obstructive cardiomyopathy, idiopathic subvalvular aortic stenosis, severe hypertension, aneurysm, or other severe cardiovascular disorders, such as coronary heart disease, tachyarrhythmia, or severe heart failure.
Care should be exercised when treating patients with a prolonged QTc interval.
Formoterol may induce prolongation of the QTc interval.
The need for and dose of inhaled corticosteroids should be reassessed in patients with active or quiescent tuberculosis, fungal, or viral infections of the airways.
High doses of β2-agonists may lead to severe hypokalemia. Concomitant treatment with β2-agonists and drugs that may cause hypokalemia or enhance hypokalemic effects, such as xanthine derivatives, steroids, and diuretics, may increase the risk of hypokalemia.
Particular care should be exercised in unstable angina, and caution should be exercised in patients with tachyarrhythmia or severe heart failure, as the risk may be increased due to hypoxia and other conditions that may predispose to hypokalemia.
As with all β2-agonists, blood potassium levels should be monitored in patients with diabetes.
Pneumonia in patients with COPD
An increased risk of pneumonia has been observed in patients with COPD receiving inhaled corticosteroids, including an increased risk of pneumonia requiring hospitalization. There is some evidence of an increased risk of pneumonia with increasing corticosteroid dose, but this has not been consistently demonstrated across all studies.
There are no clear differences in the risk of pneumonia between inhaled corticosteroid products.
Physicians should be alert to the possibility of pneumonia in patients with COPD, as the clinical features of such infections and exacerbations of COPD frequently overlap.
Risk factors for pneumonia in patients with COPD include current smoking, older age, low body mass index (BMI), and severe COPD.
Bufomix Easyhaler contains approximately 8 mg of lactose per inhalation. This amount does not usually cause problems in lactose-intolerant individuals. The excipient, lactose, contains small amounts of milk proteins, which may cause an allergic reaction.
Children and adolescents
Regular growth monitoring should be performed in children receiving long-term treatment with inhaled corticosteroids. If growth is slowed, the treatment should be reviewed, with the aim of reducing the dose of inhaled corticosteroid to the lowest dose that maintains effective control of asthma. The benefits and risks of corticosteroid treatment should be considered, as well as the potential growth retardation. Referral to a pediatric pulmonologist should be considered.
Limited long-term data suggest that most children and adolescents treated with inhaled budesonide will achieve their adult height. However, an initial, small, and temporary reduction in growth (about 1 cm) has been observed. This usually occurs within the first year of treatment.
4.5 Interaction with Other Medicinal Products and Other Forms of Interaction
Pharmacokinetic interactions
Potent CYP3A inhibitors (e.g., ketoconazole, itraconazole, voriconazole, posaconazole, clarithromycin, telithromycin, nefazodone, cobicistat, and HIV protease inhibitors) may significantly increase budesonide plasma levels and should be avoided. If this is not possible, the time interval between administration of the inhibitor and budesonide should be as long as possible (see section 4.4).
The potent CYP3A4 inhibitor ketoconazole, at a daily dose of 200 mg, increased the plasma levels of orally administered budesonide (single dose of 3 mg) on average six-fold. When ketoconazole was administered 12 hours after budesonide, the plasma levels increased on average three-fold, indicating that separation of the administration times may reduce the plasma levels.
Limited data on this type of interaction at high doses of budesonide indicate that significant increases in plasma levels (on average four-fold) may occur when itraconazole (200 mg once daily) is administered concomitantly with inhaled budesonide (single dose of 1,000 μg).
Concomitant administration of CYP3A inhibitors, including cobicistat-containing products, is expected to increase the risk of systemic corticosteroid side effects. Co-administration is contraindicated unless the benefits outweigh the increased risk of systemic corticosteroid side effects; in such cases, patients should be monitored for systemic corticosteroid side effects.
Pharmacodynamic interactions
β-blockers may weaken or abolish the effect of formoterol. Therefore, Bufomix Easyhaler should not be administered concomitantly with β-blockers (including eye drops), unless strictly necessary.
Concomitant treatment with quinidine, disopyramide, procainamide, phenothiazine derivatives, antihistamines (terfenadine), and tricyclic antidepressants may lead to an increased risk of ventricular arrhythmias.
L-dopa, L-thyroxine, oxytocin, and alcohol may impair cardiac tolerance to β-sympathomimetics.
Concomitant treatment with monoamine oxidase inhibitors, including furazolidone and procarbazine, may precipitate hypertensive crises.
There is an increased risk of arrhythmias in patients receiving concomitant anesthesia with halogenated hydrocarbons.
Concomitant use of other β2-agonists and anticholinergic drugs may have an additive bronchodilator effect.
Hypokalemia may increase the risk of arrhythmias in patients treated with digitalis glycosides.
Hypokalemia may be the result of treatment with β2-agonists and may be potentiated by concomitant treatment with xanthine derivatives, corticosteroids, and diuretics (see section 4.4).
No interactions have been observed between budesonide and formoterol and other drugs used in the treatment of asthma.
Children and adolescents
Interaction studies have only been performed in adults.
4.6 Fertility, Pregnancy, and Lactation
Pregnancy
There are no clinical data on the use of Bufomix Easyhaler during pregnancy or on the concomitant use of formoterol and budesonide. Data from an embryo-foetal development study in rats do not indicate any teratogenic effect of the combination.
There are no adequate data on the use of formoterol in pregnant women. In animal studies, formoterol has shown effects on reproductive function at very high systemic exposure (see section 5.3).
Data from approximately 2,000 pregnancies exposed to inhaled budesonide do not indicate an increased risk of teratogenic effects. In animal studies, glucocorticosteroids have been shown to induce malformations (see section 5.3). This is unlikely to be relevant for humans using recommended doses.
Animal studies have also identified an increased risk of pre-natal growth retardation, cardiovascular effects in adults, and changes in glucocorticosteroid receptor density, neurotransmitter turnover, and behaviour at exposures below the teratogenic dose range.
Bufomix Easyhaler should only be used during pregnancy if the benefits to the mother outweigh the potential risks to the fetus. The lowest effective dose of budesonide should be used to maintain asthma control.
Breast-feeding
Budesonide and its metabolites are excreted in human milk. However, at therapeutic doses of Bufomix Easyhaler, no effects on the suckling child are anticipated. It is not known whether formoterol and its metabolites are excreted in human milk. In rats, small amounts of formoterol have been detected in maternal milk. A decision must be made whether to discontinue breast-feeding or to discontinue Bufomix Easyhaler, taking into account the benefit of breast-feeding for the child and the benefit of therapy for the woman.
Fertility
There are no data on the effects of budesonide on fertility. Animal studies on formoterol have shown a small but statistically significant reduction in fertility in male rats at high systemic exposure (see section 5.3).
4.7 Effects on Ability to Drive and Use Machines
Bufomix Easyhaler has no or negligible influence on the ability to drive and use machines.
4.8 Undesirable Effects
Since Bufomix Easyhaler contains budesonide and formoterol, the same undesirable effects as reported for these substances may occur. No increased incidence of undesirable effects has been seen when the two active substances were used together compared to when each active substance was used separately.
The most common undesirable effects reported in patients treated with formoterol are pharmacologically predictable and dose-related, such as tremor and palpitations. These are usually mild and decrease within a few days of treatment.
Undesirable effects that have been associated with budesonide or formoterol are listed below, classified according to system organ class and frequency. Frequencies are defined as: very common (≥ 1/10); common (≥ 1/100 to <1>
| System organ class | Frequency | Undesirable effects |
| Infections and infestations | Common | Oral thrush, pneumonia (in patients with COPD) |
| Immune system disorders | Rare | Immediate or delayed hypersensitivity reactions, including anaphylaxis, angioedema, rash, urticaria, pruritus, and dermatitis |
| Endocrine disorders | Very rare | Cushing's syndrome, Cushingoid features, adrenal suppression, growth retardation in children and adolescents, decreased bone mineral density, cataracts, and glaucoma |
| Metabolism and nutrition disorders | Rare | Hypokalemia |
| Psychiatric disorders | Uncommon | Aggression, psychomotor hyperactivity, anxiety, sleep disturbances |
| Nervous system disorders | Common | Headache, tremor |
| Eye disorders | Uncommon | Blurred vision (see also section 4.4) |
| Cardiac disorders | Common | Palpitations |
| Vascular disorders | Very rare | Fluctuations in blood pressure |
| Respiratory, thoracic, and mediastinal disorders | Common | Mild throat irritation, cough, hoarseness |
| Gastrointestinal disorders | Uncommon | Nausea |
| Skin and subcutaneous tissue disorders | Uncommon | Bruising |
| Musculoskeletal and connective tissue disorders | Uncommon | Muscle cramps |
Oral thrush occurs due to the deposition of the drug. The risk can be minimized by advising the patient to rinse their mouth with water after each maintenance dose.
Oral thrush usually responds to topical antifungal treatment without the need to discontinue inhaled corticosteroid therapy. If oral thrush occurs, patients should also rinse their mouths with water after reliever inhalations.
As with all inhaled therapies, paradoxical bronchospasm may occur, which can lead to immediate worsening of wheezing and shortness of breath after inhalation. If paradoxical bronchospasm occurs, treatment with Bufomix Easyhaler should be discontinued immediately, the patient should be reviewed, and, if necessary, alternative treatment should be initiated. Paradoxical bronchospasm responds to a short-acting inhaled bronchodilator (see section 4.4).
Inhaled corticosteroids may cause systemic effects, particularly at high doses for prolonged periods. The risk of systemic effects is less with inhaled corticosteroids than with oral corticosteroids. Possible systemic effects include Cushing's syndrome, Cushingoid features, adrenal suppression, growth retardation in children and adolescents, decreased bone mineral density, cataracts, and glaucoma, as well as a range of psychological and behavioral effects.
These effects are dependent on the dose, duration of exposure, and individual susceptibility, as well as the concomitant use of other corticosteroids, including oral corticosteroids.
Treatment with β2-agonists may lead to an increase in blood levels of insulin, free fatty acids, glycerol, and ketone bodies.
Children and adolescents
Regular growth monitoring should be performed in children receiving long-term treatment with inhaled corticosteroids (see section 4.4).
Reporting of suspected adverse reactions
After authorization of the medicinal product, it is important to continue to collect data on suspected adverse reactions. Healthcare professionals are asked to report any suspected adverse reactions via the national reporting system.
4.9 Overdose
Overdose of formoterol may lead to exaggerated β2-agonist effects, such as tremors, headache, and palpitations. Symptoms reported in individual cases included tachycardia, hypoglycemia, hypokalemia, prolonged QTc interval, arrhythmia, nausea, and vomiting. Treatment should be symptomatic and supportive. A dose of 90 micrograms, administered over three hours in patients with acute airway obstruction, did not raise any safety concerns.
Acute overdose of budesonide, even at very high doses, is unlikely to cause clinical problems. However, with chronic use of very high doses, systemic glucocorticosteroid effects, such as Cushing's syndrome and adrenal suppression, may occur.
If treatment with Bufomix Easyhaler is to be discontinued due to overdose of formoterol, consideration should be given to providing adequate corticosteroid cover.
5. PHARMACOLOGICAL PROPERTIES
5.1 Pharmacodynamic Properties
Pharmacotherapeutic group: Drugs for obstructive airway diseases, adrenergics in combination with corticosteroids or other drugs, excluding anticholinergics.
ATC code: R03AK07
Mechanism of action and pharmacodynamic effects
Bufomix Easyhaler contains formoterol and budesonide, which have different mechanisms of action and show an additive effect in terms of bronchodilation. The mechanisms of action of both substances are described below.
Budesonide
Budesonide is a glucocorticosteroid that, when administered by inhalation, has a dose-dependent anti-inflammatory effect in the airways, leading to a reduction in symptoms and exacerbations of asthma. Inhaled budesonide causes fewer severe side effects than systemic corticosteroids. The exact mechanism responsible for the anti-inflammatory effect of glucocorticosteroids is not known.
Formoterol
Formoterol is a selective β2-agonist that, when administered by inhalation, leads to rapid and long-lasting bronchodilation in patients with reversible airway obstruction. The bronchodilatory effect is dose-dependent, with an onset of action within 1-3 minutes. After a single dose, the effect lasts for at least 12 hours.
Clinical efficacy and safety
Asthma
Clinical studies in adults have shown that the addition of formoterol to budesonide improves asthma symptoms and lung function and reduces exacerbations. In two 12-week studies, the effect of budesonide and formoterol on lung function was similar to that seen with budesonide and formoterol administered separately and was greater than that seen with budesonide alone. All treatment groups used short-acting β2-agonists as needed. No attenuation of the anti-asthmatic effect was seen over time.
Two 12-week pediatric studies were conducted in 265 children aged 6-11 years treated with a maintenance dose of budesonide and formoterol (2 inhalations (80 micrograms + 4.5 micrograms)/inhalation dose, twice daily) and short-acting β2-agonists as needed. In both studies, lung function improved, and treatment was well tolerated compared to a comparable dose of budesonide alone.
5.2 Pharmacokinetic Properties
Absorption
It has been shown that the medicinal products Bufomix Easyhaler and Symbicort Turbuhaler, which contain a fixed dose of budesonide and formoterol, are bioequivalent in terms of total systemic exposure and pulmonary exposure.
It has been shown that the medicinal product Symbicort Turbuhaler, which contains a fixed dose of budesonide and formoterol, and the respective individual products are bioequivalent in terms of systemic exposure, respectively to budesonide and formoterol. However, a slight increase in cortisol suppression was observed after administration of the fixed-dose combination product compared to the individual products. This difference is not considered to affect clinical safety.
No evidence of pharmacokinetic interactions between budesonide and formoterol was found.
The pharmacokinetic parameters for these substances were comparable after administration of budesonide and formoterol in the form of individual products and a fixed-dose combination product. In the case of budesonide, the AUC value was slightly higher, the absorption rate was more rapid, and the maximum serum concentration was higher after administration of the fixed-dose combination product. In the case of formoterol, the maximum serum concentration was comparable after administration of the fixed-dose combination product. Budesonide, when administered by inhalation, is rapidly absorbed, and the maximum serum concentration is reached within 30 minutes after inhalation. In studies, the average lung deposition of budesonide after inhalation from a dry powder inhaler ranged from 32% to 44% of the delivered dose.
The systemic bioavailability is approximately 49% of the delivered dose. In children aged 6-16 years, lung deposition is within the range observed in adults after administration of the same dose. The serum concentrations achieved have not been determined.
Formoterol, when administered by inhalation, is rapidly absorbed, and the maximum serum concentration is reached within 10 minutes after inhalation. In studies, the average lung deposition of formoterol after inhalation from a dry powder inhaler ranged from 28% to 49% of the delivered dose.
The systemic bioavailability is approximately 61% of the delivered dose.
Distribution and Metabolism
The binding to plasma proteins is approximately 50% for formoterol and 90% for budesonide. The volume of distribution is approximately 4 l/kg for formoterol and 3 l/kg for budesonide. Formoterol is inactivated by conjugation reactions (active O-demethylated and deformylated metabolites are formed, which are considered inactive conjugates).
Budesonide undergoes extensive (about 90%) biotransformation during the first pass through the liver to metabolites with low inherent glucocorticosteroid activity.
The glucocorticosteroid activity of the main metabolites, 6-beta-hydroxy-budesonide and 16-alpha-hydroxy-prednisolone, is less than 1% of the activity of budesonide. No signs of metabolic interactions or displacement reactions between formoterol and budesonide were observed.
Elimination
Most of the formoterol dose undergoes transformation through liver metabolism, followed by elimination through the kidneys. After inhalation, 8% to 13% of the delivered formoterol dose is excreted in the urine as unchanged formoterol. Formoterol is characterized by high systemic clearance (about 1.4 l/min), and the terminal elimination half-life is 17 hours.
Budesonide is eliminated through metabolism catalyzed mainly by the CYP3A4 enzyme.
Budesonide metabolites are eliminated in the urine as such or in conjugated form. Only insignificant amounts of unchanged budesonide are detected in the urine. Budesonide is characterized by high systemic clearance (about 1.2 l/min), and the terminal elimination half-life after intravenous administration is 4 hours.
The pharmacokinetics of budesonide and formoterol in children and patients with renal impairment are unknown.
Exposure to budesonide and formoterol may be increased in patients with liver disease.
Linearity or Non-Linearity
The systemic exposure of both budesonide and formoterol is linearly correlated with the administered dose.
5.3 Preclinical Safety Data
Toxicity observed in animal studies concerning budesonide and formoterol, administered simultaneously or as monotherapy, consisted of effects related to increased pharmacological activity.
In reproductive studies in animals, it was shown that corticosteroids, such as budesonide, cause developmental abnormalities (cleft palate, skeletal abnormalities). However, the results of animal studies seem to be of no significance in humans after administration of recommended doses. Studies on the effect of formoterol on reproduction in animals showed a slight reduction in fertility in male rats at high systemic exposure and problems with implantation, as well as reduced postnatal survival and birth weight at exposures significantly higher than those achieved during clinical use. However, the results of animal studies seem to be of no significance in humans.
6. PHARMACEUTICAL PARTICULARS
6.1 List of Excipients
Lactose monohydrate (which contains milk proteins).
6.2 Incompatibilities
None.
6.3 Shelf Life
In the packaging intended for sale: 2 years.
After the first opening of the laminated bag: 4 months. Do not store above 25°C. Protect from moisture.
6.4 Special Precautions for Storage
No special recommendations for storing the medicinal product.
Storage conditions for the medicinal product after the first opening, see section 6.3.
6.5 Nature and Contents of Container
A multi-dose dry powder inhaler consisting of seven plastic components and a spring made of stainless steel. The plastics used to manufacture the inhaler are: polybutylene terephthalate, LDPE, polycarbonate, styrene-butadiene copolymer, polypropylene. The inhaler is sealed in a laminated bag and packaged with or without protective packaging (polypropylene and thermoplastic elastomer) in a cardboard box.
Packaging:
Bufomix Easyhaler, (320 micrograms + 9 micrograms)/inhalation dose, powder for inhalation:
- 1 inhaler of 60 doses
- 1 inhaler of 60 doses, with protective packaging
- 2 inhalers of 60 doses
- 3 inhalers of 60 doses
Not all pack sizes may be marketed.
6.6 Special Precautions for Disposal
No special requirements.
7. MARKETING AUTHORISATION HOLDER
RESPONSIBLE FOR BATCH RELEASE
Orion Corporation
Orionintie 1
FI-02200 Espoo
Finland
8. MARKETING AUTHORISATION NUMBER
Marketing authorisation number: 21850
9. DATE OF FIRST AUTHORISATION
AND RENEWAL DATE
Date of first authorisation: 09 May 2014
Date of last renewal: 16 April 2020
10. DATE OF REVISION OF THE TEXT
OF THE SUMMARY OF PRODUCT CHARACTERISTICS
- 21.10.2022
- Country of registration
- Active substance
- Prescription requiredYes
- Manufacturer
- ImporterOrion Corporation
- This information is for reference only and does not constitute medical advice. Always consult a licensed doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to Bufomix EasihalerDosage form: Powder, (160 mcg + 4.5 mcg)/inh. doseActive substance: formoterol and budesonidePrescription requiredDosage form: Powder, (320 mcg + 9 mcg)/inh. doseActive substance: formoterol and budesonideManufacturer: Aeropharm GmbH Lek farmacevtska družba d.d. (Lek Pharmaceuticals d.d.) Salutas Pharma GmbHPrescription requiredDosage form: Powder, (160 mcg + 4.5 mcg)/inh. doseActive substance: formoterol and budesonideManufacturer: Orion CorporationPrescription required
Alternatives to Bufomix Easihaler in other countries
The best alternatives with the same active ingredient and therapeutic effect.
Alternative to Bufomix Easihaler in Ucrania
Alternative to Bufomix Easihaler in España
Online doctors for Bufomix Easihaler
Discuss dosage, side effects, interactions, contraindications, and prescription renewal for Bufomix Easihaler – subject to medical assessment and local rules.















