
GESDINE 0.075 mg/0.02 mg TABLETS

How to use GESDINE 0.075 mg/0.02 mg TABLETS
Translated with AI
This page provides general information and does not replace a doctor’s consultation. Always consult a doctor before taking any medication. Seek urgent medical care if symptoms are severe.
Show originalContents of the leaflet
Introduction
Package Leaflet: Information for the User
Gesdine0.075 mg/0.02 mgEFG tablets
Gestodene / Ethinylestradiol
Important things you should know about combined hormonal contraceptives (CHCs):
- They are one of the most reliable reversible contraceptive methods if used correctly.
- They slightly increase the risk of having a blood clot in the veins and arteries, especially in the first year or when restarting the use of a combined hormonal contraceptive after a break of 4 weeks or more.
- Be alert and consult your doctor if you think you may have symptoms of a blood clot (see section 2 "Blood clots").
Read the entire package leaflet carefully before starting to take this medication, as it contains important information for you.
-Keep this package leaflet, as you may need to read it again.
-If you have any questions, consult your doctor, family planning nurse, or pharmacist.
-This medication has been prescribed to you only, and you should not give it to others even if they have the same symptoms as you, as it may harm them.
-If you experience side effects, consult your doctor or pharmacist, even if they are side effects not listed in this package leaflet. See section 4.
Contents of the package leaflet
- What is Gesdine and what is it used for
- What you need to know before starting to take Gesdine
- How to take Gesdine
- Possible side effects
- Storage of Gesdine
- Package contents and additional information
1. What is Gesdine and what is it used for
- Gesdine is a contraceptive pill used to prevent pregnancy.
- Each tablet contains a small amount of two different female hormones, called gestodene and ethinylestradiol.
- Contraceptive pills like Gesdine that contain two hormones are called "combined" contraceptives.
2. What you need to know before starting to take Gesdine 20
General comments
Before starting to use Gesdine, you should read the information about blood clots in section 2. It is particularly important that you read the symptoms of a blood clot (see section 2 "Blood clots").
Before starting to take Gesdine, your doctor will ask you some questions about your personal and family medical history. The doctor will also measure your blood pressure, and depending on your personal situation, may carry out some other tests. This leaflet describes several situations in which you should stop using Gesdine, or in which the reliability of Gesdine may be decreased. In such situations, you should not have sexual intercourse or should take additional non-hormonal contraceptive precautions, for example, use a condom or another barrier method. Do not use the rhythm or temperature method. These methods may not be reliable since Gesdine alters the monthly changes in body temperature and cervical mucus.
Gesdine, like other hormonal contraceptives, does not protect against HIV infection (AIDS) or any other sexually transmitted disease.
Do not take Gesdine
You should not use Gesdine if you have any of the conditions listed below. Inform your doctor if you have any of the conditions listed below. Your doctor will discuss with you what other form of contraception would be more suitable.
- If you have (or have ever had) a blood clot in a blood vessel of the legs (deep vein thrombosis, DVT), in the lungs (pulmonary embolism, PE) or in other organs.
- If you know you have a disorder that affects blood clotting: for example, protein C deficiency, protein S deficiency, antithrombin III deficiency, factor V Leiden or antiphospholipid antibodies.
- If you need an operation or if you spend a long time sitting or lying down (see section "Blood clots").
- If you have ever had a heart attack or a stroke.
- If you have (or have ever had) angina pectoris (a condition that causes severe chest pain and may be the first sign of a heart attack) or a transient ischemic attack (TIA, temporary stroke symptoms).
- If you have any of the following diseases that may increase your risk of forming blood clots in the arteries:
- Severe diabetes with blood vessel damage.
- Very high blood pressure.
- Very high levels of fat in the blood (cholesterol or triglycerides).
- A condition called hyperhomocysteinemia.
- If you have (or have ever had) a type of migraine called "migraine with aura".
- If you have (or have ever had) inflammation of the pancreas (pancreatitis).
- If you have (or have ever had) a liver disease and your liver function has not yet returned to normal.
- If you have liver tumors.
- If you have (or have ever had), or if you suspect you have breast cancer or cancer of the genitals.
- If you have vaginal bleeding of unknown cause.
- If you are pregnant or think you may be pregnant.
- If you are allergic to ethinylestradiol or gestodene, or to any of the other components of this medicine (listed in section 6). This may cause itching, rash, or inflammation.
- If you have hepatitis C and are taking medicines that contain ombitasvir/paritaprevir/ritonavir and dasabuvir or glecaprevir/pibrentasvir or sofosbuvir/velpatasvir/voxilaprevir (see also section "Using Gesdine with other medicines").
Warnings and precautions
Consult your doctor, pharmacist, or nurse before starting to take Gesdine.
When should you consult your doctor? Seek urgent medical attention
To get a description of the symptoms of these serious side effects, see "How to recognize a blood clot". |
Tell your doctor if you suffer from any of the following conditions.
If the condition develops or worsens while you are using Gesdine, you should also tell your doctor.
- If you have Crohn's disease or ulcerative colitis (chronic inflammatory bowel disease).
- If you have systemic lupus erythematosus (SLE, a disease that affects your natural defense system).
- If you have hemolytic uremic syndrome (HUS: a blood clotting disorder that causes kidney failure).
- If you have sickle cell anemia (an inherited disease of the red blood cells);
- If you have high levels of fat in the blood (hypertriglyceridemia) or a known family history of this condition. Hypertriglyceridemia has been associated with an increased risk of developing pancreatitis (inflammation of the pancreas).
- If you need an operation or spend a long time sitting or lying down (see section 2 "Blood clots").
- If you have just given birth, you are at a higher risk of blood clots. You should ask your doctor when you can start taking Gesdine after giving birth.
- If you have inflammation of the veins just under the skin (superficial thrombophlebitis).
- If you have varicose veins.
- If any of your close relatives have had breast cancer.
- If you have any liver or gallbladder disease.
- If you have diabetes.
- If you have depression.
- If you have epilepsy (see section "Taking Gesdine with other medicines").
- If you have a disease that first appeared during pregnancy or during previous use of sex hormones (e.g., loss of hearing, a blood disease called porphyria, blistering rash during pregnancy (herpes gestationis), a nervous disease in which involuntary movements appear (Sydenham's chorea)).
- If you have or have ever had chloasma (brownish patches on the skin, especially on the face, known as "pregnancy patches"). In this case, you should avoid direct exposure to the sun or ultraviolet rays.
- If you experience symptoms of angioedema such as swelling of the face, tongue, and/or throat and/or difficulty swallowing or urticaria with difficulty breathing, contact a doctor immediately. Products containing estrogens may cause or worsen the symptoms of hereditary and acquired angioedema.
BLOOD CLOTS
The use of a combined hormonal contraceptive like Gesdine increases your risk of having a blood clot compared to not using it. In rare cases, a blood clot can block blood vessels and cause serious problems.
Blood clots can form:
- In the veins (this is called "venous thrombosis", "venous thromboembolism" or VTE).
- In the arteries (this is called "arterial thrombosis", "arterial thromboembolism" or ATE).
Recovery from blood clots is not always complete. In rare cases, there can be serious long-term effects or, very rarely, they can be fatal.
It is important to remember that the overall risk of a harmful blood clot due toGesdineis small.
HOW TO RECOGNIZE A BLOOD CLOT
Seek urgent medical attention if you notice any of the following signs or symptoms.
Are you experiencing any of these signs? | What might you be suffering from? |
| Deep vein thrombosis |
If you are unsure, consult a doctor, as some of these symptoms, such as cough or shortness of breath, can be confused with a milder condition such as a respiratory infection (e.g., a "common cold"). | Pulmonary embolism |
Symptoms that occur more frequently in one eye:
| Retinal vein thrombosis (blood clot in the eye). |
| Heart attack |
Sometimes the symptoms of a stroke can be brief, with almost immediate and complete recovery, but you should still seek urgent medical attention, as you may be at risk of having another stroke. | Stroke |
| Blood clots that block other blood vessels. |
BLOOD CLOTS IN A VEIN
What can happen if a blood clot forms in a vein?
- The use of combined hormonal contraceptives has been associated with an increased risk of blood clots in the veins (venous thrombosis). However, these side effects are rare. They occur more frequently in the first year of use of a combined hormonal contraceptive.
- If a blood clot forms in a vein in the leg or foot, it can cause deep vein thrombosis (DVT).
- If a blood clot moves from the leg and lodges in the lung, it can cause a pulmonary embolism.
- In very rare cases, a blood clot can form in a vein in another organ, such as the eye (retinal vein thrombosis).
When is the risk of a blood clot in a vein higher?
The risk of a blood clot in a vein is higher during the first year you take a combined hormonal contraceptive for the first time. The risk may also be higher if you start taking a combined hormonal contraceptive (the same medicine or a different one) after a break of 4 weeks or more.
After the first year, the risk decreases, but it is always slightly higher than if you were not taking a combined hormonal contraceptive.
When you stop taking Gesdine, your risk of a blood clot returns to normal within a few weeks.
What is the risk of a blood clot?
The risk depends on your natural risk of VTE and the type of combined hormonal contraceptive you are taking.
The overall risk of a blood clot in the leg or lung (DVT or PE) with Gesdine is small.
- Out of 10,000 women who do not use a combined hormonal contraceptive and are not pregnant, about 2 will have a blood clot in a year.
- Out of 10,000 women who use a combined hormonal contraceptive that contains levonorgestrel, norethisterone, or norgestimate, about 5-7 will have a blood clot in a year.
- Out of 10,000 women who use a combined hormonal contraceptive that contains gestodene, such as Gesdine, about 9-12 will have a blood clot in a year.
- The risk of a blood clot will depend on your personal history (see "Factors that increase your risk of a blood clot" below).
Risk of a blood clot in a year | |
Women who do not usea combined hormonal contraceptive pill/patch/ring and who are not pregnant. | About 2 out of 10,000 women |
Women who use a combined hormonal contraceptive pill that contains levonorgestrel, norethisterone, or norgestimate. | About 5-7 out of 10,000 women |
Women who use Gesdine | About 9-12 out of 10,000 women |
Factors that increase your risk of a blood clot in a vein
The risk of a blood clot with Gesdine is small, but some conditions increase the risk. Your risk is higher:
- If you are overweight (body mass index or BMI over 30 kg/m2).
- If any of your close relatives have had a blood clot in the leg, lung, or other organ at a young age (i.e., before the age of about 50). In this case, you may have an inherited blood clotting disorder.
- If you need an operation or spend a long time sitting or lying down due to an injury or illness, or if you have your leg in a cast. You may need to stop using Gesdine several weeks before the operation or while you have reduced mobility. If you need to stop using Gesdine, ask your doctor when you can start using it again.
- As you get older (especially above about 35 years).
- If you have just given birth.
The risk of a blood clot increases the more conditions you have.
Long-distance air travel (more than 4 hours) may temporarily increase the risk of a blood clot, especially if you have any of the other risk factors listed.
It is important to tell your doctor if you suffer from any of the conditions above, even if you are not sure. Your doctor may decide that you should stop using Gesdine.
If any of the conditions above change while you are using Gesdine, for example, a close relative experiences a blood clot without a known cause or you gain a lot of weight, tell your doctor.
BLOOD CLOTS IN AN ARTERY
What can happen if a blood clot forms in an artery?
Like a blood clot in a vein, a blood clot in an artery can cause serious problems. For example, it can cause a heart attack or a stroke.
Factors that increase your risk of a blood clot in an artery
It is important to note that the risk of a heart attack or stroke due to using Gesdine is very small, but it can increase:
- With age (above about 35 years).
- If you smoke.When using a combined hormonal contraceptive like Gesdine, you are advised to stop smoking. If you are unable to stop smoking and are over 35 years old, your doctor may advise you to use a different type of contraceptive.
- If you are overweight.
- If you have high blood pressure.
- If any of your close relatives have had a heart attack or stroke at a young age (less than about 50 years). In this case, you may also be at higher risk of having a heart attack or stroke.
- If you or any of your close relatives have high levels of fat in the blood (cholesterol or triglycerides).
- If you have migraines, especially migraines with aura.
- If you have a heart condition (valvular disorder, heart rhythm disturbance called atrial fibrillation).
- If you have diabetes.
If you have one or more of these conditions or if any of them are particularly severe, the risk of a blood clot may be increased even further.
If any of the conditions above change while you are using Gesdine, for example, you start smoking, a close relative experiences a blood clot without a known cause, or you gain a lot of weight, tell your doctor.
Gesdine and cancer
Breast cancer has been slightly more common in women who use combined contraceptives, but it is not known if this is due to the treatment. For example, it may be that more tumors are detected in women who take combined contraceptives because they are examined by a doctor more often. The incidence of breast tumors decreases gradually after stopping combined hormonal contraceptives. It is important to have your breasts checked regularly and you should see your doctor if you notice any lump.
In rare cases, benign liver tumors, and even more rarely, liver cancers, have been reported in users of hormonal contraceptives. This can cause internal bleeding that leads to severe abdominal pain.
See your doctor if you experience unusual severe abdominal pain. You may need to stop taking Gesdine.
Cases of cervical cancer that occur more frequently in women who use hormonal contraceptives for a long time have been reported. This finding may not be caused by hormonal contraceptives but may be related to sexual behavior or other factors.
Psychiatric disorders
Some women who use hormonal contraceptives like Gesdine have reported depression or a depressed mood. Depression can be severe and sometimes can lead to suicidal thoughts. If you experience mood changes and depressive symptoms, contact your doctor for further medical advice as soon as possible.
Bleeding between periods
During the first few months that you are taking Gesdine, you may have unexpected bleeding (bleeding outside of the withdrawal bleed week). If this bleeding persists for more than a few months, or starts after a few months,
3. How to take Gesdine
Follow exactly the administration instructions of this medication indicated by your doctor or pharmacist. In case of doubt, consult your doctor or pharmacist again.
Take one Gesdine tablet every day, with some water if necessary. You can take the tablets with or without food, but every day at approximately the same time.
The pack (blister) contains 21 tablets. Next to each tablet is printed the day of the week on which it should be taken. If, for example, you start on a Wednesday, take a tablet with "WED" next to it. Follow the direction of the arrow on the pack until you have taken all 21 tablets.
After that, you should not take any tablets for 7 days. During these 7 days when you do not take tablets (called the rest week), you should have your period. The period, which can also be called withdrawal bleeding.
On the 8th day after taking the last tablet (i.e., after the 7-day rest period), you should start with the next pack, even if you have not yet finished your period. This means you should start each pack on the same day of the week, and your period should take place during the same days every month.
If you use Gesdine in this way, you are also protected against pregnancy during the 7 days when you do not take any tablets.
When can you start with the first pack?
- If you have not taken any hormonal contraceptive in the previous month.
Start taking Gesdine on the first day of your cycle (i.e., the first day of your period). If you start Gesdine on the first day of your period, you are immediately protected against pregnancy. You can also start on days 2-5 of your cycle, but you must use additional contraceptive methods (e.g., a condom) during the first 7 days.
- Switching from a combined hormonal contraceptive, combined vaginal ring, or patch.
You can start taking Gesdine the day after the rest week of your previous contraceptive (or after taking the last inactive tablet of your previous contraceptive). When switching from a combined vaginal ring or patch, follow your doctor's recommendations.
- Switching from a progestogen-only method (progestogen-only pill, injection, implant, or intrauterine device (IUD)).
You can switch at any time, from an injectable on the day corresponding to the next injection, from a progestogen-only pill, an implant, or an IUD, on the day of its removal; but in all cases, use additional contraceptive measures (e.g., a condom) during the first 7 days of tablet-taking.
•After an abortion.
Follow your doctor's recommendations.
- After having a child.
You can start taking Gesdine between 21 and 28 days after having a child. If you start later, use a barrier method (e.g., a condom) during the first 7 days of using Gesdine.
If, after having a child, you have already had sexual intercourse before starting to take Gesdine again, you must be sure you are not pregnant or wait for your next menstrual period.
Ask your doctor if you are unsure when to start taking Gesdine.
If you are breastfeeding and want to start taking Gesdine again after having a child.
Gesdine should not be used during breastfeeding. Read the section "2. Pregnancy and breastfeeding".
If you take more Gesdine than you should
No cases have been reported in which an overdose of Gesdine has caused serious harm.
The symptoms that may appear if you take many tablets at once are nausea, dizziness, abdominal pain, drowsiness/fatigue, or vomiting. Adolescent girls may experience vaginal bleeding.
If you have taken too many Gesdine tablets, or discover that a child has taken them, consult your doctor or pharmacist.
If you forget to take Gesdine
- If you are less than 12 hourslate in taking a tablet, your protection against pregnancy will not decrease. Take the tablet as soon as you remember and the following tablets at the usual time.
- If you are more than 12 hourslate in taking a tablet, your protection against pregnancy may be reduced. The more tablets you have missed, the higher the risk that your protection against pregnancy has decreased.
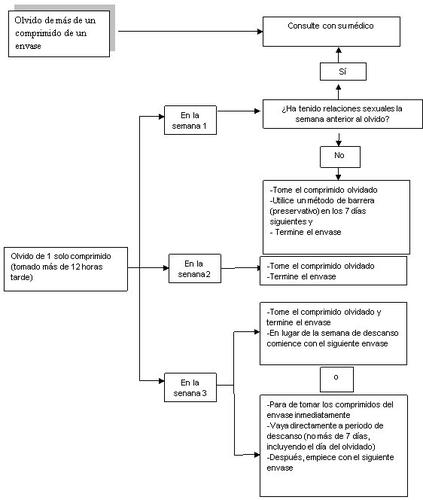
The risk of incomplete protection against pregnancy is highest if you miss a tablet at the beginning or end of the pack. Therefore, you should follow these recommendations (see also the following diagram):
- If you missed more than one tablet in this pack
Consult your doctor.
- If you missed a tablet in week 1
Take the missed tablet as soon as you remember, even if it means taking two tablets at the same time. Continue taking the tablets at the usual time and use additional precautions, for example, condoms, during the next 7 days. If you have had sexual intercourse in the week before missing the tablet or have missed starting a new pack after the rest week, you should consider the risk of pregnancy. In that case, consult your doctor.
- If you missed a tablet in week 2
Take the missed tablet as soon as you remember, even if it means taking two tablets at the same time. Continue taking the tablets at the usual time. Your protection against pregnancy will not decrease, and you do not need to take additional precautions.
•If you missed a tablet in week 3
You can choose between two options:
- Take the missed tablet as soon as you remember, even if it means taking two tablets at the same time. Continue taking the tablets at the usual time. Instead of starting the rest week, start the next pack.
You will probably have your period at the end of the second pack, although you may experience light bleeding or spotting during the second pack.
- You can also stop taking tablets and go directly to the rest week (noting the day you missed the tablet). If you want to start a new pack on the day you always start, your rest week should last less than 7 days.
If you follow one of these two recommendations, you will remain protected against pregnancy.
- If you have missed taking a tablet and do not have a period during the first rest week, you may be pregnant. You should contact your doctor before starting with the next pack.
Advice in case of gastrointestinal disorders
In case of severe gastrointestinal disorders (e.g., vomiting or diarrhea), absorption may not be complete, and you should take additional contraceptive measures. If you vomit within 3-4 hours after taking a tablet or have severe diarrhea, the situation is similar to if you missed a tablet. After vomiting or diarrhea, you should take another tablet from a reserve pack as soon as possible. If possible, take it within 12 hoursof when you would normally have taken the tablet. If this is not possible or more than 12 hours have passed, you should follow the advice given in the section "If you forget to take Gesdine”.
Delay of your menstrual period: what you should know
Although it is not recommended, delaying your menstrual period (withdrawal bleeding) is possible. You can do this by starting directly with a new pack of Gesdine instead of taking the rest week after the first pack. You may experience spotting (drops or spots of blood) or breakthrough bleeding while using the second pack. After the usual 7-day rest week, continue withthe next pack.
You should ask your doctor for advice before deciding to delay your menstrual period.
Changing the first day of your menstrual period: what you should know
If you take the tablets according to the instructions, your menstrual period will begin during the rest week. If you need to change the day, reduce the number of rest days (but never increase them, 7 at most!). For example, if your rest days start on a Friday and you want to change to a Tuesday (3 days earlier), start a new pack 3 days earlier than usual. If you make the rest week very short (e.g., 3 days or less), you may not have bleeding during these days. Then you may experience spotting (drops or spots of blood) or breakthrough bleeding.
If you are unsure how to proceed, consult your doctor.
If you stop treatment with Gesdine
You can stop taking Gesdine whenever you want. If you do not want to become pregnant, consult your doctor about other effective methods of birth control.
If you have any additional doubts about the use of this product, consult your doctor or pharmacist.
4. Possible side effects
Like all medications, Gesdine can cause side effects, although not everyone will experience them. If you experience any side effect, especially if it is severe and persistent, or have any change in health that you think may be due to Gesdine, consult your doctor.
All women who take combined hormonal contraceptives are at a higher risk of developing blood clots in the veins (venous thromboembolism (VTE)) or blood clots in the arteries (arterial thromboembolism (ATE)). For more detailed information on the different risks of taking combined hormonal contraceptives, see section 2 "What you need to know before you start using Gesdine".
- Harmful blood clots in a vein or artery, for example:
- In a leg or foot (i.e., DVT).
- In a lung (i.e., PE).
- Heart attack.
- Stroke.
- Mild stroke or temporary symptoms similar to those of a stroke, called a transient ischemic attack (TIA).
- Blood clots in the liver, stomach/intestine, kidneys, and eye.
The chances of having a blood clot can be higher if you have any other condition that increases this risk (see section 2 for more information on conditions that increase the risk of blood clots and symptoms of a blood clot).
Contact a doctor immediately if you experience any of the following symptoms of angioedema: swelling of the face, tongue, and/or throat, and/or difficulty swallowing or urticaria potentially with difficulty breathing (see also the section "Warnings and precautions").
The following list of side effects has been associated with the use of Gesdine:
- Frequent(may affect up to 1 in 10 women):
- headache,
- nervousness,
- intolerance to contact lenses,
- visual disturbances,
- nausea,
- acne,
- migraine,
- weight gain,
- fluid retention,
- during the first few months of use, sometimes bleeding or spotting between periods may occur, but this stops once your body has adjusted to Gesdine. If this continues, worsens, or starts again, contact your doctor,
- absence of menstruation,
- breast pain,
- decreased interest in sex,
- depressive mood,
- irritability.
- Uncommon(may affect up to 1 in 100 women):
- excess lipids in the blood,
- vomiting,
- hypertension.
- Rare(may affect up to 1 in 1,000 women):
- liver disease,
- skin and subcutaneous tissue disorders (lupus erythematosus),
- middle ear disorders,
- gallstones,
- thrombosis (the formation of a blood clot in the blood vessels),
- pigmentation disorders, which can occur even if you have been using Gesdine for several months. This can be reduced by avoiding excessive sun exposure.
- changes in vaginal discharge.
- Very rare(may affect up to 1 in 10,000 women):
- movement disorders,
- pancreatic disease.
Reporting side effects
If you experience any side effects, consult your doctor or pharmacist, even if they are not listed in this leaflet. You can also report them directly through the Spanish Pharmacovigilance System for Human Use Medicines: https://www.notificaram.es *By reporting side effects, you can help provide more information on the safety of this medication.
5. Storage of Gesdine
Keep this medication out of the sight and reach of children.
Do not use this medication after the expiration date stated on the pack and carton after the phrase "Do not use after:" or "EXP:". The expiration date is the last day of the month indicated.
Do not store above 30°C. Keep the pack in the outer packaging to protect it from light.
Medicines should not be disposed of via wastewater or household waste. Return packs and any unused medication to a pharmacy for proper disposal. By doing so, you will help protect the environment.
6. Packaging Content and Additional Information
Gesdine Composition
The active ingredients are gestodene and ethinylestradiol.
- Each tablet contains 0.075 mg of gestodene and 0.02 mg of ethinylestradiol.
- The other components are: lactose, microcrystalline cellulose, povidone K-30, magnesium stearate, and potassium polacrylate.
Product Appearance and Packaging Content
Gesdine tablets are round, white, with a diameter of approximately 5.7 mm and marked with a "C" on one side and "34" on the other.
Gesdine is available in boxes of 1, 3, and 6 blisters, each with 21 tablets.
Marketing Authorization Holder
Exeltis Healthcare S.L.
Av.Miralcampo 7, Poligono Ind.Miralcampo, 19200,
Azuqueca de Henares. Guadalajara
Spain
Manufacturer
Laboratorios León Farma, S.A.
C/ La Vallina s/n PI Navatejera
Villaquilambre (León), Spain
This product is marketed in other countries under the following names:
- Netherlands: Marynarka 0.075 mg /0.020 mg tablets
- Czech Republic: Lusienne 0.075 mg/ 0.020 mg tablets
- Slovakia: Marynarka 0.075 mg /0.020 mg tablets
- Romania: Marynarka 0.075 mg/ 0.020 mg tablets
- Poland: Axonella PL
- Spain: Gesdine 0.075 mg / 0.020 mg tablets EFG
Date of the Last Revision of this Leaflet:12/2022
Detailed and updated information on this medication is available on the website of the Spanish Agency for Medicines and Health Products (AEMPS) http://www.aemps.gob.es
- Country of registration
- Active substance
- Prescription requiredYes
- Manufacturer
- This information is for reference only and does not constitute medical advice. Always consult a doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to GESDINE 0.075 mg/0.02 mg TABLETSDosage form: TABLET, 75/20 µg/µgActive substance: gestodene and ethinylestradiolManufacturer: Laboratorios Effik S.A.Prescription requiredDosage form: TABLET, 0.075 mg gestodene; 0.03 ethinylestradiolActive substance: gestodene and ethinylestradiolManufacturer: Bayer Hispania S.L.Prescription requiredDosage form: TABLET, 0.020 mg Ethinylestradiol/0.075 mg GestodeneActive substance: gestodene and ethinylestradiolManufacturer: Wyeth Farma S.A.Prescription required
Online doctors for GESDINE 0.075 mg/0.02 mg TABLETS
Discuss questions about GESDINE 0.075 mg/0.02 mg TABLETS, including use, safety considerations and prescription review, subject to medical assessment and local regulations.
Frequently Asked Questions






