VICTOZA 6 mg/ml SOLUTION FOR INJECTION IN PRE-FILLED PEN


How to use VICTOZA 6 mg/ml SOLUTION FOR INJECTION IN PRE-FILLED PEN
Translated with AI
This page provides general information and does not replace a doctor’s consultation. Always consult a doctor before taking any medication. Seek urgent medical care if symptoms are severe.
Show originalContents of the leaflet
Introduction
Package Leaflet: Information for the User
Victoza 6mg/ml solution for injection in pre-filled pen
liraglutide
Read all of this leaflet carefully before you start using this medicine, because it contains important information for you.
- Keep this leaflet, as you may need to read it again.
- If you have any further questions, ask your doctor, pharmacist, or nurse.
- This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their symptoms are the same as yours.
- If you get any side effects, talk to your doctor, pharmacist, or nurse. This includes any possible side effects not listed in this leaflet. See section 4.
Contents of the pack
- What is Victoza and what is it used for
- What you need to know before you use Victoza
- How to use Victoza
- Possible side effects
- Storing Victoza
- Contents of the pack and other information
1. What is Victoza and what is it used for
Victoza contains the active substance liraglutide. It helps your body to reduce your blood sugar level only when your blood sugar level is too high. Additionally, it slows down the movement of food from your stomach and may help to prevent a heart disease.
Victoza is used on its own if your blood sugar level is not controlled adequately by diet and exercise alone, and you cannot use metformin (another diabetes medicine).
Victoza is used together with other diabetes medicines, when these are not enough to control your blood sugar level. These may include:
- oral anti-diabetics (such as metformin, pioglitazone, sulphonylurea, sodium-glucose co-transporter-2 (SGLT2) inhibitor) and/or insulin.
2. What you need to know before you use Victoza
Do not use Victoza
- if you are allergic to liraglutide or any of the other ingredients of this medicine (listed in section 6).
Warnings and precautions
Talk to your doctor, pharmacist, or nurse:
- before you start using Victoza.
- if you have or have had pancreatitis.
If you know that you are going to have a surgical operation where you will be under anaesthesia (put to sleep), tell your doctor that you are taking Victoza.
This medicine must not be used if you have type 1 diabetes (your body does not produce any insulin) or diabetic ketoacidosis (a complication of diabetes with high blood sugar and increased breathing rate). It is not an insulin and must not be used as a substitute for insulin.
Victoza must not be used if you are on dialysis.
Victoza must not be used if you have severe liver disease.
The use of Victoza is not recommended if you have severe heart failure.
This medicine must not be used if you have a severe stomach or gut problem that causes a delay in emptying of the stomach (called gastroparesis), or inflammatory bowel disease.
If you get symptoms of acute pancreatitis, such as severe and persistent stomach pain, you should contact your doctor immediately (see section 4).
If you have thyroid disease, including thyroid nodules and increased size of the thyroid gland, talk to your doctor.
In some cases, when starting treatment with Victoza, you may experience dehydration (loss of fluids), for example, if you have vomiting, nausea, and diarrhoea. It is important to avoid dehydration by drinking plenty of fluids. Talk to your doctor if you have any questions.
Children and adolescents
Victoza can be used in adolescents and children from 10 years of age. There is no experience in children under 10 years of age.
Other medicines and Victoza
Tell your doctor, pharmacist, or nurse if you are using, have recently used, or might use any other medicines.
In particular, tell your doctor, pharmacist, or nurse if you are using medicines that contain any of the following active substances:
- Sulphonylurea (such as glimepiride or glibenclamida) or insulin. You may get low blood sugar (hypoglycaemia) when you use Victoza with a sulphonylurea or insulin, because sulphonylureas and insulin increase the risk of hypoglycaemia. When you start using these medicines together for the first time, your doctor may tell you to reduce the dose of sulphonylurea or insulin. For warning signs of low blood sugar, see section 4. If you are also taking a sulphonylurea (such as glimepiride or glibenclamida) or insulin, your doctor may ask you to have your blood sugar levels checked. This will help your doctor to decide if the dose of sulphonylurea or insulin needs to be changed.
- If you are taking insulin, your doctor will tell you how to reduce your insulin dose and will recommend that you check your blood sugar level more often to avoid high blood sugar (hyperglycaemia) and diabetic ketoacidosis (a complication of diabetes that occurs when the body cannot break down glucose because there is not enough insulin).
- Warfarin or other anticoagulant medicines. You may need to have more frequent blood tests to check how well your blood can clot.
Pregnancy and breast-feeding
Tell your doctor if you are pregnant, think you may be pregnant, or are planning to have a baby. Victoza must not be used during pregnancy because it is not known if it could harm the baby.
It is not known if Victoza passes into breast milk. Therefore, do not use this medicine during breast-feeding.
Driving and using machines
Low blood sugar (hypoglycaemia) may reduce your ability to concentrate. Avoid driving or using machines if you get symptoms of hypoglycaemia. See section 4 for warning signs of low blood sugar. Talk to your doctor for further information.
Important information about some of the ingredients of Victoza
This medicine contains less than 1 mmol sodium (23 mg) per dose, i.e., essentially “sodium-free”.
3. How to use Victoza
Follow the instructions for administration of this medicine exactly as told by your doctor. If you are not sure, ask your doctor, pharmacist, or nurse again.
- The initial dose is 0.6 mg once a day for at least one week.
- Your doctor will tell you when to increase the dose to 1.2 mg once a day.
- Your doctor may tell you to further increase the dose to 1.8 mg once a day if your blood sugar is not adequately controlled on a dose of 1.2 mg.
Do not change the dose unless your doctor tells you to.
Victoza is given as an injection under the skin (subcutaneously). Do not inject into a vein or muscle. The best places to give the injection are the front of your thigh, the area around your navel, or the top of your arm. Change the injection site each day to reduce the risk of developing lumps under the skin.
The injection can be given at any time of day, independent of meals. Once you have decided on the best time of day for you, it is best to inject Victoza at about the same time every day.
Before using the pen for the first time, your doctor or nurse will show you how to use it.
On the other side of this leaflet, you will find detailed instructions on how to use the pen.
If you use more Victoza than you should
If you use more Victoza than you should, talk to a doctor immediately. You may need medical treatment. You may get nausea, vomiting, diarrhoea, or low blood sugar (hypoglycaemia). See the warning signs of low blood sugar in section 4.
If you forget to use Victoza
If you miss a dose, use Victoza as soon as you remember.
However, if it is more than 12 hours since you should have used Victoza, skip the missed dose. Give the next dose at the usual time on the next day.
Do not use a double dose or increase the dose on the next day to make up for the missed dose.
If you stop using Victoza
Do not stop using Victoza without talking to your doctor first. If you stop, your blood sugar levels may increase.
If you have any other questions on the use of this medicine, ask your doctor, pharmacist, or nurse.
4. Possible side effects
Like all medicines, this medicine can cause side effects, although not everybody gets them.
Serious side effects
Common: may affect up to 1 in 10 people
- Low blood sugar (hypoglycaemia). The warning signs of low blood sugar may come on suddenly and include: cold sweat, cool pale skin, headache, fast heartbeat, nausea, excessive hunger, vision changes, drowsiness, feeling of weakness, shakiness, anxiety, confusion, difficulty concentrating, and shivering. Your doctor will tell you how to treat low blood sugar and what to do if you notice these warning signs. This is more likely to happen if you are also using a sulphonylurea or insulin. Your doctor may reduce your dose of these medicines before you start using Victoza.
Rare: may affect up to 1 in 1,000 people
- A severe allergic reaction (anaphylactic reaction) with additional symptoms such as breathing difficulties, swelling of the throat and face, fast heartbeat, etc. If you notice any of these symptoms, seek medical help immediately and talk to your doctor as soon as possible.
- Intestinal obstruction. A severe form of constipation with additional symptoms such as stomach pain, bloating, vomiting, etc.
Very rare: may affect up to 1 in 10,000 people
- Cases of pancreatitis (inflammation of the pancreas). Pancreatitis can be a serious and potentially fatal disease. Stop using Victoza and contact your doctor immediately if you notice any of the following serious side effects:
- severe and persistent stomach pain (abdominal pain) that may radiate to your back, as well as nausea and vomiting, as it could be a sign of pancreatitis.
Other side effects
Very common: may affect more than 1 in 10 people
- Nausea. This side effect normally goes away with time.
- Diarrhoea. This side effect normally goes away with time.
Common
- Vomiting.
When starting treatment with Victoza, you may experience loss of fluids/dehydration in some cases. For example, if you have vomiting, nausea, and diarrhoea. It is important to avoid dehydration by drinking plenty of fluids.
- Headache
- Indigestion
- Inflamed stomach (gastritis). The symptoms include stomach pain, nausea, and vomiting.
- Gastroesophageal reflux disease (GERD). The symptoms include heartburn.
- Bloated or painful abdomen
- Abdominal discomfort
- Constipation
- Gas (flatulence)
- Decreased appetite
- Bronchitis
- Common cold
- Dizziness
- Fast heartbeat
- Fatigue
- Toothache
- Injection site reactions (bruising, pain, irritation, itching, and rash).
- Increased pancreatic enzymes (such as lipase and amylase).
Uncommon: may affect up to 1 in 100 people
- Allergic reactions such as itching (pruritus) and hives (urticaria)
- Dehydration, sometimes with decreased kidney function
- Feeling unwell
- Gallstones
- Inflamed gallbladder
- Change in taste
- Delayed emptying of the stomach.
Frequency not known: cannot be estimated from the available data
- Lumps under the skin may occur due to the accumulation of a protein called amyloid (cutaneous amyloidosis; the frequency with which this occurs is not known).
Reporting of side effects
If you get any side effects, talk to your doctor, pharmacist, or nurse. This includes any possible side effects not listed in this leaflet. You can also report side effects directly via the national reporting system listed in Appendix V. By reporting side effects, you can help provide more information on the safety of this medicine.
5. Storing Victoza
Keep this medicine out of the sight and reach of children.
Do not use this medicine after the expiry date which is stated on the label and on the pen after EXP. The expiry date is the last day of the month stated.
Before use:
Store in a refrigerator (2°C - 8°C). Do not freeze. Keep away from the freezer.
During use:
You can store the pen for a maximum of 1 month at a temperature below 30°C or in a refrigerator (2°C - 8°C), away from the freezer. Do not freeze.
When not in use, store the pen with the cap on to protect it from light.
Do not use this medicine if you notice that the solution is not clear and colourless or almost colourless.
Medicines should not be disposed of via wastewater or household waste. Ask your pharmacist how to dispose of medicines no longer required. These measures will help protect the environment.
6. Container Contents and Additional Information
Composition of Victoza
- The active substance is liraglutide. 1 ml of injectable solution contains 6 mg of liraglutide. A pre-filled pen contains 18 mg of liraglutide.
- The other components are disodium phosphate dihydrate, propylene glycol, phenol, and water for injectable preparations.
Appearance of the Product and Container Contents
Victoza is supplied as a clear and colorless or almost colorless injectable solution in a pre-filled pen. Each pen contains 3 ml of solution, which can deliver 30 doses of 0.6 mg, 15 doses of 1.2 mg, or 10 doses of 1.8 mg.
Victoza is available in packs of 1, 2, 3, 5, or 10 pens. Not all pack sizes may be marketed.
Needles are not included.
Marketing Authorization Holder and Manufacturer
Novo Nordisk A/S
Novo Allé
DK-2880 Bagsværd
Denmark
Date of Last Revision of this Leaflet:
Other Sources of Information
Detailed information on this medicine is available on the European Medicines Agency website: http://www.ema.europa.eu
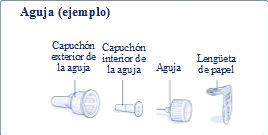
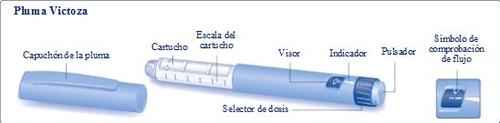
INSTRUCTIONS FOR USE OF THE VICTOZA PEN Read these instructions carefully before using your pen. Your pen contains 18 mg of liraglutide. You can select doses of 0.6 mg, 1.2 mg, and 1.8 mg. The pen is designed to be used with NovoFine or NovoTwist disposable injection needles up to 8 mm in length and as thin as 32 G (0.25/0.23 mm). |
|
| |
Preparing the Pen Check the name and color of the labelon your pen to ensure it contains liraglutide. Using the wrong medicine could harm you. Remove the pen cap. |
|
Remove the paper tab from a new disposable needle. Screw the needle straight and firmly onto the pen. |
|
Remove the outer needle cap and save it for later. |
|
Remove the inner needle cap and discard it. |
|
Always use a new needle for each injection. This reduces the risk of contamination, infection, loss of liraglutide, needle blockage, and inaccurate dosing. Be careful not to bend or damage the needle. Never attempt to put the inner needle cap back on. You could stick yourself with the needle. | |
Maintenance of Your Pen
| |
Important Information
| |
Checking the Flow with Each New Pen Check the flow before the first injection with each new pen. If your pen is already in use, go to “Selecting Your Dose”, step H. Turn the dose selector until the indicator points to the flow check symbol. |
|
Hold the pen with the needle pointing upwards. Gently tap the cartridge with your finger several times. This will collect any air bubbles at the top of the cartridge. |
|
Hold the needle pointing upwards and press the injection button until the indicator points to 0 mg. A drop of liraglutide should appear at the tip of the needle. If no drop appears, repeat steps E to G up to four times. If still no drop of liraglutide appears, change the needle and repeat steps E to G once more. Do not use the pen if a drop of liraglutide still does not appear. This indicates that the pen is defective, and you should use a new one. |
|
If you drop the pen onto a hard surface or suspect it is not working correctly, always put a new disposable needle on and check the flow before using it. | |
Selecting Your Dose Always check that the indicator points to 0 mg. Turn the dose selector until the indicator points to the required dose (0.6 mg, 1.2 mg, or 1.8 mg). If you accidentally select the wrong dose, to change it, simply turn the dose selector backwards or forwards until the indicator points to the correct dose. Be careful not to press the injection button while turning the dose selector backwards, as liraglutide may be released. If the dose selector stops before the indicator points to the required dose, this means there is not enough liraglutide left for a full dose. In this case, you can: Divide your dose into two injections: Turn the dose selector in either direction until the indicator points to 0.6 mg or 1.2 mg. Inject the dose. Then prepare a new pen and inject the remaining number of mg to complete your dose. Only divide your dose between the current pen and a new pen if you have received proper training or advice from your healthcare provider. Use a calculator to plan your doses. If you divide your dose incorrectly, you may inject too much or too little liraglutide. Inject the full dose with a new pen: If the dose selector stops before the indicator points to 0.6 mg, prepare a new pen and inject the full dose with it. |
|
Do not attempt to select doses other than 0.6 mg, 1.2 mg, or 1.8 mg. The numbers on the window must be exactly aligned with the indicator to ensure you receive the correct dose. You will hear a click each time you turn the dose selector. Do not use these clicks to select your dose. Do not use the cartridge scale to measure the amount of liraglutide to be injected, as it is not precise enough. | |
Injecting Your Dose Insert the needle under the skin using the injection technique recommended by your doctor or nurse.Then follow these instructions: Press the injection button until the indicator points to 0 mg. Be careful not to touch the window with your other fingers or press the dose selector button while injecting, as this may block the injection. Keep the injection button pressed and leave the needle under the skin for at least 6 seconds. This ensures that the full dose is administered. |
|
Remove the needle. You may see a drop of liraglutide at the tip of the needle. This is normal and does not affect your dose. |
|
Insert the needle tip into the outer needle cap without touching the needle or the outer needle cap. |
|
When the needle is covered, carefully press the outer needle cap down until it clicks. Then unscrew the needle. Carefully dispose of the needle and replace the pen cap. When the pen is empty, carefully dispose of it without any needle attached. Please dispose of the pen and needle according to local regulations. |
|
Always remove the needle after each injection and store your pen without the needle attached. This reduces the risk of contamination, infection, loss of liraglutide, needle blockage, and inaccurate dosing. Healthcare providers must be careful when handling used needles to avoid accidental needlestick injuries and infections. |
- Country of registration
- Average pharmacy price114.72 EUR
- Active substance
- Prescription requiredYes
- Manufacturer
- This information is for reference only and does not constitute medical advice. Always consult a doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to VICTOZA 6 mg/ml SOLUTION FOR INJECTION IN PRE-FILLED PENDosage form: INJECTABLE, 6 mg/mlActive substance: liraglutideManufacturer: Sun Pharmaceutical Industries (Europe) B.V.Prescription requiredDosage form: INJECTABLE, 6 mg/mlActive substance: liraglutideManufacturer: Sun Pharmaceutical Industries (Europe) B.V.Prescription requiredDosage form: INJECTABLE, 6 mg/mlActive substance: liraglutideManufacturer: Zentiva K.S.Prescription required
Online doctors for VICTOZA 6 mg/ml SOLUTION FOR INJECTION IN PRE-FILLED PEN
Discuss questions about VICTOZA 6 mg/ml SOLUTION FOR INJECTION IN PRE-FILLED PEN, including use, safety considerations and prescription review, subject to medical assessment and local regulations.
Frequently Asked Questions