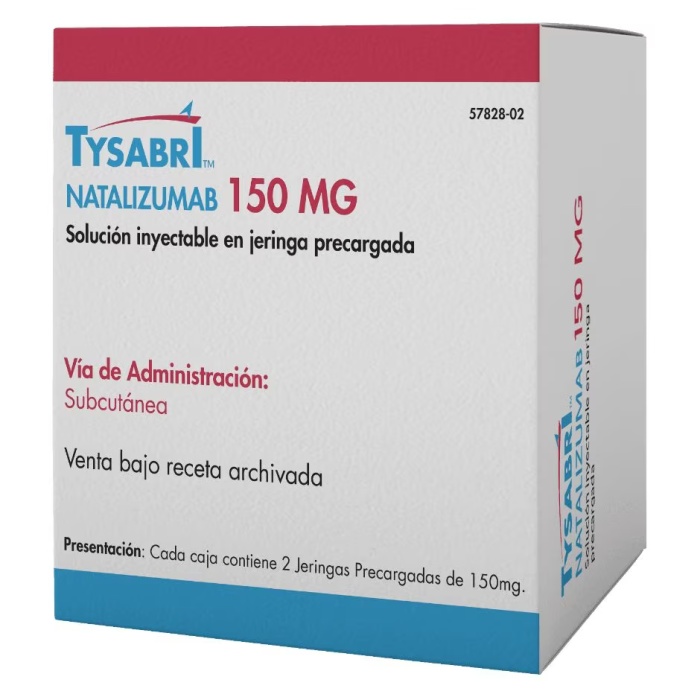
TYSABRI 150 mg Injectable Solution in Pre-filled Syringe

How to use TYSABRI 150 mg Injectable Solution in Pre-filled Syringe
Translated with AI
This page provides general information and does not replace a doctor’s consultation. Always consult a doctor before taking any medication. Seek urgent medical care if symptoms are severe.
Show originalContents of the leaflet
Introduction
Package Leaflet: Information for the Patient
Tysabri 150mg solution for injection in a pre-filled syringe
Natalizumab
Read all of this leaflet carefully before you start using this medicine because it contains important information for you.
In addition to this leaflet, you will be given a patient information card and, in case of self-administration or administration by a caregiver, a Pre-Treatment Checklist. These contain important safety information that you should be aware of before receiving and during treatment with Tysabri.
- Keep this leaflet and the patient information card, as you may need to read them again. Keep the leaflet and the patient information card with you during treatment and for six months after the last dose of this medicine, as side effects can occur even after treatment has been discontinued.
If you or your caregiver administer the treatment, review the Pre-Treatment Checklist before each dose.
- If you have any questions, ask your doctor.
- This medicine has been prescribed for you only, and you should not give it to others, even if they have the same symptoms as you, as it may harm them.
- If you experience side effects, consult your doctor, even if they are not listed in this leaflet. See section 4.
Contents of the package leaflet:
- What is Tysabri and what is it used for
- What you need to know before you start receiving Tysabri
- How Tysabri is administered
- Possible side effects
- Storage of Tysabri
- Contents of the pack and further information
1. What is Tysabri and what is it used for
TYSABRI is used to treat multiple sclerosis (MS). It contains the active substance natalizumab. It is what is called a monoclonal antibody.
MS causes inflammation in the brain that damages nerve cells. This inflammation occurs when white blood cells reach the brain and spinal cord. This medicine prevents white blood cells from reaching the brain. This reduces nerve damage caused by MS.
Symptoms of multiple sclerosis
The symptoms of MS can vary from patient to patient; you may experience some or none.
They can include: problems walking, tingling in the face, arms, or legs; vision problems; fatigue; feeling unsteady or dizzy; bladder and bowel problems; difficulty thinking and concentrating; depression; acute or chronic pain; sexual problems; muscle stiffness and spasms.
When symptoms worsen, it is called a relapse(also exacerbation or flare-up). When a relapse occurs, you may notice symptoms suddenly, within hours, or with a slow progression over several days. Symptoms usually improve gradually (this is called remission).
How Tysabri can help
In trials, this medicine reduced the increase in disability caused by MS by about half and reduced the number of MS relapses by about two-thirds. While you are being treated with this medicine, you may not notice any improvement, but it can continue to work to prevent MS from getting worse.
2. What you need to know before you start receiving Tysabri
Before starting treatment with this medicine, it is important that you and your doctor have discussed the benefits you can expect from this treatment and the risks associated with it.
Tysabri must not be administered to you
- If you are allergic to natalizumab or any of the other components of this medicine (listed in section 6).
- If you have been diagnosed with progressive multifocal leukoencephalopathy(PML). PML is a rare brain disease.
- If your immune systemhas a serious problem. This can be due to a disease (such as HIV infection) or medications you are using or have used in the past (see below).
- If you are taking medicines that affect the immune system, including certain medicines used to treat MS. These medicines cannot be used with Tysabri.
- If you have cancer(unless it is a type of skin cancer called basal cell carcinoma).
Warnings and precautions
Consult your doctorif Tysabri is the right treatment for you. Do this before starting to use this medicine and when you have been receiving it for more than two years.
Keep a record
In order to improve the traceability of this medicine, your doctor or pharmacist must record the name and batch number of the medicine that has been administered to you in your medical records. You can also write down these details in case you are asked for them in the future.
Possible brain infection (PML)
Some people who receive this medicine (less than 1 in 100) have had a rare brain infection called PML (progressive multifocal leukoencephalopathy). PML can cause severe disability or death.
- Before starting treatment, your doctor will perform a blood test on all patientsto detect JC virus infection. The JC virus is a common virus that normally does not make you sick. However, PML is associated with an increase in JC virus in the brain. The reason for this increase in some patients treated with Tysabri is not clear. Before and during treatment, your doctor will perform a blood test to check if you have antibodies against the JC virus (anti-JCV antibodies), which are a sign that you have been infected with the JC virus.
- Your doctor will perform an MRI scan, which will be repeated during treatment to rule out PML.
- Symptoms of PMLcan be similar to those of an MS relapse (see section 4, Possible side effects). You can also develop PML up to 6 months after stopping treatment with Tysabri.
Tell your doctor as soon as possibleif you notice that your MS is getting worse or if you notice any new symptoms while you are being treated with Tysabri or up to 6 months after.
- Tell your partner or caregiverswhat to look out for (see also section 4, Possible side effects). Some symptoms can be difficult to detect by yourself, such as changes in mood or behavior, confusion, speech and communication difficulties. If you experience any of these, you may need to have more tests. Be aware of symptoms during the 6 months after stopping Tysabri.
- Keep the patient information card that your doctor has given you. It includes this information. Show it to your partner or caregivers.
- If you or your caregiver administer the treatment, review the Pre-Treatment Checklist before each dose.
Three things can increase the risk of PMLwith Tysabri. If you have two or more of these risk factors, the risk increases even more:
- If you have anti-JCV antibodiesin your blood. They are a sign that the virus is in your body. You will be tested before and during treatment with Tysabri.
- If you are receiving long-term treatmentwith Tysabri, especially if it is for more than two years.
- If you have taken a medicine calledimmunosuppressant, which reduces the activity of the immune system.
The JC virus also causes another condition, called JCV granular cell neuronopathy (JCV GCN), which has occurred in some patients receiving this medicine. The symptoms of JCV GCN are similar to those of PML.
In the case of patients with a lower risk of PML, your doctor may repeat tests periodically to check:
- If you still do not have anti-JCV antibodies in your blood.
- If you have received treatment for more than 2 years, if you still have a lower level of anti-JCV antibodies in your blood.
If someone develops PML
PML can be treated and treatment with Tysabri will be discontinued. However, some people experience a reactionwhen Tysabri is removed from the body. This reaction (known as IRISor immune reconstitution inflammatory syndrome) can cause your condition to worsen, including a decline in brain function.
Be aware of other infections
Some infections other than PML can also be serious and can be caused by viruses, bacteria, and other causes.
Tell your doctor or nurse immediatelyif you think you have an infection (see also section 4, Possible side effects).
Changes in blood platelet count
Natalizumab can reduce the number of platelets in the blood, which are responsible for blood clotting. This can lead to a disorder called thrombocytopenia (see section 4) where your blood may not clot quickly enough to stop bleeding. This can cause bruising, as well as more serious problems such as excessive bleeding. Tell your doctor immediately if you experience unexplained bruising, red or purple spots on the skin (called petechiae), bleeding from cuts in the skin that do not stop or ooze, prolonged bleeding from the gums or nose, blood in the urine or stool, or bleeding in the white part of the eyes.
Children and adolescents
Do not give this medicine to children or adolescents under 18 years of age.
Other medicines and Tysabri
Tell your doctor if you are using, have recently used, or might use any other medicines.
- You must not be given this medicineif you are currently being treated with medicines that affect your immune system, such as certain medicines for the treatment of MS.
- You may not be able to use this medicine if you have everreceived a medicine that affects the immune system.
Pregnancy and breastfeeding
- Do not use this medicine if you are pregnant, unless you have discussed it with your doctor. If you are pregnant, think you may be pregnant, or plan to become pregnant, tell your doctor immediately.
- Do not breastfeed while using Tysabri.Your doctor will help you decide whether to stop breastfeeding or stop using the medicine.
If you are pregnant or breastfeeding, think you may be pregnant, or plan to become pregnant, consult your doctor before using this medicine. Your doctor will consider the risk to the baby and the benefit to the mother.
Driving and using machines
Dizziness is a very common side effect. If you experience this symptom, do not drive or use machines.
Tysabri contains sodium
This medicine contains less than 1 mmol of sodium (23 mg) per 300 mg dose; this is essentially “sodium-free”.
3. How Tysabri is administered
Tysabri injections will be prescribed by a doctor who has experience in treating MS. Your doctor may switch you directly from another MS medicine to Tysabri if there are no signs of problems caused by the previous treatment.
- Your doctor will request blood teststo detect anti-JCV antibodies and other possible problems.
- Your doctor will perform an MRI scan, which will be repeated during treatment.
- To switch from some MS medicines, your doctor may recommend that you wait for a certain period to ensure that most of the previous medicine has been eliminated from your body.
- If your condition allows, your doctor may discuss with you the option of receiving injections outside a hospital setting (e.g., at home). These injections can be administered by a healthcare professional, you, or a caregiver, provided you meet certain criteria. You will still need to attend the medical center or hospital for appointments, including those for periodic blood tests and MRI scans.
- If your doctor decides that you are suitable for self-administration (or administration by your caregiver), a healthcare professional will supervise you during the administration of the first two doses (2 injections each).
- The healthcare professional will give you or your caregiver detailed instructions and show you how to prepare and inject the medicine before using the syringes for the first time.
- If your doctor decides that you are suitable for self-administration or administration by your caregiver, make sure to read the patient information card to review the list of PML symptoms and to review the Pre-Treatment Checklist before each dose. If any symptoms appear or worsen, do not administer the dose and contact your doctor immediately.
- The recommended dose for adults is 300 mg every four weeks.
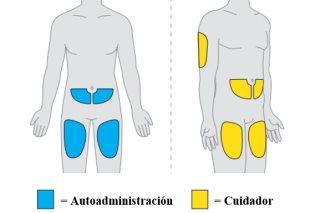
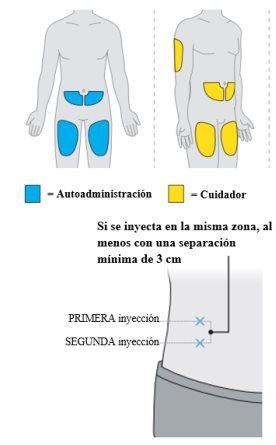
- Each dose is administered in two injectionsunder the skin, in the thigh, abdomen (at least 6 cm from the navel), or the back of the arm (only in the case of injection by a healthcare professional or caregiver). Administration takes up to 30 minutes.
- At the end of the package leaflet, information is provided on how to prepare and inject the medicine.
If you stop treatment with Tysabri
It is important to continue administering Tysabri, especially during the first months of treatment. It is important that you continue treatment while you and your doctor decide that it is helping you. Do not stop taking your medicine without your doctor's advice. Patients who received one or two doses of Tysabri and then took a break in treatment of 3 months or more had a higher chance of experiencing an allergic reaction when restarting treatment.
Checking for allergic reactions
Some patients have experienced an allergic reaction to this medicine. Your doctor will check for allergic reactions during and 1 hour after injections. In case of self-administration or administration by a caregiver, if you experience an allergic reaction, stop the injection and go to the doctor immediately. See also section 4, Possible side effects.
If you miss a dose of Tysabri
If you did not receive your usual dose of Tysabri, talk to your doctor to have it administered as soon as possible. After that, you can continue receiving Tysabri every 4 weeks.
It is necessary to administer two syringes to provide the full dose. It is important that both syringesare administered and that you follow the prescribed administration schedule. If you or your caregiver administer the injections and have missed a dose or have injected only one syringe, contact your doctor as soon as possible for guidance.
Will Tysabri always work?
In some patients who receive Tysabri, the body's natural defenses can prevent the medicine from working properly over time as the body produces antibodies against the medicine. Your doctor may decide if this medicine is not working properly for you based on your blood tests and will discontinue treatment if necessary.
If you have any further questions on the use of Tysabri, ask your doctor. Follow the instructions for administration of the medicine contained in this package leaflet or as directed by your doctor. In case of doubt, ask your doctor.
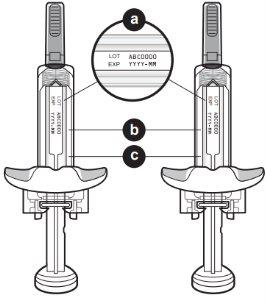
Subcutaneous is abbreviated as SC on the syringe label.
4. Possible Adverse Effects
Like all medicines, this medicine can cause adverse effects, although not all people suffer from them.
Tell your doctor or nurse immediatelyif you notice any of the following symptoms.
Signs of brain infection
- Changes in personality and behavior such as confusion, delirium, or loss of consciousness
- Seizures (epileptic attacks)
- Headache
- Nausea/vomiting
- Neck stiffness
- Extreme sensitivity to bright light
- Fever
- Rash (on any part of the body)
These symptoms may be due to a brain infection (encephalitis or PML) or the membrane that surrounds it (meningitis).
Signs of other serious infections
- Unexplained fever
- Severe diarrhea
- Shortness of breath
- Prolonged dizziness
- Headache
- Weight loss
- Lack of energy
- Visual disturbance
- Pain or redness of the eye(s)
Signs of allergic reaction
- Hives (itchy rash)
- Swelling of the face, lips, or tongue
- Difficulty breathing
- Chest pain or discomfort
- Increased or decreased blood pressure (your doctor or nurse will alert you if they are monitoring your blood pressure)
They are more likely to occur during or shortly after injection.
Signs of possible liver problems
- Yellowing of the skin or whites of the eyes
- Unusual darkening of urine
- Abnormal liver function test
If you experience any of the adverse effects described above or if you think you have an infection, consult your doctor or nurse immediately. Show your patient information cardand this leaflet to any doctor or nurse who treats you, not just your neurologist.
Other adverse effects
Very common(may affect more than 1 in 10 people)
- Urinary tract infection
- Sore throat and nasal congestion or secretion
- Headache
- Dizziness
- Feeling of discomfort (nausea)
- Joint pain
- Fatigue
Common(may affect up to 1 in 10 people)
- Anemia (reduced number of red blood cells that can make your skin pale and make you feel short of breath or lacking energy)
- Allergy (hypersensitivity)
- Chills
- Hives (itchy rash)
- Vomiting
- Fever
- Difficulty breathing (dyspnea)
- Redness of the face or body (flushing)
- Herpes virus infections
- Discomfort around the injection site. May include pain, bruising, redness, itching, or swelling
Uncommon(may affect up to 1 in 100 people)
- Severe allergy (anaphylactic reaction)
- Progressive multifocal leukoencephalopathy (PML)
- Inflammatory disorder after stopping the medicine
- Facial swelling
- Increased number of white blood cells (eosinophilia)
- Reduced number of platelets
- Easy bruising (purpura)
Rare(may affect up to 1 in 1000 people)
- Herpes virus infection in the eye
- Severe anemia (reduced number of red blood cells that can make your skin pale and make you feel short of breath or lacking energy)
- Severe swelling under the skin
- High levels of bilirubin in the blood (hyperbilirubinemia)that can cause symptoms such as yellowing of the eyes or skin, fever, and fatigue
Frequency not known(cannot be estimated from the available data)
- Rare brain and eye infections
- Liver damage
Tell your doctor as soon as possibleif you think you have an infection.
You will also find this information in the patient information card that your doctor has given you.
Reporting of adverse effects
If you experience any side effect, consult your doctor, even if it is a possible side effect not listed in this leaflet. You can also report them directly through the national reporting system included in Appendix V. By reporting side effects, you can help provide more information on the safety of this medicine.
5. Storage of TYSABRI
Keep this medicine out of the sight and reach of children.
Do not use this medicine after the expiry date that appears on the label and carton. The expiry date is the last day of the month indicated.
Store in a refrigerator (between 2 °C and 8 °C).
Do not freeze.
Keep the syringes in the outer packaging to protect them from light.
The pre-filled syringes can be stored at room temperature (up to 30 °C) for a maximum combined time of up to 24 hours, including the time needed to reach room temperature for administration. The syringes can be put back in the refrigerator and used before the expiry date indicated on the label and carton. The date and time the package is removed from the refrigerator should be noted on the carton. Discard the syringes if they are left out of the refrigerator for more than 24 hours. Do not use external heat sources, such as hot water, to warm the pre-filled syringes.
Do not use this medicine if you notice particles in the liquid or changes in the color of the liquid.
6. Container Contents and Additional Information
Tysabri Composition
The active ingredient is natalizumab.
Each 1 ml pre-filled syringe contains 150 mg of natalizumab.
The other components are:
Sodium monobasic phosphate monohydrate
Sodium dibasic phosphate heptahydrate
Sodium chloride (see section 2 "Tysabri contains sodium")
Polysorbate 80 (E 433)
Water for injectable preparations
Product Appearance and Container Contents
Tysabri is a colorless to slightly yellowish liquid and slightly opalescent to opalescent.
Each box contains two syringes.
Tysabri is available in packs containing 2 pre-filled syringes.
Marketing Authorization Holder and Manufacturer
Biogen Netherlands B.V.
Prins Mauritslaan 13
1171 LP Badhoevedorp
Netherlands
You can request more information about this medicine by contacting the local representative of the marketing authorization holder:
Belgium/Belgique/Belgien Biogen Belgium N.V./S.A. Tel: +32 2 219 12 18 | Lithuania Biogen Lithuania UAB Tel: +370 5 259 6176 |
| Luxembourg/Luxemburg Biogen Belgium N.V./S.A. Tel: +352 2 219 12 18 |
Czech Republic Biogen (Czech Republic) s.r.o. Tel: +420 255 706 200 | Hungary Biogen Hungary Kft. Tel: +36 (1) 899 9883 |
Denmark Biogen (Denmark) A/S Tel: +45 77 41 57 57 | Malta Pharma MT limited Tel: +356 213 37008/9 |
Germany Biogen GmbH Tel: +49 (0) 89 99 6170 | Netherlands Biogen Netherlands B.V. Tel: +31 20 542 2000 |
Estonia Biogen Estonia OÜ Tel: +372 618 9551 | Norway Biogen Norway AS Tel: +47 23 40 01 00 |
Greece Genesis Pharma SA Tel: +30 210 8771500 | Austria Biogen Austria GmbH Tel: +43 1 484 46 13 |
Spain Biogen Spain SL Tel: +34 91 310 7110 | Poland Biogen Poland Sp. z o.o. Tel: +48 22 351 51 00 |
France Biogen France SAS Tel: +33 (0)1 41 37 95 95 | Portugal Biogen Portugal Sociedade Farmacêutica Unipessoal, Lda Tel: +351 21 318 8450 |
Croatia Biogen Pharma d.o.o. Tel: +358 (0) 1 775 73 22 | Romania Johnson & Johnson Romania S.R.L. Tel: +40 21 207 18 00 |
Ireland Biogen Idec (Ireland) Ltd. Tel: +353 (0)1 463 7799 | Slovenia Biogen Pharma d.o.o. Tel: +386 1 511 02 90 |
Iceland Icepharma hf Tel: +354 540 8000 | Slovakia Biogen Slovakia s.r.o. Tel: +421 2 323 340 08 |
Italy Biogen Italia s.r.l. Tel: +39 02 584 9901 | Finland Biogen Finland Oy Tel: +358 207 401 200 |
Cyprus Genesis Pharma (Cyprus) Ltd Tel: +357 22 76 57 15 | Sweden Biogen Sweden AB Tel: +46 8 594 113 60 |
Latvia Biogen Latvia SIA Tel: +371 68 688 158 |
Date of Last Revision of this Leaflet:05/2025
Other Sources of Information
Detailed information on this medicine is available on the European Medicines Agency website: https://www.ema.europa.eu
--------------------------------------------------------------------------------------------------------------------
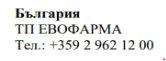
INSTRUCTIONS FOR USE
Tysabri 150 mg
injectable solution
natalizumab
subcutaneous injection
Full Dose = 2 pre-filled syringes
These "Instructions for Use" contain information on how to inject the medicine using the Tysabri pre-filled syringe.
Read these Instructions for Use before starting to use the Tysabri pre-filled syringe (referred to as "syringe" in these instructions) and each time you get a new pack. There may be new information.
This information does not replace consultation with your healthcare professional about your medical condition or treatment.
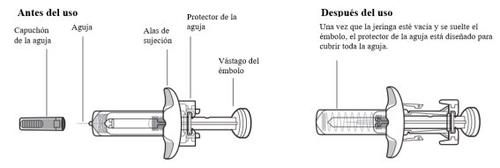
Parts of the Tysabri Device
Do not remove the wings. The wings will allow you to hold the syringe more firmly during the injection process.
Important Information to Know Before Injecting Tysabri
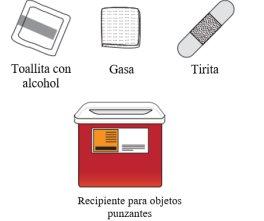
Tysabri is presented in a pre-filled syringe (referred to as "syringe" in these instructions). Each Tysabri box contains two syringes. You must use both syringes, within a maximum of 30 minutes between them, to get your full dose.
- In case of self-administration or administration by a caregiver, your healthcare professional should teach you or your caregiver how to prepare and inject the syringes before using them for the first time. If you or your caregiver administer the injections and have missed a dose or have injected only one syringe, contact your pharmacist or the doctor who treats you.
- The syringes are for subcutaneous injection (injecting directly into the fatty layer under the skin) only.
- Each syringe can only be used once (single use). They cannot be reused.
- Do not share the syringes with other people, even if they have the same disease as you. You could infect them or get an infection from them.
Note for Healthcare Professionals:
Patient supervisionis required during subcutaneous injections and for 1 hour afterto detect signs and symptoms of injection reactions, including hypersensitivity. After the first six doses of Tysabri, regardless of the route of administration, patients should be supervised after subcutaneous injection according to medical judgment.
Storage of Tysabri
- Keep the syringe and all medicines out of the sight and reach of children.
- Store the syringes in the refrigerator (between 2°C and 8°C).
- If necessary, the syringes can be stored at room temperature (up to 30°C) for up to 24 hours in total. If the syringes have been out of the refrigerator for more than 24 hours, do not use them.
- Keep the syringes in the original box to protect them from light.
- Do not freeze the syringes or expose them to temperatures above 30°C.
- The syringes can be put back in the refrigerator and used before the expiry date stated on the label and on the box.
Preparing the Tysabri Injection:
|
|
|
|
Do notuse external heat sources, such as warm water, to warm up the syringes. | |
|
|
|
|
Do notuse the syringe if it has passed the expiry date. | |
| |
Do notuse the syringe if it is damaged or cracked. | |
| |
Do notuse the syringe if the liquid has visible particles. Do notuse the syringe if it has been dropped before use. Inform your healthcare professional if you have any of these problems with the syringes. | |
You may see bubbles in the medicine. This is normal. Note:the appearance of the medicine may change after taking it out of the refrigerator. This is normal. | |
|
|
|
|
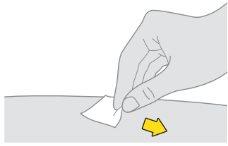
Do nottouch, fan, or blow on the cleaned area. |
Injecting the First Syringe
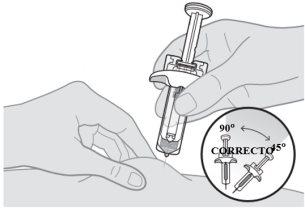
Note:you may see a drop of liquid on the tip of the needle. This is normal. |
|
| |
|
|
|
|
Make sure to push the plunger rod all the way down so that all the medicine is injected and the needle shield clicks into place. | |
|
|
If the needle shield does not activate to cover the needle, do notput the needle shield back on the syringe. Put it in the sharps container and contact your healthcare professional for help. | |
|
|
Injecting the Second Syringe
|
|
|
|
Do not touch, fan, or blow on the cleaned area. | |
Administer the injections one after the other without significant delay. The second injection should be administered no later than 30 minutes after the first. |
|
Disposal of Tysabri
|
|
Do not throw the sharps container or the used syringes in the household trash. | |
If you do not have a sharps container, you can ask your healthcare professional for one or you can use a household container that:
When the sharps container is almost full, you should follow your community guidelines for the proper way to dispose of it. There may be state or local laws about how to dispose of used syringes. Do not throw the used sharps container in the household trash unless your community guidelines permit it. Do not recycle the sharps container. |
- Country of registration
- Active substance
- Prescription requiredYes
- Manufacturer
- This information is for reference only and does not constitute medical advice. Always consult a doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to TYSABRI 150 mg Injectable Solution in Pre-filled SyringeDosage form: INJECTABLE PERFUSION, 300 mgActive substance: natalizumabManufacturer: Sandoz GmbhPrescription requiredDosage form: INJECTABLE PERFUSION, 20 mgActive substance: natalizumabManufacturer: Biogen Netherlands B.V.Prescription requiredDosage form: INJECTABLE PERFUSION, 120 mg (80 mg/kg) belimumabActive substance: belimumabManufacturer: Glaxosmithkline (Ireland) LimitedPrescription required
Online doctors for TYSABRI 150 mg Injectable Solution in Pre-filled Syringe
Discuss questions about TYSABRI 150 mg Injectable Solution in Pre-filled Syringe, including use, safety considerations and prescription review, subject to medical assessment and local regulations.
Frequently Asked Questions