
PACLITAXEL TEVA 6 mg/ml CONCENTRATE FOR INFUSION SOLUTION

How to use PACLITAXEL TEVA 6 mg/ml CONCENTRATE FOR INFUSION SOLUTION
Translated with AI
This page provides general information and does not replace a doctor’s consultation. Always consult a doctor before taking any medication. Seek urgent medical care if symptoms are severe.
Show originalContents of the leaflet
Introduction
Package Leaflet: Information for the User
Paclitaxel Teva 6mg/ml concentrate for solution for infusion EFG
Read all of this leaflet carefully before you start using this medicine because it contains important information for you.
- Keep this leaflet, you may need to read it again.
- If you have any further questions, ask your doctor or pharmacist.
- This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours.
- If you experience any side effects, talk to your doctor or pharmacist or nurse. This includes any possible side effects not listed in this leaflet. See section 4.
Contents of the pack
- What Paclitaxel Teva is and what it is used for.
- What you need to know before you use Paclitaxel Teva.
- How to use Paclitaxel Teva.
- Possible side effects.
- Storage of Paclitaxel Teva.
- Contents of the pack and other information
Paclitaxel Teva concentrate for solution for infusion is administered only by healthcare professionals, who can answer any questions you may have after reading this leaflet.
1. What Paclitaxel Teva is and what it is used for
Paclitaxel is an anti-neoplastic or anti-cancer medicine. It can interrupt the division and growth of cancer cells.
Paclitaxel Teva is used to treat different types of cancer, such as:
Ovarian carcinoma(inadvanced or metastatic ovarian carcinoma, residual disease >1 cmafter laparotomy)
Both as initial therapy in combination with platinum-containing medications, cisplatin, or as second-line treatment when platinum-containing treatments have failed.
Breast carcinoma(treatment of early breast cancer after surgical removal of the primary tumor, advanced or metastatic breast cancer)
In adjuvant treatment, after treatment with anthracycline and cyclophosphamide (AC treatment).
As initial treatment, either in combination with an anthracycline medication in patients for whom anthracycline treatment is indicated, or in combination with a medication called trastuzumab.
As monotherapy, in patients who have not responded to standard anthracycline treatments, or in whom such treatment should not be used.
Certain type oflung cancer(Non-small cell lung carcinoma)
In combination with cisplatin, in patients who are not candidates for potentially curative surgery and/or radiotherapy.
It is also used to treat a special form ofcancer related toAIDSthat develops in connective tissue (Kaposi's sarcoma)
When other treatments, such as liposomal anthracyclines, have failed
2. What you need to know before you use Paclitaxel Teva
Do not usePaclitaxel Teva:
- If you are allergic (hypersensitive) to paclitaxel or any of the other ingredients of this medicine (listed in section 6), especially macrogolglycerol ricinoleate.
- If you are breastfeeding.
- If your liver function is severely reduced.
- If your white blood cell count is too low (neutrophils). Your doctor will take blood samples to check this.
- If you have severe and uncontrolled recurrent infections, and you are being treated for Kaposi's sarcoma.
If you are in any of the above situations, talk to your doctor before starting treatment with paclitaxel.
Warnings and precautions:
Talk to your doctor or pharmacist before starting Paclitaxel Teva
- If you experience severe allergic reactions (e.g., difficulty breathing, shortness of breath, chest tightness, low blood pressure, dizziness, dizziness, skin reactions such as rash or inflammation).
- If you have a fever, severe chills, sore throat, or mouth ulcers (signs of bone marrow suppression); your doctor will take blood samples frequently to check this.
- If you have mouth sores or redness (signs of mucositis) and you are being treated for Kaposi's sarcoma. You may need a lower dose.
- If you have heart problems during treatment with paclitaxel; your doctor should check your heart function before starting the next treatment with paclitaxel.
- If you experience numbness or weakness in arms and legs (signs of peripheral neuropathy); a dose reduction of paclitaxel may be necessary.
- If you develop severe or persistent diarrhea, with fever and stomach pain, during or shortly after treatment with paclitaxel. Your colon may be inflamed (pseudomembranous colitis).
- If you have received previous radiotherapy in the chest (as it may increase the risk of pulmonary inflammation).
- If you experience heart problems during treatment with paclitaxel; your doctor must check your heart function before the next treatment with paclitaxel.
You will be given several different medications, belonging to the class of corticosteroids (e.g., dexamethasone), antihistamines (e.g., diphenhydramine or chlorphenamine), and H2 antagonists (e.g., cimetidine or ranitidine) before each treatment with paclitaxel. Premedication is necessary to reduce the risk of severe hypersensitivity reactions (see section 4. Possible side effects, uncommon).
Other medicines and Paclitaxel Teva
Tell your doctor if you are using, have recently used, or might use any other medicines, including those obtained without a prescription. This is because paclitaxel or the other medicine may not work as well as expected, or you may be more likely to experience a side effect.
- Interaction means that different medicines can influence each other. Consult your doctor when using paclitaxel at the same time as the following: medications for treating infections (i.e., antibiotics such as erythromycin, rifampicin, etc.: if in doubt about whether the medication you are taking is an antibiotic, ask your doctor, nurse, or pharmacist), and medications for treating fungal infections (e.g., ketoconazole)
- medications used to help stabilize mood, also called antidepressants (e.g., fluoxetine)
- medications used to treat seizure disorders (epilepsy) (e.g., carbamazepine, phenytoin)
- medications used to help reduce lipid levels in the blood (e.g., gemfibrozil)
- medications used for stomach acidity or stomach ulcers (e.g., cimetidine)
- medications used to treat HIV and AIDS (e.g., ritonavir, saquinavir, indinavir, nelfinavir, efavirenz, nevirapine)
- a medication called clopidogrel, used to prevent blood clot formation.
- a medication called rifampicin, an antibiotic used for tuberculosis. It may be necessary to increase the dose of paclitaxel.
- vaccines: if you have been vaccinated recently, or if you are planning to be vaccinated, inform your doctor. The use of paclitaxel with some vaccines may lead to serious complications.
- cisplatin (for cancer treatment): paclitaxel should be administered before cisplatin. It may be necessary to monitor your kidney function more frequently.
- doxorubicin (for cancer treatment): paclitaxel should be administered 24 hours after doxorubicin, to avoid high levels of doxorubicin in your body.
If you are treated with Paclitaxel Teva and doxorubicin or trastuzumab; your heart function should be monitored before and during treatment.
Pregnancy, breastfeeding, and fertility
If you are pregnant or breastfeeding, think you may be pregnant, or are planning to have a baby, ask your doctor or pharmacist for advice before using this medicine.
Paclitaxel should not be used during pregnancy, unless clearly necessary. Paclitaxel may cause fetal harm. Pregnancy should be avoided and effective contraceptives used during treatment. If you become pregnant, you should inform your doctor immediately. Female and male patients of childbearing potential, and/or their partners, should use effective contraceptives during and for at least 6 months after treatment with paclitaxel.
Male patients should seek advice on sperm preservation before treatment with paclitaxel due to the possibility of infertility.
Paclitaxel Teva should not be used during breastfeeding. You should interrupt breastfeeding during treatment with Paclitaxel Teva. Do not restart breastfeeding until your doctor advises you to do so.
Driving and using machines:
There is no reason why you should not drive between Paclitaxel Teva cycles, but you should remember that this medicine contains alcohol and it may be inadvisable to drive immediately after a treatment cycle. As with all cases, you should not drive or use machines if you feel dizzy or drowsy.
Consult your doctor, nurse, or pharmacist if you have any doubts.
Paclitaxel Teva contains alcohol and macrogolglycerol ricinoleate
A vial of paclitaxel contains 49.5% v/v (ethanol).
This medicine contains 2 g of alcohol (ethanol) in each 5 ml vial, 7 g in each 16.7 ml vial, 10 g in each 25 ml vial, and 20 g in each 50 ml vial, which is equivalent to 396 mg/ml concentrate. The amount in one ml of this medicine is equivalent to 10 mg of beer or 4 ml of wine.
The amount of alcohol in this medicine may affect your ability to drive and use machines because it can alter your judgment and reaction ability.
If you suffer from epilepsy or liver problems, consult your doctor or pharmacist before taking this medicine.
The amount of alcohol in this medicine may alter the effect of other medicines. Consult your doctor or pharmacist if you are taking other medicines.
If you are pregnant or breastfeeding, consult your doctor or pharmacist before taking this medicine. If you have an alcohol addiction, consult your doctor or pharmacist before taking this medicine.
Because this medicine is usually administered slowly over 3 or 24 hours, the effects of alcohol may be reduced.
Macrogolglycerol ricinoleate can cause severe allergic reactions.
3. How to use Paclitaxel Teva
To minimize the risk of allergic reactions, before starting treatment with paclitaxel, you will receive other medications. These medications may be administered orally, intravenously, or both.
Your doctor will determine the dose and number of doses to be administered. Paclitaxel Teva is administered under the supervision of a doctor, who can provide you with more information.
The amount (dose) of Paclitaxel Teva that you will receive will depend on your body surface area in square meters (m2). It is calculated from your height and weight. The dose you receive will also depend on the results of your blood tests. Depending on the type and severity of the cancer, you will receive Paclitaxel Teva alone or in combination with another anti-cancer agent (e.g., cisplatin, doxorubicin, trastuzumab). Paclitaxel Teva is administered intravenously by infusion over 3 or 24 hours. Normally, Paclitaxel Teva is administered every 3 weeks (2 weeks in patients with Kaposi's sarcoma), unless your doctor decides otherwise. Your doctor will inform you about the number of paclitaxel cycles you need to receive. The needle should remain in the vein while the medicine is being administered. If the needle comes out or is dislodged, or the solution spills into the tissue outside the vein (you may notice discomfort or pain), inform your doctor or nurse immediately.
Pediatric use
The use of Paclitaxel is not recommended in children and adolescents (under 18 years) due to the lack of safety and efficacy data.
If you receive more Paclitaxel Teva than you should
There is no known antidote for paclitaxel overdose, so you will receive treatment for the symptoms.
In case of overdose or accidental ingestion, consult your doctor or pharmacist immediately or call the Toxicology Information Service, phone 91 562 04 20, indicating the medicine and the amount administered.
If you have any further questions on the use of this medicine, ask your doctor or nurse.
4. Possible Adverse Effects
Like all medicines, this medicine can cause adverse effects, although not all people suffer from them.
Immediately report to your doctor if you notice any signs of an allergic reaction. You may experience one or more of the following signs:
- Redness (rubefaction).
- Skin reactions.
- Itching (pruritus).
- Chest tightness.
- Shortness of breath or difficulty breathing.
- Inflammation
All of these can be signs of serious adverse effects.
Inform your doctor immediately:
Very common (may affect more than 1 in 10 patients)
- Infection (mainly urinary tract infections and upper respiratory tract infections: inflammation of the nasal mucosa characterized by nasal congestion, sneezing, and secretion (rhinitis) and inflammation of the throat (pharyngitis) including herpes simplex, fungal infection of the mouth), with a fatal outcome in some cases
- Alteration of blood count due to bone marrow suppression (myelosuppression)
- Lack of platelets that produces bruising and bleeding tendency (thrombocytopenia)
- Lack of white blood cells that produces increased sensitivity to infections (severe leucopenia, severe neutropenia), anemia, bleeding
- Mild hypersensitivity reactions (mainly facial flushing and skin rash)
- Anorexia
- Neuropathies, mainly persistent numbness, tingling, or pain in hands and feet (all symptoms of peripheral neuropathy)*
- Insomnia
- Paresthesia
- Low blood pressure
- Nausea, vomiting, diarrhea
- Inflammation of the digestive mucosa (mucositis)
- Inflammation of the mouth mucosa (stomatitis), abdominal pain
- Hair loss (most cases of hair loss occurred within a month after starting treatment with paclitaxel. When it occurs, hair loss is pronounced (more than 50%) in most patients)
- Joint and muscle pain
- Pain
- Abnormal fluid accumulation in hands, feet, and face (edema)
*May persist for more than 6 months after discontinuation of paclitaxel treatment
Common: may affect up to 1 in 10 patients
- Cold-like syndrome
- Alteration in blood count (lack of white blood cells) with fever and increased sensitivity to infections (febrile neutropenia)
- Depression
- Severe form of neuropathy that produces mainly persistent numbness, tingling, or pain in hands and feet (peripheral neuropathy), nervousness, insomnia, abnormal thoughts, sense of perversion, abnormal gait, movement disorders (hypokinesia), decreased sense of touch (hypoesthesia)
- Decreased heart rate (bradycardia), increased heart rate (tachycardia), palpitations
- Loss of consciousness
- Vasodilation producing flushing
- Nosebleeds
- Dry mouth, mouth ulcers
- Black stools with blood (melena)
- Indigestion
- Dry skin, itching, acne, transient and mild alterations of nails and skin
- Bone pain
- Muscle cramps, muscle weakness, back pain
- Difficult urination
- Mild reactions at the injection site (skin swelling due to fluid retention (edema), pain, redness (erythema), skin hardening (induration), sensitivity, skin discoloration or swelling, extravasation (leakage of the medication outside the vein) that can produce cellulitis (inflammation and redness with pain), formation of fibrous tissue (cutaneous fibrosis), and skin tissue necrosis (cutaneous necrosis). The appearance of reactions at the injection site may be delayed from one week to 10 days
- Chest pain
- Chills
- Increased levels of certain enzymes in the blood (AST, SGOT).
Uncommon: may affect up to 1 in 100 patients
- Severe infection
- Severe decrease in blood pressure due to bacteria in the blood, accompanied by paleness and agitation, rapid pulse, moist skin (septic shock)
- Severe anemia
- Delayed hypersensitivity
- Severe hypersensitivity reactions (angioedema), which require therapy (e.g., due to decreased or increased blood pressure, facial swelling, tongue or lip swelling, respiratory problems, generalized rash, chills, back pain, chest pain, rapid heartbeat, stomach pain, hand and foot pain, sweating.)
- Weight loss, weight gain
- Dry eyes, lazy eye (amblyopia)
- Alteration in the visual field
- Myocardial infarction
- Heart failure (congestive heart failure)
- Cardiac muscle disorder (cardiomyopathy)
- Heart rhythm disorders (rapid heart rate: asymptomatic ventricular tachycardia, tachycardia with bigeminism)
- Heart conduction disorder (AV block), sometimes with loss of consciousness
- Alterations in the electrocardiogram
- Increased blood pressure
- Thrombosis, inflammation of the veins with the formation of blood clots in the veins, which often produces pain and tense, red skin
- Discoloration of the nails or nail matrix
- Severe increase in bilirubin (jaundice)
Rare: may affect up to 1 in 1,000 patients
- Severe blood infection (sepsis)
- Lung inflammation (pneumonia)
- Inflammation of the abdominal membrane (peritonitis)
- Fever associated with a decrease in white blood cells necessary to fight an infection (febrile neutropenia)
- Severe generalized hypersensitivity reactions with possible life-threatening potential (anaphylactic reactions)
- Alteration of the nerves related to movement, producing muscle weakness in arms and legs (motor neuropathy)
- Heart failure
- Respiratory failure
- Pleural effusion, pneumonia (interstitial pneumonia)
- Lung fibrosis, airway obstruction (pulmonary embolism), difficulty breathing
- Abdominal pain caused by constipation or a perforation in the intestine (intestinal obstruction/perforation)
- Pancreatitis, which produces severe abdominal and back pain
- Inflammation of the small intestine with possible severe persistent diarrhea (ischemic colitis)
- Redness of the skin
- Skin rash, intense itching rash (pruritus)
- Fever
- Loss of body fluids (dehydration)
- Fluid retention (edema)
- Weakness, general malaise
- Increased creatinine in the blood.
Very rare: may affect up to 1 in 10,000 patients
- Unexpected disorder of the cells that form the blood (acute myeloid leukemia, myelodysplastic syndrome)
- Severe generalized hypersensitivity reactions with possible life-threatening potential and shock
- Confusion, affectation of certain nerves (autonomic neuropathy), leading to paralysis of the intestinal muscles (paralytic ileus) and a sudden drop in blood pressure, sometimes with dizziness, produced for example by standing up quickly after sitting or lying down (orthostatic hypotension)
- Seizures (epileptic), brain affectation characterized by convulsions and decreased consciousness (encephalopathy), coordination problems (ataxia)
- Headache
- Dizziness
- Affectation of the optic nerve and/or visual alterations (scintillating scotoma)
- Ear damage (ototoxicity), hearing loss, dizziness (vertigo)
- Perception of noises (tinnitus)
- Irregular and rapid heart rhythm (atrial fibrillation)
- Rapid heart rate originating from a specific part of the heart (supraventricular tachycardia)
- Shock
- Cough
- High blood pressure in the lungs
- Inflammation of the small intestine with possible severe persistent diarrhea (neutropenic colitis, pseudomembranous colitis; necrotizing colitis)
- Blood clots in the abdominal membrane (mesenteric thrombosis)
- Inflammation of the throat (esophagitis)
- Fluid retention in the abdominal cavity (ascites)
- Constipation
- Alterations in liver function (liver necrosis, hepatic encephalopathy), with reported cases of fatal outcome
- Severe hypersensitivity reactions, including fever, red spots on the skin, joint pain, and/or eye inflammation (Stevens-Johnson syndrome)
- Local skin necrosis (necrotizing epidermolysis); irregular redness (exudative) with red spots (erythema multiforme), hives, and blister formation (urticaria)
- Nail loss (patients should protect their hands and feet from the sun)
- Inflammation of the hair follicles (folliculitis)
- Inflammation of the skin with blisters or peeling (exfoliative dermatitis)
Frequency not known: the frequency cannot be estimated from the available data
- Complications produced by the waste products of destroyed cancer cells (tumor lysis syndrome)
- Fluid accumulation in the eyes (macular edema), flashes in the eyes (photopsia), small spots or particles floating in the visual field (vitreous floaters), increased tear secretion
- Inflammation of a vein (phlebitis)
- Excessive collagen deposits in the skin (scleroderma)
- Autoimmune disease with multiple symptoms, such as red, scaly patches on the skin, joint pain, or fatigue (systemic lupus erythematosus) or red, thick, and frequently scaly and ulcerative rashes that can burn or itch (cutaneous lupus erythematosus)
- Redness and swelling of the palms of the hands and the soles of the feet that can cause skin peeling
- Disseminated intravascular coagulation (DIC) has been reported. This is a serious condition that causes easy bleeding, easy blood clotting, or both.
- Acute inflammatory reaction limited to previously irradiated areas, triggered by the administration of systemic precipitating agents after radiation treatment (recall phenomenon)
- Excessive sweating (hyperhidrosis)
Reporting of Adverse Effects
If you experience any of the adverse effects, consult your doctor or pharmacist, even if it is a possible adverse effect that is not listed in this prospectus. You can also report them directly through the Spanish Pharmacovigilance System for Human Use Medicines, Website: www.notificaram.es. By reporting adverse effects, you can contribute to providing more information on the safety of this medicine.
5. Storage of Paclitaxel Teva
Keep this medicine out of the sight and reach of children.
Do not use this medicine after the expiration date that appears on the vial and on the packaging after "EXP" or "CAD". The first two numbers indicate the month, the last numbers indicate the year. The expiration date is the last day of the month indicated.
This medicine does not require any special storage temperature, store in the original packaging.
Freezing does not have harmful effects on the medicine
Medicines should not be disposed of through wastewater or household waste. Deposit the packaging and medicines that you no longer need at the SIGRE Point in the pharmacy. In case of doubt, ask your pharmacist how to dispose of the packaging and medicines that you no longer need. This way, you will help protect the environment.
6. Container Contents and Additional Information
Composition of Paclitaxel Teva
The active ingredient is paclitaxel.
Each ml of Paclitaxel Teva concentrate for solution for infusion contains 6 mg of paclitaxel.
The other components are: macrogolglycerol ricinoleate, anhydrous ethanol, and citric acid.
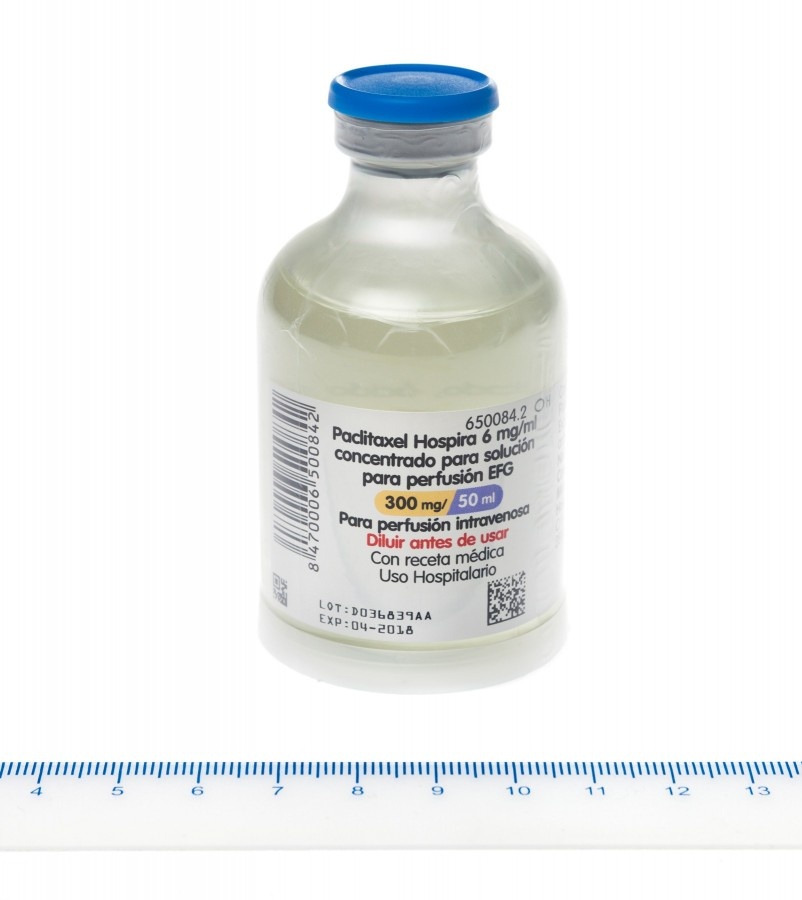
Appearance of the Product and Container Contents
Paclitaxel is a viscous, transparent, colorless or slightly yellowish solution. It is presented in vials of 5 ml, 16.7 ml, 25 ml, and 50 ml.
Each 5 ml vial contains 30 mg of paclitaxel.
Each 16.7 ml vial contains 100 mg of paclitaxel.
Each 25 ml vial contains 150 mg of paclitaxel.
Each 50 ml vial contains 300 mg of paclitaxel.
Only some pack sizes may be marketed.
Marketing Authorization Holder
Teva Pharma, S.L.U.
C/Anabel Segura, 11. Edificio Albatros B, 1ª planta.
28108 Alcobendas (Madrid)
Spain
Manufacturer:
Pharmachemie B.V.
Swensweg 5, P.O. Box 552
2003 RN Haarlem
Netherlands
This medicinal product is authorized in the Member States of the European Economic Area under the following names:
Belgium Paclitaxin 6 mg/ml concentrate for solution for infusion (30 mg/5 ml)
Paclitaxin 6 mg/ml concentrate for solution for infusion (100 mg/16.7 ml)
Paclitaxin 6 mg/ml concentrate for solution for infusion (150 mg/25 ml)
Paclitaxin 6 mg/ml concentrate for solution for infusion (300 mg/50 ml)
Estonia Paclitaxel-Teva
France Paclitaxel-Teva 6 mg/ml solution to be diluted for infusion
Germany Paclitaxel-GRY® 6 mg/ml concentrate for solution for infusion
Greece Paxene Paclitaxin
Hungary Paclitaxel-Teva 6 mg/ml concentrate for solution for infusion
Italy Paclitaxel Teva 6 mg/ml concentrated solution for infusion
Lithuania Paclitaxel-Teva 6 mg/ml concentrate for infusion solution
Luxembourg Paclitaxin 6 mg/ml solution to be diluted for infusion (30 mg/5 ml)
Paclitaxin 6 mg/ml solution to be diluted for infusion (100 mg/16.7 ml)
Paclitaxin 6 mg/ml solution to be diluted for infusion (150 mg/25 ml)
Paclitaxin 6 mg/ml solution to be diluted for infusion (300 mg/50 ml)
Netherlands Paclitaxin concentrate for intravenous solution 6 mg/ml
Slovenia Paclitaxin 6 mg/ml, concentrate for solution for infusion
Spain Paclitaxel Teva 6 mg/ml, concentrate for solution for infusion EFG
Date of the last revision of this leaflet:November 2024
This information is intended only for healthcare professionals:
The following is a summary of information to aid in the administration of Paclitaxel. You should have experience in handling and using cytotoxics and be familiar with the Paclitaxel Summary of Product Characteristics. Refer to the guidelines for the safe handling of antineoplastic agents.
Handling:As with this type of drug, paclitaxel should be handled with caution. Pregnant women should not handle this product.
Dilutions should be carried out under aseptic conditions by experienced personnel and in a specific area. Precautions should be taken to avoid any contact with the skin and mucous membranes. Protective gloves should be worn. In case of skin contact, the affected area should be washed with water and soap. After topical exposure, tingling, burning sensation, and redness have been described.
In case of contact with mucous membranes, wash abundantly with water. In case of inhalation, difficulty in breathing, chest pain, burning sensation in the throat, and nausea may occur.
If the closed vials are refrigerated or frozen, a precipitate may form that redissolves by gently shaking or without shaking when it reaches room temperature. This does not affect the quality of the product. If the solution remains turbid or if an insoluble precipitate remains, the vial should be discarded.
After multiple insertions and withdrawals of the needles, the vials maintain microbiological, physical, and chemical stability for up to 28 days at 25°C. Storage under other conditions and times are the responsibility of the user.
The "Chemo-Dispensing Pin" devices or similar ones should not be used, as they may cause the collapse of the elastomer, resulting in the loss of sterility integrity.
Preparation for Intravenous Administration:
Before proceeding with the infusion, Paclitaxel Teva should be diluted using aseptic techniques employing 0.9% sodium chloride solution for infusion (9 mg/ml), or 5% glucose solution for infusion (50 mg/ml), or a mixture of 5% glucose solution for infusion (50 mg/ml) and 0.9% sodium chloride solution for infusion (9 mg/ml), or 5% glucose Ringer's solution for infusion, to a final concentration of 0.3 to 1.2 mg/ml.
It has been demonstrated that the prepared infusion solution is physically and chemically stable for use for 27 hours at 25°C, when diluted in a mixture of 0.9% sodium chloride solution for infusion (9 mg/ml) and 5% glucose solution for infusion (50 mg/ml) or 5% glucose Ringer's solution for infusion.
Chemical and physical stability of the prepared infusion solution has been demonstrated for 14 days at 5°C and 25°C when diluted in 5% glucose solution for infusion (50 mg/ml) and 0.9% sodium chloride solution for infusion (9 mg/ml).
Microbiological stability has been demonstrated for the use of the prepared infusion solution for 27 hours at 25°C. Storage under other conditions is the responsibility of the user.
After preparation, these solutions may present a slightly turbid appearance attributed to the excipient of the preparation, which is not eliminated by filtration. Paclitaxel should be administered with a series filter provided with a microporous filtering membrane, with pores ≤ 0.22 μm. No significant losses of potency have been observed after simulated release of the solution through IV infusion filter equipment.
Isolated cases of precipitation during paclitaxel infusions have been reported, usually towards the end of the 24-hour infusion period. Although the cause of this precipitation has not been established, it is probably related to the supersaturation of the diluted solution. To reduce the risk of precipitation, paclitaxel should be administered as soon as possible after dilution, and excessive agitation, vibration, or shaking should be avoided. Infusion equipment should be thoroughly washed before use. During infusion, the appearance of the solution should be regularly examined, and if precipitation is observed, the infusion should be interrupted.
To minimize patient exposure to DEHP (di-(2-ethylhexyl) phthalate) that may be formed by leaching of PVC present in bags, infusion equipment, or other medical devices, the diluted paclitaxel solutions should be stored in non-PVC containers (glass, polypropylene) or plastic bags (polypropylene, polyolefin) and administered with polyethylene equipment. The use of filter models that have a short PVC plastic inlet/outlet tube is not significant because the amount of DEHP that may be released is not significant.
Disposal of Waste:All remnants of the medicinal product and materials used in the preparation and administration, and those that may have come into contact with paclitaxel, must comply with local regulations regarding the handling of cytotoxic products.
Administration and Dosage:
Prior to administration, all patients should receive premedication with corticosteroids, antihistamines, and H2 antagonists. The diluted Paclitaxel infusion should be administered through a series filter that does not contain PVC with a microporous membrane ≤ 0.22 μm.
The recommended doses for intravenous infusion of paclitaxel are as follows:
First-line ovarian cancer: 135 mg/m2 for 24 hours, followed by cisplatin 75 mg/m2; or 175 mg/m2 for 3 hours, followed by cisplatin 75 mg/m2;
Second-line ovarian or breast carcinoma: 175 mg/m2 for 3 hours;
Adjuvant treatment of breast cancer: 175 mg/m2 for 3 hours; following treatment with anthracyclines and cyclophosphamide (AC);
First-line breast cancer: 220 mg/m2 for 24 hours, 24 hours after doxorubicin (50 mg/m2), 175 mg/m2 for 3 hours, followed by trastuzumab (see Trastuzumab Summary of Product Characteristics);
Non-small cell lung cancer: 175 mg/m2 for 3 hours, followed by cisplatin 80 mg/m2;
AIDS-related Kaposi's sarcoma: 100 mg/m2 for 3 hours.
Storage:
No special storage conditions are required. If refrigerated, a precipitate may form that redissolves by gently shaking or without shaking when it reaches room temperature. This does not affect the quality of the product. If the solution remains turbid or if an insoluble precipitate remains, the vial should be discarded. Freezing does not adversely affect the product.
An expiry date is indicated on the outer packaging and the product label. It should not be used after this date.
- Country of registration
- Active substance
- Prescription requiredYes
- Manufacturer
- This information is for reference only and does not constitute medical advice. Always consult a doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to PACLITAXEL TEVA 6 mg/ml CONCENTRATE FOR INFUSION SOLUTIONDosage form: INJECTABLE PERFUSION, 100 mgActive substance: paclitaxelManufacturer: Bristol-Myers Squibb Pharma EeigPrescription requiredDosage form: INJECTABLE PERFUSION, 5 mg/mlActive substance: paclitaxelManufacturer: Whiteoak Pharmaceutical B.V.Prescription requiredDosage form: INJECTABLE PERFUSION, 5 mg/mlActive substance: paclitaxelManufacturer: Laboratorio Stada S.L.Prescription required
Online doctors for PACLITAXEL TEVA 6 mg/ml CONCENTRATE FOR INFUSION SOLUTION
Discuss questions about PACLITAXEL TEVA 6 mg/ml CONCENTRATE FOR INFUSION SOLUTION, including use, safety considerations and prescription review, subject to medical assessment and local regulations.
Frequently Asked Questions






