EMEND 80 mg HARD CAPSULES


How to use EMEND 80 mg HARD CAPSULES
Translated with AI
This page provides general information and does not replace a doctor’s consultation. Always consult a doctor before taking any medication. Seek urgent medical care if symptoms are severe.
Show originalContents of the leaflet
Introduction
Package Leaflet: Information for the User
EMEND 80 mg hard capsulesaprepitant
Read all of this leaflet carefully before you start taking this medicine because it contains important information for you. If you are the parent of a child who is taking EMEND, read this information carefully.
- Keep this leaflet, you may need to read it again.
- If you have any further questions, ask your doctor, pharmacist or nurse.
- This medicine has been prescribed for you or your child only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours or your child's.
- If you or your child get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in this leaflet. See section 4.
Contents of the pack
- What is EMEND and what is it used for
- What you need to know before you take or give EMEND
- How to take EMEND
- Possible side effects
- Storing EMEND
- Contents of the pack and other information
1. What is EMEND and what is it used for
EMEND contains the active substance aprepitant and belongs to a group of medicines called "neurokinin 1 (NK1) receptor antagonists". The brain has a specific area that controls nausea and vomiting. EMEND works by blocking the signals to this area, and thus reducing nausea and vomiting. EMEND hard capsules are used in adults and adolescents from 12 years of age, in combination with other medicinesto prevent nausea and vomiting caused by a type of chemotherapy (cancer treatment) that induces strong and moderate nausea and vomiting (such as cisplatin, cyclophosphamide, doxorubicin or epirubicin).
2. What you need to know before you take or give EMEND
Do not take EMEND
- if you or your child are allergic to aprepitant or any of the other ingredients of this medicine (listed in section 6).
- with medicines that contain pimozide (used to treat psychiatric disorders), terfenadine and astemizole (used for allergic rhinitis and other allergic disorders), cisapride (used to treat digestive problems). Tell your doctor if you or your child are taking these medicines as the treatment may need to be changed before you or your child start taking EMEND.
Warnings and precautions
Consult your doctor, pharmacist or nurse before you start taking EMEND or giving it to your child.
Before treatment with EMEND, tell your doctor if you or your child have liver disease, as the liver is important for removing the medicine from the body. Your doctor may need to monitor your liver or your child's liver.
Children and adolescents
Do not give EMEND 80 mg and 125 mg capsules to children under 12 years of age, as the 80 mg and 125 mg capsules have not been studied in this population.
Other medicines and EMEND
EMEND may affect other medicines during and after treatment with EMEND. There are some medicines that should not be taken with EMEND (such as pimozide, terfenadine, astemizole and cisapride) or that require a dose adjustment (see also ‘Do not take EMEND’).
The effects of EMEND or other medicines may be influenced if you or your child take EMEND with other medicines, including those listed below. Consult your doctor or pharmacist if you or your child are taking any of the following medicines:
- contraceptive medicines that may include birth control pills, skin patches, implants and certain intrauterine devices (IUDs) that release hormones, may not work properly when taken with EMEND. During treatment with EMEND and for up to 2 months after using EMEND, you or your child must use other or additional non-hormonal methods of contraception,
- ciclosporin, tacrolimus, sirolimus, everolimus (immunosuppressants),
- alfentanil, fentanyl (used to treat pain),
- quinidine (used to treat irregular heartbeat),
- irinotecan, etoposide, vinorelbine, ifosfamide (cancer medicines),
- medicines that contain ergot derivatives, such as ergotamine or dihydroergotamine (used to treat migraines),
- warfarin, acenocoumarol (blood thinners; blood tests may be needed),
- rifampicin, clarithromycin, telithromycin (antibiotics used to treat infections),
- phenytoin (a medicine used to treat seizures),
- carbamazepine (used to treat depression and epilepsy),
- midazolam, triazolam, phenobarbital (medicines used to calm or help sleep),
- St. John's Wort (a herbal preparation used to treat depression),
- HIV protease inhibitors (used to treat HIV infections),
- ketoconazole, except shampoo (used to treat Cushing's syndrome - when the body produces too much cortisol),
- itraconazole, voriconazole, posaconazole (antifungals),
- nefazodone (used to treat depression),
- corticosteroids (such as dexamethasone and methylprednisolone),
- anxiety medicines (such as alprazolam),
- tolbutamide (a medicine used to treat diabetes).
Tell your doctor or pharmacist if you or your child are taking, have recently taken or might take any other medicines.
Pregnancy and breast-feeding
Do not use this medicine during pregnancy unless clearly necessary. If you or your daughter are pregnant or breast-feeding, think you may be pregnant or are planning to have a baby, ask your doctor for advice before taking this medicine.
For information on contraception, see ‘Other medicines and EMEND’.
It is not known if EMEND passes into breast milk; therefore, breast-feeding should be avoided during treatment with this medicine. It is important to tell your doctor before taking this medicine if you or your daughter are breast-feeding or plan to breast-feed.
Driving and using machines
Some people may feel dizzy or drowsy after taking EMEND. If you or your child feel dizzy or drowsy, do not drive, ride a bicycle or use machines or tools after taking this medicine (see ‘Possible side effects’).
EMEND contains sucrose
EMEND hard capsules contain sucrose. If your doctor has told you or your child that you or they have an intolerance to some sugars, consult your doctor before taking this medicine.
EMEND contains sodium
This medicine contains less than 23 mg of sodium (1 mmol) per capsule; this is essentially “sodium-free”.
3. How to take EMEND
Always take or give EMEND exactly as your doctor, pharmacist or nurse has told you or your child. If you are not sure, check with your doctor, pharmacist or nurse. Take EMEND always with other medicines to prevent nausea and vomiting. After treatment with EMEND, your doctor may ask you or your child to continue taking other medicines to prevent nausea and vomiting, including corticosteroids (such as dexamethasone) and a ‘5-HT3 antagonist’ (such as ondansetron). If you are not sure, check with your doctor, pharmacist or nurse.
The recommended oral dose of EMEND is:
Day 1:
- one 125 mg capsule 1 hour before starting chemotherapy
and
Days 2 and 3:
- one 80 mg capsule each day.
- if you are not receiving chemotherapy, take EMEND in the morning.
- if you are receiving chemotherapy, take EMEND 1 hour before starting your chemotherapy session.
EMEND can be taken with or without food. Swallow the capsule whole with some liquid.
If you take more EMEND than you should
Do not take more capsules than your doctor recommends. If you or your child have taken too many capsules, contact your doctor immediately.
If you forget to take EMEND
If you or your child have missed a dose, ask your doctor for advice.
If you have any further questions on the use of this medicine, ask your doctor or pharmacist.
4. Possible side effects
Like all medicines, this medicine can cause side effects, although not everybody gets them.
Stop taking EMEND and contact your doctor immediately if you or your child notice any of the following serious side effects, for which you or your child may need urgent medical treatment:
- Hives, rash, itching, difficulty breathing or swallowing (frequency not known, cannot be estimated from the available data): these are signs of an allergic reaction.
Other side effects that have been reported are listed below.
Common side effects (may affect up to 1 in 10 people) are:
- constipation, indigestion,
- headache,
- fatigue,
- loss of appetite,
- hiccups,
- increased amount of liver enzymes in the blood.
Uncommon side effects (may affect up to 1 in 100 people) are:
- dizziness, drowsiness,
- acne, rash,
- anxiety,
- belching, nausea, vomiting, heartburn, stomach pain, dry mouth, flatulence,
- increased painful or burning urination,
- weakness, general feeling of being unwell,
- flushing/redness of the face or skin,
- rapid or irregular heartbeat,
- fever with increased risk of infection, decrease in red blood cells.
Rare side effects (may affect up to 1 in 1,000 people) are:
- difficulty thinking, lack of energy, altered taste,
- sensitivity of the skin to sunlight, excessive sweating, oily skin, skin ulcers, itchy rash, Stevens-Johnson syndrome/toxic epidermal necrolysis (a rare, serious skin reaction),
- euphoria (feeling of extreme happiness), disorientation,
- bacterial infection, fungal infection,
- severe constipation, stomach ulcer, inflammation of the small intestine and colon, mouth ulcers, abdominal swelling,
- frequent need to urinate, urinating more than usual, presence of sugar or blood in the urine,
- chest discomfort, swelling, changes in walking,
- cough, mucous in the back of the throat, throat irritation, sneezing, sore throat,
- eye discharge and itching,
- ringing in the ears,
- muscle spasms, muscle weakness,
- excessive thirst,
- slow heartbeat, problems with blood vessels and veins,
- decrease in white blood cells, low sodium levels in the blood, weight loss,
Reporting of side effects
If you or your child experience any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in this leaflet. You can also report side effects directly via the national reporting system listed in the Appendix.
- By reporting side effects, you can help provide more information on the safety of this medicine.
5. Storing EMEND
Keep this medicine out of the sight and reach of children.
Do not use this medicine after the expiry date which is stated on the carton after EXP. The expiry date refers to the last day of the month.
Store in the original package to protect from moisture. Do not remove the capsule from the blister until you are ready to take it.
Medicines should not be disposed of via wastewater or household waste. Ask your pharmacist how to dispose of medicines no longer required. These measures will help protect the environment.
6. Contents of the pack and other information
What EMEND contains
- The active substance is aprepitant. Each 125 mg hard capsule contains 125 mg of aprepitant. Each 80 mg hard capsule contains 80 mg of aprepitant.
- The other ingredients are sucrose, microcrystalline cellulose (E-460), hydroxypropylcellulose (E-463), sodium lauryl sulfate, gelatin, titanium dioxide (E-171), lacquer, potassium hydroxide and iron oxide black (E-172); the 125 mg hard capsule also contains iron oxide red (E-172) and iron oxide yellow (E-172).
Appearance and packaging
The 125 mg hard capsule is opaque with a white body and a pink cap with “462” and “125 mg” printed in a radial manner in black ink on the body.
The 80 mg hard capsule is opaque with a white body and a white cap with “461” and “80 mg” printed in a radial manner in black ink on the body.
EMEND 125 mg and 80 mg hard capsules are supplied in the following pack sizes:
- Aluminium blister pack containing one 80 mg capsule
- 2-day treatment pack containing two 80 mg capsules
- 5 aluminium blister packs, each containing one 80 mg capsule
- Aluminium blister pack containing one 125 mg capsule
- 5 aluminium blister packs, each containing one 125 mg capsule
- 3-day treatment pack containing one 125 mg capsule and two 80 mg capsules
Not all pack sizes may be marketed.
Marketing authorisation holder and manufacturer
Merck Sharp & Dohme B.V.
Waarderweg 39
2031 BN Haarlem
Netherlands
For further information on this medicine, contact the local representative of the Marketing Authorisation Holder:
Belgique/België/Belgien Lietuva
MSD Belgium BVBA/SPRL UAB Merck Sharp & Dohme Tel/Tel: +32(0)27766211 Tel. + 370 5278 02 47 [email protected] [email protected]
????????
???? ???? ? ???? ???????? ???? ???.: +359 2 819 3737 [email protected]
Ceská republika
Merck Sharp & Dohme s.r.o. Tel: +420 233 010 111 [email protected]
Danmark
MSD Danmark ApS Tlf: + 45 4482 4000 [email protected]
Deutschland
MSD SHARP & DOHME GMBH Tel: 0800 673 673 673 (+49 (0) 89 4561 2612) [email protected]
Eesti
Merck Sharp & Dohme OÜ Tel.: +372 6144 200 [email protected]
Eλλ?δα
MSD Α.Φ.Β.Ε.Ε. Τηλ: +30 210 98 97 300 [email protected]
España
Merck Sharp & Dohme de España, S.A. Tel: +34 91 321 06 00 [email protected]
France
MSD France Tél:+33(0)1 80 4640 40
Hrvatska
Merck Sharp & Dohme d.o.o. Tel: + 385 1 6611 333 [email protected]
Ireland
Merck Sharp & Dohme Ireland (Human Health) Limited Tel: +353 (0)1 2998700 [email protected]
Ísland
Vistor hf. Simi: +354 535 7000
Luxembourg/Luxemburg
MSD Belgium BVBA/SPRL Tél/Tel: +32(0)27766211 [email protected]
Magyarország
MSD Pharma Hungary Kft. Tel.: +36 1 888 5300 [email protected]
Malta
Merck Sharp & Dohme Cyprus Limited Tel: 8007 4433 (+356 99917558) [email protected]
Nederland
Merck Sharp & Dohme B.V. Tel: 0800 9999000
(+31 23 5153153) [email protected]
Norge
MSD (Norge) AS Tlf: +47 32 20 73 00 [email protected]
Österreich
Merck Sharp & Dohme Ges.m.b.H. Tel: +43 (0) 1 26 044 [email protected]
Polska
MSD Polska Sp. z o.o. Tel: +48 22 549 51 00 [email protected]
Portugal
Merck Sharp & Dohme, Lda Tel: +351 21 4465700 [email protected]
România
Merck Sharp & Dohme Romania S.R.L. Tel: +40 21 529 29 00 [email protected]
Slovenija
Merck Sharp & Dohme, inovativna zdravila
d.o.o. Tel: +386 1 5204 201 [email protected]
Slovenská republika
Merck Sharp & Dohme, s. r. o. Tel: +421 2 58282010 [email protected]
Ιtalia
MSD Italia S.r.l. Tel: +39 06 361911 [email protected]
Κ?προς
Merck Sharp & Dohme Cyprus Limited Τηλ.: 800 00 673 (+357 22866700) [email protected]
Latvija
SIA Merck Sharp & Dohme Latvija Tel: +371 67364224 [email protected]
Suomi/Finland
MSD Finland Oy Puh/Tel: +358 (0)9 804 650 [email protected]
Sverige
Merck Sharp & Dohme (Sweden) AB Tel: +46 77 5700488 [email protected]
United Kingdom
Merck Sharp & Dohme Limited Tel: +44 (0) 1992 467272 [email protected]
Date of last revision of this leaflet:
Other sources of information
Detailed information on this medicine is available on the European Medicines Agency web site: http://www.ema.europa.eu.
This information is intended solely for healthcare professionals:
Instructions for healthcare professionals on the preparation of the oral suspension
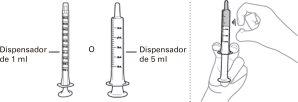
Each box of EMEND contains a sachet with the powder for oral suspension, a 1 ml oral dispenser, a 5 ml oral dispenser, a cap, and a mixing cup. |
|
|
|
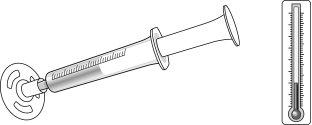
Check that there is no air in the oral dispenser (if there is air, remove it). |
|
|
|
|
|
Hold the EMEND powder sachet for oral suspension upright and shake the contents down before opening the sachet.
|
|
To avoid foam, do not shake the mixing cup. The mixture will be a cloudy to clear pink color. |
|
|
| ||
Check that there is no air in the oral dispenser (if there is air, remove it). Check that the oral dispenser contains the prescribed dose. |
| ||
Day 1 | Day 2 | Day 3 | |
EMEND oral suspension 25 mg/ml | 3 mg/kg orally Maximum dose 125 mg | 2 mg/kg orally Maximum dose 80 mg | 2 mg/kg orally Maximum dose 80 mg |
|
| ||
Discard any leftover suspension and materials that have come into contact with it. The disposal of unused medication and all materials that have come into contact with it will be carried out in accordance with local regulations. |
- Country of registration
- Active substance
- Prescription requiredYes
- Manufacturer
- This information is for reference only and does not constitute medical advice. Always consult a doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to EMEND 80 mg HARD CAPSULESDosage form: CAPSULE, 125 and 80 mgActive substance: aprepitantManufacturer: Accord Healthcare S.L.U.Prescription requiredDosage form: CAPSULE, 125 mgActive substance: aprepitantManufacturer: Qilu Pharma Spain S.L.Prescription requiredDosage form: CAPSULE, 125 mg/80 mgActive substance: aprepitantManufacturer: Qilu Pharma Spain S.L.Prescription required
Online doctors for EMEND 80 mg HARD CAPSULES
Discuss questions about EMEND 80 mg HARD CAPSULES, including use, safety considerations and prescription review, subject to medical assessment and local regulations.
Frequently Asked Questions